1 |
P a g e
PRESENTING PROBLEMS IN RESPIRATORY DISEASE:
Cough
:
Cough is the most frequent symptom of respiratory disease. It is caused by
stimulation of sensory nerves in the mucosa of the pharynx, larynx, trachea and
bronchi .
Acute sensitization of the normal cough reflex occurs in a number of
conditions, and it is typically induced by changes in air temperature or
exposure to irritants such as cigarette smoke or perfumes .
The explosive quality of a normal cough is lost in patients with respiratory
muscle paralysis or vocal cord palsy.
Paralysis of a single vocal cord gives rise to a prolonged, low-pitched,
inefficient 'bovine' cough accompanied by hoarseness .
Coexistence of an inspiratory noise (stridor) indicates partial obstruction of
a major airway (e.g. laryngeal oedema, tracheal tumor, scarring,
compression or inhaled foreign body) and requires urgent investigation
and treatment.
Sputum production is common in patients with acute or chronic cough,
and its nature and appearance can provide clues to the etiology
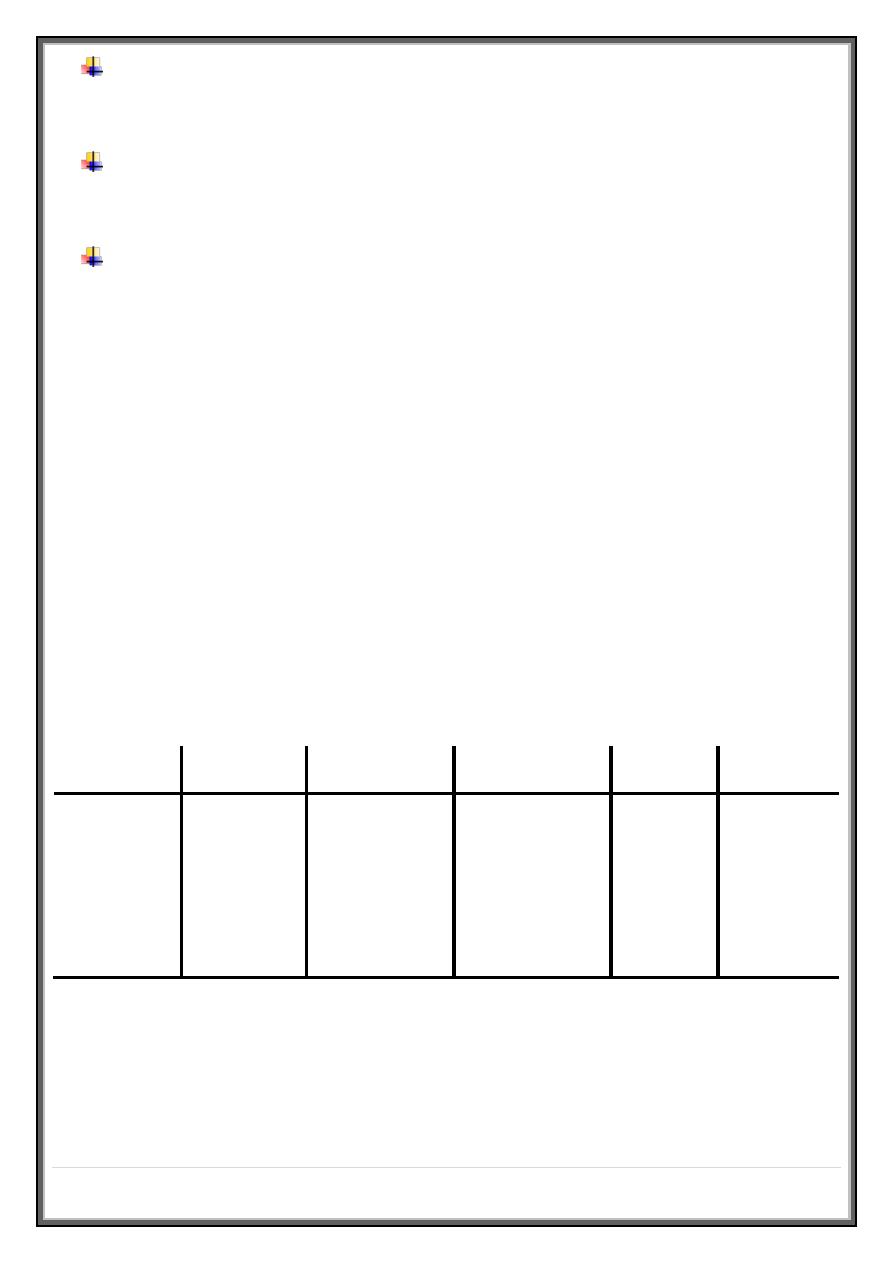
Causes of cough
Acute transient cough is most commonly caused by viral lower respiratory tract
infection, post-nasal drip resulting from rhinitis or sinusitis, aspiration of a
foreign body or throat-clearing secondary to laryngitis or pharyngitis.
When it occurs in the context of more serious diseases such as pneumonia,
aspiration, congestive heart failure or pulmonary embolism, it is usually easy to
diagnose from other clinical features .
