1 |
P a g e
Epidemiology of Diphtheria, Pertussis and Tetanus
Identification
An acute bacterial disease primarily involving tonsils, pharynx, larynx, nose, occasionally
other mucous membranes or skin and sometimes conjunctivae or vagina.
The characteristic lesion, caused by liberation of a specific cytotoxin ( secondary to
proliferation of bacteria at a focus of infection ) is an asymmetrical adherent greyish
white membrane with surrounding inflammation, with cervical lymph nodes enlarged and
tender; in moderate to severe cases there is marked swelling and oedema of the neck that
progress to airway obstruction.
Inapparent infections (colonization) outnumber clinical cases.
The toxin can cause myocarditis, with heart block and progressive congestive failure
beginning about 1 week after onset. Later effect include neuropathies that can mimic
Guillain-Barre´ syndrome.
Diphtheria should be suspected in the differential diagnosis of bacterial especially
streptococcal and viral pharyngitis, infectious mononucleosis, oral syphilis and
candidiasis.
Presumptive diagnosis is based
Observation of an asymmetrical greyish white membrane especially if it extends to the
uvula and soft palate and is associated with tonsillitis, pharyngitis or cervical
lymphadenopathy, or a serosanguineous nasal discharge. Bacteriological examination of
lesions confirms the diagnosis .
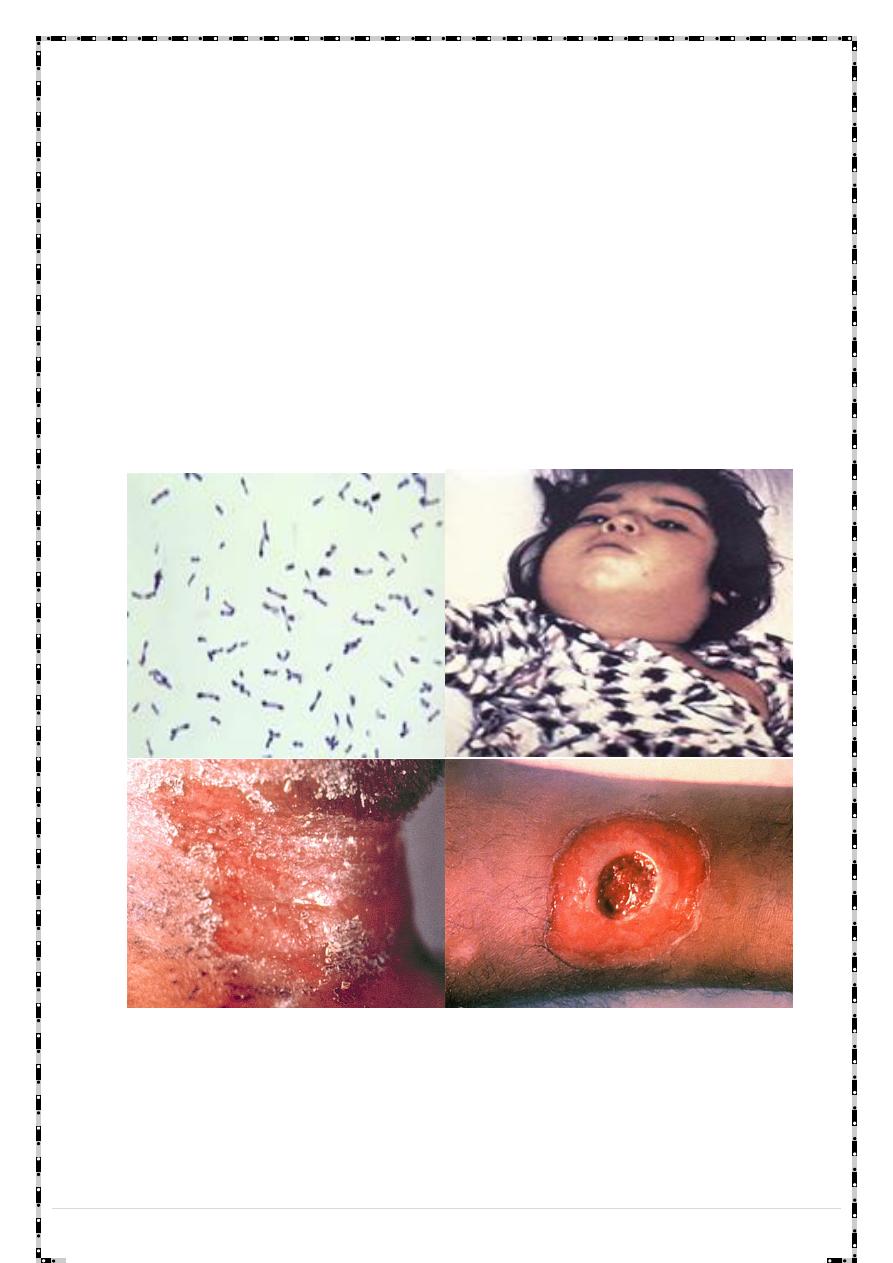
Infectious agent
Corynebacterium diphtheria of biotype : Gravis , Mitis ,Intermedius.
