1
PULMONARY EMBOLISM
Dr.Mohammed Ali
Refers to exogenous or endogenous material that travels to the lungs through the
pulmonary circulation, causing a potential spectrum of consequences. It occurs in
approximately 1% of all patients admitted to hospital and accounts for around 5%
of in-hospital deaths. It is a common mode of death in patients with cancer, stroke
and pregnancy.
POTENTIAL SOURCES OF EMBOLI
Thrombotic PE :The majority (79%) of pulmonary emboli arise from the
propagation of lower limb Deep venous thrombosis
Non thrombotic PE
Septic emboli (endocarditis affecting the tricuspid or pulmonary valves)
Tumor cells especially choriocarcinoma
Air bubbles,
Amniotic fluid and placenta.
Intravenous catheters,
Fat droplets,
Intravenous drug abusers.
Risk factors of VENOUS THROMBOEMBOLISM
I
. Surgery
Major abdominal/pelvic surgery
Hip/knee surgery
Post-operative intensive care
II. Obstetrics
Pregnancy / puerperium .
Oral contraceptives .
Postmenopausal
hormone
replacement.
III. Cardiorespiratory disease
COPD.
Congestive cardiac failure .
IV. Lower limb problems
Fracture
Varicose veins
Stroke/spinal cord injury
V. Malignant disease
Abdominal pelvic
Advanced/metastatic
Concurrent chemotherapy
VI. Thrombotic disorders
Antiphospholipid antibody syndrome.
Antithrombin deficiency
Protein C and S deficiencies
VII. Miscellaneous
Obesity.
Cigarette smoking
Increasing age
Previous proven VTE
Immobility .
Trauma
2
PATHOPHISIOLOGY
1-Embolization :Venous thrombi develop most commonly in the leg veins .
2. Gas exchange abnormalities :Hypoxemia
Other pathophysiological abnormalities
Increased pulmonary vascular resistance
Impaired gas exchange
Alveolar hyperventilation
Increased airway resistance due to constriction of airways distal to the
bronchi
Decreased pulmonary compliance due to lung edema, lung hemorrhage, or
loss of surfactant
Right ventricular failure
Clinical features
VTE can be difficult to diagnose. It may be helpful to consider the following:
1. Is the clinical presentation consistent with PE?
2. Does the patient have risk factors for PE?
3. Are there any alternative diagnoses that can explain the patient's
presentation?
Presentation varies depending on the number, size and distribution of emboli, and
the underlying cardiorespiratory reserve . A recognised risk factor is present in
between 80% and 90% of patients. The presence of one or more risk factors may
multiply the risk.
Predicting the pre-test probability of deep vein thrombosis
Clinical characteristic
Score
Active cancer (patient receiving treatment for cancer within the previous 6 months
or currently receiving palliative treatment)
1
Paralysis, paresis or recent plaster immobilisation of the lower extremities
1
Recently bedridden for 3 days or more, or major surgery within the previous 4
week1
Localised tenderness along the distribution of the deep venous system
1
Entire leg swollen
1
Calf swelling at least 3 cm larger than that on the asymptomatic side (measured 10
cm
below
the
tibial
tuberosity)
1
3
Pitting
oedema
confined
to
the
symptomatic
leg
1
Collateral superficial veins (non-varicose)
1
Alternative
diagnosis
at
least
as
likely
as
DVT
-2
Clinical probability
Total score
DVT low probability < 1
DVT moderate probability
1-2
DVT high probability
> 2
Pulmonary embolism wells score
Symptom
of
DVT
(3PIONTS)
No
alternative
diagnosis
better
explain
the
illness
(3PIONTS)
Tachycardia with pulse rate >100b/m (1.5
PIONTS)
Immobilization ( >= 3days ) or surgery in the previous 4 weeks (1.5
PIONTS)
Prior history of DVT or pulmonary embolism (1.5
PIONTS)
Presence of hemoptysis (1
PIONTS)
Presence of malignancy (1
PIONTS)
Score >6 high probablity
Score >=2 and<=6 moderate probablity
Score <2 low probablity
Other symptoms
Dyspnea
Pleuritic chest pain
Cough
Hemoptysis
Leg swelling
Leg pain
Palpitations
Wheezing
Signs
Tachypnea (≥20/min)
Rales (crackles)
Tachycardia (>100/min)
Fourth heart sound
Increased pulmonary component of second sound
Deep venous thrombosis
Diaphoresis
4
Angina-like pain
Temperature >38.5°C
Wheezes
Homans' sign
Right ventricular lift
Pleural friction rub
Third heart sound
Cyanosis
The clinical features of PE depend
1. largely upon the size of embolism.
