
breast
COMPARATIVE AND SURGICAL ANATOMY
* overlying the second to the sixth ribs and extending from the lateral border
of the sternum to the anterior axillary line.
The axillary tail
of the breast is of surgical importance. In some normal
subjects it is palpable and, in a few, it can be seen premenstrually or during
lactation. A well-developed axillary tail is sometimes mistaken for a mass of
enlarged lymph nodes or a lipoma.
The
ligaments of Cooper
are hollow conical projections of fibrous tissue filled
with breast tissue; the apices of the cones are attached firmly to the
superficial fascia and thereby to the skin overlying the breast. These ligaments
account for the dimpling of the skin overlying a carcinoma.
The areola contains
involuntary muscle arranged in concentric rings as well as
radially in the subcutaneous tissue.
The nipple
is covered by thick skin with corrugations.
The
lymphatics
of the breast drain predominantly into the axillary
and internal mammary lymph nodes.
The axillary nodes receive approximately 85% of the drainage and are
arranged in the following groups:
• lateral
, along the axillary vein;
• anterior,
along the lateral thoracic vessels;
• posterior
, along the subscapular vessels;
• central,
embedded in fat in the centre of the axilla;
• interpectoral
, a few nodes lying between the pectoralis major and minor
muscles;
• apical
, which lie above the level of the pectoralis minor tendon in continuity
with the lateral nodes and which receive the efferents of all the other
groups.