Occurrence
A disease of colder months, primarily involving non immunized children under 15; often
found among adults in population groups whose immunization was neglected.
It is rare in developed countries while it is endemic in developing countries . (diphtheria
is endemic in Iraq) .
Reservoir
:Humans
Carrier
: exist but are less infective than cases .
Mode of transmission
1. Contact with the respiratory droplets of a case or carrier.
2. Soiled articles (indirect).
3. In rare cases raw milk has served as a vehicle.
2 |
P a g e
Incubation period
Usually 2–5 days
Period of communicability
Untreated patients are infectious for 2 to 3 weeks - until virulent bacilli have disappeared
from discharges and lesions. The rare chronic carrier can shed bacilli for 6 months or more.
The disease is usually not contagious 48 hours after antibiotics are instituted.
Susceptibility
Infants born to immune mothers have passive protection, which is usually lost before the
6th month. Disease or inapparent infection usually, but not always, induces lifelong
immunity.
People most susceptible to infection are those who are not completely immunized and
have been exposed to a carrier or diseased individual.
Diphtheria is classified clinically into :
1. Nasal diphtheria : initially resemble common cold with rhinorrhea .
2. Tonsillar and pharyngeal : insidious and more severe .cervical lymphadenitis is
variable . ( Bull neck : odema of the soft tissue of the neck).
3. Laryngeal .
4. Cutaneous, vulvovaginal, conjectival .
Methods of control
The control of diphtheria is based on 3 measures:
1. Ensuring high population immunity through vaccination.
2. Rapid investigation and treatment of contacts.
3. Early diagnosis and proper case management.
A) Preventive measures
1. Educational measures are important: inform the public particularly parents of young
children, of the hazards of diphtheria and the need for active immunization
2. Immunization
Doses of 0.5 ml DTP intramuscularly in outer part of thigh, according to national schedule.
If immunization is started later, there must be an interval of 4 weeks between doses.
DTP vaccine must be stored between +2°C and +8°C.
DTP vaccine can be given to immunocompromised children up to 7 years old; Td vaccine
can be given to immunocompromised adults.
3 |
P a g e
There are four combination vaccines used to prevent diphtheria, tetanus and pertussis:
DTaP, Tdap, DT, and Td. Two of these (DTaP and DT) are given to children younger than 7
years of age, and two (Tdap and Td) are given to older children and adults.
Children should get 5 doses of DTaP, one dose at each of the following ages: 2, 4, 6, and
15-18 months and 4-6 years. DT does not contain pertussis, and is used as a substitute for
DTaP for children who cannot tolerate pertussis vaccine.
For persons 7 years and older
Because adverse reactions may increase with age, a preparation with a reduced
concentration of diphtheria toxoid (adult Td) is usually given after the seventh birthday
for booster doses. For a previously unimmunized individual, a primary series of 3 doses of
tetanus and diphtheria toxoids (Td) is advised, 2 doses at 4-8 weeks intervals and the third
6 months to 1 year after the second dose.
