1
Lec.1
Pediatrics
6
th
stage
Session notes
د.ربيع الدبوني
-
:
s
r
ea
uestions from previous y
Q
A neonate 1 month age , with persistent jaundice , hard stool ,
posterior fontanlle open
The result of investigations :
TSB( total serum bilirubin ) =? , Hb=14g/dl , T3=low , T4=low ,
TSH= high
Dx:- Cretinism (1ry or congemital hypothyroidism).
A child 2 years old ,presented with fever for 2 weeks ,
on exam:-
his temperature = 38.9 degree centigrades , spleen ,L.N all are
NOT palpable ,liver 1finger palpable
1.mention two possible differential diagnose?
2.mention most important investigation ?
Hint:-
Platlets count=60
Hb=6g/dl
Bilirubin=normal
WBCs =5000 (5 x 10
9
/L)
DDx:-
1-leukemia
2-aplastic anemia
Others ( rarely parvovirus infection , infectious mononuclosis )
Investigation:-Bone Marrow exam .
Note:- always consider B.M exam in pancytopenia .(very imp)

2
When two line of cell affected in bone marrow then we need BM
biopsy
Neonatal jaundice :-
65% of infants are having jaundice in 1
st
wk of life.
In most cases it is benign condition &resolved by itself.
Others is pathological and can end with persistent damage and
kernictrus
Pathophysiology:-
the liver is incapable of dealing with the excess bilirubin ,this
excess bilirubin resulted from the normal polycythemic state of
the infant in the intrauterine life,when baby is delivered there will
be no need for the polycythemic state(lazy circulation is being
established),and hyperviscosity syndrome so the excess RBCs will
be degraded & bilirubin level will start to raise .
this bilirubin needs mature hepatocytes to deal with it & sufficient
amount & activity of transferase enzyme.
prematurity predisposes neonates to more severe jaundice.
Notes :-
Dusky color of a neonate masks the yellow tint of jaundice,
that's explain the late presentation of jaundice baby.
Hb in neonate=(18-20) +/- 2 .
There is physiological anemia in 2 months infant
Hb=9g/dl(full term baby).
Hb=7.5g/dl(preterm baby).
((if that range 9 or 7.5 g/dl in neonate , he will be considered
as anemic))
3
Bilirubin is one of the most potent anti-oxidant ,when it is
raised in the early days of life this will help in getting rid of the
free radicals.
1g/dl of Hb will give 34mg/dl of bilirubin.
Papkin's reflex :palmomental reflex ,if persisted beyond 4-6mo
,this is mostly due to frontal lobe damage"CP".
Glanzmann disease:-platelets dysfunction.
In first days of neonate life Hb < 18 mg/dl considered anemic
Hx of baby with jaundice:-
1-cause
2-effect of this jaundice
3-duration(in hours not days)
4-LMP/EDD
Birth weight , Rh , ABO of father and mother
5-prenatal ( mother's disease , chemical exposure , drugs , previous
Hx of mother's ( jaundice + HBV )
Natal ( mode of delivery )
postnatal Hx
Did he cry immediately after birth? Need resusitation ?
Time of start of feeding?type?
Child now receive adequate nutrition?
6-ask about signs &symptoms of jaundice?
Poor sucking
Poor reflexes
Lethargy
7-ask on family History :-
did other siblings have the same?
Did they exposed to phototherapy ?
exchange transfusion?
4
Did anyone of them have hemolytic disease"G6PD" & Gall stones"
Hereditary spherocytosis
don’t mention thalassemia &Sickle cell anemia as HbF is high in te first 3
months ".
At last you can say:-the health of the baby is severely disturbed.
Example :-
A baby who was delivered by NVD at (39)wks was presented to hospital
with jaundice started at 2
nd
day as it was observed by the family.
Physical exam :-
Is it jaundice really??
By gentle pressure on the nose or forehead or sternum .
What is the cause?
What is the effect?
Eye exam:-by holding the baby from axilla ,bending him fore
&backward ,he will open the eye & we can see the sclera.
Dont try to open eye forcefully because this can lead to Orbicularis
muscle damage of eye in neonate )
Measure the wt?
Mature or premature ?
Dysmorphic features?
Anterior & posterior fontannelles?"wide posterior fontannelle in
hypothyroidism"
Birth markers ?(bruises&cephalohematoma).
Hepatosplenomegaly?
Rash?"TORCHS infection & severe Rh incompatibility"
Anemia"pallor"
Activity"primitive reflexes"
Define "important"
5
Small for gestational age:- a baby weight at birth <10
th
centile mostly
due to IUGR Lead to placental insufficiency "hypoxia" this cause 2ry
polucyehemia increase Hb breakdown increase bilirubin
*(between 10
th
&90
th
centile he is appropriate for age )
Large for date:-infant of diabetic mother .(high insulin = high growth
hormone).
LBW:- a baby wt at birth <2500kg.
