“Clinical ophthalmology”
Alkindy college of medicine
Fifth year
2015 - 2016
Mostafa Hatim
List of contents
Slide number
Introduction
3
The Orbit
19
The Lacrimal apparatus
33
Eyelid
46
Conjunctiva
64
Sclera & Episclera
99
Cornea
109
Uveal tract (Iris, Ciliary body and choroid)
131
Lens
139
Raised intraocular pressure (IOP)
156
Refractive error (Ametropia)
171
Retina
180
Neuro-ophthalmology
204
Squint
217
Eye trauma
227
Differential diagnosis
252
“Introduction”
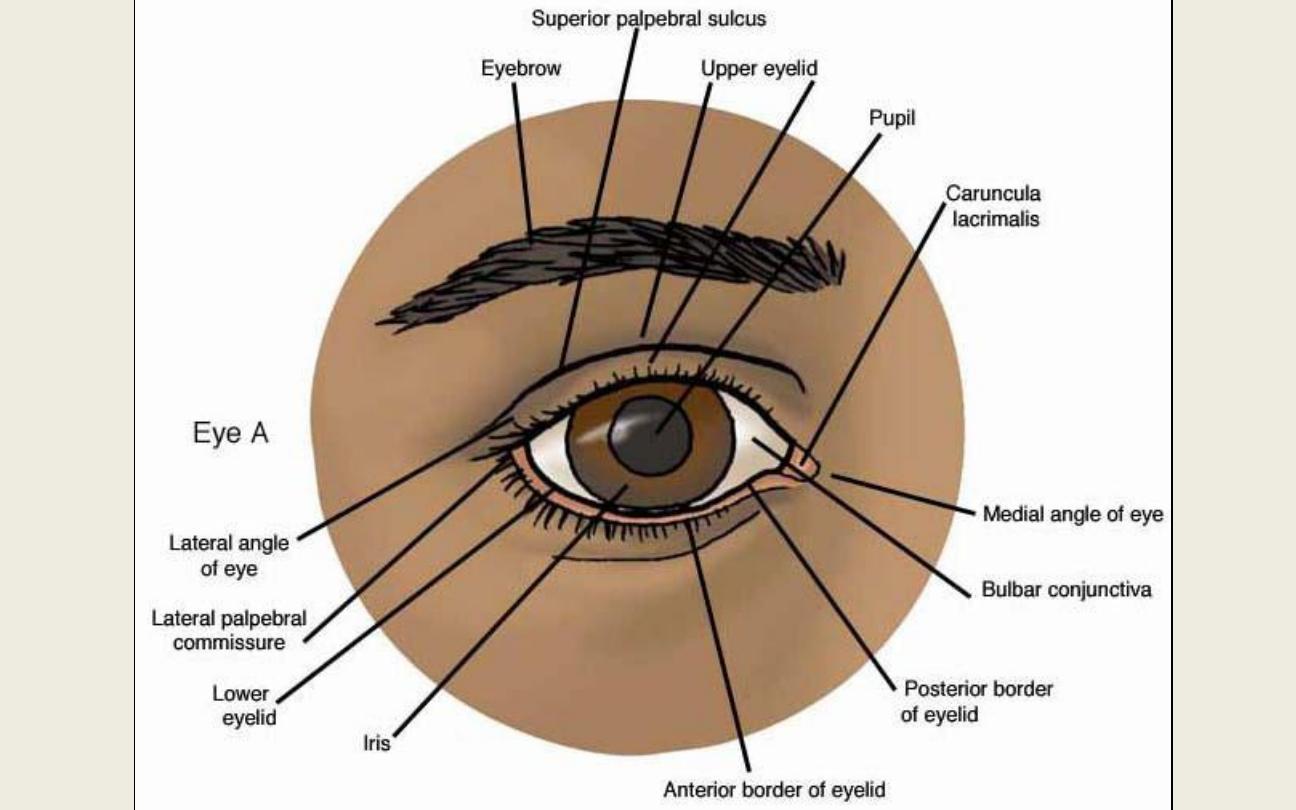
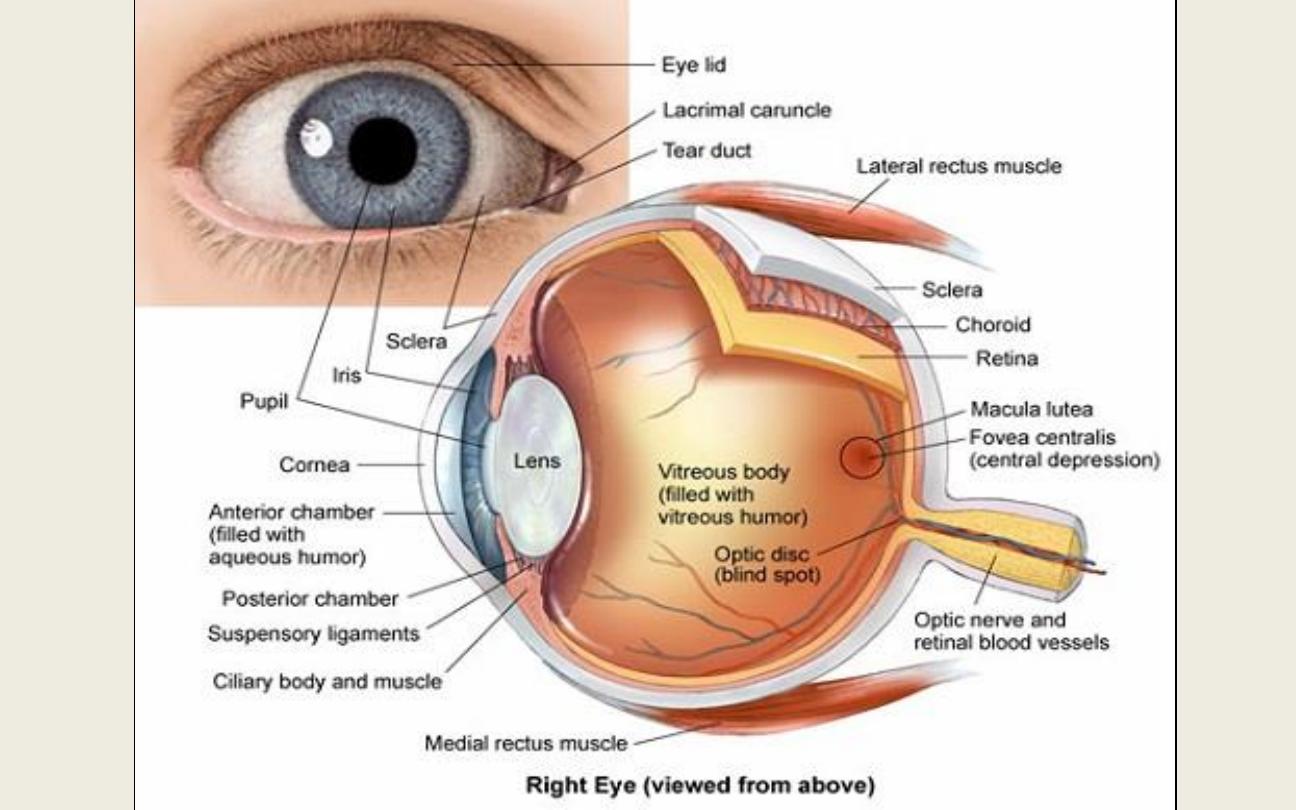
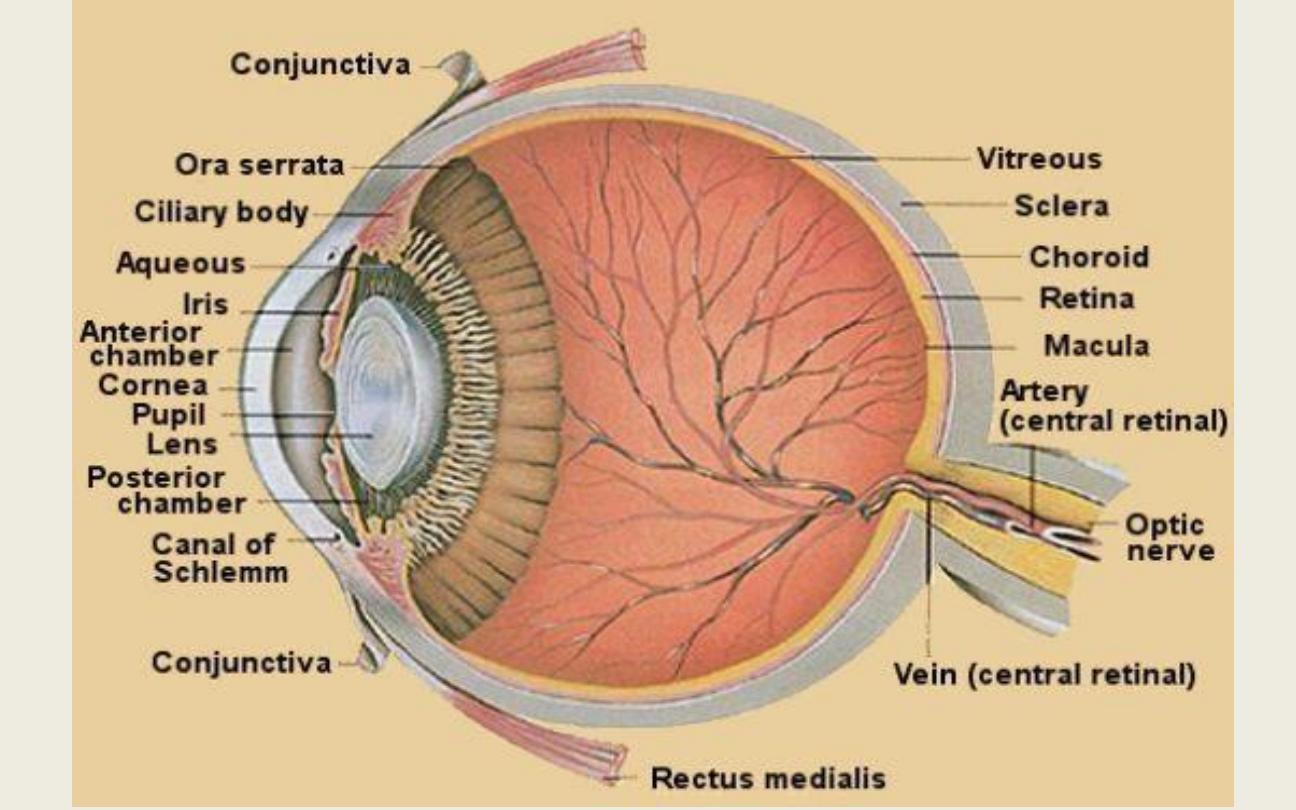
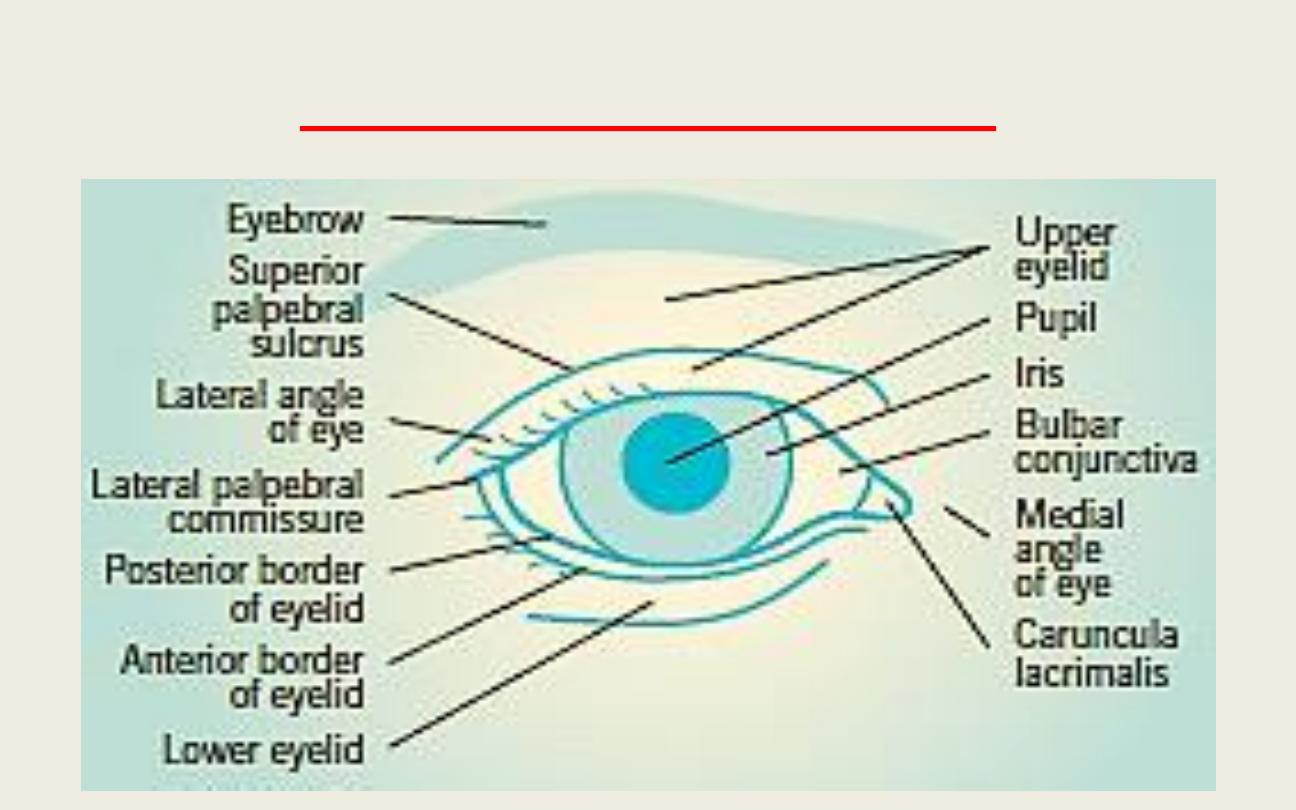
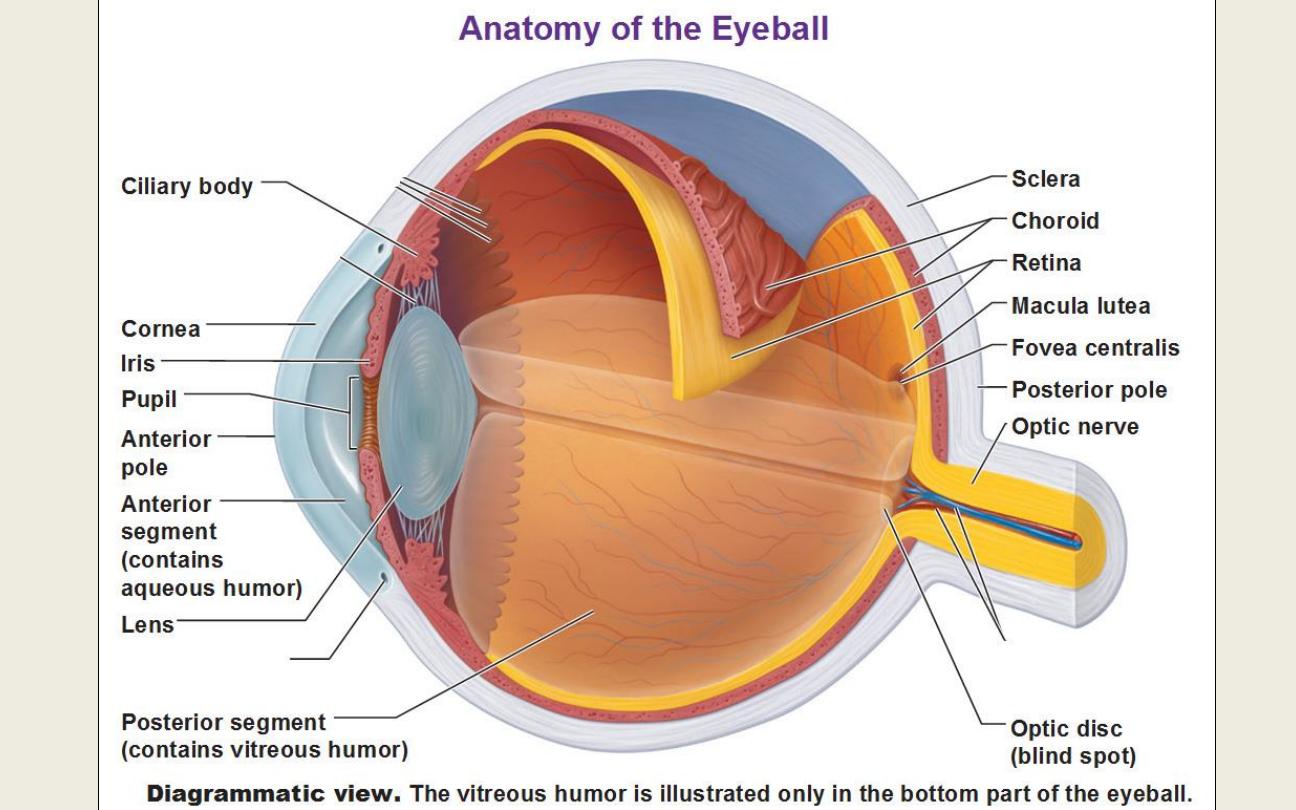