INVESTIGATION
Mammography
; Soft tissue radiographs ,It is a very safe investigation.
( normal mammogram does not exclude the presence of carcinoma).
Ultrasound
; It is particularly useful in young women with dense breasts in
whom mammograms are difficult to interpret, and in distinguishing cysts
from solid lesions .
It can also be used to localise impalpable areas of breast pathology.
(guided percutaneous biopsy of any suspicious glands may be performed).
Magnetic resonance imaging (MRI)
• It can be useful to distinguish scar from recurrence in women who have had
previous breast conservation therapy for cancer.
• It is the best imaging modality for the breasts of women with implants.
• It has proven to be useful as a screening tool in high-risk women (positive
family history).
• It is less useful than ultrasound in the management of the axilla in both
primary breast cancer and recurrent disease .
Needle biopsy/cytology;
Cytology is obtained using a 21G or 23G needle and
10-ml syringe with multiple
passes through the lump with negative pressure in the syringe.
Fine-needle aspiration cytology (FNAC)
is the least invasive technique of
obtaining a cell diagnosis and is rapid and very accurate if both operator and
cytologist are experienced.
Large-needle biopsy with vacuum systems*
using 8G or 11G needles allows
more extensive biopsies to be taken. This is useful in the management of
microcalcifications or in the complete excision of benign lesions such as
fibroadenomas.
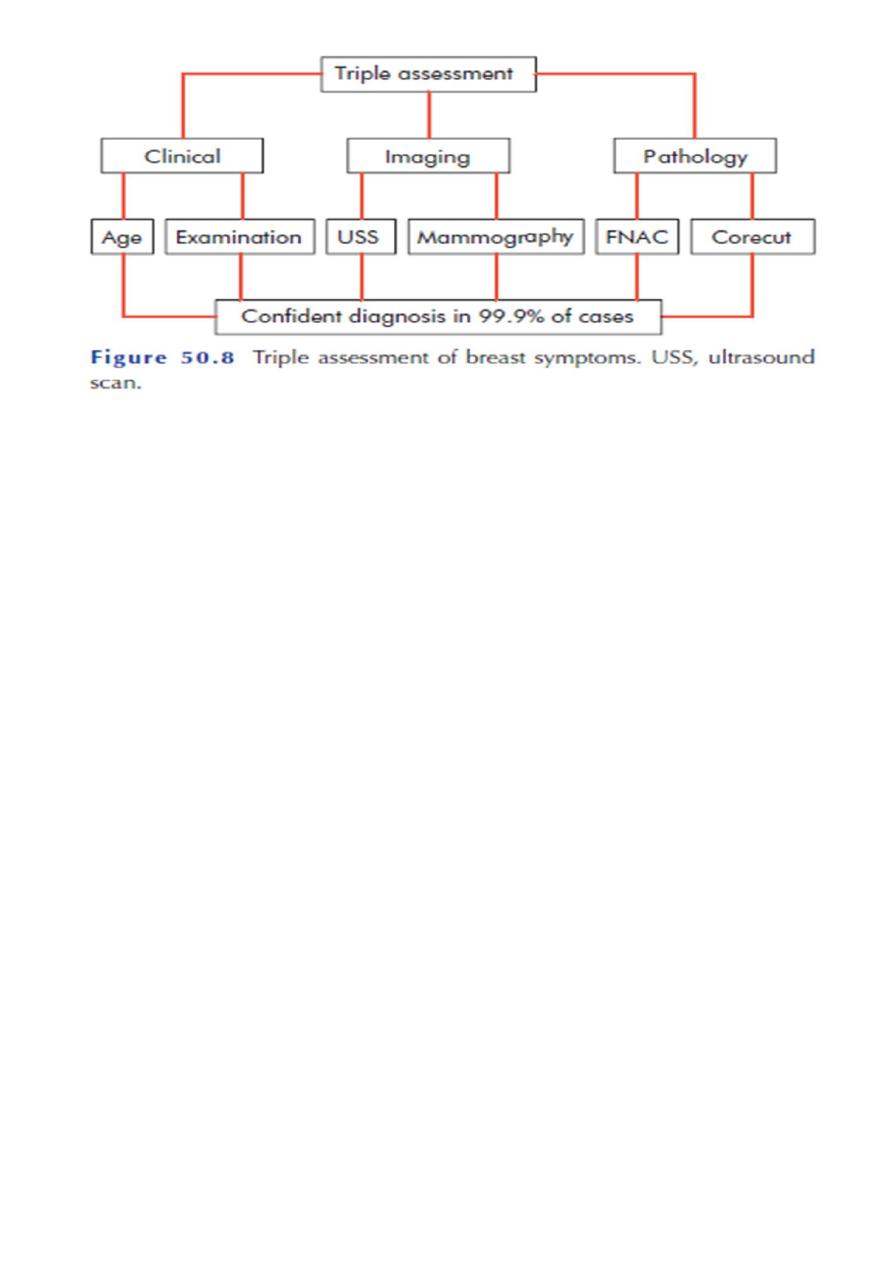
Triple assessment
*clinical assessment, radiological imaging and a tissue sample taken for either
cytological or histological analysis .
The positive predictive value (PPV) of this combination should exceed 99.9%.
THE NIPPLE
Amazia(congenital absence of the breast).
Supernumerary nipples not uncommonly occur along a Line extending from
the
anterior fold of the axilla to the fold of the groin.
Nipple retraction;-
This may occur at puberty or later in life.
*at puberty, also known as simple nipple inversion, is of Unknown aetiology .
In about 25% of cases it is bilateral.
It may cause problems with breast-feeding and infection can occur, especially
during lactation, because of retention of secretions.
Recent retraction of the nipple may be of considerable pathological
significance.
A slit-like retraction of the nipple may be caused by duct ectasia and chronic
periductal mastitis , but circumferential retraction, with or without an
underlying lump, may well indicate an underlying carcinoma.
Treatment
Treatment is usually unnecessary and the condition may Spontaneously
resolve during pregnancy or lactation.
Simple cosmetic surgery can produce an adequate correction but has the
drawback of dividing the underlying ducts.
Mechanical suction devices have been used to evert the nipple, with some
effect.