2. Size of the artery.
3. Co_morbidity.
PE divided in to:
1.Acute massive PE
small/medium PE
2. Chronic PE.
Acute massive PE
massive embolus lodge in the proximal pulmonary arteries & the chambers of the
right heart.
Symptoms: Faintness or collapse, crushing central chest pain, severe dyspnoea
Signs: Major circulatory collapse: tachycardia, hypotension,↑ JVP, right
ventricular gallop rhythm, loud P
2
, severe cyanosis,↓urinary output
Acute small/medium PE
Occlusion of segmental pulmonary artery → infarction ± effusion.Symptoms:
Pleuritic chest pain, restricted breathing, haemoptysis .Signs: Tachycardia, pleural
rub, raised hemidiaphragm, crackles, effusion (often blood-stained), low-grade
fever
Chronic PE
Chronic occlusion of pulmonary microvasculature, pulmonary hyper tension and
right heart failure.
Symptoms: Exertional dyspnoea. Late symptoms of pulmonary hypertension or
right heart failure.Signs: May be minimal early in disease. Later: RV heave, loud
P
2
. Terminal: signs of right heart failure
DIFFERENTIAL DIAGNOSIS of PE:
1. Myocardial infarction
2. Pericarditis
3. Heart failure
4. Pneumonia
9. Pleuritis
from
connective
tissue
disease
10. Thoracic herpes zoster (“shingles”)
11. Rib fracture
5
5. Asthma
6. Chronic obstructive pulmonary
disease
7. Pneumothorax
8. Pleurodynia
12. Musculoskeletal pain
13. Primary or metastatic intrathoracic
cancer
14. Infradiaphragmatic processes (e.g.,
acute cholecystitis, splenic infarction)
15. Hyperventilation syndrome
DVT
1. Ruptured Baker s cyst.
2. Cellulitis .
3. Post phelibitic syndrome , venous insufficiency.
DIAGNOSIS
Investigations of PE