Gross anatomy of the eyeball
The globe has 3 main layers (coats), each of which s further divided:
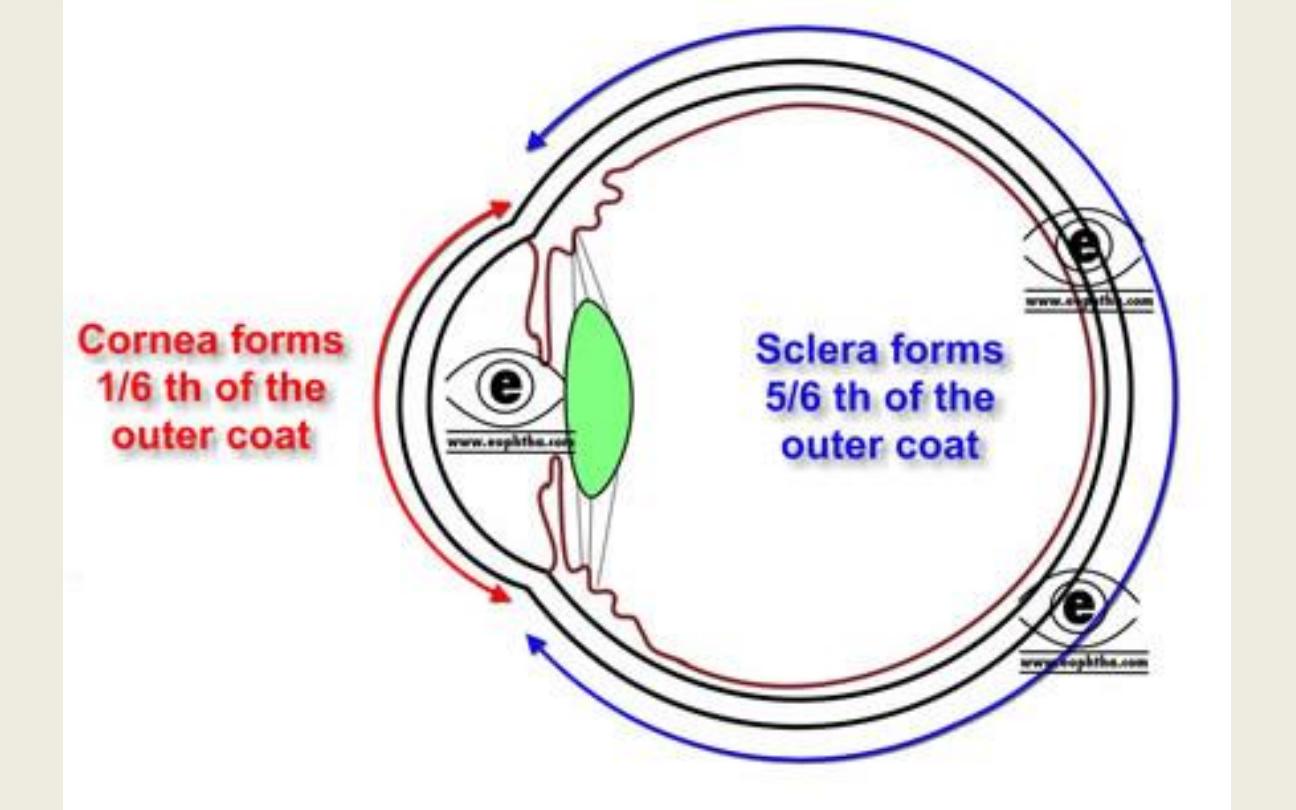
1)The outermost tunic (coat):
• Consists of
anterior one-sixth transparent part- the cornea and
the remainder five-sixths opaque part-the sclera.
The transitional junction area is – the limbus.
• Function:
Sclera: protection of intra ocular contents and also it facilitates the insertion of
external ocular muscles. Posteriorly, Sclera contains many perforations and orifices
for entrance and exit of vessels and nerves including the optic nerve.
Cornea: is to refract light on the retina and it is even more important than lens in
focusing light on the retina.
2) The middle coat (uvea or uveal tract):
• Consists of:
the posterior part which is called the Choroid,
a triangular shape muscular thickening called ciliary body and
anteriorly, diaphragm like structure called the iris.
The iris perforated centrally by regular and round opening called the pupil.
• Function:
Choroid, is nourishment to the outer 1/3rd of the thickness of retina.
The Ciliary body is secretion of aqueous humor and accommodation.
The iris is to determine the size of the pupil in order to determine the amount of
light inter the eye through the pupil and also gives the eye its color.
3)The inner coat:
• light sensitive layers, called retina,
composed of 10 layers, the inner 9 layers called sensory retina and outer one layer
called retinal pigment epithelium (RPE).
There is a deep yellowish-color area at the center of retina called macula lutea
(lutea = yellow), the center of macula lutea is called fovea centralis, which is the
most sensitive point in the retina.
Retina has two types of photosensitive cells, cones and rods. Fovea centralis
contains only cones which is responsible of sharp day and color vision, while
• The lens: is crystalline and transparent structure suspended in its position through
the Zonule to the epithelium of Ciliary body.