Td is a tetanus-diphtheria vaccine given to adolescents and adults as a booster shot every
10 years, or after an exposure to tetanus under some circumstances (such as health
workers are fully immunized and receive a booster dose of Td every 10 years ).
For those who are severely immunocompromised or infected with HIV, diphtheria
immunization is indicated, with the same schedule and dose as for immunocompetent
persons.
B) Control of patient, contacts and the immediate environment.
Diphtheria antitoxin and antibiotic therapy are the cornerstone of therapy for diphtheria
and it is started immediately without waiting for lab results.
antitoxin to neutralize (counteract) the toxin produced by the bacteria.
antibiotics kill and eliminate diphtheria bacteria.
Patients
Diphtheria antitoxin (DAT ) I.M (20,000 to 100,000 units) in a single dose, immediately
after throat swabs have been taken. Procaine penicillin G I .M (25,000 to 50,000
units/kg/day for children; 1.2 million units/day for adults in 2 divided doses) or
erythromycin until the patient can swallow; then Oral penicillin V in 4 doses a day.
Antibiotic treatment should be continued for a total period of 14 days.
Isolation: strict isolation for pharyngeal diphtheria or contact isolation for cutaneous
diphtheria, until 2 cultures from both throat and nose (and skin lesions in cutaneous
diphtheria),not less than 24 hours apart, and not less than 24 hours after cessation of
antibiotherapy.
Tracheostomy and artificial respiration .
4 |
P a g e
Note: Clinical diphtheria does not necessarily confer natural immunity, and patients
should therefore be vaccinated before discharge from a health facility.
Close Contacts
All close contacts should have cultures taken from nose and throat. All must receive a
single dose of benzathine penicillin G i.m. (600,000 units for children < 6 years; 1.2 million
units for 6 years or older).
Previously immunized contacts should receive a booster dose of diphtheria toxoid.
primary series should be initiated in nonimmunized contacts, depending on the contact’s
age.
Carriers
All must receive a single dose of benzathine penicillin G i.m. (600,000 units for children <
6 years; 1.2 million units for 6 years or older. If culture is positive, treat as patients.
Epidemiology of pertussis ( Whooping cough )
Identification
A highly contagious upper respiratory tract bacterial infection. Clinically has 3 stages; the
initial catarrhal stage is characterized by the insidious onset of coryza (runny nose),
5 |
P a g e
sneezing, low-grade fever, and a mild, occasional cough, similar to the common cold. The
cough gradually becomes more severe and irritating.
In the convalescent stage, recovery is gradual. The cough becomes less paroxysmal and
disappears over 2 to 3 weeks and vomiting stop . However, paroxysms often recur with
subsequent respiratory infections for many months after the onset of pertussis. Fever is
generally minimal throughout the course of pertussis.
Complication
B) Arise from increased pressure during attacks of paroxysmal cough and secondary
bacterial infection & malnutrition .
C) Pneumonia is a relatively common complication
D) Haemorrhages (subconjunctival, petechiae and epistaxis)
E) Convulsions.
F) Encephalopathies
G) Death occur more rarely ( in children less than 3 years ).
H) Complications are more frequent and severe in younger infants. Older persons
(adolescent and adults), and those partially protected by the vaccine usually have
milder disease.
Clinical case definition
1. A case diagnosed as pertussis by a physician, or
2. A person with a cough lasting at least 2 weeks with at least one of the following
symptoms:
3. Paroxysms of coughing.
4. Inspiratory “whooping”.
5. Post-tussive vomiting (vomiting immediately after coughing).
Case classification
Clinical case: A case that meets the clinical case definition.
Confirmed case: A clinical case that is laboratory confirmed (isolation of Bordetella
pertussis, by PCR, culture , or positive paired serology).
In infants, older vaccinated children,adolescents,and adults the clinical course may not
be typical , and prolonged coughing may be the only symptom.
In these cases, diagnosis of pertussis requires lab. Methods for confirmation
Infectious agent
Bacterium: Bordetella pertussis(small Gram-negative coccobacillus that infects the
mucosal layers of the human respiratory tract).