Cracked nipple
This may occur during lactation and be the forerunner of acute infective
mastitis.
If the nipple becomes cracked during lactation, it should be rested for 24–48
hours and
the breast should be emptied with a breast pump. Feeding should be resumed
as soon as possible.
Papilloma of the nipple
It has the same features as any cutaneous papilloma and should be excised with
a tiny disc of skin.
Retention cyst of a gland of Montgomery
These glands, situated in the areola, secrete sebum and if they become blocked
a sebaceous cyst forms.
Eczema
of the nipples is a rare condition and is often bilateral; it is usually
associated
with eczema elsewhere on the body. It is treated with 0.5% hydrocortisone .
Paget’s disease
of the nipple must be distinguished from eczema.
The former is caused by malignant cells in the subdermal layer.
Eczema tends to occur in younger people who have signs of eczema elsewhere
(look at the antecubital fossae).
Discharges from the nipple
Cytology may reveal malignant cells but a negative result does not
exclude a carcinoma.
Discharge from the surface
■ Paget’s disease ■ Skin diseases (eczema, psoriasis) ■ Rare causes
(e.g. chancre)
Discharge from a single duct
Blood-stained:■ Intraduct papilloma ■ Intraduct carcinoma ■ Duct ectasia
Serous (any colour):■ Fibrocystic disease■ Duct ectasia■
Carcinoma
Discharge from more than one duct
Blood-stained:■ Carcinoma■ Ectasia■
Fibrocystic disease
Black or green:■ Duct ectasia
Purulent:■ Infection
Serous:■ Fibrocystic disease■ Duct ectasia■
Carcinoma
Milk:■ Lactation■ Rare causes (hypothyroidism, pituitary tumour)

Treatment
1-Treatment must firstly be to exclude a carcinoma by occult blood test
and cytology.
2-Simple reassurance may then be sufficient but,
3-if the discharge is proving intolerable, an operation to remove the
affected duct or ducts can be performed.
Procedures;-
*Microdochectomy
*Ductoscopy (inspection of the internal structure of the duct system)
*Cone excision of the major ducts.
BENIGN BREAST DISEASE
The most common symptoms are pain, lumpiness or a lump.
The aim of treatment is to exclude cancer .
Congenital abnormalities
Amazia
;-Congenital absence of the breast may occur on one or both sides.
It is sometimes associated with absence of the sternal portion of the pectoralis
major
(Poland’s syndrome). It is more common in males.
Polymazia
;-Accessory breasts have been recorded in the axilla, groin, buttock
and thigh.
Mastitis of infants
Mastitis of infants is at least as common in boys as in girls. On the third or fourth
day of life,
This is popularly known as ‘witch’s milk’ It is caused by stimulation of the fetal
breast by
prolactin in response to the drop in maternal oestrogens and is essentially
physiological.
True mastitis is uncommon and is predominately caused by Staphylococcus
aureus.

Diffuse hypertrophy
Can occurs sporadically in otherwise healthy girls at puberty (benign virginal
hypertrophy)
and, much less often, during the first pregnancy.
the condition is rarely unilateral.
This tremendous overgrowth is apparently caused by an alteration in the normal
sensitivity of the
breast to oestrogenic hormones and some success in treating it with anti-
oestrogens has been reported.
Treatment is by reduction mammoplasty.
Injuries of the breast
Haematoma
It gives rise to a lump, which, in the absence of overlying bruising, is difficult to
diagnose correctly unless it is biopsied.
Traumatic fat necrosis
It may be acute or chronic and usually occurs in stout, middle-aged women.
Following a blow, or even indirect violence (e.g. contraction of the pectoralis
major), a lump, often painless, appears.
This may mimic a carcinoma, even displaying skin tethering and nipple
retraction, and biopsy is required for diagnosis.
A history of trauma is not diagnostic as this may merely have drawn the
patient’s attention to a pre-existing lump.
A seatbelt may transect the breast with a sudden deceleration injury, as in a
road traffic accident.
Acute and sub acute inflammations of the breast
Bacterial mastitis
It is associated with lactation in the majority of cases. Most cases are caused by
Staphylococcus aureus and, if hospital acquired, are likely to be penicillin
resistant.
Although ascending infection from a sore and cracked nipple may initiate the
mastitis,
Clinical features=classical signs of acute inflammation.
Early on this is a generalized cellulitis but later an abscess will form.

