
1
Surgery Dr.Hussein
Retrosternal goiter
Very few retrosternal goitres arise from ectopic thyroid tissue; most arise from the
lower pole of a nodular goitre. If the neck is short and the pretracheal muscles are
strong, particularly in men, the negative intrathoracic pressure tends to draw these
nodules into the superior mediastinum.
Clinical features
A retrosternal goitre is often symptomless and discovered on a routine chest
radiograph . There may, however, be severe symptoms:
Dyspnoea, particularly at night, cough and stridor (harsh sound on inspiration).
Many patients attend a chest clinic with a diagnosis of asthma before the true
nature of the problem is discovered.
Dysphagia.
Engorgement of facial, neck and superficial chest wall veins; in severe cases there
may be obstruction of the superior vena cava.
Chest and thoracic inlet radiographs show a soft-tissue shadow in the superior
mediastinum, sometimes with calcification and often causing deviation and
compression of the trachea. A CT scan gives the most accurate and often dramatic
anatomical visualisation.
Recurrent nerve paralysis is rare; the goitre may also be malignant or toxic.
Significant tracheal compression and obstruction may be demonstrated objectively by
a flow–volume loop pulmonary function test in which the rate of flow is plotted
against the volume of air inspired and then expired. Deterioration in flow because of
an increase in tracheal compression, either acutely or in the long term, may be used
to monitor progression of the disease and indicate the need for surgery.
Treatment
If obstructive symptoms are present in association with thyrotoxicosis it is unwise to
treat a retrosternal goitre with antithyroid drugs or radioiodine as these may enlarge
the goitre. Resection can almost always be carried out from the neck, but median
sternotomy is sometimes necessary .
2
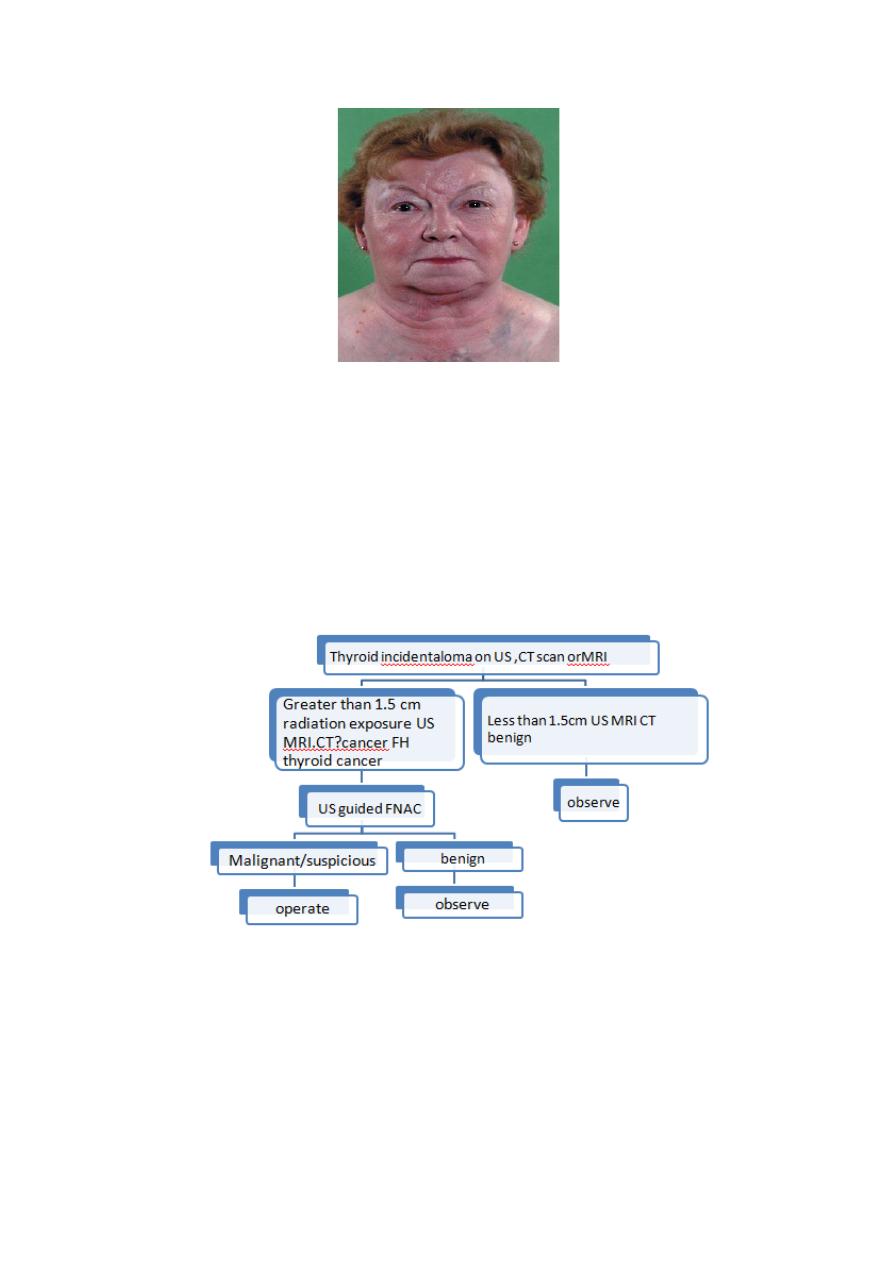
Thyroid incidentaloma
These are clinically unsuspected and impalpable thyroid swellings and, in some parts
of the world, this has reached ‘epidemic’ proportions.