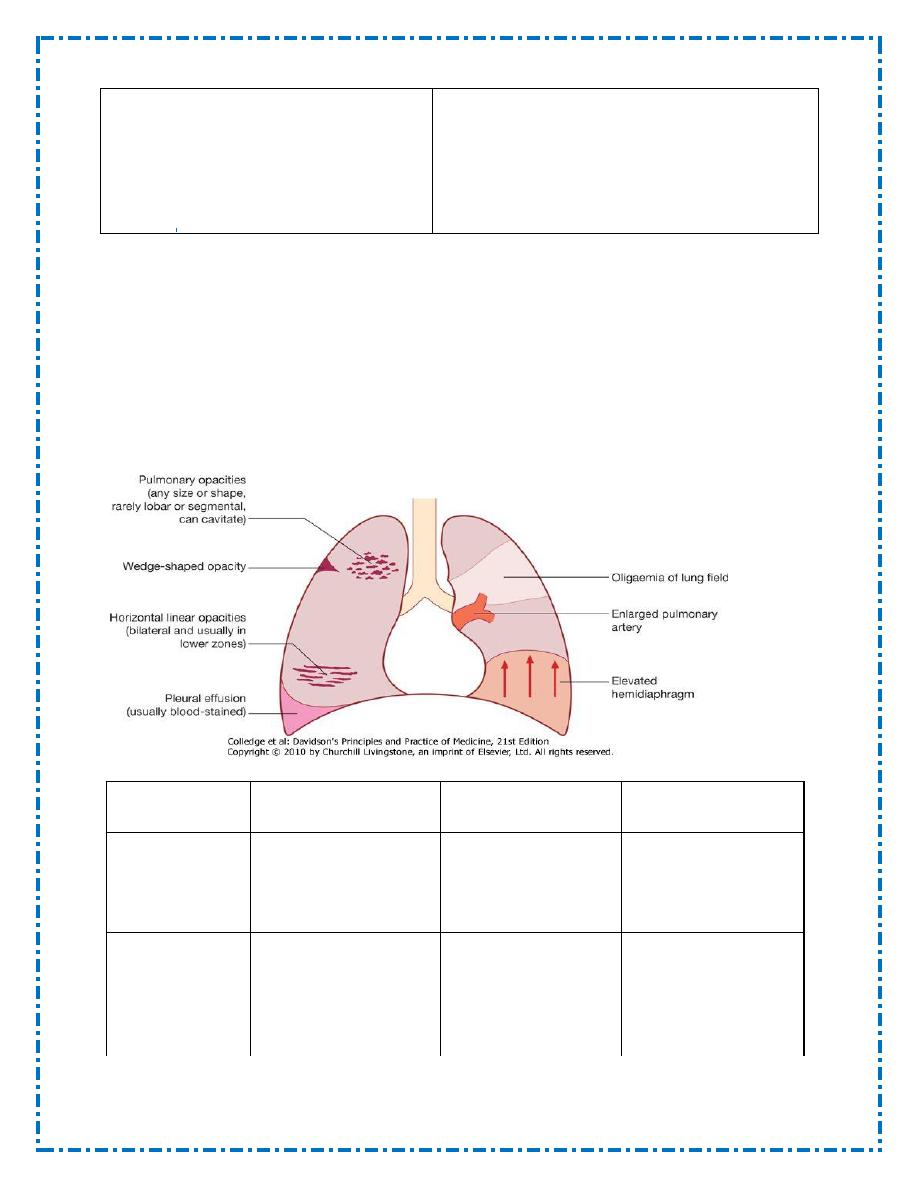
Chest radiography: A variety of non-specific appearances have been described
Features of pulmonary thromboemboli
Acute massive PE
Acute small/medium
PE
Chronic PE
Pathophysiology Major haemodynamic
effects: ↓cardiac
output; acute right
heart failure
Occlusion of
segmental
pulmonary artery →
infarction ± effusion
Chronic occlusion of
pulmonary
microvasculature,
right heart failure
Symptoms
Faintness or collapse,
crushing central chest
pain, apprehension,
severe dyspnoea
Pleuritic chest pain,
restricted breathing,
haemoptysis
Exertional dyspnoea.
Late symptoms of
pulmonary
hypertension or right
heart failure
6
Signs
Major circulatory
collapse: tachycardia,
hypotension,↑ JVP,
right ventricular
gallop rhythm, loud
P
2
, severe cyanosis,
↓urinary output
Tachycardia, pleural
rub, raised
hemidiaphragm,
crackles, effusion
(often blood-
stained), low-grade
fever
May be minimal
early in disease.
Later: RV heave,
loud P
2
. Terminal:
signs of right heart
failure
Chest X-ray
Usually normal. May
be subtle oligaemia
Pleuropulmonary
opacities, pleural
effusion, linear
shadows, raised
hemidiaphragm
Enlarged pulmonary
artery trunk,
enlarged heart,
prominent RV
ECG
S
1
Q
3
T
3
anterior T-
wave inversion, right
bundle branch block
(RBBB)
Sinus tachycardia
RV hypertrophy and
strain
Arterial blood
gases
Markedly abnormal
with ↓PaO
2
and
↓PaCO
2
. Metabolic
acidosis
May be normal or
↓PaO
2
or ↓PaCO
2
Exertional ↓PaO
2
or
desaturation on
formal exercise
testing
Alternative
diagnoses
Myocardial
infarction, pericardial
tamponade, aortic
dissection
Pneumonia,
pneumothorax,
musculoskeletal
chest pain