2 |
P a g e
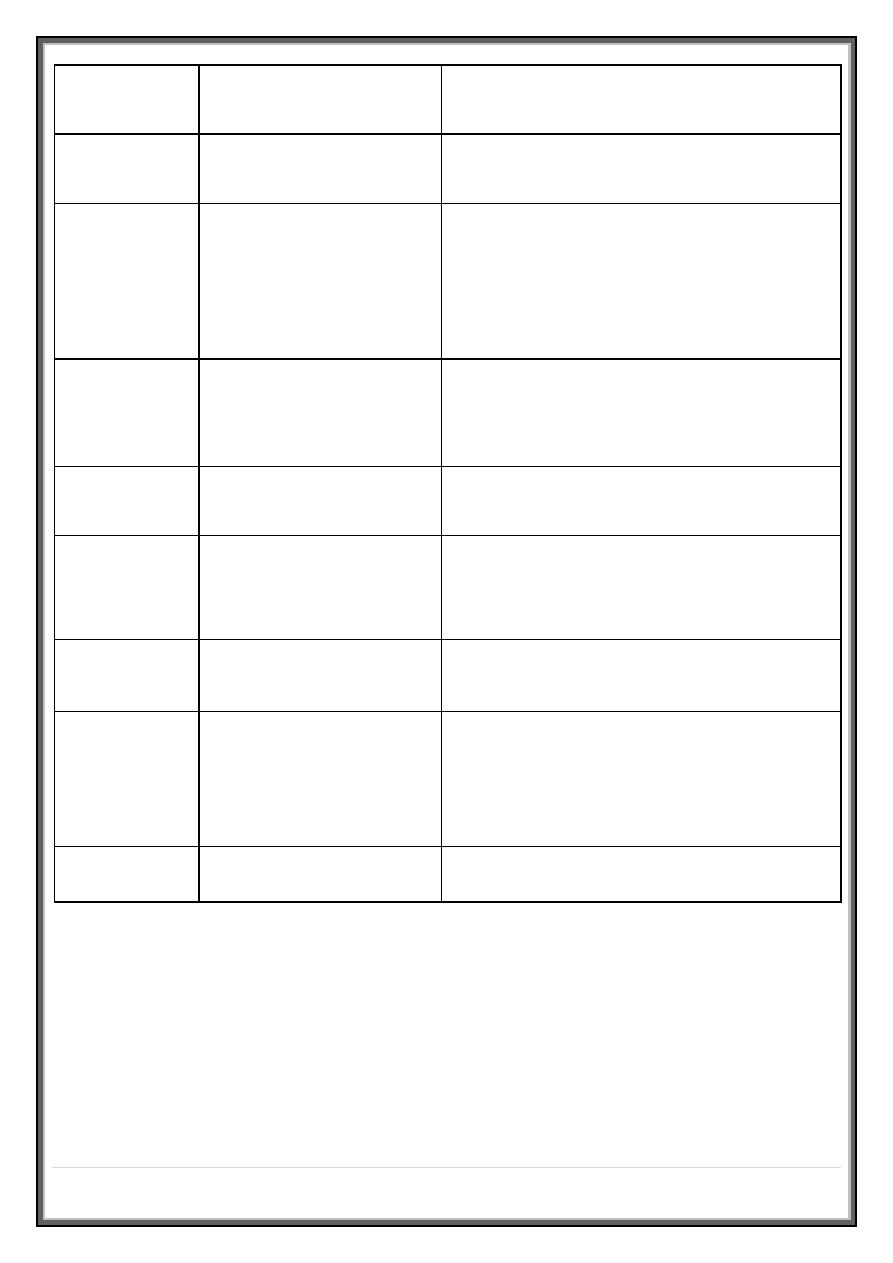
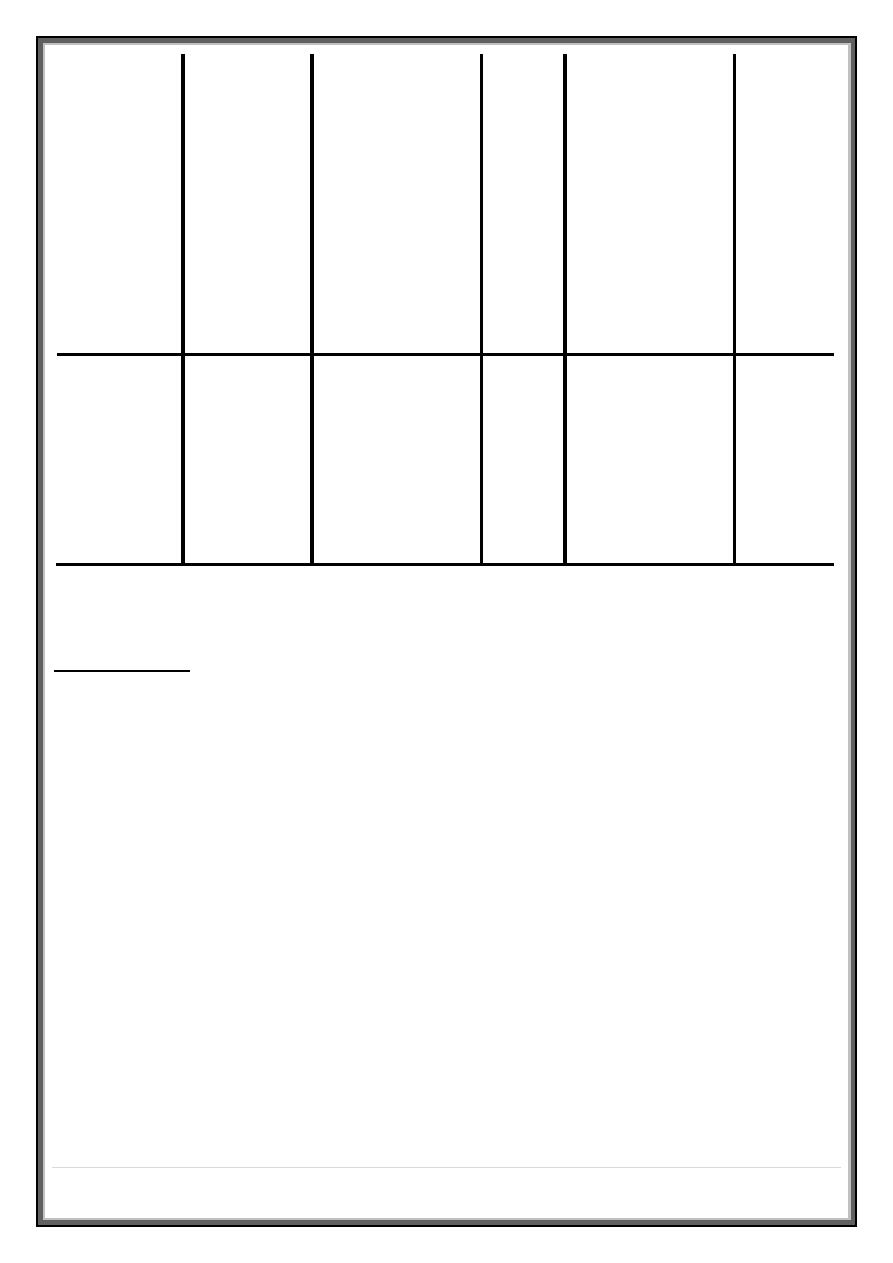
Origin
Common causes
Clinical features
Pharynx
Post-nasal drip
History of chronic rhinitis
Larynx
Laryngitis, tumor,
whooping cough, croup
Voice or swallowing altered, harsh or
painful cough
Paroxysms of cough, often associated
with stridor
Trachea
Tracheitis
Raw retrosternal pain with cough
Bronchi
Bronchitis (acute) and
COPD
Dry or productive, worse in mornings
Asthma
Usually dry, worse at night
Eosinophilic bronchitis Features similar to asthma but no
airway hyper-reactivity (AHR)
Bronchial carcinoma
Persistent (often with hemoptysis)
3 |
P a g e
Lung
parenchyma
Tuberculosis
Productive, often with hemoptysis
Pneumonia
Dry initially, productive later
Bronchiectasis
Productive, changes in posture induce sputum
production
Pulmonary
oedema
Often at night (may be productive of pink,
frothy sputum)
Interstitial
fibrosis
Dry, irritant and distressing
Drug side-
effect
ACE inhibitors
Dry cough
Patients with chronic cough present more of a diagnostic challenge, especially
when physical examination, chest X-ray and lung function studies are normal.
