BY.Fatima Ehsan Avci
|
P a g e
1
FUNCTIONAL ANATOMY AND PHYSIOLOGY
_ The lungs occupy the upper two-thirds of the bony thorax, bounded
medially by the spine, the heart and the mediastinum and inferiorly by
the diaphragm. During breathing, free movement of the lung surface
relative to the chest wall is facilitated by sliding contact between the
parietal and visceral pleura, which cover the inner surface of the chest
wall and the lung respectively, and are normally in close apposition.
_
Inspiration
involves downward contraction of the dome-shaped
diaphragm (innervated by the phrenic nerves originating from C3, 4
and 5) and upward, outward movement of the ribs on the
costovertebral joints, caused by contraction of the external intercostal
muscles (innervated by the corresponding intercostal nerves
originating from the thoracic spinal cord).
_
Expiration
is largely passive, driven by elastic recoil of the lungs.
_The conducting airways from the nose to the alveoli connect the external environment
with the extensive, thin and vulnerable alveolar surface. As air is inhaled through the
upper airways, it is filtered in the nose, heated to body temperature and fully saturated
with water vapour; partial recovery of this heat and moisture occurs on expiration.
Total airway cross-section is smallest in the glottis and trachea, which means that
airflow is rapid here and the airway is particularly vulnerable to obstruction by foreign
bodies and tumours. Normal breath sounds originate mainly from the rapid turbulent
airflow in the larynx and in these central airways
BY.Fatima Ehsan Avci
|
P a g e
2
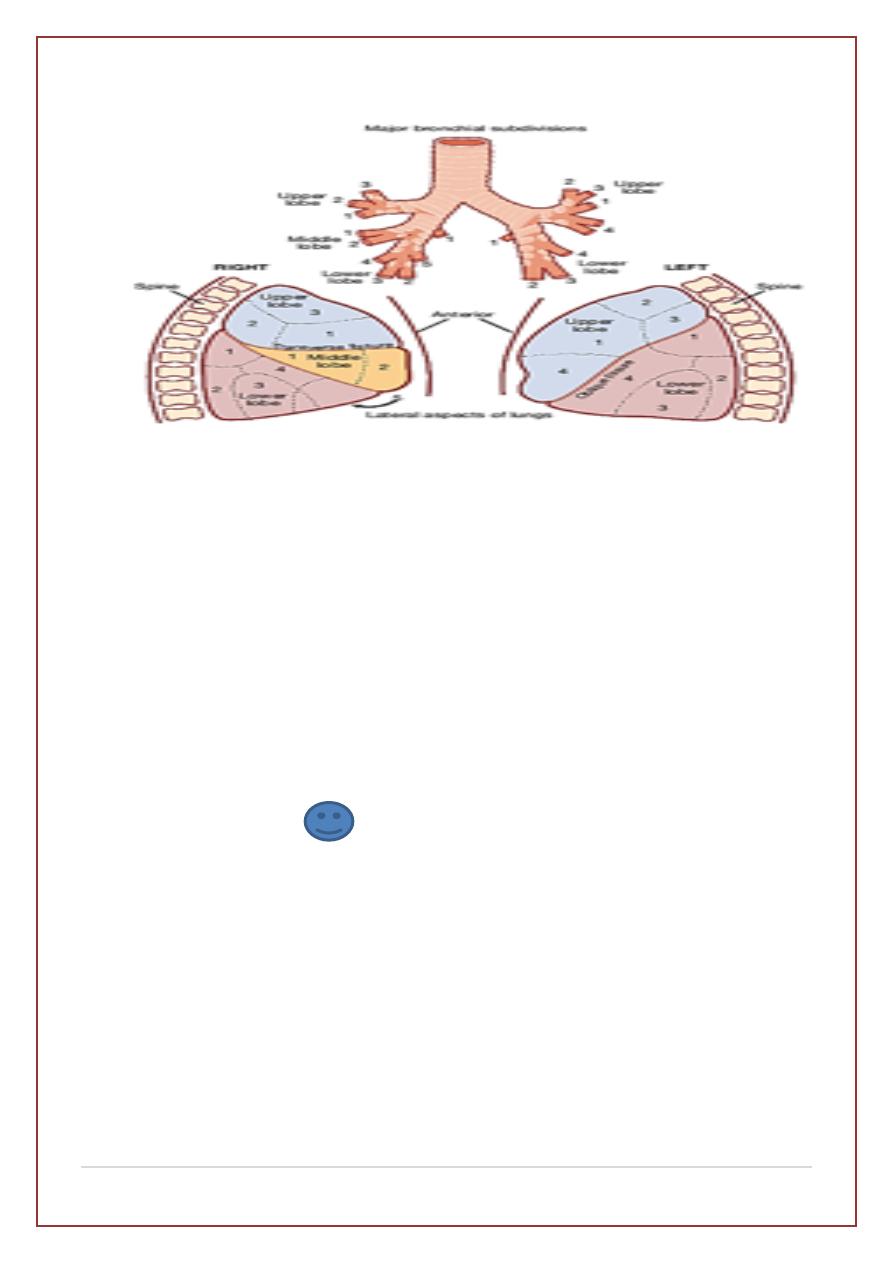
The acinus
is the gas exchange unit of the lung (Fig. 19.2) and
comprises branching respiratory bronchioles and clusters of alveoli.