Occurrence
6 |
P a g e
An endemic disease common to children (especially young children), regardless of
ethnicity, climate or geographic location.
Outbreaks occur typically every 3 to 4 years cyclical disease.
In Iraq according to MOH report 2012 , the number of whooping cough cases were 2370
,the highest no. of cases was reported from Baghdad followed by Babylon.
Reservoir
Humans are the only host for pertussis.
Mode of transmission
direct contact with discharges from respiratory mucous membranes of infected persons
via the airborne route.
Even though the disease may be milder in older persons, these infected persons may
transmit the disease to other susceptible persons, including non-immunized or under-
immunized infants. Adults are often found to be the first case in a household with multiple
pertussis cases.
Incubation period
Average 9–10 days (range 6–20 days).
Period of communicability
Pertussis is highly communicable in the early catarrhal stage. Communicability gradually
decreases after the onset of the paroxysmal cough. Untreated patients may be
contagious for up to 3 weeks after the onset of paroxysmal cough in the absence of
treatment or up to 5 days after onset of treatment.
Susceptibility
Anyone who has not had pertussis previously or who has not received the pertussis
vaccine can get the disease.
Immunity following disease or vaccination is not lifelong. Older children, adolescents and
adults can become susceptible to pertussis five-to 10-years after their last dose of
pertussis-containing vaccine.
Begin at birth , no maternally acquired immunity.
The highest around school age (5-7) years and almost all become immune by the age of
15 years .
Sex incidence and fatality more in female than in males .
7 |
P a g e
Adults may occasionally be affected.
Methods of control
A) Preventive measures:
Active immunization by pertussis vaccine (killed vaccine) used in form of DPT for children
below 4 years.
DTP-containing multi-antigen vaccines (with Hep B, Hib, or IPV) are increasingly being
used in national immunization campaigns.
No single antigen pertussis vaccine is available.
Protective value : around 80% prevent the disease ,and lowers duration and severity
&fatality of disease in the vaccinated children
Pertussis vaccine must not be given to :
1. All children over 4 years .
2. At risk ,below 4 years.
cases of convulsion history given by the mother
History of epilepsy in 1
st
degree relative
Those showing adverse reaction after giving vaccine ,further doses should not be given
(give DT).
The reactions are :
1. Persistent crying lasting 3 hours or more or unusual high pitch cry occur within 48
hours.
2. Fever of 40C or greater within 24 hours.
3. Collapse or shock like state (hypotonic ) within 24 hours.
4. Acute encephalopathy within 7 days including sever alteration in consciousness with
generalized or focal neurological signs.
5. Convulsion with or without fever within 3 days.
Health education: of parents for basic knowledge of the disease & the protective value
and precautions with the vaccination.
Seroprophylaxis: antipertussis immunoglobulin 2.5 ml IM can be given to protect
susceptible contact , specially infants &young children . Protective value is not certain, So
chemoprophylaxis is preferred.
Chemoprophylaxis oral erythromycin or clarithromycin can be given in proper dosage, for
5 days after the last contact with the case to:
Infants & young children not actively immunized before.
8 |
P a g e
Susceptible school contacts .
Control measures (Case management)
Reporting to local health authority .
Isolation at home : practically difficult since the majority of cases are mild with no or slight
fever , they usually move in the community and go to school and spread infection to
exposed susceptible children .
Suspected cases who do not receive AB should be isolated for 3 weeks .
Erythromycin or clarithromycin should be administered for 14 days to all cases and close
contacts of persons with pertussis, regardless of age and vaccination status, 40 mg/kg/day
for children and 1 g/day for adults.
Drug administration both
(1) modifies the course of illness (if initiated early)
(2) eradicates the organism from secretions, thereby decreasing communicability.
Trimethoprim –sulfamthoxazole may be used in case of allergies
contacts
If the contact is an infant, should be separated From the patient, given prophylactic
erythromycin for 10 days.
If the infant cant be separated erythromycin should be given for the whole period of
communicability.
Child 3-4 years and has been immunized , should be given a booster dose as soon as
possible.