• Function: with the cornea forming the major refractive system of the eyeball that
converge light to focus on the retina. (the Cornea forming 2/3rd of the power of
the this system while the lens forming 1/3rd)
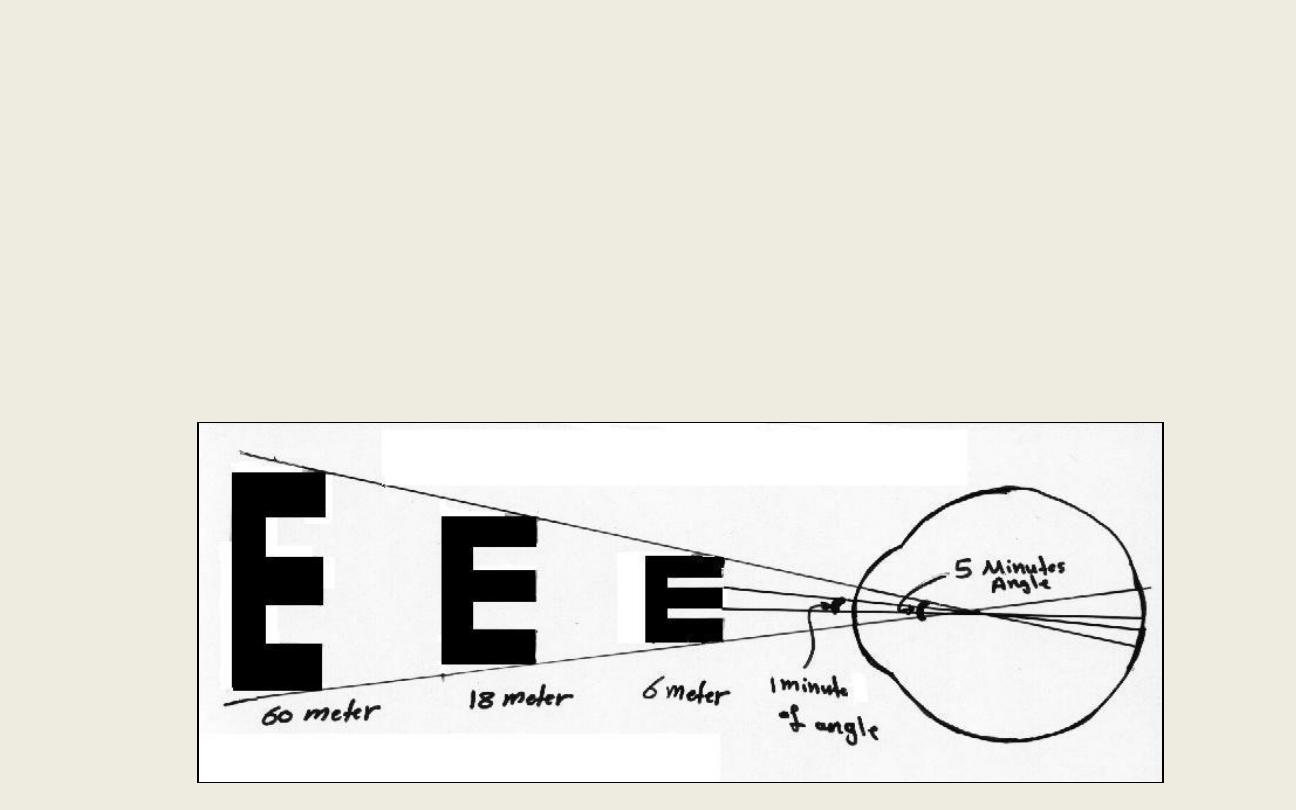
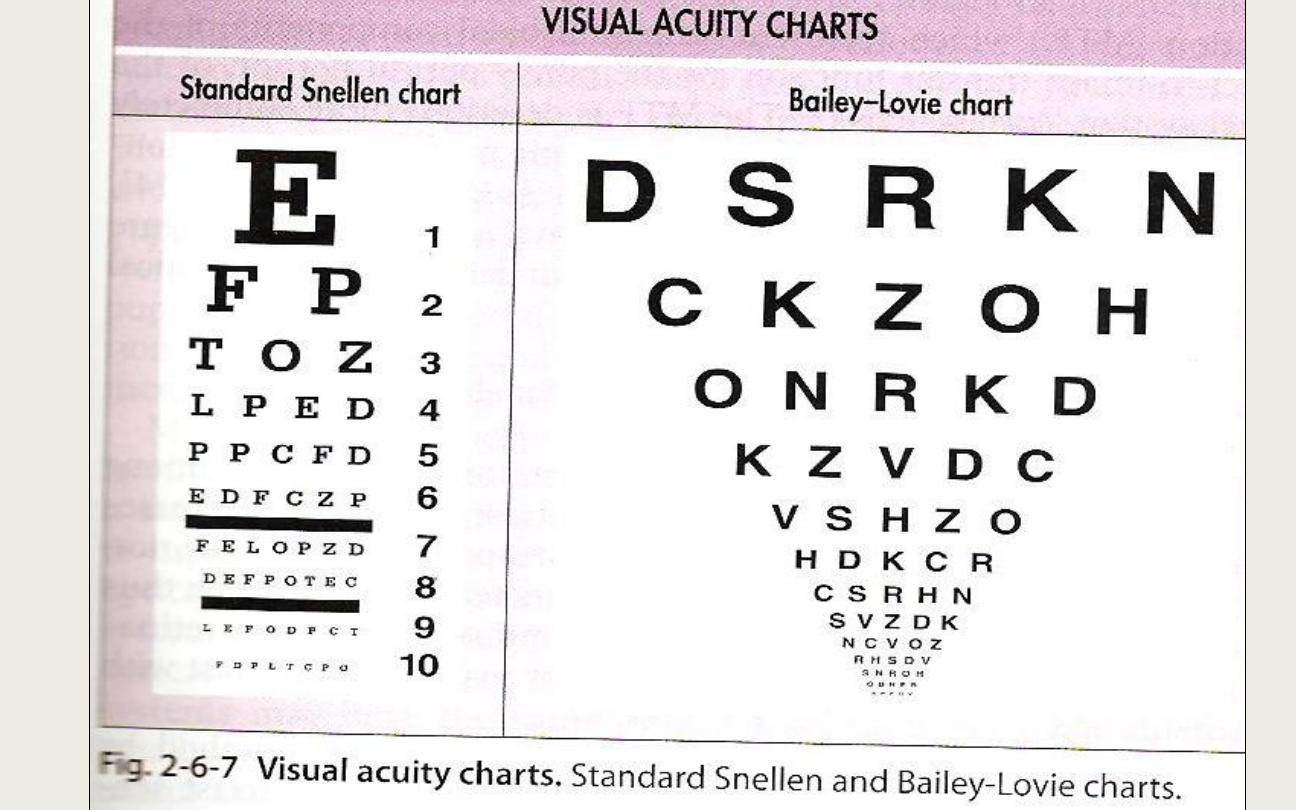
Visual Acuity
• Definition: it is the ability of the eye to distinguish the shape of symbols such as
letters, numbers and pictures. It is the cone function of the fovea centralis.