The vast majority of impalpable thyroid swellings can be safely managed expectantly
by a single annual review, with no intervention unless certain criteria are met or the
swelling becomes palpable.
HYPERTHYROIDISM
Thyrotoxicosis
Clinical types are:
1) diffuse toxic goitre (Graves’ disease);
2) toxic nodular goitre;
3) toxic nodule;
4) hyperthyroidism due to rarer causes.
3
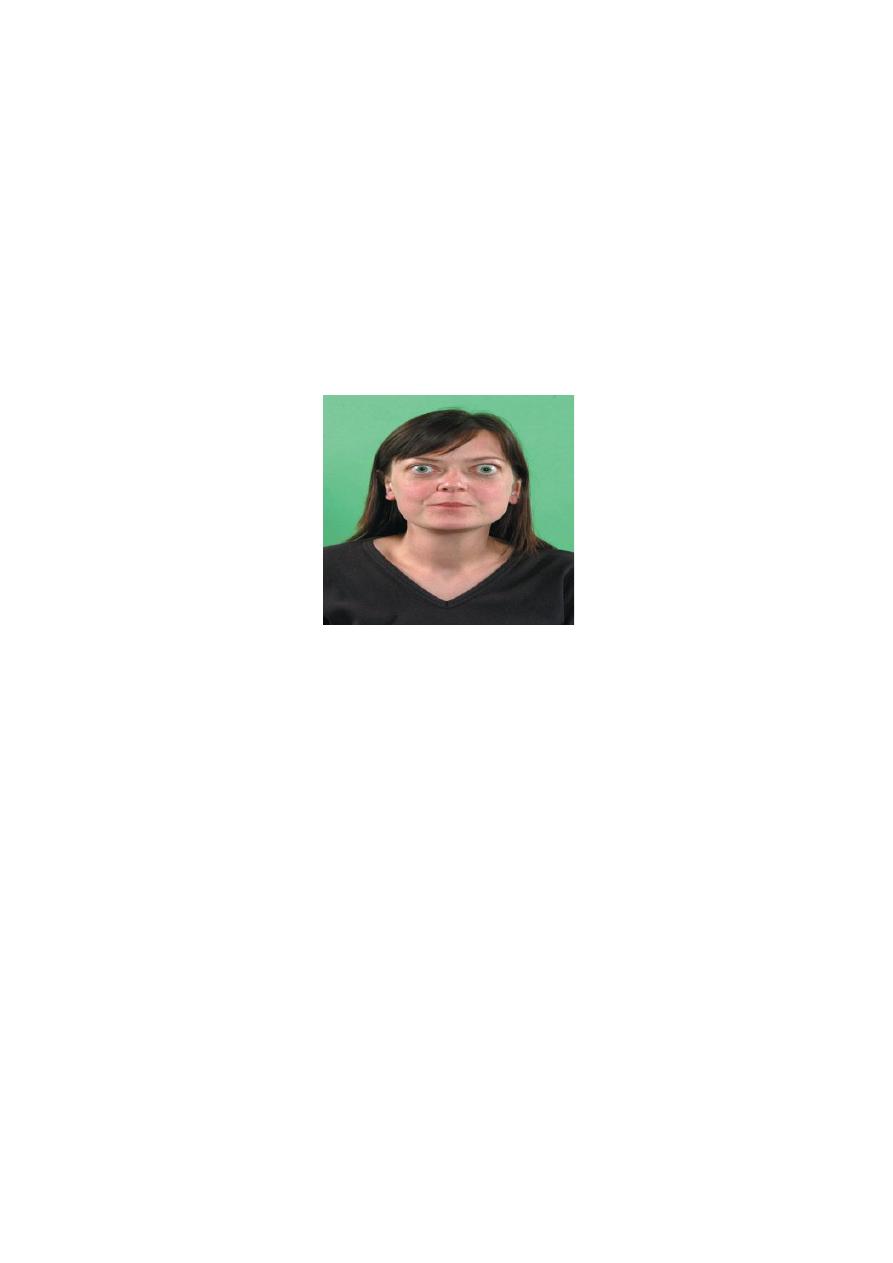
Diffuse toxic goitre :
Graves’ disease, a diffuse vascular goitre appearing at the same time as the
hyperthyroidism, usually occurs in younger women and is frequently associated with
eye signs. The syndrome is that of primary thyrotoxicosis ; 50% of patients have a
family history of autoimmune endocrine diseases. The whole of the functioning
thyroid tissue is involved, and the hypertrophy and hyperplasia are due to abnormal
thyroid-stimulating antibodies (TSH-RAbs) that bind to TSH receptor sites and
produce a disproportionate and prolonged effect.
Toxic nodular goitre
A simple nodular goitre is present for a long time before the hyperthyroidism, usually
in the middle-aged or elderly, and is very infrequently associated with eye signs. The
syndrome is that of secondary thyrotoxicosis.
Toxic nodule
A toxic nodule is a solitary overactive nodule, which may be part of a generalised