Other causes of
pulmonary
hypertension
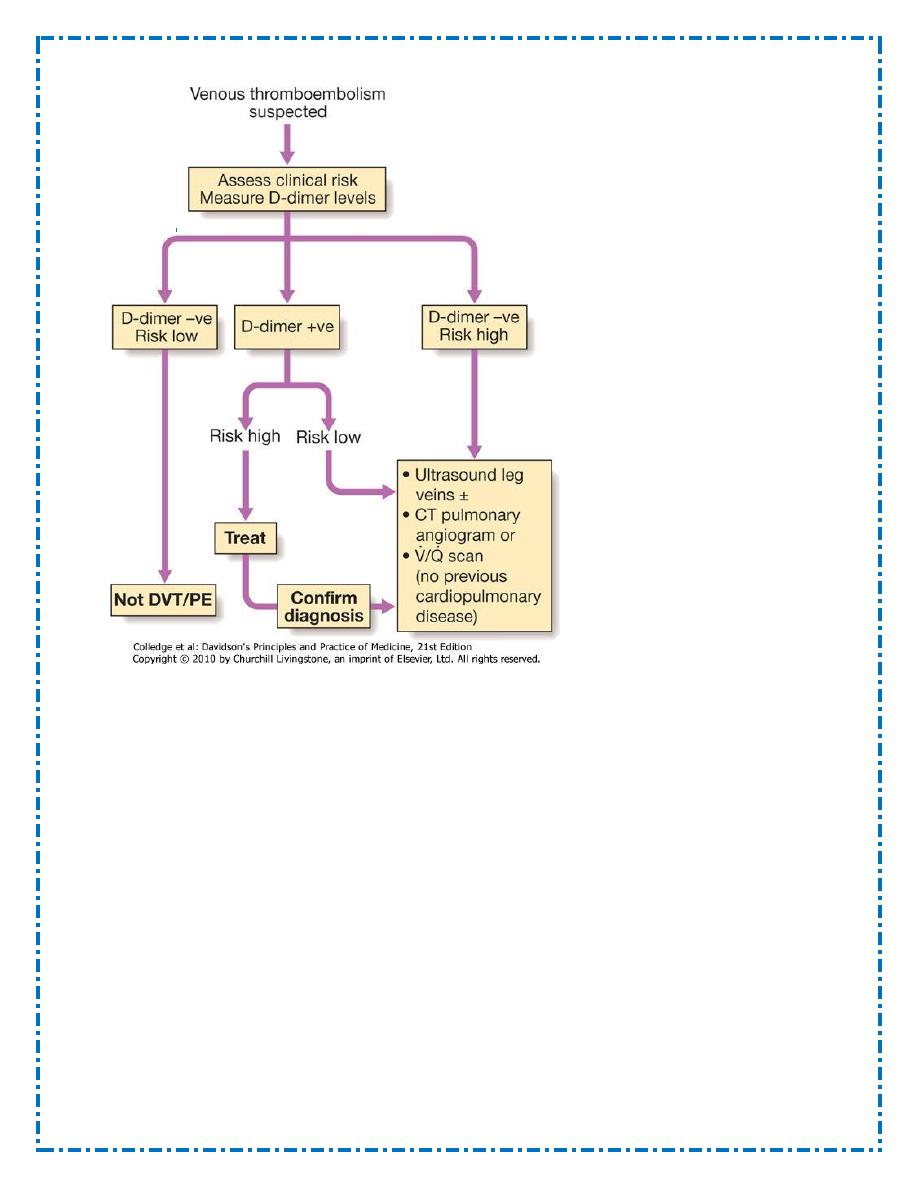
D-dimer:
D-dimer is a specific degradation product released into the circulation when cross-
linked fibrin undergoes endogenous fibrinolysis. An elevated D-dimer is of limited
value, as it occurs in a number of conditions including PE, myocardial infarction,
pneumonia and sepsis. Low D-dimer levels (< 500 ng/mL measured by ELISA),
particularly where clinical risk is low, have a high negative predictive value and
further investigation is unnecessary.The D-dimer result should be disregarded in
high-risk patients, as further investigation is mandatory even if it is normal. Other
circulating markers that reflect right ventricular micro-infarction, such as troponin
I and brain natriuretic peptide, are under investigation.
Imaging A range of imaging techniques can be used to confirm suspected PE. The
choice depends on the clinical probability of VTE, the condition of the patient,
local availability, risks from iodinated contrast medium, radiation exposure and the
associated costs.
7
CT pulmonary angiography (CTPA):is the most commonly sought first-line
diagnostic test.It has the advantage of visualising the distribution and extent of the
emboli, or highlighting alternative diagnoses such as consolidation, pneumothorax
or aortic dissection. The sensitivity of CT may be increased by simultaneous
visualisation of the femoral and popliteal veins. As contrast may be nephrotoxic,
care should be taken in patients with renal impairment and the use of iodinated
contrast media should be avoided in those with a history of allergy to it.