In this context, it is most often explained by cough-variant asthma (where
cough may be the principal or exclusive clinical manifestation), post-nasal drip
secondary to nasal or sinus disease, or gastro-oesophageal reflux with
aspiration.
4 |
P a g e
Diagnosis of the latter may require ambulatory pH monitoring or a prolonged
trial of anti-reflux therapy .
Between 10 and 15% of patients (particularly women) taking angiotensin-
converting enzyme (ACE) inhibitors develop a drug-induced chronic cough .
Bordetella pertussis infection in adults can also result in protracted cough and
should be suspected in those in close contact with children.
While most patients with a bronchogenic carcinoma have an abnormal chest X-
ray on presentation, fibreoptic bronchoscopy or thoracic CT is advisable in most
adults (especially smokers)
In a small percentage of patients, dry cough may be the presenting feature of
interstitial lung disease .
Breathlessness
:
Breathlessness or dyspnea can be defined as the feeling of an uncomfortable
need to breathe.
It is unusual among sensations in having no defined receptors, no localised
representation in the brain, and multiple causes both in health (e.g. exercise)
and in diseases of the lungs, heart or muscles .
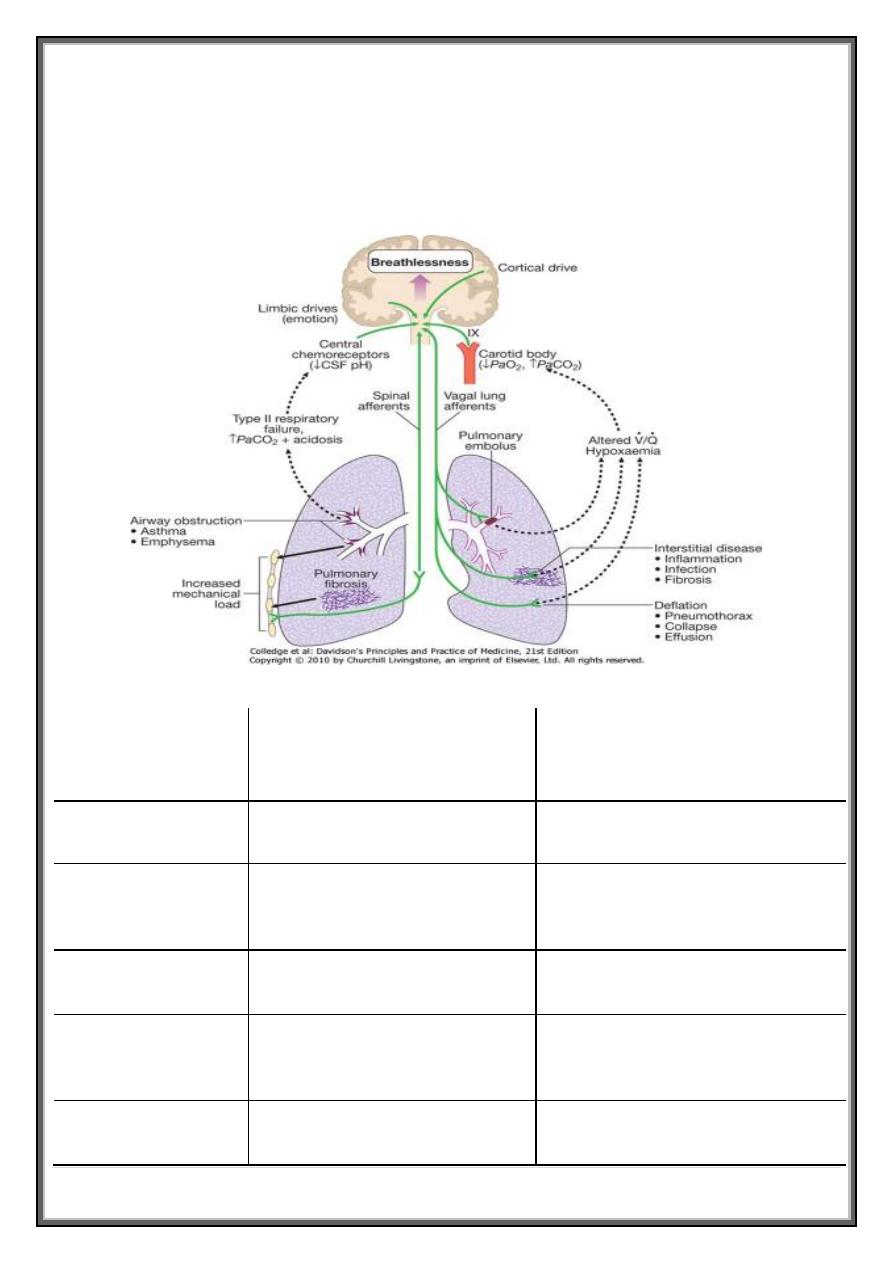
Pathophysiology
Respiratory diseases can stimulate breathing and dyspnoea by :
1. stimulating intrapulmonary sensory nerves (e.g. pneumothorax, interstitial
inflammation and pulmonary embolus)
2. increasing the mechanical load on the respiratory muscles (e.g. airflow
obstruction or pulmonary fibrosis)
3. Causing hypoxia, hypercapnia or acidosis, stimulating chemoreceptors .
5 |
P a g e
4. In cardiac failure, pulmonary congestion reduces lung compliance and can
also obstruct the small airways .
5. In addition, during exercise, reduced cardiac output limits oxygen supply
to the skeletal muscles, causing early lactic academia and further
stimulating breathing via the central chemoreceptors .