Premature:- baby NOT completed 37wks calculated from 1
st
day of
LMP.
*full term "37-42"wks.
Rash + jaundice = TORCH infection
Criteria of physiological jaundice ? important .
Rh incompatibility:-
No naturally occurring Anti-D,it should be induced by presence of
D+ve RBCs ,abortion,BT , previous delivery,previous still birth.
History :- yellowish discoloration started from the 1
st
day ,his mother
Rh-ve.
His brother has the same state , or one of his brother has
kernicterus.
4 investigations:-
1-TSB:-
a-direct
b-indirect
2-CBP
3-Rh & ABO incompatibility
6
4-coomb's test=+ve.
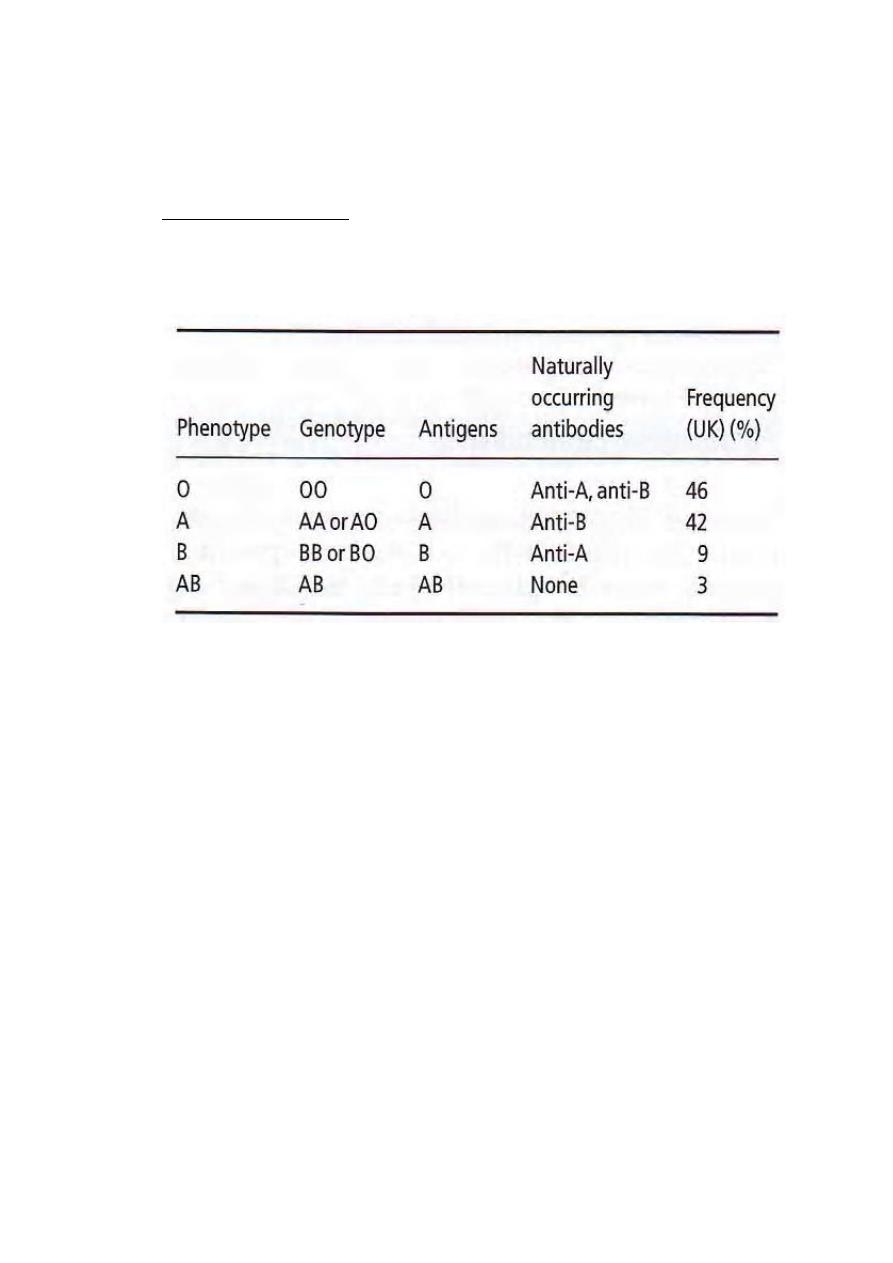
ABO incompatibility:-
Mother =O
Infant=A/B/AB.
Coomb's test=weakly +ve
Retic # raised
Hb reduced.
In the film of ABO incompatibility :-
brisk spherocytosis .
this condition is also encountered in
1-autoimmune Hemolytic anemia.
2-burns.
Mother A , baby B is there is sensitization ?
All AB is isoglobenization , IgM > 6 times of IgG and this can't pass
placenta , if mother is O 80% IgM from it have a subtype 15% of these
mothers have IgG of O can cross placental and lead to problem in A ,
B , ABO
7
G-6-PD deficiency
Characters :-
Hb low
Retic# raised
FHx +ve X- linked recesive ( Brother, mothers , aunt )
Coomb's test-ve .