Ventilation-perfusion scanning :is less commonly used, as its utility is limited in
patients with pre-existing chronic cardiopulmonary pathology and the scan is most
frequently regarded as indeterminate.
It is most useful in patients without significant cardiopulmonary disease and a
normal chest X-ray; interpretation should be informed by clinical probability.
Colour Doppler Ultrasound :Colour Doppler ultrasound of the leg veins remains
the investigation of choice in patients with suspected DVT, but may also be
applied to patients in whom PE is suspected, particularly if there are clinical signs
in a limb, as many will have identifiable proximal thrombus in the leg veins.
8
Echocardiography:Echocardiography is extremely helpful in the differential
diagnosis.Acute dilatation of the right heart is usually present in massive PE, and
thrombus may be visible.
Alternative diagnoses, including left ventricular failure, aortic dissection and
pericardial tamponade, can also be established.
Pulmonary angiography:Conventional pulmonary angiography has been largely
superseded by CTPA but may still be used in selected settings
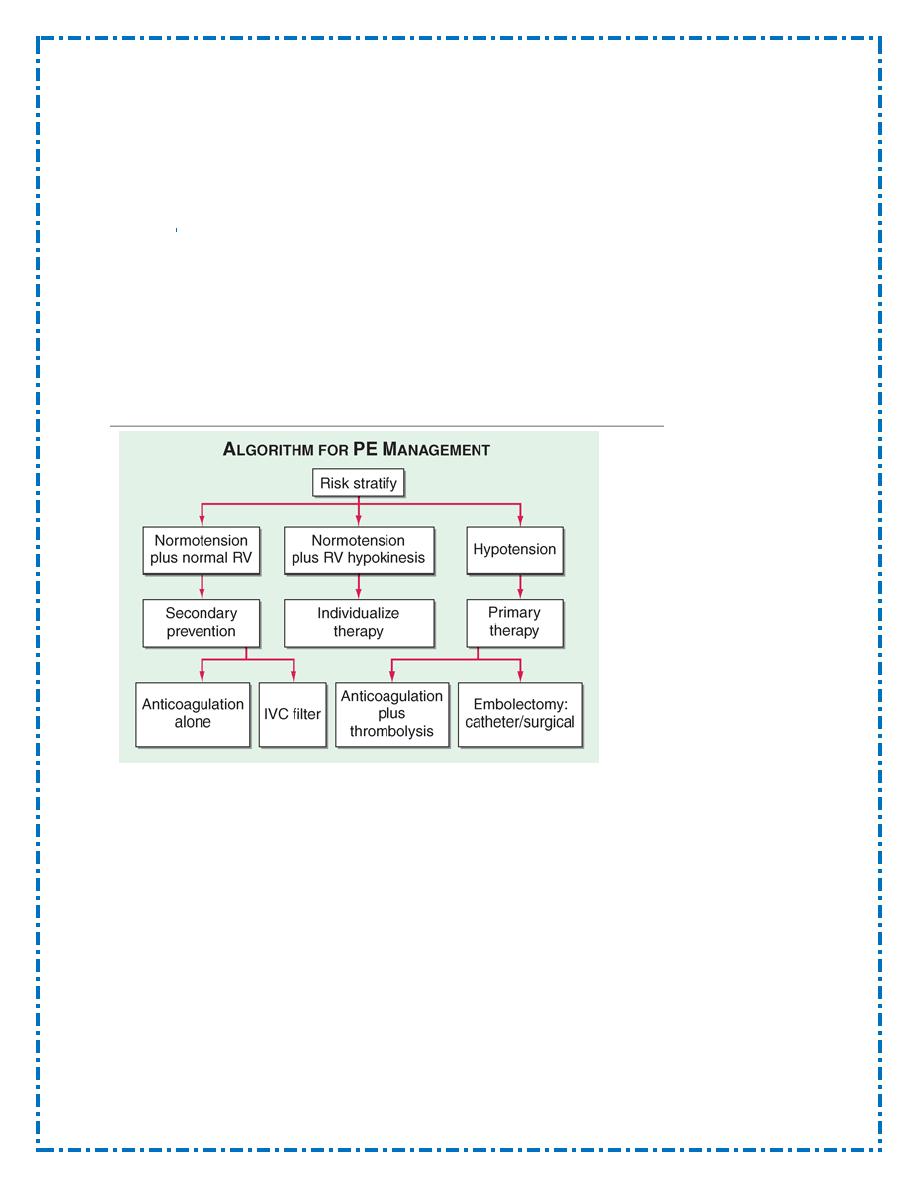
Risk Stratification
1. The presence of hemodynamic instability
2. RV dysfunction
3. elevation of the troponin level due to RV microinfarction can identify high-
risk patients
4. RV hypokinesis on echocardiography
5. RV enlargement on chest CT
Management
General measures
Oxygen should be given to all hypoxaemic patients in a concentration necessary to
restore arterial oxygen saturation to over 90%. Opiates may be necessary to relieve
pain and distress but should be used with great caution in the hypotensive patient
Diuretics and vasodilators should also be avoided
hypotension should be treated by giving intravenous fluid
: cautiously because
right ventricular function is often markedly compromised.