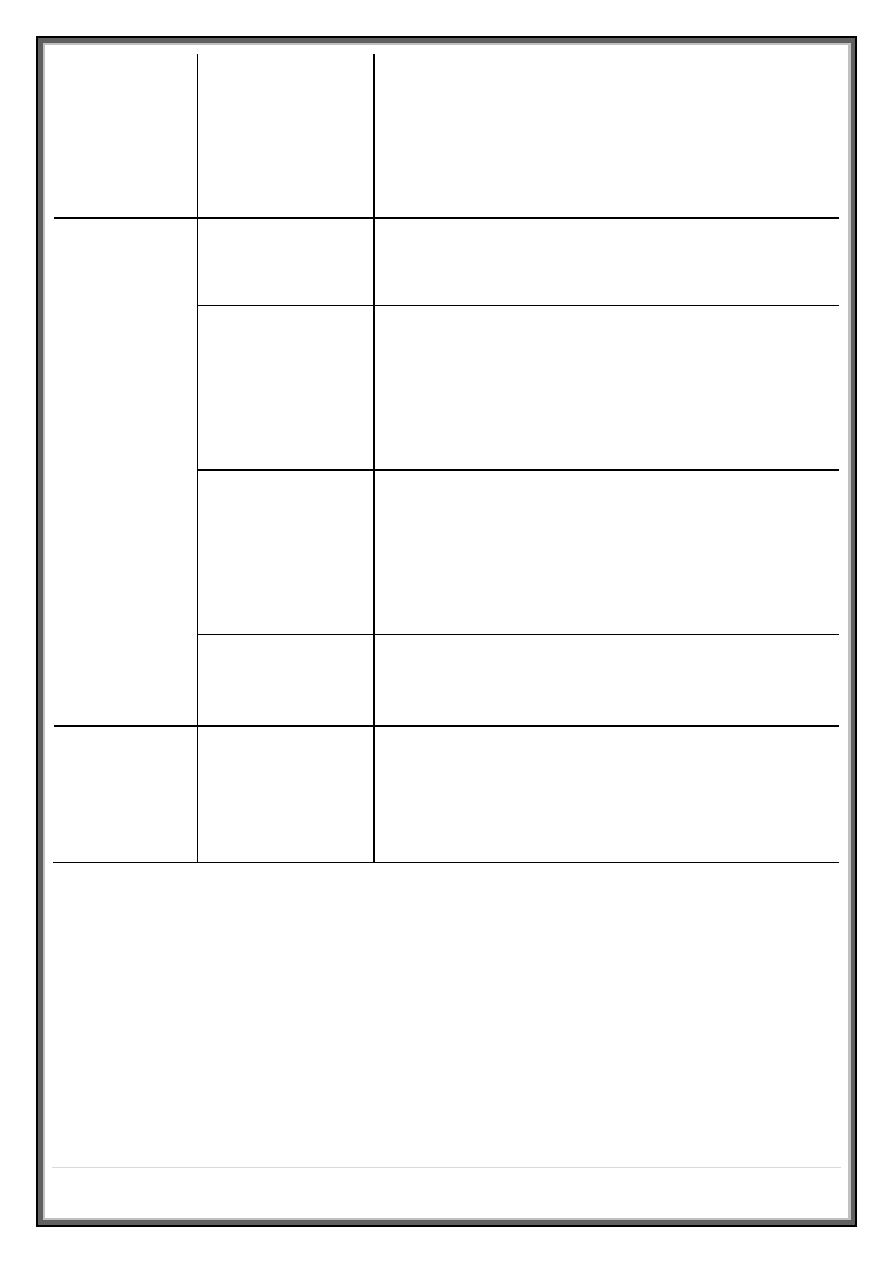
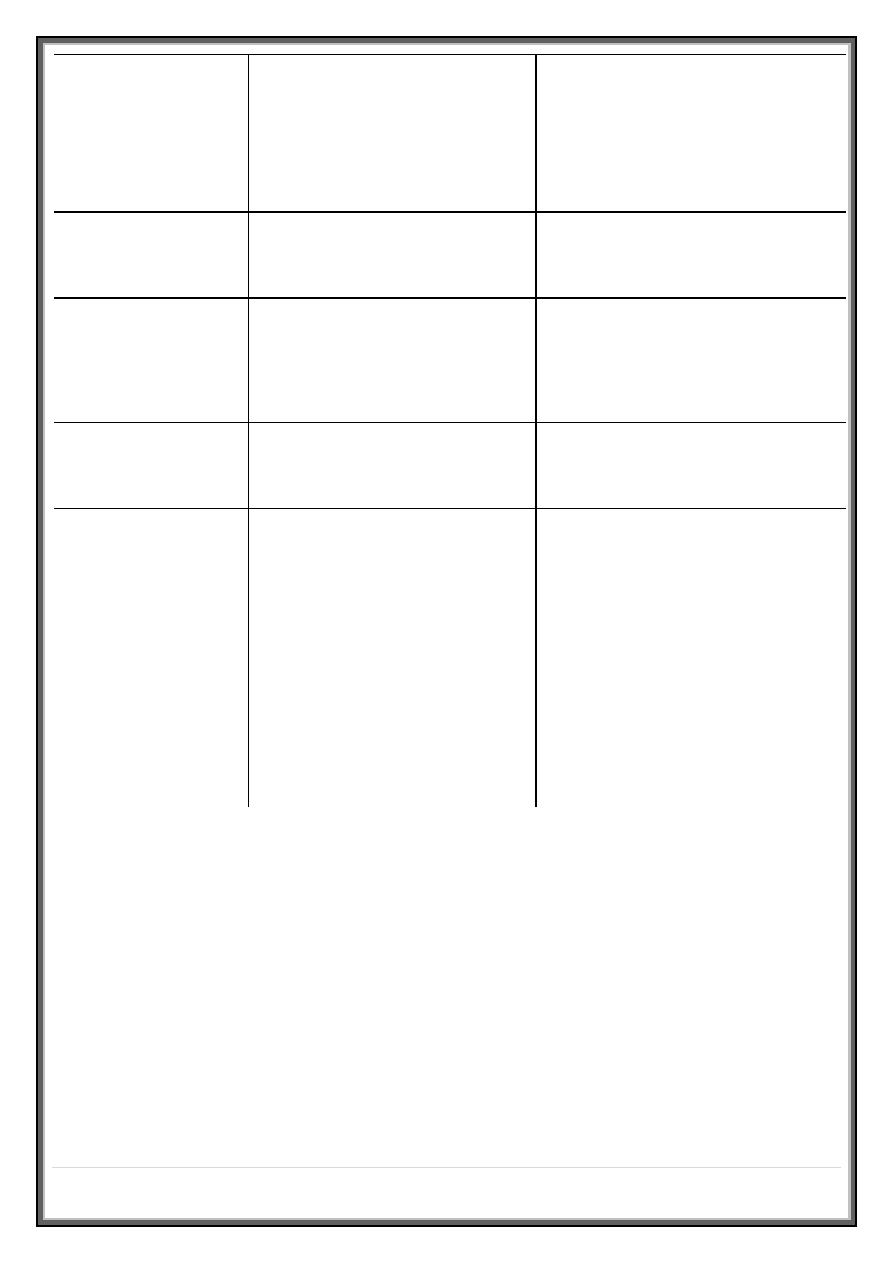
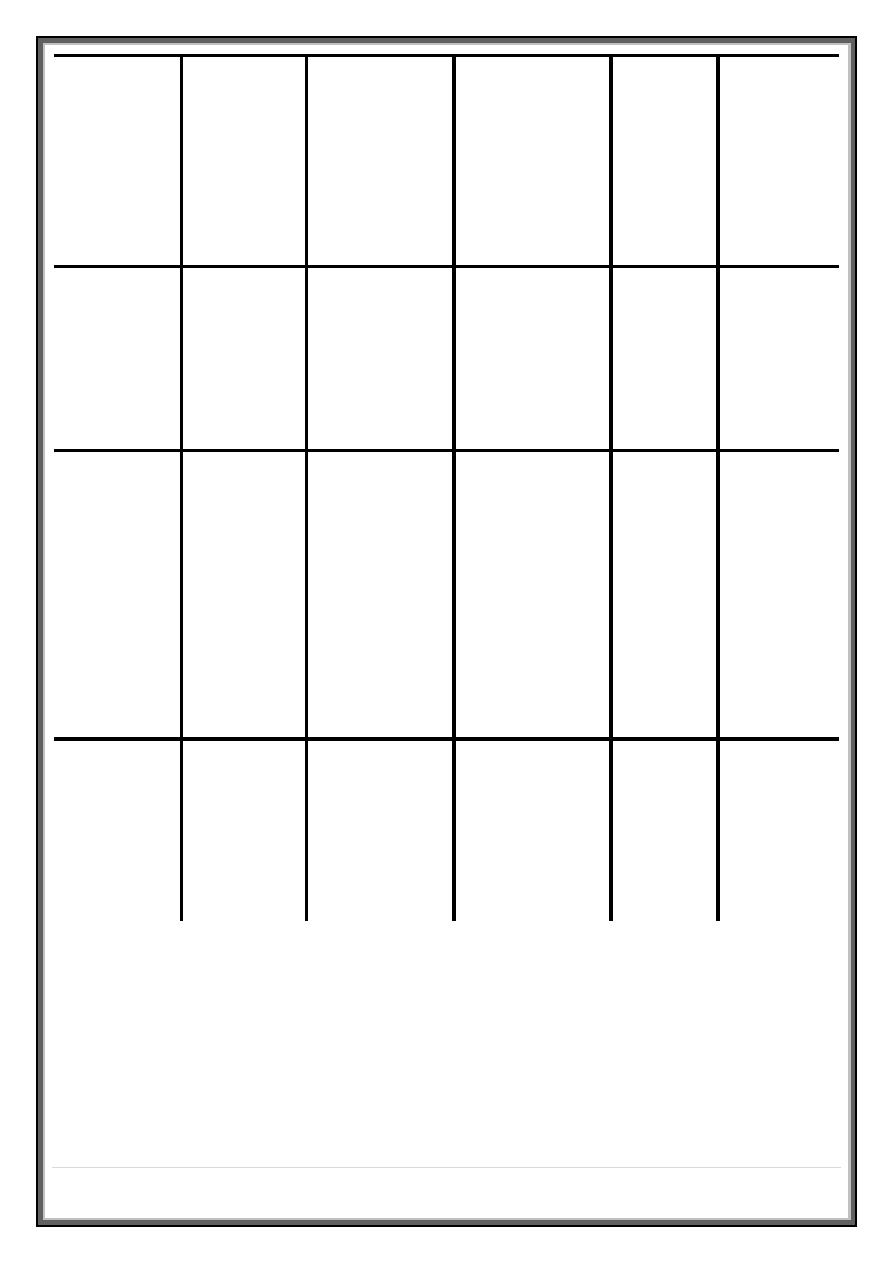
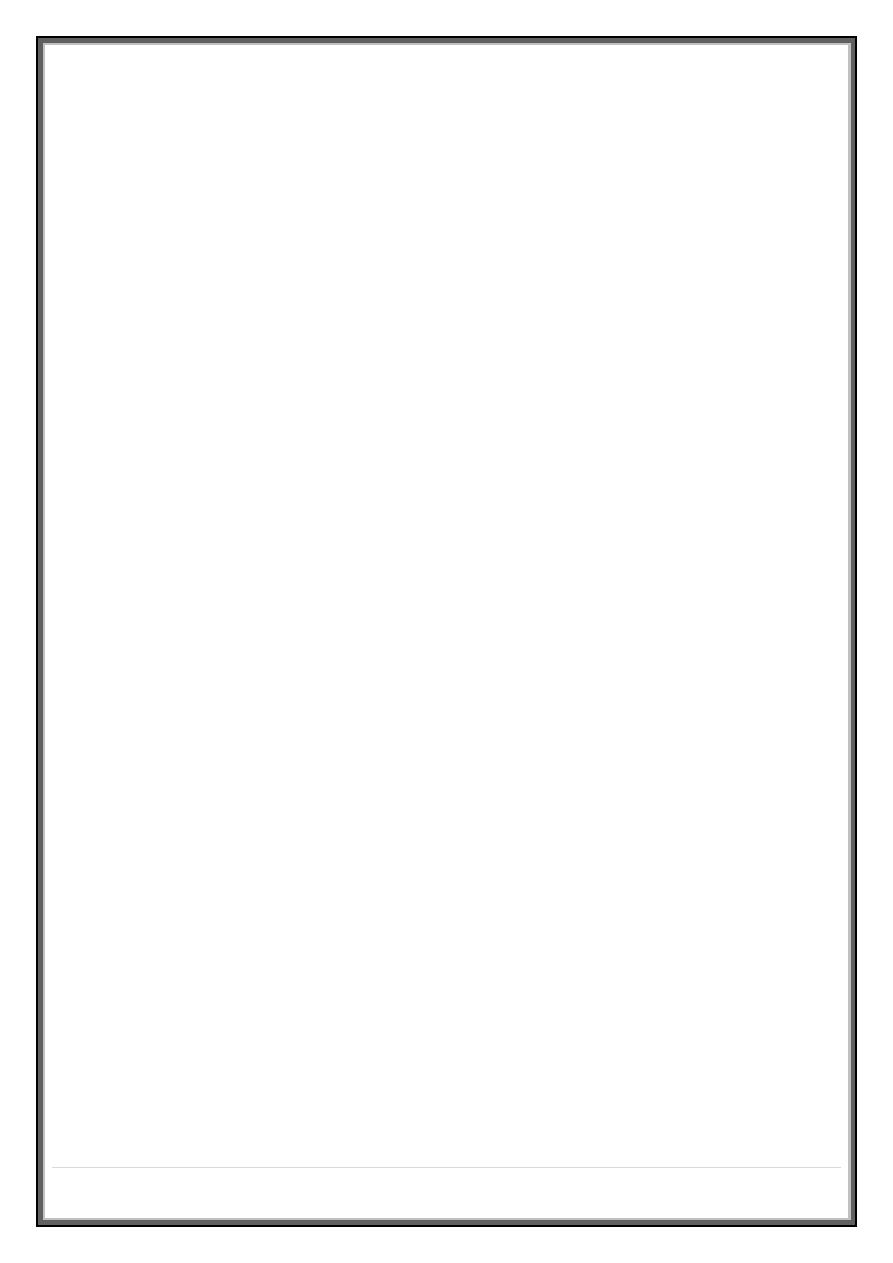
System
Acute dyspnea
Chronic exertional
dyspnea
Cardiovascular
*Acute pulmonary edema Chronic heart failure
Myocardial ischemia
(angina equivalent)
Respiratory
*Acute severe asthma
*COPD
*Acute exacerbation of
COPD
*Chronic asthma
*Pneumothorax
Bronchial carcinoma
6 |
P a g e
*Pneumonia
*Pulmonary embolus
Interstitial lung disease
(sarcoidosis, fibrosing
alveolitis, extrinsic allergic
alveolitis, pneumoconiosis)
Acute respiratory distress
syndrome (ARDS)
Chronic pulmonary
thromboembolism
Inhaled foreign body
(especially in the child)
Lobar collapse
Lymphatic carcinomatosis
(may cause intolerable
breathlessness)
Laryngeal oedema (e.g.