• VA is designated by two numbers:
1
st
- Numerator: indicates the distance separating the test object from the patient.
2
nd
- Denominator: indicates the distance at which the test object subtends an
angle of 5 minutes of arc, and each part of the test object subtends an angle of 1
minute of arc.
• In examination of the visual acuity of the patient by snellen's chart,
we ask him about the test object in the first line (size 60), if recognize it well, we
go downwards, but if he was unable, so we start to take the patient closer to the
chart meter by meter, so if he see the first line at 5m, 4m, 3m, 2m or 1m, it is
5/60, 4/60, 3/60, 2/60 or 1/60 subsequently.
If the patient till now can't recognize the test object then we shift to
o counting fingers then
o hand movement and then to
o light projection by applying light in different directions and ask the patient to tell
us what is the direction the light is coming from, if he can't determine the
direction, then we shift to
o light perception by asking the patient if he is seeing the light,
o if no light perception then say it is blindness.
Color vision:
• Most normal humans have 3 types of cones and consequently a 3-variable color-
vision (3 cone opsins) system. These 3 types are:
Middle wavelength sensitive (M) cones for detecting high resolution achromatic
(black and white) contrast.
Short wavelength sensitive (S) cones used only color by comparing its signals with
those of the M cones. This mechanism creates blue/yellow color vision.
Long wavelength cones (L) which are creates red/green color vision.
• Color vision deficiencies can be
autosomal, e.g. congenital achromatopsia & cone degeneration.
Color vision abnormalities can be acquired:
1- Retrobulbar neuritis.
2- Foveal degeneration caused by vascular disease.
3- Retinal detachment (involving the fovea).
Visual field
• Definition: Island of vision in sea of darkness.
• The function of the extrafoveal retina is assessed by measurement of the visual
field when the ability to recognize the special target diminishes rapidly in all
directions away from the fovea centralis.
• The macula also can be assessed through performing central visual field, so we
have 2 types of visual field:
1. Central visual field (macular) central 30°.
2. Peripheral visual field (extramacular) out of central 30°.
The peripheral extension of visual field is: 50° superioly (limited by eye brow), 60°
nasally (limited by nose), 70° inferiorly (limited by cheek) and 90° temporally (no
limitation).
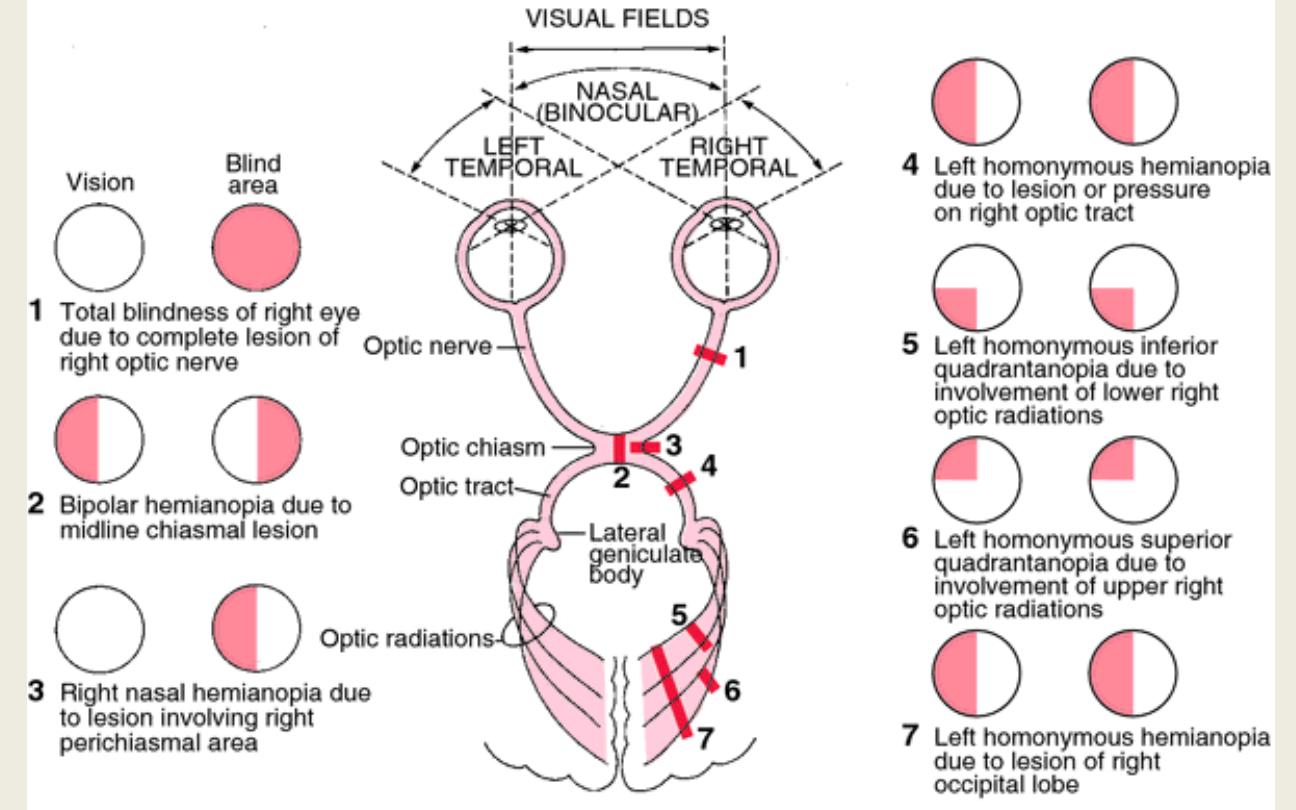
• Interpretations of visual field abnormalities:
Mono-ocular VF defect: Disease involving retina and optic nerve.