The mother is carrier in 40-60% of cases.
Lyon hypothesis :-Randomly one
x
will be inactivated ,other one
remains active (dose effective).
Management of jaundice in the 1
st
week of life :
25 mg/dl Bilirubin is considered the limit border
Either there is no need for Tx especially if there is no hemolysis , full
term baby , healthy active and the jaundice is not deep with criteria of
phsiologic jaundice
For safe management start at 20 mg/dl to prepare for blood transfusion
Double volume exchange
Technique : a double voume exchange removes approximately twice the
infant circulting blood volume 170 ml/kg of the ( infant is approximately
80-90 ml/kg body wt ) replacing it with cross matched whole blood . the
procedure involves placement of central catheter and removing and
placing blood in a volume that is approximately 10% or less of the infant
blood volume.
Most of bilirubin is extravascular , as a result excahange transfusion
remove approximately 25% of thr total body bilirubin , after the
procedure serum bilirubin falls to approximately 1/2 of pre excahange
value the increase to 2/3 of that levels as extravascular and vascular
bilirubin re-equilibirate .
8
Side effects of exchange transfusion
o Hyperkalemia(old blood is being used > 72 hours ).
o Hypocalcemia(Ca hadn't given)
o Hypoglycemia(if we didn't monitor blood glucose especially in Rh
incompatibility)
o Volume overload (if your transfusion wasn't accurate).
o Shock(if large amount had been drawn at first)
o Anemia(you didin't shake well the contents ,RBCs precipitate
downward )
you should monitor the heart
should be in adequte weather avoid hypothermia
acid glucos-phosphate added
phosphate chelate the calcium can lead to convlusio by hypocalcemia
bicarbonate added to resolve ascidosis
fatality in this procedure can is 1-2%
advice mother to prevent feeding before 1 hour
check blood glucose
Rh in glucose + hypothermia what is the difference from others ?
Rh patient has Neisu-diabilstosis ( hyperplasia pf islet cell in pancreas )
This lead to surge secretion of insulin which cause hypoglycemia
Phototherapy
o visible spectrum of light(it is NOT ultraviolet light).
o The most appropriate spectrum is blue light with450nm .
bilirubin in the skin absorbs the light energy which by
-
Mechanism:
photoisomerization converts the toxic unconjucated bilirubin to a
9
product which can be excreted in bile without the need for
conjucation,also phototherapy converts unconjucated bilirubin to
lumirubin which is excreted in the kidney.
Side effects of phototherapy:-( very important).
i
Hypo/hyperthermia
ii
Dehydration
iii
Diarrhea
iv
Rash
v
Bronze baby syndrome.
vi
Eye injury & nasal obstruction .
Note :-
TSB at first 7hrs it began to raise , then it goes down as the
phototherapy continued.
As you perform phototherapy , you should increase the
maintainance fluid by(30%-10%)
Jaundice (prolonged neonatal jaundice)
>10days
Divided into two divisions:-
Indirect hyperbilirubinemia cholestatic jaundice
Direct Bilirubin <20% of total 1-direct bilirubin>20%of
total serum bilirubin.
Serum bilirubin.
**4 causes
1-hemolysis
11
2-crigler Najjar syndrome
3-Breast milk jaundice
4-hypothyroidism.
Prolonged jaundice + indirect hyperbilirubinemia screen
for hemolysis is indicated .
Direct hyperbilirubinemia
1-extrahepatic biliary atresia:-clay color stool ,,portal
hypertension,,operation is the Rx :-kasai operation
(portojejunostomy)/Alkaline phosphatase raised as there is
obstruction(malrotation of mid gut ,diagnosed by :Ba
enema//choledochal cyst :diagnosed by Ultrasound).
2-idiopathic neonatal hepatitismostly male , defecation of the baby
had been normal color & consistency for some time before the
condition deteriorates//ALT & AST will be raised.
How to differentiate between the two ?
By HIDA test:-Radio-isotope in vein
If the uptake is Normal but the excretion is slow biliary atresia.
Hepatitis
عكس هذا يحدث في
Rx:-
1-medium chain triglycerides.
2-vitamines injection"A>E<K>D"
3-cholestramine
4-supportive care
5-liver transplant.
Others :-
11
o Torchserology
o HBV/HCVserology
o Sepsis (Blood,CSF&urine cultures)
o UTIurine culture.
o CFsweat chloride test
o Alpha -1- anti-trypsin deficiency(immunoassay).
o Galactosemia(deficiency in Glucose -1-PUT):this enzyme is
estimated in RBCs & fibroblasts//if there is +ve reducing substance
in urine other than glucose means galactosemia(Isomil is
prescribed for them)
Notes:-
glucose deposition in the eyescataract.
In brainconvulsion
In kidneyRTA
In liverjandice