anaphylaxis)
Large pleural effusion(s)
Others
Metabolic acidosis (e.g.
diabetic ketoacidosis,
lactic acidosis, uremia,
overdose of salicylates,
ethylene glycol
poisoning) Psychogenic
hyperventilation (anxiety
or panic-related)
Severe anemia
Obesity
Deconditioning
Chronic exertional breathlessness
The cause of breathlessness is often apparent from a careful clinical
history. Key questions include :
How is your breathing at rest and overnight ?
7 |
P a g e
In COPD, there is a fixed, structural limit to maximum ventilation, and a
tendency for progressive hyperinflation during exercise .
Breathlessness is mainly apparent during mobilization, and patients
usually report minimal symptoms at rest and overnight.
In contrast, patients with significant asthma are often woken from their sleep
by breathlessness with chest tightness and wheeze .
Orthopnea
, however, is common in COPD as well as in heart disease, because
airflow obstruction is made worse by cranial displacement of the diaphragm by
the abdominal contents when recumbent, so many patients choose to sleep
propped up .
It may thus not be a useful differentiating symptom, unless there is a clear
history of previous angina or infarction to suggest cardiac disease .
Variability within and between days is a hallmark of asthma; in mild asthma the
patient may be free of symptoms and signs when well .
Gradual, progressive loss of exercise capacity over months and years with
consistent disability over days is typical of COPD .
When asthma is suspected, the degree of variability is best documented by
home peak flow monitoring .
Relentless, progressive breathlessness that is also present at rest, often
accompanied by a dry cough, suggests interstitial fibrosis .
8 |
P a g e
Impaired left ventricular function can also cause chronic exertional
breathlessness, cough and wheeze. A history of angina, hypertension or
myocardial infarction may be useful in implicating a cardiac cause.
The suspicion of cardiac impairment may be confirmed by a displaced apex
beat, a raised JVP and cardiac murmurs (although these signs can occur in
severe cor pulmonale) .
The chest X-ray may show cardiomegaly and an electrocardiogram (ECG) and
echocardiogram may provide evidence of left ventricular disease.
Measurement of arterial blood gases may be of value, since in the absence of
an intracardiac shunt or pulmonary oedema the PaO2 in cardiac disease is
normal and the PaCO2 is low or normal .
Did you have breathing problems in childhood or at school ?
When present, a history of childhood wheeze increases the likelihood of
asthma, although this history may be absent in late-onset asthma .
Similarly, a history of atopic allergy increases the likelihood of asthma .
Do you have other symptoms along with your breathlessness ?
Digital or perioral paresthesia and a feeling that 'I cannot get a deep enough
breath in' are typical features of psychogenic hyperventilation, but this cannot
be diagnosed until investigations have excluded other potential causes of
breathlessness.
Additional symptoms include lightheadedness, central chest discomfort or
even carpopedal spasm due to acute respiratory alkalosis .
These alarming symptoms may provoke further anxiety and exacerbate
hyperventilation .
9 |
P a g e
Psychogenic breathlessness rarely disturbs sleep, frequently occurs at
rest, may be provoked by stressful situations and may even be relieved by
exercise .
The Nijmegen questionnaire can be used to enumerate some of the typical
symptoms of hyperventilation. Arterial blood gases show normal PO2, low PCO2
and alkalosis .
Pleuritic chest pain in a patient with chronic breathlessness, particularly if it
occurs in more than one site over time, should raise suspicion of
thromboembolic disease .
Thromboembolism may occasionally present as chronic breathlessness with no
other specific features, and should always be considered before a diagnosis of
psychogenic hyperventilation is made.
Factors suggesting psychogenic hyperventilation
'Inability to take a deep breath '
Frequent sighing/erratic ventilation at rest
Short breath-holding time in the absence of severe respiratory disease
Difficulty in performing/inconsistent spirometry man [oelig ]uvres
High score (over 26) on Nijmegen questionnaire
Induction of symptoms during submaximal hyperventilation
Resting end-tidal CO2 < 4.5%
Associated digital paresthesia
Morning headache is an important symptom in patients with breathlessness, as
it may signal the onset of carbon dioxide retention and respiratory failure .
10 |
P a g e
This is particularly significant in patients with musculoskeletal disease impairing
respiratory function (e.g. kyphoscoliosis or muscular dystrophy) .
Acute severe breathlessness
This is one of the most common and dramatic medical emergencies .
Although there are a number of possible causes, the history and a rapid but
careful examination will usually suggest a diagnosis which can be confirmed by
routine investigations, including chest X-ray, ECG and arterial blood gases .
History
It is important to establish the rate of onset and severity of the breathlessness
and whether associated cardiovascular symptoms (chest pain, palpitations,
sweating and nausea) or respiratory symptoms (cough, wheeze, hemoptysis,
stridor) are present.
A previous history of repeated episodes of left ventricular failure, asthma or
exacerbations of COPD is valuable .
In the severely ill patient it may be necessary to obtain the history from
accompanying relatives or careers .
In children, the possibility of inhalation of a foreign body or acute epiglottitis
should always be considered .
Pulmonary oedema is suggested by pink frothy sputum and bi-basal
crackles, asthma or COPD by wheeze and prolonged expiration ,
Pneumothorax by a silent resonant hemi thorax, and pulmonary embolus
by severe breathlessness with normal breath sounds .
11 |
P a g e
The peak expiratory flow should be measured whenever possible. Leg
swelling may suggest cardiac failure or, if asymmetrical, venous
thrombosis .
Arterial blood gases, chest X-ray and an ECG should be obtained to confirm
the clinical diagnosis, and high concentrations of oxygen given pending
results.
Urgent endotracheal intubation may become necessary if the conscious
level declines or if severe respiratory acidosis is present .
Clinical assessment
The following should be assessed and documented immediately :
1. Level of consciousness
2. Degree of central cyanosis
3. Evidence of anaphylaxis (urticaria or angioedema)
4. Patency of the upper airway
5. Ability to speak (in single words or sentences)
6. Cardiovascular status (heart rate and rhythm, blood pressure and degree
of peripheral perfusion) .