Treatment
1- cellulitic stage the patient should be treated with an appropriate antibiotic,
for example flucloxacillin or co-amoxiclav.
Feeding from the affected side may continue if the patient can manage.
Support of the breast, local heat and analgesia will help to relieve pain.
2-If an antibiotic is used in the presence of undrained pus, an
‘antibioma
’ may
form.
This is a large, sterile, brawny oedematous swelling that takes many weeks to
resolve.
It used to be recommended that the breast should be incised and drained if the
infection
did not resolve within 48 hours or if after being emptied of milk there was an
area of tense
Induration or other evidence of an underlying abscess.
Chronic intramammary abscess
It may follow inadequate drainage or injudicious antibiotic treatment,*the
condition cannot be distinguished from a carcinoma without the histological
evidence from a biopsy.
Tuberculosis of the breast
*is comparatively rare, is usually associated with active pulmonary tuberculosis
or
tuberculous cervical adenitis.
* occurs more often in parous women and usually presents with multiple
chronic
abscesses and sinuses and a typical bluish, attenuated appearance of the
surrounding skin.
diagnosis = bacteriological and histological examination.
Treatment is with anti-tuberculous chemotherapy.
* mastectomy should be restricted to patients with persistent residual infection.
Actinomycosis
; The lesions present the essential characteristics of faciocervical
actinomycosis.
Mondor’s disease
= thrombophlebitis of the superficial veins of the breast and
anterior chest wall . The pathognomonic feature is a thrombosed
subcutaneous cord, usually attached to the skin.

The differential diagnosis is lymphatic permeation from an occult carcinoma of
the breast. The only treatment required is restricted arm movements and, in
any case, the condition subsides within a few months without recurrence,
complications or deformity.
Duct ectasia/periductal mastitis
*the disease is much more common in smokers.
It is a dilatation in one or more of the larger lactiferous ducts, which fill with a
stagnant brown or green
secretion. This may discharge. These fluids then set up an irritant reaction in
surrounding tissue leading
to periductal mastitis or even abscess and fistula formation.
In some cases, a chronic indurated mass forms beneath the areola, which
mimics a carcinoma.
Clinical features
1-Nipple discharge (of any colour),
2-a subareolar mass, abscess, mammary duct fistula and/or nipple retraction .
Treatment
carcinoma must be excluded by obtaining a mammogram and negative cytology
or histology.
If any suspicion remains the mass should be excised.
Antibiotic therapy may be tried, the most appropriate agents being co-amoxiclav
or flucloxacillin and metronidazole.
*surgery is consists of excision of all of the major ducts. It is particularly
important to shave the back of
the nipple to ensure that all terminal ducts are removed. Failure to do so will
lead to recurrence.
Aberrations of normal development and Involution (ANDI)
Aetiology; The pathogenesis of ANDI involves disturbances in the breast
physiology extending
from a Perturbation of normality to well-defined disease processes.
Pathology; four features that may vary in extent and degree in any one breast.
1• Cyst formation. Cysts are almost inevitable and very variable in size.

2• Fibrosis. Fat and elastic tissues disappear and are replaced with dense white
fibrous trabeculae.
The interstitial tissue is infiltrated with chronic inflammatory cells.
3• Hyperplasia of epithelium in the lining of the ducts and acini may occur, with
or without atypia.
5• Papillomatosis. The epithelial hyperplasia may be so extensive that it results
in papillomatous overgrowth within the ducts.
Clinical features; The symptoms include an area of lumpiness (seldom discrete)
and/or breast pain (mastalgia
). About 5% of breast cancers exhibit pain
at presentation.
1• A benign discrete lump is commonly a cyst or fibroadenoma. True lipomas
occur rarely.
2• Lumpiness may be bilateral, commonly in the upper outer quadrant or, less
commonly.
The changes may be cyclical, with an increase in both lumpiness and often
tenderness before a menstrual period.
3• Non-cyclical mastalgia is more common in peri-menopausal than post-
menopausal women.
It may be associated with ANDI or with periductal mastitis.
It should be distinguished from referred pain, for example a musculoskeletal
disorder.
‘Breast’ pain in post-menopausal women not taking hormone replacement
therapy (HRT) is usually derived from the chest wall.
Treatment of lumpy breasts
*mammography and/or ultrasound scanning if appropriate), then initially ;-
1- firm reassurance. (6 weeks after the initial visit).
2- multiple random biopsies because the clinician lacks the courage of his or her
convictions.
Treatment of mastalgia
1-Initially, firm reassurance that the symptoms are not associated with cancer will help
the majority of women.
In the first instance, an appropriately fitting and supportive bra should be worn
throughout the day and a soft bra (such as a sports bra) worn at night. Avoiding
caffeine drinks is said to help..
2-A patient symptom diary will help her to chart the pattern of pain throughout the
month and thus determine whether this is cyclical mastalgia.