nodularity or a true toxic adenoma. It is autonomous and its hypertrophy and
hyperplasia are not due to TSH-RAb. TSH secretion is suppressed by the high level of
circulating thyroid hormones and the normal thyroid tissue surrounding the nodule is
itself suppressed and inactive.
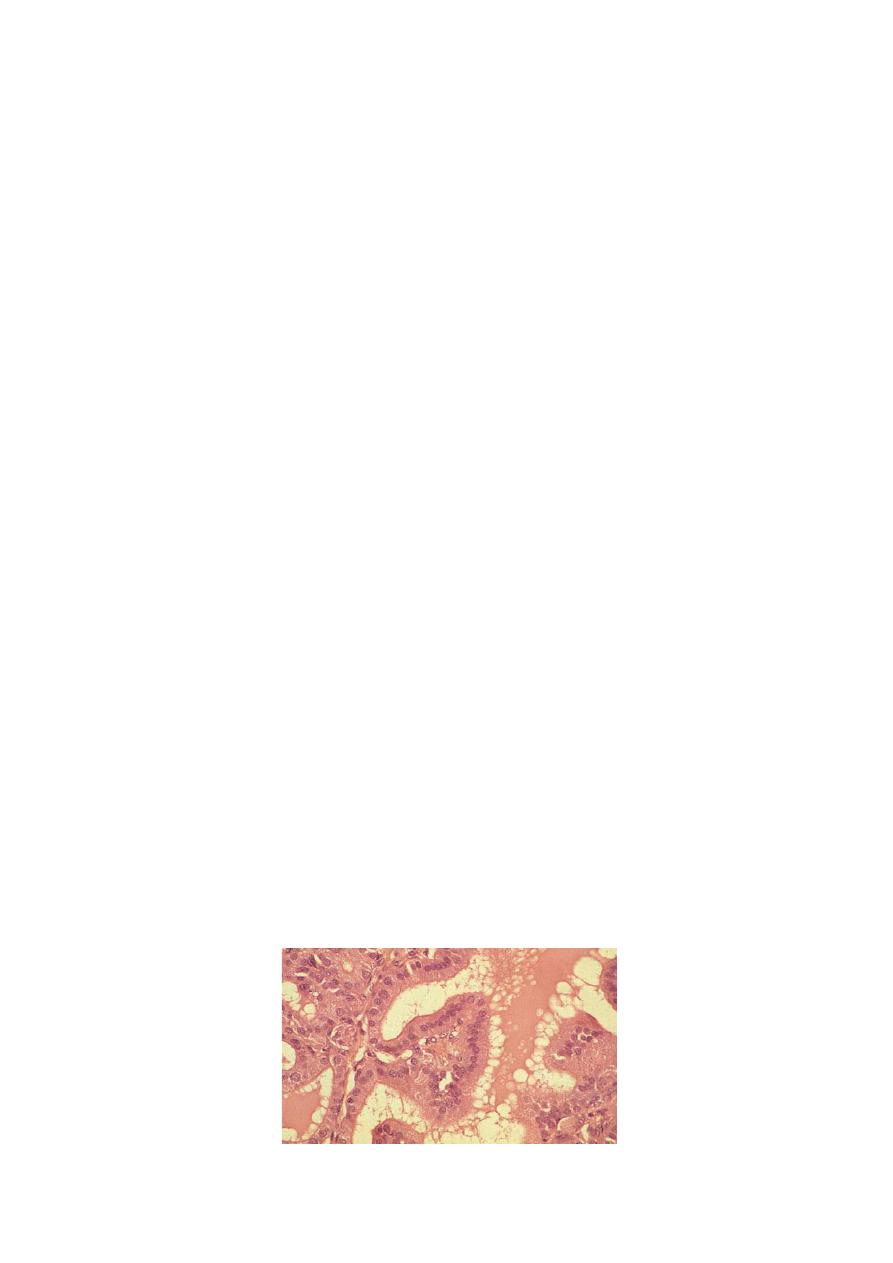
Histology
The normal thyroid gland consists of acini lined with flattened cuboidal epithelium
and filled with homogeneous colloid. In hyperthyroidism there is hyperplasiaof acini,
which are lined by high columnar epithelium. Many of them are empty and others
contain vacuolated colloid with a characteristic ‘scalloped’ pattern adjacent to the
thyrocytes.
4
Clinical features
The symptoms are:
1) tiredness;
2) emotional lability;
3) heat intolerance;
4) weight loss;
5) excessive appetite;
6) palpitations.
Symptomatology
Thyrotoxicosis is eight times more common in women than in men. It may occur at
any age. The goitre in primary thyrotoxicosis is diffuse and vascular; it may be large or
small, firm or soft, and a thrill and a bruit may be present. The onset is abrupt but
remissions and exacerbations are not infrequent. Hyperthyroidism is usually more
severe than in secondary thyrotoxicosis but cardiac failure is rare. Manifestations of
