PERITONITIS
Bacterial peritonitis is usually polymicrobial,( both aerobic and anaerobic organisms ).
The exception is primary peritonitis (‘spontaneous’ peritonitis), in which a pure
infection with streptococcal, pneumococcal or Haemophilus bacteria occurs.
Paths to peritoneal infection
1- Gastrointestinal perforation, e.g. perforated ulcer, diverticular perforation.
2-Non-gastrointestinal causes of peritonitis
*Pelvic infection via the fallopian tubes
•
Immunodeficient patients, for example those with human immunodeficiency
virus (HIV) infection or those on immunosuppressive treatment, may present
with opportunistic peritoneal infection, e.g. Mycobacterium avium-intracellulare
(MAI).
A- Exogenous contamination, e.g. drains, open surgery, trauma
B- Transmural bacterial translocation (no perforation), e.g. inflammatory bowel
disease, appendicitis, ischaemic bowel
C- Female genital tract infection, e.g. pelvic inflammatory disease
D- Haematogenous spread (rare), e.g. septicaemia.
Mortality of patient with peritonitis depend on;-
1• the degree and duration of peritoneal contamination
2• the age of the patient
3• the general health of the patient
4• the nature of the underlying cause
.

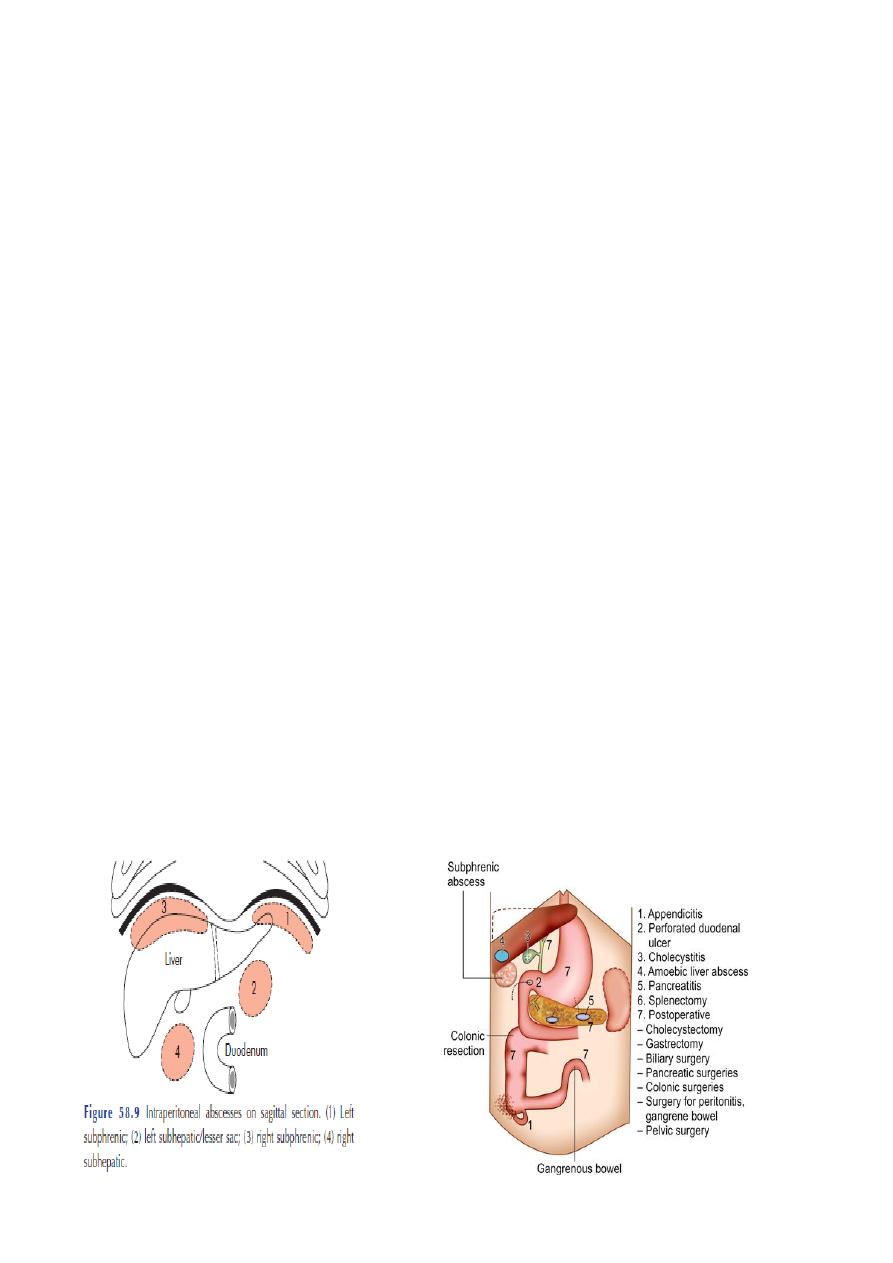
Localized peritonitis
Anatomical;-
The greater sac of the peritoneum is divided into
(1) the subphrenic spaces,
(2) the pelvis.