3-Oil of evening primrose, in adequate doses given over 3 months.
4- For those with intractable symptoms, an anti-gonadotrophin, such as danazol, or a
prolactin inhibitor, such as bromocriptine, may be tried.
5-Very rarely it is necessary to prescribe an anti-oestrogen, for example Tamoxifen, or a
luteinising hormone-releasing hormone (LHRH) agonist to deprive the breast
epithelium of oestrogenic drive.
6-Ablative surgery should never be contemplated for breast pain and any patient seeking
this treatment should be referred to a psychiatrist.
*** For non-cyclical mastalgia it is important to exclude extramammary causes such as
chest wall pain.
This is common in postmenopausal women who are not on HRT and the neck and
shoulders are common sights of referred pain.
It is seldom necessary these days to carry out a biopsy on a very localized tender area that
might be harbouring a
subclinical cancer as imaging is so much better.
Treatment may be with non-steroidal analgesics or by injection with local anaesthetic on
a ‘trigger spot’.
Benign breast disorder classification
Congenital disorders;-
■
Inverted nipple
■
Supernumerary breasts/nipples
■
Non-breast disorders
■
Tietze’s disease (costochondritis)
■
Sebaceous cysts and other skin conditions Injury
Inflammation/infection
ANDI
(aberations of normal differentiation and involution):
■
Cyclical nodularity and mastalgia
■
Cysts
■
Fibroadenoma
Duct ectasia/periductal mastitis
Pregnancy-related
:■
Galactocele
■
Puerperal abscess

Breast cysts
These occur most commonly in the last decade of reproductive life as a result of
a non- integrated involution of stroma and epithelium.
They are often multiple, may be bilateral and can mimic malignancy.
Diagnosis can be confirmed by aspiration and/or ultrasound.
They typically present suddenly and cause great alarm; prompt diagnosis and
drainage provides immediate relief.
Treatment
1-A solitary cyst or small collection of cysts can be aspirated. If they resolve
completely, and if the fluid is not blood-stained, no further treatment is
required.
However, 30% will recur and require reaspiration.
Cytological examination of cyst fluid is no longer practised routinely.
2- If there is a residual lump or if the fluid is blood-stained, a core biopsy or local
excision for histological diagnosis is advisable, which is also the case if the cyst
reforms repeatedly.
This will exclude cystadenocarcinoma, which is more common in elderly women.
Galactocele
Galactocele, which is rare, usually presents as a solitary, subareolar cyst and
always
dates from lactation. It contains milk and in longstanding cases its walls tend to
calcify.