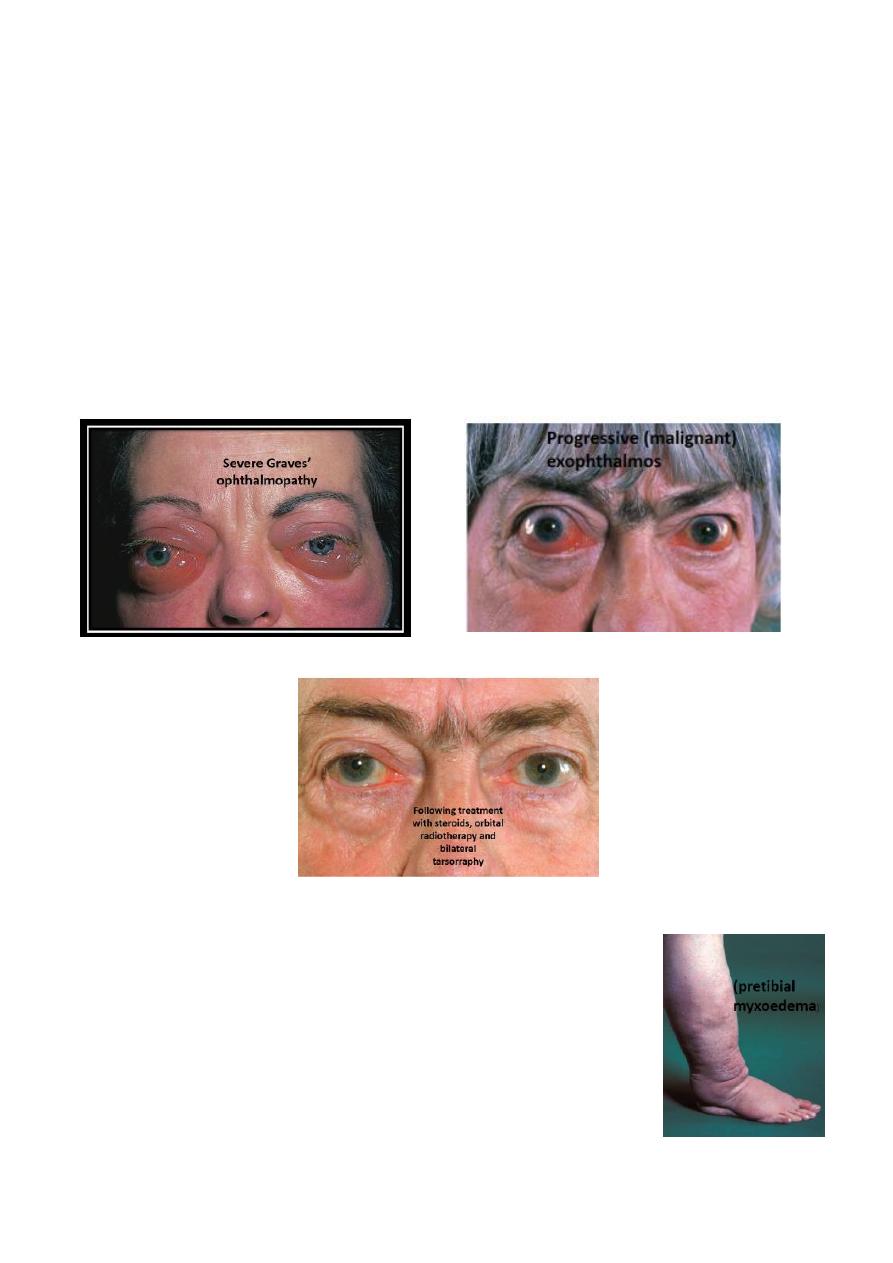
thyrotoxicosis not due to hyperthyroidism per se, for example orbital proptosis,
ophthalmoplegia and pretibial myxoedema, may occur in primary thyrotoxicosis.
In secondary thyrotoxicosis the goitre is nodular. The onset is insidious and may
present with cardiac failure or atrial fibrillation. It is characteristic that the
hyperthyroidism is not severe. Eye signs other than lid lag and lid spasm (due to
hyperthyroidism) are very rare.
Cardiac rhythm
A fast heart rate, which persists during sleep, is characteristic. Cardiac arrhythmias
are more common in older patients with thyrotoxicosis because of the prevalence of
coincidental heart disease.
The signs of thyrotoxicosis are:
1) tachycardia;
2) hot, moist palms;
3) exophthalmos;
4) lid lag/retraction;
5) agitation;
6) thyroid goitre and bruit.
5
Stages of development of thyrotoxic arrhythmias are:
1. multiple extrasystoles;
2. paroxysmal atrial tachycardia;
3. paroxysmal atrial fibrillation;
4. persistent atrial fibrillation, not responsive to digoxin.
Myopathy :
Weakness of the proximal limb muscles is commonly found if looked
for. Severe muscular weakness (thyrotoxic myopathy), resembling myasthenia gravis,