(3) the peritoneal cavity proper. (supracolic and an infracolic compartment by the
transverse colon and transverse mesocolon ,which deters the spread of infection from
one to the other.
Pathological
1-Inflamed peritoneum loses its glistening appearance and becomes reddened and
velvety.
2-Flakes of fibrin appear and cause loops of intestine to become adherent to one
another and to the parietes.
3-There is an outpouring of serous inflammatory exudate rich in leucocytes and plasma
proteins that soon becomes turbid; if localisation occurs, the turbid fluid becomes frank
pus.
4- Peristalsis is retarded in affected bowel and this helps to prevent distribution of the
infection.
5-The greater omentum, by enveloping and becoming adherent to inflamed structures,
often forms a substantial barrier to the spread of infection.
Surgical
Drains are frequently placed during operation to assist localization (and exit) of intra-
abdominal collections:. They may act as conduits for exogenous infection.
Diffuse peritonitis
A number of factors may favour the development of diffuse peritonitis:
1• Speed of peritoneal contamination is a prime factor.
If an inflamed appendix or other hollow viscus perforates before localisation has taken
place, there is a gush of
contents into the peritoneal cavity, which may spread over a large area almost
instantaneously.
2-• Stimulation of peristalsis by the ingestion of food or even water hinders localisation.
3• The virulence of the infecting organism.
4-• Young children have a small omentum, which is less effective in localising infection.
5-• Disruption of localized collections may occur with injudicious handling, e.g. appendix
mass or pericolic abscess.

6• Deficient natural resistance (‘immune deficiency’) may result from use of drugs (e.g.
steroids), disease [e.g. acquired immune deficiency syndrome (AIDS)] or old age.
Clinical features in peritonitis
1■ Abdominal pain, worse on movement
2■ Guarding/rigidity of abdominal wall
3■ Pain/tenderness on rectal/vaginal examination (pelvic peritonitis)
4■ Pyrexia (may be absent)
5■ Raised pulse rate
6■ Absent or reduced bowel sounds
7■ ‘Septic shock’ [systemic inflammatory response syndrome (SIRS)] in later stages
(Investigations in peritonitis)-
1• A radiograph of the abdomen may confirm the presence of dilated gas-filled loops of
bowel (consistent with a paralytic ileus) or show free gas, although the latter is best
shown on an erect chest radiograph .
2 • Serum amylase estimation may establish the diagnosis of acute pancreatitis, * Serum
amylase > 4× normal indicates acute pancreatitis.it can be also elevated in e.g.
perforated duodenal ulcer.
3• Ultrasound and computerised tomography (CT) scanning are increasingly used to
identify the cause of peritonitis.
4• Peritoneal diagnostic aspiration (with or without ultrasound guidance) .
*Bile-stained fluid indicates a perforated peptic ulcer or gall bladder; the presence of
pus indicates bacterial peritonitis.
Blood is aspirated in a high proportion of patients with intraperitoneal bleeding
5- Raised white cell count and C-reactive protein.