CARCINOMA OF THE BREAST
Aetiological factors
Geographical;
-Carcinoma of the breast occurs commonly in the western world.
Age;
-* extremely rare below the age of 20years, the incidence steadily rises so that
by the age of 90 years nearly 20% of women are affected.
Gender
;-Less than 0.5% of patients with breast cancer are male.
Genetic
;-It occurs more commonly in women with a family history of breast cancer.
Breast cancer related to a specific mutation accounts for about 5% .
Diet;
-There is some evidence that there is a link with diets low in phytoestrogens.
A high intake of alcohol is associated with an increased risk of developing breast
cancer.
Endocrine;-
Breast cancer is more common in nulliparous women and breastfeeding
in particular appears to be protective.
Also protective is having a first child at an early age, especially if associated with
late menarche and early menopause.
It is known that in postmenopausal women, breast cancer is more common in the
obese.
This is thought to be because of an increased conversion of steroid hormones to
oestradiol in the body fat.
Recent studies have clarified the role of exogenous hormones, in particular the oral
contraceptive pill and
HRT, in The development of breast cancer. For most women the benefits of these
treatments will far
outweigh the small Putative risk; however, long-term exposure to the combined
preparation of HRT does significantly increase the risk of developing breast
cancer.
Previous radiation;
This was considered to be of historical interest, with the
majority of women exposed to the atomic bombs at Hiroshima and
Pathology
1-Ductal carcinoma
is the most common variant with lobular carcinoma
occurring in up to 15% of cases.
2-Invasive lobular carcinoma
is commonly multifocal and/or bilateral.
3-Inflammatory carcinoma
is a fortunately rare, highly aggressive cancer that
presents as a painful, swollen breast, which is warm with cutaneous
oedema.
This is the result of blockage of the subdermal lymphatics with carcinoma cells.

Inflammatory cancer usually involves at least one-third of the breast and may
mimic
a breast abscess. A biopsy will confirm the diagnosis and show undifferentiated
carcinoma cells. It used to be rapidly fatal but with aggressive chemotherapy
and
radiotherapy and with salvage surgery the prognosis has improved
considerably.
4-In situ carcinoma is pre-invasive cancer
that has not breached the epithelial
basement membrane.
5-Staining for oestrogen and progesterone receptors
is now considered routine,
as their presence will indicate the use of adjuvant hormonal therapy with
tamoxifen or the newer aromatase inhibitors .
Paget’s disease of the nipple
It is a superficial manifestation of an underlying breast carcinoma.
It presents as an eczema-like condition of the nipple and areola, which persists
despite local treatment.
The nipple is eroded slowly and eventually disappears.
If left, the underlying carcinoma will sooner or later become clinically evident.
Nipple eczema should be biopsied if there is any doubt about its cause.
The spread of breast cancer
Local spread
The tumour increases in size and invades other portions of the breast.
It tends to involve the
skin and to penetrate the pectoral muscles and even the chest wall if
diagnosed late.
Lymphatic metastasis
1- primarily to the axillary .
2-Tumours in the posterior one third of the breast are more likely to
drain to the internal
mammary nodes.

3-Involvement of supraclavicular nodes and of any contralateral lymph
nodes represents advanced disease.
Spread by the bloodstream
It is by this route that skeletal metastases occur, although the initial
spread may be via the lymphatic system.
In order of frequency the lumbar vertebrae, femur, thoracic vertebrae,
rib and skull are affected and these deposits are generally
osteolytic.
Metastases may also commonly occur in the liver, lungs and brain and,
occasionally, the
adrenal glands and ovaries; they have, in fact, been described in most
body sites.
Clinical presentation
1-Most breast cancers will present as a hard lump, which may be
associated with indrawing
of the nipple.
2-As the disease advances locally there may be skin involvement with
peau d’orange or
3-frank ulceration and fixation to the chest wall(described as cancer-en-
cuirasse) when the disease progresses around the chest wall.
Staging of breast cancer
Classical staging of breast cancer by means of the TNM (tumour–node–
metastasis) or
UICC (Union Internationale Contre le Cancer) criteria is used less often
as we gain more
nowledge of the biological variables that affect prognosis.
management of operable breast cancer
1-Achieve local control
2-Appropriate surgery
■
Wide local excision (clear margins) and radiotherapy, or
■
Mastectomy ± radiotherapy (offer reconstruction –immediate or delayed)