occasionally occurs. Recovery proceeds as hyperthyroidism is controlled.
Thyroid dermopathy (‘pretibial myxoedema’) is a rare condition
characterised by thickening of the skin, usually in areas of trauma,
by deposition of hyaluronic acid in the dermis and subcutis. It
usually occurs a few years after the onset of thyrotoxicosis and
usually responds to treatment of the underlying thyroid disorder
and topical steroids.

6
Thyrotoxicosis should always be considered in:
children with a growth spurt, behaviour problems or myopathy;
tachycardia or arrhythmia in the elderly;
unexplained diarrhoea;
loss of weight.
Diagnosis of thyrotoxicosis
Most cases are readily diagnosed clinically. Difficulty is most likely to arise in the
differentiation of mild hyperthyroidism from an anxiety state when a goitre is
present. T3 thyrotoxicosis is diagnosed by estimating the free T3. It should be
suspected if the clinical picture is suggestive but routine tests of thyroid function
reveal a normal T4 but suppressed TSH. A thyroid scan is required to diagnose an
autonomous toxic nodule and differentiate it from a dominant swelling in a toxic
multinodular goitre.
Principles of treatment of thyrotoxicosis
Non-specific measures are rest and sedation; the use of anti-thyroid drugs, surgery
and radioiodine.