9
Anticoagulation
Although anticoagulants do not dissolve existing clots in DVT or PE directly, they
limit further thrombus formation and allow fibrinolysis to occur. Immediately
effective anticoagulation is initiated with a parenteral drug: unfractionated heparin
(UFH), low-molecular-weight heparin (LMWH), or fondaparinux.
Warfarin requires 5–7 days to achieve a therapeutic effect. During that period, one
should overlap the parenteral and oral agents.Warfarin Anticoagulation Usual start
dose is 5 mg.Titrate to INR, target 2.0–3.0The duration of anticoagulation for an
initial DVT or PE is at least 3–6 months. Recurrent DVT or PE typically requires
lifelong anticoagulation.
Thrombolytic therapy
Thrombolysis is indicated in any patient presenting with acute massive PE
accompanied by cardiogenic shock. In the absence of shock, the benefits are less
clear but it may be considered in patients presenting with right ventricular
dilatation and hypokinesis or severe hypoxaemia.
The most complication associated with thrombolytics is intracranial hemorrhage,
which occurs in approximately 1 to 3% of patients. Pulmonary embolectomy is
appropriate in patients who have massive embolism with hypotension and cannot
receive thrombolytic therapy. Surgical pulmonary embolectomy may be considered
in selected patients but carries a high mortality risk.
Caval filters
1. recurrent PE despite adequate anticoagulation
2. anticoagulation is contraindicated
When
chronic
thromboembolic
pulmonary
hypertension is
diagnosed,
anticoagulation should be instituted and an inferior vena cava filter placed.
Pulmonary
thromboendarterectomy
through
median
sternotomy
on
cardiopulmonary bypass should be considered in selected cases .Treatment of
nonoperable chronic thromboembolic pulmonary hypertension with medications
such as the oral endothelin antagonist bosentan In more severely ill patients,
epoprostenol .Lung transplantation can be considered in selected patients with
severe pulmonary hypertension in whom thrombi are too distal to be extracted
prevention
most effective treatment of thromboembolic disease is prevention. In patients at
high risk for DVT or PE (e.g., patients in the intensive care unit, patients
undergoing major surgery, patients with recent onset of paralysis).prophylactic
therapy with subcutaneous unfractionated heparin (5000 U every 12 hours) or
LMWHs significantly reduces the risk. Prophylaxis is generally recommended for
7 to 10 days. In patients with contraindications to this therapy the use of
pneumatic compression boots is an acceptable alternative
Management of pregnancy:Heparin does not cross the placenta ,and does not cause
these fetal complications.
10
Fat Embolism
Treatment :supportive, including oxygen and mechanical ventilation
Amniotic Fluid Embolism
Although administration of heparin, antifibrinolytic agents such as ε-aminocaproic
acid, and cryoprecipitate has been suggested, the primary treatment is supportive,
with oxygen, mechanical ventilation, and any necessary hemodynamic support.
Air Embolism
Trendelenburg–left lateral decubitus position , administration of 100% oxygen. If
a central venous catheter is in place near the right atrium, air aspiration should be
attempted .Anticonvulsants are administered in the presence of seizures
Diaa