Management of peritonitis
1-General care of patient:
■ Correction of fluid and electrolyte imbalance
■ Insertion of nasogastric drainage tube
■ Broad-spectrum antibiotic therapy
■ Analgesia
■ Vital system support
2-Operative treatment
of cause when appropriat (perforated appendix with peritoneal
debridement/lavage. (Peritoneal lavage all seropurulent exudate is removed. The use of
a large
volume of saline (1–2 litres) containing dissolved antibiotic (e.g. tetracycline)
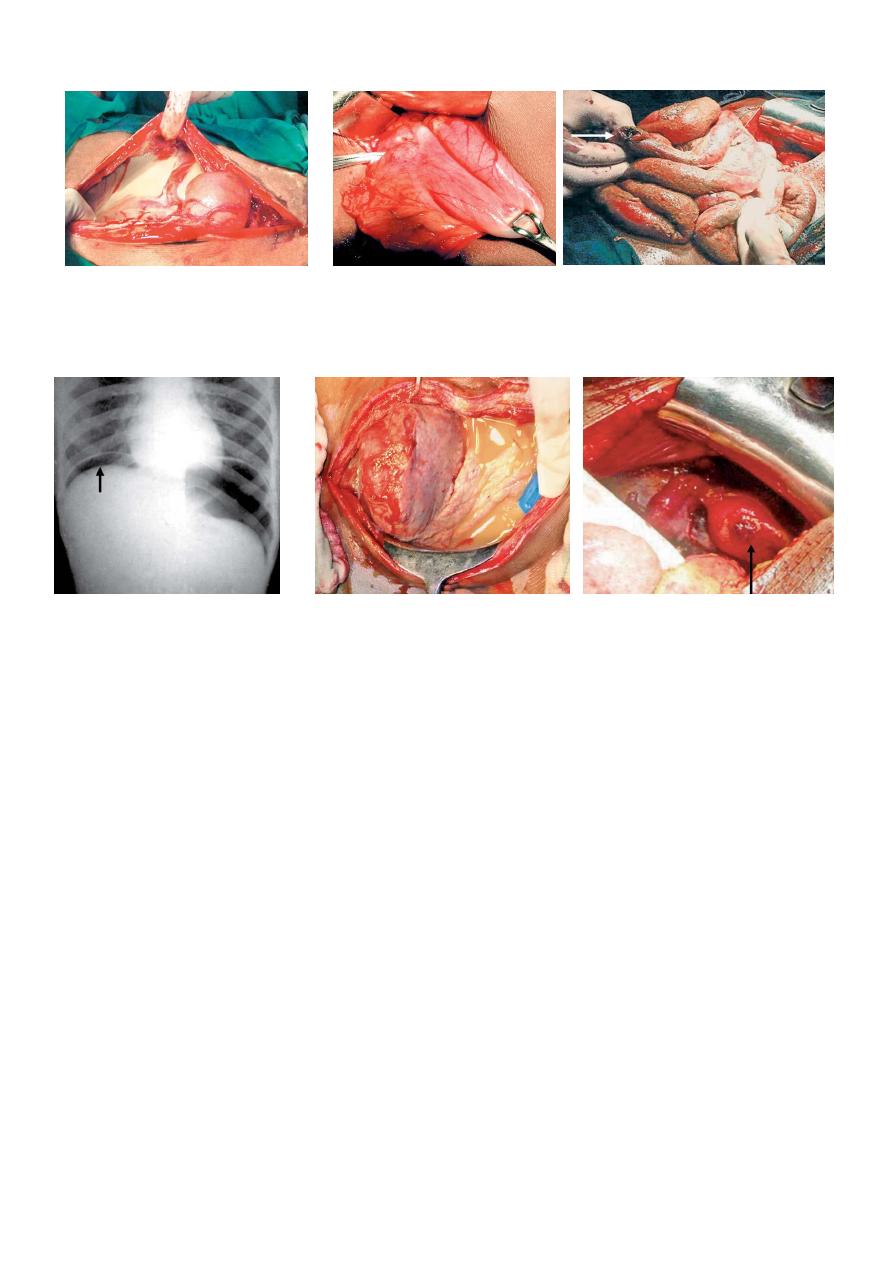
On table finding in a case of peritonitis, Duodenal ulcer perforation Ileal perforation with severe peritonitis.
where the peritoneal cavity is filled with causing peritonitis
pus
Plain X-ray abdomen showing gas Severe peritonitis showing pus in the Perforation in the fundus of the
under diaphragm.Perforation is peritoneal cavity. Uterus due to the attemoted abortion
the most common cause of it caused severe peritonitis
peritonitiS
Clinical features of an abdominal/pelvic abscess
Abscess formation following local or diffuse peritonitis .