Anti-thyroid drugs
Those in common use are carbimazole and propylthiouracil. β- Adrenergic blockers
such as propranolol and nadolol are used to block the cardiovascular effects of the
elevated T4. Iodides,
which may reduce the vascularity of the thyroid, should be used only as immediate
preoperative preparation in the 10 days before surgery.
- Advantages. No surgery and no use of radioactive materials.
- Disadvantages. Treatment is prolonged and the failure rate is atleast 50%. The
duration of treatment may be tailored to the severity of the toxicity, with milder
cases being treated for only 6 months and severe cases for 2 years before stopping
therapy.
Surgery
In diffuse toxic goitre and toxic nodular goitre with overactive internodular tissue,
surgery cures by reducing the mass of overactive tissue.

7
- Advantages. The goitre is removed, the cure is rapid and the cure rate is high if
surgery has been adequate.
- Disadvantages. Recurrence of thyrotoxicosis occurs in approximately 5% of cases if
less than total thyroidectomy is carried out. There is a risk of permanent
hypoparathyroidism and nerve injury. Young women tend to have a worse
cosmetic result from the scar.
Radioiodine
Radioiodine destroys thyroid cells and, as in thyroidectomy, reduces the mass of
functioning thyroid tissue to below a critical level.
- Advantages. No surgery and no prolonged drug therapy.
- Disadvantages. Isotope facilities must be available.
Choice of therapy
Diffuase toxic goitre :
In patients over 45 years, radioiodine is appropriate. In those
under 45 years, surgery for the large goitre and anti-thyroid drugs or radioiodine for
the small goitre is recommended.
Toxic nodular goitre :
Large goitres should be treated surgically because they do not
respond as well or as rapidly to radioiodine or anti-thyroid drugs as a diffuse toxic
goitre.
Toxic nodule
Surgery or radioiodine treatment is appropriate. Resection is easy, certain and
without morbidity. Radioiodine is a good alternative for those over the age of 45
years because the suppressed thyroid tissue does not take up iodine and there is thus
no risk of delayed thyroid insufficiency.
Recurrent thyrotoxicosis after surgery
In general, radioiodine is the treatment of choice, but antithyroid drugs may be used
in young women intending to have children. Further surgery has little place.
Failure of previous treatment with anti-thyroid drugs or radioiodine
In this case, surgery or thyroid ablation with 123I is appropriate.
8
Surgery for thyrotoxicosis
Preoperative preparation
Preparation is as an out-patient and only rarely is admission to hospital necessary,
because of severe symptoms at presentation, failure to control the hyperthyroidism
or non-compliance with medication. Failure to control with anti-thyroid drugs is
unusual but may be the result of uneven dosage, i.e. not taking the drug at 6- or 8-
hourly intervals.
Propranolol or nadolol controls symptoms very rapidly and has additional value in
combination with carbimazole in the immediate treatment of patients with very
severe hyperthyroidism.
Preoperative investigations to be carried out and recorded are:
1. Thyroid function tests.
2. Laryngoscopy. Whether this is routine is a matter for local protocols because every
RLN must be routinely and obsessionally preserved.
3. Thyroid antibodies.
4. Serum calcium estimation.
5. An isotope scan before preoperative preparation in toxic nodular goitre if total
thyroidectomy is not planned.
Postoperative complications
1) Haemorrhage A tension haematoma deep to the cervical fascia is usually due to
reactionary haemorrhage from one of the thyroid arteries; occasionally,
haemorrhage from a thyroid remnant or a thyroid vein may be responsible.
2) Respiratory obstruction This is very rarely due to collapse or kinking of the
trachea (tracheomalacia). Most cases are caused by laryngeal oedema.
3) Recurrent laryngeal nerve paralysis and voice change RLN injury may be unilateral
or bilateral, transient or permanent.
4) Thyroid insufficiency Following subtotal thyroidectomy this usually occurs within
2 years;
5) Parathyroid insufficiency This is due to removal of the parathyroid glands or to
infarction through damage to the parathyroid end artery; often, both factors occur
together.
6) Thyrotoxic crisis (storm) This is an acute exacerbation of hyperthyroidism.
9
7) Wound infection Cellulitis requiring prescription of antibiotics,
8) Hypertrophic or keloid scar This is more likely to form if the incision overlies the
sternum and in dark-skinned individuals.
9) Stitch granuloma This may occur with or without sinus formation and is seen after
the use of non-absorbable, particularly silk, suture material.