The filtered, moistened and heated air makes close contact here with
the blood in the pulmonary capillaries (gas-to-blood distance < 0.4 µm),
and oxygen uptake and CO2 excretion occur. The alveoli are lined
with flattened epithelial cells (type I pneumocytes) and a few, more
cuboidal, type II pneumocytes. The latter produce surfactant, which is
a mixture of phospholipids that reduces surface tension and
counteracts the tendency of alveoli to collapse. Type II pneumocytes
can also divide to reconstitute type I pneumocytes after lung injury
Control of breathing
1-Central chemoreceptors in the ventrolateral medulla sense the pH of the
cerebrospinal fluid (CSF) and are indirectly stimulated by a rise in arterial
PCO2.
2-The carotid bodies sense hypoxaemia but are mainly activated by arterial
PO2 values below 8 KPa (60 mmHg).
3- Muscle spindles in the respiratory muscles sense changes in mechanical
load.
BY.Fatima Ehsan Avci
|
P a g e
3
4-Vagal sensory fibres from the lung may be stimulated by stretch or by
various disease processes in the interstitium.
5-Cortical influences can override the automatic
The pulmonary circulation
The pulmonary circulation in health operates at low pressure
(approximately 24/9 mmHg), and can accommodate large increases in flow
without much rise in pressure, e.g. during exercise. Pulmonary
hypertension occurs when pulmonary vessels are destroyed by emphysema,
obstructed by thrombus or involved in interstitial inflammation or fibrosis.
The right ventricle responds by hypertrophy, with right axis deviation and P
pulmonale on the ECG. Pulmonary hypertension with hypoxia and
hypercapnia is associated with generalised salt and water retention (‘cor
pulmonale’), with elevation of the jugular venous pressure (JVP) and
peripheral oedema. This is thought to result mainly from a failure of the
hypoxic and hypercapnic kidney to excrete sufficient salt and water.
Lung defences
Upper airway defences
Large airborne particles are trapped by nasal hairs, and smaller particles
settling on the mucosa are cleared towards the oropharynx by the columnar
ciliated epithelium which covers the turbinates and septum (Fig. 19.3).
During cough, expiratory muscle effort against a closed glottis results in
high intrathoracic pressure, which is then released explosively. The flexible
posterior tracheal wall is pushed inwards by the high surrounding pressure,
reducing tracheal cross-section and maximizingthe airspeed to achieve
effective expectoration. The larynx also acts as a sphincter protecting the
airway during swallowing and vomiting.
BY.Fatima Ehsan Avci
|
P a g e
4
Lower airway defences
The innate response
in the lungs is characterised by a number of non-
specific defence mechanisms. Inhaled particulate matter is trapped in
airway mucus and cleared by the mucociliary escalator. Cigarette smoke
increases mucus secretion but reduces mucociliary clearance and
predisposes towards lower respiratory tract infections, including
pneumonia. Defective muco-ciliary transport is also a feature of several
rare diseases, including Kartagener’s syndrome, Young’s syndrome and
ciliary dysmotility syndrome, which are charac-terised by repeated sino-
pulmonary infections and bronchiectasis.
Airway secretions contain an array of antimicrobial peptides (such as
defensins, immunoglobulin A (IgA) and lysozyme), antiproteinases and
antioxidants. Many of these assist with the opsonisation and killing of
bacteria, and the regulation of the powerful proteolytic enzymes secreted by
inflammatory cells. In particular, α1-antiproteinase (A1Pi) regulates
neutrophil elastase, and deficiency of this may be associated with
premature emphysema
Macrophages engulf microbes, organic dusts and other particulate matter.
They are unable to digest inorganic agents such as asbestos or silica, which
result in their death and the release of powerful proteolytic enzymes that
cause parenchymal damage. Neutrophil numbers in the airway are low, but
the pulmonary circulation contains a marginated pool that may be recruited
rapidly in response to bacterial infection. This may explain the prominence
of lung injury in sepsis syndromes and trauma.
Adaptive immunity
is characterised by the specificity of the response and
the development of memory. Lung dendritic cells facilitate antigen
presentation to T- and B-lymphocytes..