Binocular VF defect: Disease involving the optic chiasma, optic tract, optic
radiation and occipital cortex.
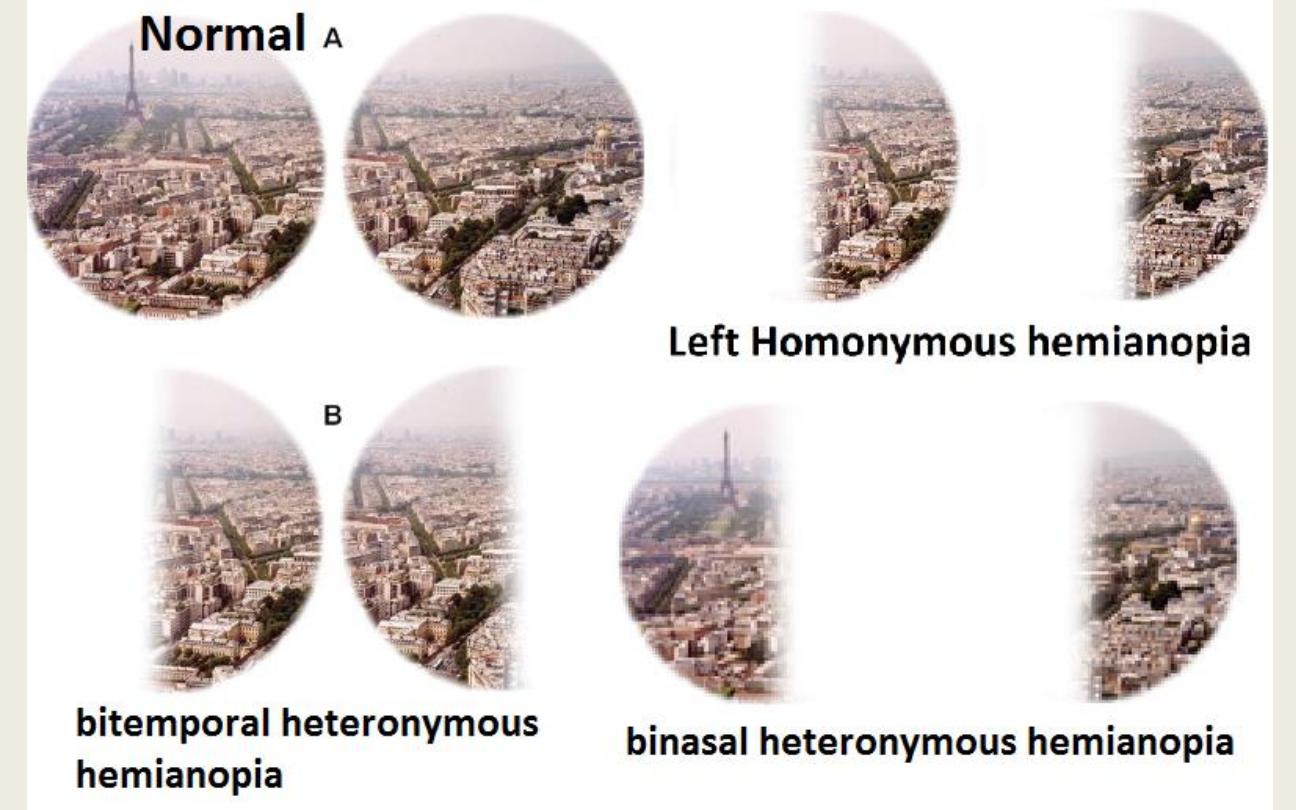
Hemianopia: half-blindness, left and right retina of opposite side.
o Homonymous hemianopia: binocular right or left Homonymous hemianopia.
o Heteronymous hemianopia: binocular, right from one eye and left from other. Usually
we use either bitemporal or binasal heteronymous hemianopia.
• Defects in the VF are usually described as:
1.
Central (within central 30°).
2.
Peripheral (outside central 30°).
Central VF defect (central scotoma): characterized diseases involving the fovea
centralis and the papillomacular bundle of nerve fibers in the optic nerve.
Centrocecal scotomas: involve both, physiological blind spot and fixation point, e.g.
toxic diseases of the optic nerve.
Annular scotoma: e.g. retinal pigmentary degenerations (retintis pigmentosa),
advance glaucoma, and senile miosis of pupil.
Arcuate (arched) scotoma: Early Glaucoma.