■
Combined with axillary procedure (see text)
■
Await pathology and receptor measurements
■
Use risk assessment tool; stage if appropriate
3-Treat risk of systemic disease
■
Offer chemotherapy if prognostic factors poor; include Herceptin if Her-2 positive
■
Radiotherapy as decided above
■
Hormone therapy if oestrogen receptor or progesterone receptor positive
Treatment of early breast cancer
The aims of treatment are:
■ ‘Cure’
: likely in some patients but late recurrence is possible.
■
Control of local disease in the breast and axilla.
■
Conservation of local form and function.
■
Prevention or delay of the occurrence of distant metastases.
Treatment of advanced breast cancer
Management should be aimed at palliation of the symptoms and treatment of the breast
cancer,
usually by endocrine manipulation with or without radiotherapy.
Locally advanced inoperable breast cancer
Locally advanced inoperable breast cancer, including inflammatory breast cancer, is
usually treated
with systemic therapy, either chemotherapy or hormone therapy.
Occasionally, ‘toilet mastectomy’ or radiotherapy is required to control a fungating
tumour but often
incision through microscopically permeated tissues results in a worse outcome.
Metastatic carcinoma of the breast
Metastatic carcinoma of the breast will also require palliative systemic therapy to
alleviate symptoms.
Hormone manipulation is often the first-line treatment because of its minimal sideeffects.
It is particularly useful for bony metastases. However, only about 30% of these tumours
will be
hormone responsive and, unfortunately, in time even these will become resistant to
treatment.
Cytotoxic therapy is used particularly in younger women or those with visceral metastases
and rapidly growing tumours.
Local treatment may also prove useful for some metastatic disease such as radiotherapy
for painful bony deposits
And internal fixation of pathological fractures.

Surgery;-
Mastectomy is indicated for;-
1- large tumours (in relation to the size of the breast),
2-central tumours beneath or involving the nipple,
3- multifocal disease,
4-local recurrence or patient preference.
Procedures ;-
1-The radical Halsted mastectomy
, which included excision of the breast,
axillary lymph
nodes and pectoralis major and minor muscles, is no longer indicated as it
causes excessive
Morbidity with no survival benefit.
2-The modified radical (Patey) mastectomy -
excised mass is composed of:
• the whole breast;
• a large portion of skin, the centre of which overlies the tumour but
which always includes the nipple;
• all of the fat, fascia and lymph nodes of the axilla.
is more commonly performed .
3-Simple mastectomy
involves removal of only the breast with no
dissection of the axilla,
except for the region of the axillary tail of the breast, which usually has
attached to it a few
nodes low in the anterior group.
Conservative breast cancer surgery
This is aimed at removing the tumour plus a rim of at least 1 cm of
normal breast tissue.
1- wide local excision.
2- lumpectomy should be reserved for an operation in which a benign
tumour is
excised and in which a large amount of normal breast tissue is not
resected.

3-A quadrantectomy involves removing the entire segment of the
breast that contains the
tumour.
Both of these operations are usually combined with axillary surgery,
usually via a separate
incision in the axilla.
The role of axillary surgery is to stage the patient and to treat the axilla.
The presence of metastatic disease within the axillary lymph nodes
remains the best single marker for prognosis;
Sentinel node biopsy
This technique is currently becoming the standard of care in the
management of the axilla
in patients with clinically node-negative disease.
Radiotherapy;- used
to the chest wall after mastectomy is indicated in
selected patients in whom the risks of local recurrence are high.
This includes patients with large tumours and those with large numbers
of positive nodes or extensive lymphovascular invasion.
Adjuvant systemic therapy;-
Over the last 25 years there has been a
revolution in our understanding of the biological nature of
carcinoma of the breast.
It is now widely accepted that the outcomes of treatment are
predetermined by the extent
of micrometastatic disease at the time of diagnosis.
Hormone therapy;-
Tamoxifen has been the most widely used
‘hormonal’ treatment in breast cancer.
The beneficial effects of tamoxifen in reducing the risk of tumours in
the contralateral breast have also been observed, as has its role as
a preventative agent .
Chemotherapy;-
Chemotherapy using a first-generation regimen such
as a 6-monthly cycle of cyclophosphamide,Methotrexate and 5-