If the child has not been immunized ,should be given prophylactic erythromycin
Epidemiology of tetanus
Identification
An acute disease induced by an exotoxin of the tetanus bacillus, which grows
anaerobically at the site of an injury. The disease is characterized by painful muscular
contractions, primarily of the masseter and neck muscles, secondarily of trunk muscles. A
common first sign suggestive of tetanus in older children and adults is abdominal rigidity,
though rigidity is sometimes confined to the region of injury. Generalized spasms occur,
frequently induced by sensory stimuli; typical features of the tetanic spasm are the
position of opisthotonos and the facial expression known as “risus sardonicus
Generalized spasms occur, frequently induced by sensory stimuli; typical features of the
tetanic spasm are the position of opisthotonos and the facial expression known as “risus
sardonicus.
9 |
P a g e
History of an injury or apparent portal of entry may be lacking. The case-fatality rate
ranges from 10% to over 80%, it is highest in infants and the elderly.
Infectious agent
Clostridium tetani, the tetanus bacillus.
Occurrence
The disease is more common in agricultural regions and in areas where contact with
animal excreta is more likely and immunization is inadequate. In rural and tropical areas
people are especially at risk, and tetanus neonatorum is common. The disease is sporadic
and relatively uncommon in most industrial countries.
Reservoir
Intestines of horses and other animals, including humans, in which the organism is a
harmless normal inhabitant. Soil or fomites contaminated with animal and human feces.
Tetanus spores, can contaminate wounds of all types.
Mode of transmission
Tetanus spores are usually introduced into the body through a puncture wound
contaminated with soil, street dust or animal or human feces; through lacerations, burns
and trivial or unnoticed wounds; or by injected contaminated drugs (e.g. street drugs).
Tetanus occasionally follows surgical procedures, which include circumcision and
abortions performed under unhygienic conditions. The presence of necrotic tissue and/or
foreign bodies favors growth of the anaerobic pathogen.
Incubation period
Usually 3–21 days, average 10 days. Most cases occur within 14 days. In general, shorter
incubation periods are associated with more heavily contaminated wounds, more severe
disease and a worse prognosis.
Period of communicability
No direct person-to-person transmission.
Susceptibility and resistance
Susceptibility is general. Active immunity is induced by tetanus toxoid and persists for at
least 10 years after full immunization; transient passive immunity follows injection of
tetanus immune globulin (TIG) or tetanus antitoxin (equine origin). Infants of actively
immunized mothers acquire passive immunity that protects them from neonatal tetanus.
Recovery from tetanus may not result in immunity; second attacks can occur and primary
immunization is indicated after recovery.

10 |
P a g e
Methods of control
A-Preventive measures.
1. Educate the public on the necessity for complete immunization with tetanus toxoid, the
hazards of puncture wounds and closed injuries that are particularly liable to be
complicated by tetanus, and the potential need after injury for active and/or passive
prophylaxis.
2. Active immunization with adsorbed tetanus toxoid (TT), which gives durable protection
for at least 10 years; after the initial basic series has been completed, single booster doses
elicit high levels of immunity. In children under 7, the toxoid is generally administered
together with diphtheria toxoid and pertussis vaccine as a triple (DTP or DTaP) antigen, or
as double (DT) antigen when contraindications to pertussis vaccine exist.
3. Prophylaxis in wound management: Tetanus prophylaxis in patients with wounds is
based on careful assessment of whether the wound is clean or contaminated, the
immunization status of the patient, proper use of tetanus toxoid and/or TIG, wound
cleaning and, where required, surgical debridement and the proper use of antibiotics.
B- Control measures
Report to local health authority.
Specific treatment: TIG IM in doses of 3000–6000 IU. If immunoglobulin not available,
tetanus antitoxin in a single large dose should be given. Metronidazole should be given
for 7–14 days in large doses, muscle relaxants and sedatives required. Maintain an
adequate airway and employ sedation as indicated; muscle relaxant drugs together with
tracheostomy or nasotracheal intubation and mechanically assisted respiration may be
lifesaving. Active immunization should be initiated concurrently with treatment