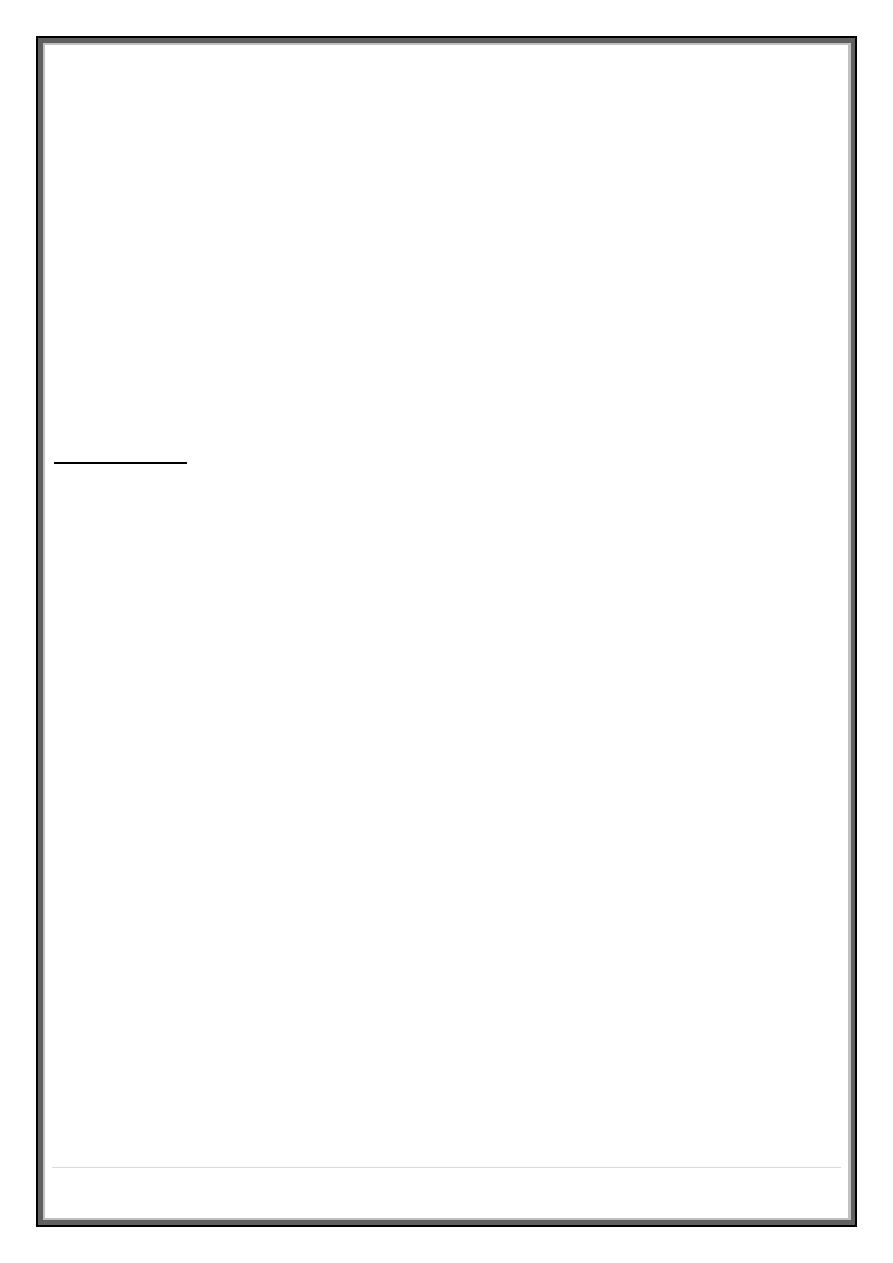
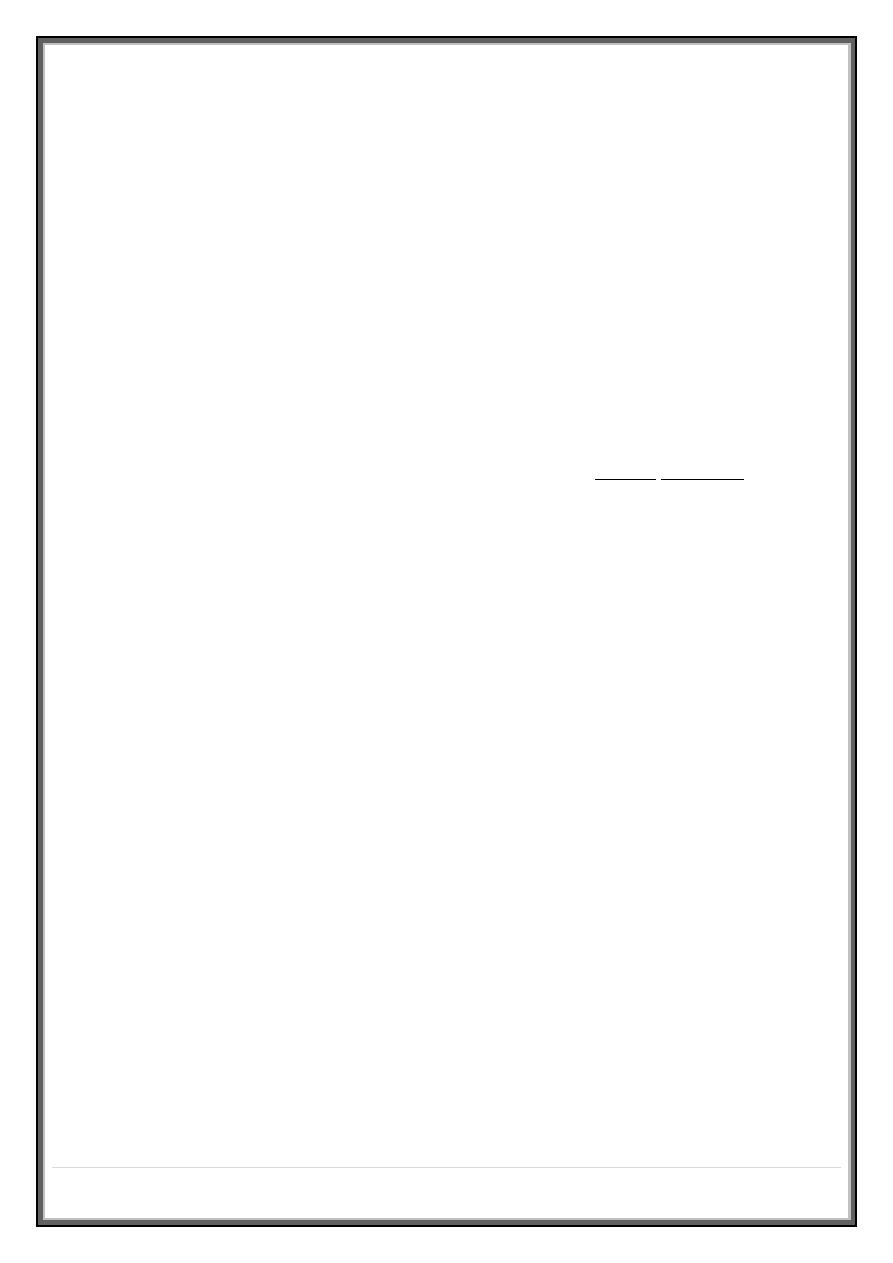
Condition
History
Signs
CXR
ABG
ECG
Pulmonary
oedema
Chest pain,
palpitations,
orthopnea,
cardiac
history*
Central
cyanosis, ↑JVP,
sweating, cool
extremities,
basal
crepitation's*
Cardiomegaly,
oedema/pleural
effusions*
↓PaO
2
↓PaCO
2
Sinus
tachycardia,
ischemia*,
arrhythmia
12 |
P a g e
Massive
pulmonary
embolus
Risk factors,
chest pain,
pleurisy,
syncope*,
dizziness*
Central
cyanosis,
↑JVP*, absence
of signs in the
lung*, shock
(tachycardia,
hypotension)
Often normal
Prominent hilar
vessels, oligaemic
lung fields*
↓PaO
2
↓PaCO
2
Sinus
tachycardia,
RBBB, S
1
Q
3
T
3
pattern
↓T (V
1
-V
4
)
Acute
severe
asthma
History of
asthma,
asthma
medications,
wheeze*
Tachycardia,
pulses
paradoxes,
cyanosis (late),
JVP →*, ↓peak
flow, wheeze*
Hyperinflation
only (unless
complicated by
pneumothorax)*
↓PaO2
↓PaCO2
(↑PaCO2
in
extremis)
Sinus
tachycardia
(bradycardia
in extremis)
Acute
exacerbatio
n of COPD
Previous
episodes*,
smoker. If in
type II
respiratory
failure may be
drowsy
Cyanosis,
hyperinflation*,
signs of CO2
retention (flapping
tremor, bounding
pulses)*
Hyperinflation*,
bullae, complicating
pneumothorax
↓ or ⇓PaO2
PaCO2 in type
II failure ±
↑H+, ↑HCO3
in chronic
type II failure
Normal, or signs
of right
ventricular
strain
Pneumonia
Prodromal
illness*,
fever*,
rigors*,
pleurisy*
Fever,
confusion,
pleural rub*,
consolidation*,
cyanosis (if
severe)
Pneumonic
consolidation*
↓PaO2
↓PaCO2
(↑ in
extremis)
Tachycardia
13 |
P a g e
Metabolic
acidosis
Evidence of
diabetes
mellitus or
renal
disease,
aspirin or
ethylene
glycol
overdose
Fetor (ketones),
hyperventilation
without heart or
lung signs*,
dehydration*,
air hunger
Normal PaO2 normal
⇓
PaCO2, ↑H+
Psychogenic Previous
episodes,
digital or
peri-oral
dysesthesias
No cyanosis, no
heart or lung
signs,
carpopedal
spasm
Normal PaO2 normal*
⇓
PaCO2, ↓H+*
Hemoptysis
Coughing up blood, irrespective of the amount, is an alarming symptom and
patients nearly always seek medical advice .
o A history should be taken to establish that it is true hemoptysis and not
hematemesis, or gum or nose bleeding .
o Hemoptysis must always be assumed to have a serious cause until this is
excluded.
o Many episodes of hemoptysis remain unexplained even after full
investigation, and are likely to be caused by simple bronchial infection .
o A history of repeated small hemoptysis, or blood-streaking of sputum, is
highly suggestive of bronchial carcinoma .
o Fever, night sweats and weight loss suggest tuberculosis .
14 |
P a g e
o Pneumococcal pneumonia often causes 'rusty'-colored sputum but can
cause frank hemoptysis, as can all supportive pneumonic infections
including lung abscess .
o Bronchiectasis and intracavitary mycetoma can cause catastrophic
bronchial hemorrhage, and in these patients there may be a history of