fluorouracil (CMF) will achieve a 25% reduction in the risk of relapse
over a 10- to 15-year period.
Follow-up of breast cancer;-
Patients with breast cancer used to be
followed for life to detect recurrence and dissemination.
It is current practice to arrange yearly or 2-yearly mammography of the
treated
and contralateral breast.
Phenomena resulting from lymphatic obstruction in advanced breast
cancer
Peau d’orange;-
Peau d’orange is caused by cutaneous lymphatic oedema.
Where the infiltrated
skin is tethered by the sweat ducts it cannot swell, leading to an
appearance like orange skin.
Occasionally, the same phenomenon is seen over a chronic abscess.
Late oedema of the arm is a troublesome complication of breast cancer
treatment, fortunately seen less often now that radical axillary
dissection and radiotherapy are rarely combined.
This neoplastic infiltration is often painful because of brachial plexus nerve
involvement.
An oedematous limb is susceptible to bacterial infections following quite
minor trauma and these require vigorous antibiotic treatment.
Treatment of late oedema is difficult but limb elevation, elastic arm
stockings and pneumatic compression devices can be useful.
Cancer-en-cuirasse;-
The skin of the chest is infiltrated with carcinoma and
has been likened to a
coat. It may be associated with a grossly swollen arm. This usually occurs in
cases with local
recurrence after mastectomy and is occasionally seen to follow the
distribution of irradiation to the chest wall. The condition may respond
to palliative systemic treatment but prognosis in terms of survival is
poor.

Lymphangiosarcoma;-
Lymphangiosarcoma is a rare complication of
lymphoedema with an onset many years after the original treatment. It
takes the form of multiple subcutaneous nodules in the upper limb and
must be distinguished from recurrent carcinoma of the breast.
The prognosis is poor but some cases respond to cytotoxic therapy or
irradiation.
Interscapulothoracic (forequarter) amputation is rarely indicated.
Pregnancy
*in a similar way to breast cancer in a nonpregnant young woman and should
be treated accordingly.
*radiotherapy should be avoided during pregnancy, making
*mastectomy a more frequent option than breast conservation surgery;
* chemotherapy should be avoided during the first trimester but appears safe
subsequently;
*most tumours are hormone receptor negative and so hormone treatment,
which is potentially teratogenic, is not required.
* women are usually advised to wait at least 2 years as it is within this time
that
recurrence most often occurs.
*The risk of developing breast cancer with oral contraceptive use is only slight,
and disappears 10 years after stopping the oral contraceptive pill.
THE MALE BREAST
Gynaecomastia –causes ;-
1-Idiopathic;-Hypertrophy of the male breast may be unilateral or bilateral.
The breasts enlarge at puberty and sometimes present the characteristics of
female breasts .
2-Hormonal;-
* It may also occur as a result of a teratoma of the testis, in anorchism and after
castration.
* ectopic hormonal production in bronchial carcinoma and in adrenal and
pituitary disease.
*Body builders may use steroids to improve their physique, which may cause
gynaecomastia.

3-Associated with leprosy; This is possibly because of bilateral testicular
atrophy.
4-Associated with liver failure; occurs in patients with cirrhosis as a result of
failure of the liver to metabolise oestrogens.
It is also seen with certain drugs such as cimetidine, digitalis and spironolactone.
5-Associated with Klinefelter syndrome; - a sex chromosome anomaly having
47XXY trisomy.
Treatment
1-Provided that the patient is healthy and comparatively young, reassurance
may be sufficient.
2- If not, mastectomy with preservation of the areola and nipple can be
performed.
The patient must be warned about the side-effects of this procedure, which are
common and a cause of many medico-legal complaints in the UK.
Carcinoma of the male breast
The known predisposing causes include gynaecomastia and excess endogenous
or
exogenous oestrogen. As in the female it tends to present as a lump and is
most commonly an infiltrating ductal carcinoma.
Treatment;-Adequate local excision, because of the small size of the breast,
should always be with a ‘mastectomy’.
OTHER TUMOURS OF THE BREAST
Lipoma ;-A true lipoma is very rare.
Sarcoma of the breast;- Sarcoma tends to occur in younger women between the
ages of 30 and 40 years.
Treatment is by simple mastectomy followed by radiotherapy.
Metastases
On rare occasions cancer elsewhere may present with a metastasis in the breast.
The breast is also occasionally infiltrated by Hodgkin’s disease and other
lymphomas.