The symptoms and signs
of a purulent collection may be vague and consist of
1-lassitude, malaise.
2- Anorexia and weight loss anorexia.
2- Swinging Pyrexia, Sweats with or without rigors.
3-tachycardia.
4-leucocytosis, raised C-reactive protein.
5- Localised abdominal tenderness (with or without mass) also common.
6- Abdominal/pelvic (with or without shoulder tip) pain.
7- Symptoms from local irritation, e.g. hiccoughs (subphrenic), diarrhoea and mucus
(pelvic)

complications of peritonitis
Systemic;-
■ shock (Bacteraemic/endotoxic).
■ Bronchopneumonia/respiratory failure.
■ Renal failure.
■ Bone marrow suppression(sepsis….
■ Multisystem failure.
Abdominal complications of peritonitis; -
■ Paralytic ileus
■ Adhesional small bowel obstruction
■ Residual or recurrent abscess
■ Portal pyaemia/liver abscess
Pelvic abscess
Causes;-
1-The pelvis is the commonest site of an intraperitoneal abscess because the vermiform
appendix is often pelvic in position and the fallopian tubes are frequent sites of
infection.
2-A pelvic abscess can also occur as a sequel to any case of diffuse peritonitis and is
common after anastomotic leakage following colorectal surgery.
Clinical features;-
3-The most characteristic symptoms are diarrhea and the passage of mucus in the
stools.
4- Rectal examination reveals a bulging of the anterior rectal wall, which, when the
abscess is ripe, becomes softly cystic.
Treatment ;-
1- conservative- (antibiotic ,rest…. a proportion of these abscesses Burst into the
rectum, after which the patient nearly always recovers rapidly.
2-If this does not occur, the abscess should be drained deliberately.
*In women, vaginal drainage through the posterior fornix is often chosen.
In other cases, when the abscess is definitely pointing into the rectum, rectal drainage
is employed.
If any uncertainty exists, the presence of pus should be confirmed by ultrasound or
CT scanning
with needle aspiration if indicated.

**** Laparotomy is almost never necessary.
Rectal drainage of a pelvic abscess is far preferable to suprapubic drainage, which
risks exposing the
general peritoneal cavity to infection.
Drainage tubes can also be inserted percutaneously or Via the vagina or rectum under
ultrasound or CT guidance
SUBPHRENIC SPACES AND SUBPHRENIC ABSCESS
Clinical Features;- “Pus somewhere, pus nowhere else, pus under diaphragm”.
History relevant of the specific causes; history of any previous surgery:
*Fever with chills and rigors.
*Pain in right hypochondrium, epigastrium or lower thorax.
*Tenderness in right hypochondrium.
*Sympathetic right sided pleural effusion due to congestion and hyperaemia of the
diaphragm.
*Collapse of the lung/basal atelectasis—right side may be evident.
*Tachypnoea and respiratory distress can be observed.
*Pain in the right shoulder due to irritation of phrenic nerve.
* Hiccough, tachycardia.
*Hoover’s sign: Scoliosis towards same side in subphrenic abscess.
*Wasting and anorexia is common.
*Occasionally tender mass in the right hypochondrium may be palpable.
*Tenderness over 11th intercostal space may be evident in right subhepatic space
abscess.
Differential diagnosis;
*Amoebic liver abscess
*Pylephlebitis
*Empyema
*Pulmonary collapse
Investigations;-
Plain X-ray chest and abdomen shows soft tissue shadow, pleural
effusion, tenting of diaphragm, collapse of the lung. * U/S abdomen confirms the
diagnosis. *CT scan is very useful .

Treatment ;-
1-Antibiotics: Ampicillin, metronidazole, gentamicin, cephalosporins.
2- Percutaneous drainage: Initially ultrasound guided aspiration( under ultrasound or
CT guidance)
Open drainage is indicated:
1-When symptoms persist
2-When abscess increases in size
3- When there is thick pus or multiloculated pus or multiple abscesses
4- Failure of/contraindications for catheter drainage
5-Multiple abscesses
6- Presence of foreign body/necrosis/haematoma/obstruction/ fistula
SPECIAL FORMS OF PERITONITIS
Postoperative peritonitis
1-The patient is ill with raised pulse and peripheral circulatory failure.
2-Local symptoms and signs are less definite.