previous tuberculosis or pneumonia in early life .
o Finally, pulmonary thromboembolism is a common cause of hemoptysis
and should always be considered.
Causes of hemoptysis
Bronchial disease
1. Carcinoma *
2. Bronchiectasis *
3. Acute bronchitis *
4. Bronchial adenoma
5. Foreign body
Parenchymal disease
1. Tuberculosis *
2. Supportive pneumonia
3. Lung abscess
4. Parasites (e.g. hydatid disease, flukes)
5. Trauma
6. Actinomycosis
7. Mycetoma
Lung vascular disease
1. Pulmonary infarction *
2. Good pasture's syndrome
3. Polyarthritis' nodosa
15 |
P a g e
4. Idiopathic pulmonary haemosiderosis
Cardiovascular disease
1. Acute left ventricular failure *
2. Mitral stenosis
3. Aortic aneurysm
Blood disorders
1. Leukemia
2. Hemophilia
3. Anticoagulants
Physical examination may reveal additional clues. Finger clubbing suggests
bronchial carcinoma or bronchiectasis; other signs of malignancy, such as
cachexia, hepatomegaly and lymphadenopathy, should also be sought .
Fever, pleural rub or signs of consolidation occur in pneumonia or
pulmonary infarction; a minority of patients with pulmonary infarction
also have unilateral leg swelling or pain suggestive of deep venous
thrombosis .
Rashes, hematuria and digital infarcts suggest an underlying systemic
disease such as a vasculitis, which may be associated with hemoptysis .
In the vast majority of cases, however, the haemoptysis itself is not life-
threatening and a logical sequence of investigations should be followed :
Chest X-ray, which may give evidence of a localized lesion including
pulmonary infarction, tumor (malignant or benign), pneumonia,
mycetoma or tuberculosis
Full blood count and clotting screen
Bronchoscopy after acute bleeding has settled, which may reveal a central
bronchial carcinoma (not visible on the chest X-ray) and permit biopsy and
tissue diagnosis
16 |
P a g e
CTPA, which may reveal underlying pulmonary thromboembolic disease or
alternative causes of hemoptysis not seen on the chest X-ray (e.g.
pulmonary arteriovenous malformation or small or hidden tumors) .
Management
In severe acute hemoptysis, the patient should be nursed upright (or on the side
of the bleeding if this is known), and given high-flow oxygen and appropriate
hemodynamic resuscitation .
Bronchoscopy in the acute phase is difficult and often merely shows blood
throughout the bronchial tree .
If radiology shows an obvious central cause, then rigid bronchoscopy under
general anesthesia may allow intervention to stop bleeding; however, the
source often cannot be visualized .
Intubation with a divided endotracheal tube may allow protected ventilation of
the unaffected lung to stabilize the patient .
Bronchial arteriography and embolization , or even emergency pulmonary
surgery, can be life-saving in the acute situation.
Done by: #MOHDZ Dr.bilal –
medicine
17 |
P a g e