3-Abdominal pain may not be prominent and is often difficult to assess because of
normal wound pain and postoperative analgesia.
treatment ;-
1-Antibiotic therapy alone is inadequate;
2-surgical operation.
PERITONITIS In patients on treatment with steroids;-
1-Pain is frequently slight or absent.
2-Physical signs are similarly vague and misleading.
PERITONITIS In children
The diagnosis can be more difficult, particularly in the preschool child .
Physical signs should be elicited by a gentle, patient and sympathetic approach.
PERITONITIS In patients with dementia
Such patients can be fractious and unable to give a reliable history.
Abdominal tenderness is usually well localised, but guarding and rigidity are less
marked because the abdominal muscles are often thin and weak.

Bile peritonitis;-
Causes of bile peritonitis
1■ Perforated cholecystitis
2■ Post cholecystectomy:
*Cystic duct stump leakage
*Leakage from an accessory duct in the gall bladder bed
*Bile duct injury
*T-tube drain dislodgement (or tract rupture on removal)
3■ Following other operations/procedures:
*Leaking duodenal stump post gastrectomy
*Leaking biliary–enteric anastomosis
*Leakage around percutaneous placed biliary drains
4■ Following liver trauma
Tuberculous peritonitis
■ it can be Acute and chronic forms.
Clinical features;-
1-■ Abdominal pain, sweats, malaise and weight loss are frequent.
2■ Caseating peritoneal nodules are common .
3■ Ascites common, may be loculated
4■ Intestinal obstruction .
Origin of the infection
1• tuberculous mesenteric lymph nodes
2• tuberculosis of the ileocaecal region
3• a tuberculous pyosalpinx
4• blood-borne infection from pulmonary tuberculosis, usually the ‘miliary.
Varieties of tuberculous peritonitis;-
There are four varieties
1- ascitic, 2-encysted, 3- fibrous 4- purulent.

NEOPLASMS OF THE PERITONEUM
Carcinoma peritonei
The main forms of peritoneal metastases are:
• discrete nodules – by far the most common variety
• plaques varying in size and colour
• diffuse adhesions – this form occurs at a late stage of the disease and gives rise,
sometimes, to a ‘frozen pelvis’.
Differential diagnosis
1- tuberculous peritonitis are greyish and translucent .
2- Fat necrosis can usually be distinguished from a carcinomatous nodule by its
opacity.
3-Peritoneal hydatids can also simulate malignant disease after rupture of a hydatid
cyst, with seeding of daughter cysts.
Treatment
1-Ascites by systemic or intraperitoneal chemotherapy.
2- endocrine therapy in the case of hormone receptor-positive tumours.
Pseudomyxoma peritonei
1-This rare condition occurs more frequently in women.
2-The abdomen is filled with a yellow jelly, large quantities of which are often
encysted.
3-it is associated with mucinous cystic tumours of the ovary and appendix.
4-It is often painless and there is frequently no impairment of general health.
5-it does not give rise to extraperitoneal metastases.
diagnosis is more often suggested by;-
1-ultrasound and CT scanning .
2-made at operation.
Treatment ;-
1- At laparotomy, masses of jelly are scooped out.
2-The appendix, if present, should be excised together with any ovarian tumour.
3- recurrence is inevitable.
4-patients may gain symptomatic benefit from repeated ‘debulking’ surgery.
5-Occasionally, the condition responds to radioactive isotopes or intraperitoneal
chemotherapy.

Mesenteric cysts
Mesenteric cysts are classified as:
• chylolymphatic
• simple (mesothelial)
• enterogenous;
• urogenital remnant
• dermoid (teratomatous cyst).
Clinical features of a mesenteric cyst
1-• A painless abdominal swelling.
2-• Recurrent attacks of abdominal pain with or without vomiting.
3-• An acute abdominal catastrophe, which arises as a result of:
– torsion of that portion of the mesentery containing the cyst;
– rupture of the cyst, often as a result of a comparatively trivial accident;
– haemorrhage into the cyst;
– infection.
Diagnosis;-
1-Ultrasound and CT scanning .
2-A barium meal and follow-through may show displacement of the hollow viscera
around the cyst .
Treatment;-
1-Many chylolymphatic cysts can be enucleated in toto.
2- Aspiration of the contents of the cyst.