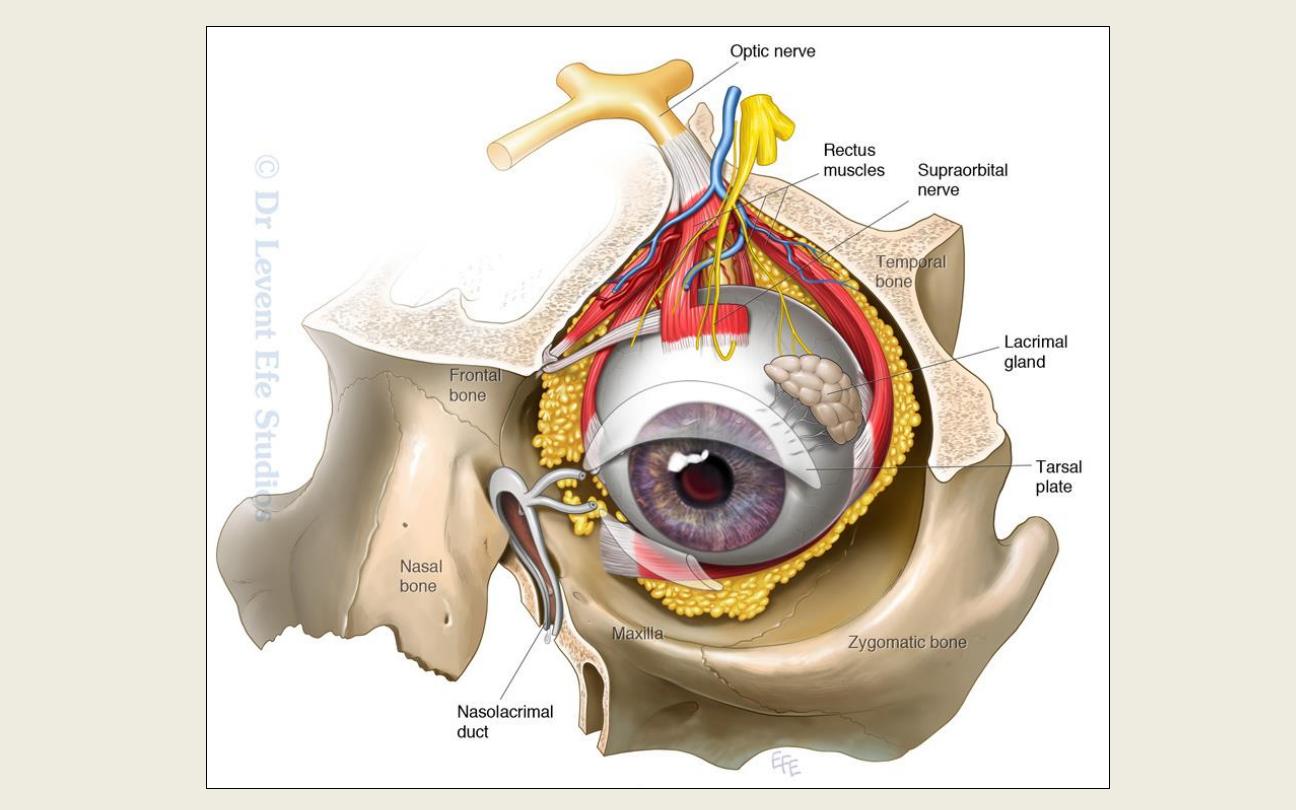
“The orbit”
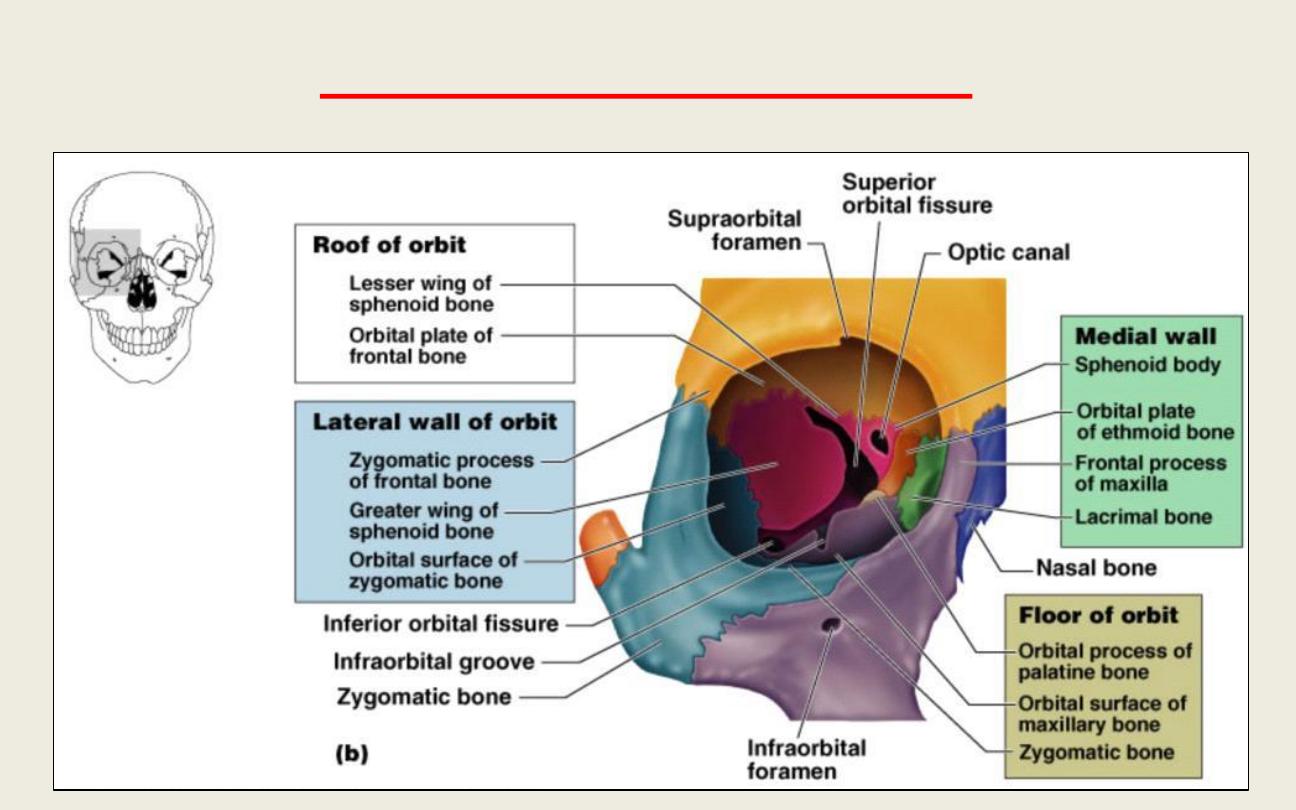
Anatomy of the orbit
Clinical signs of orbital disease
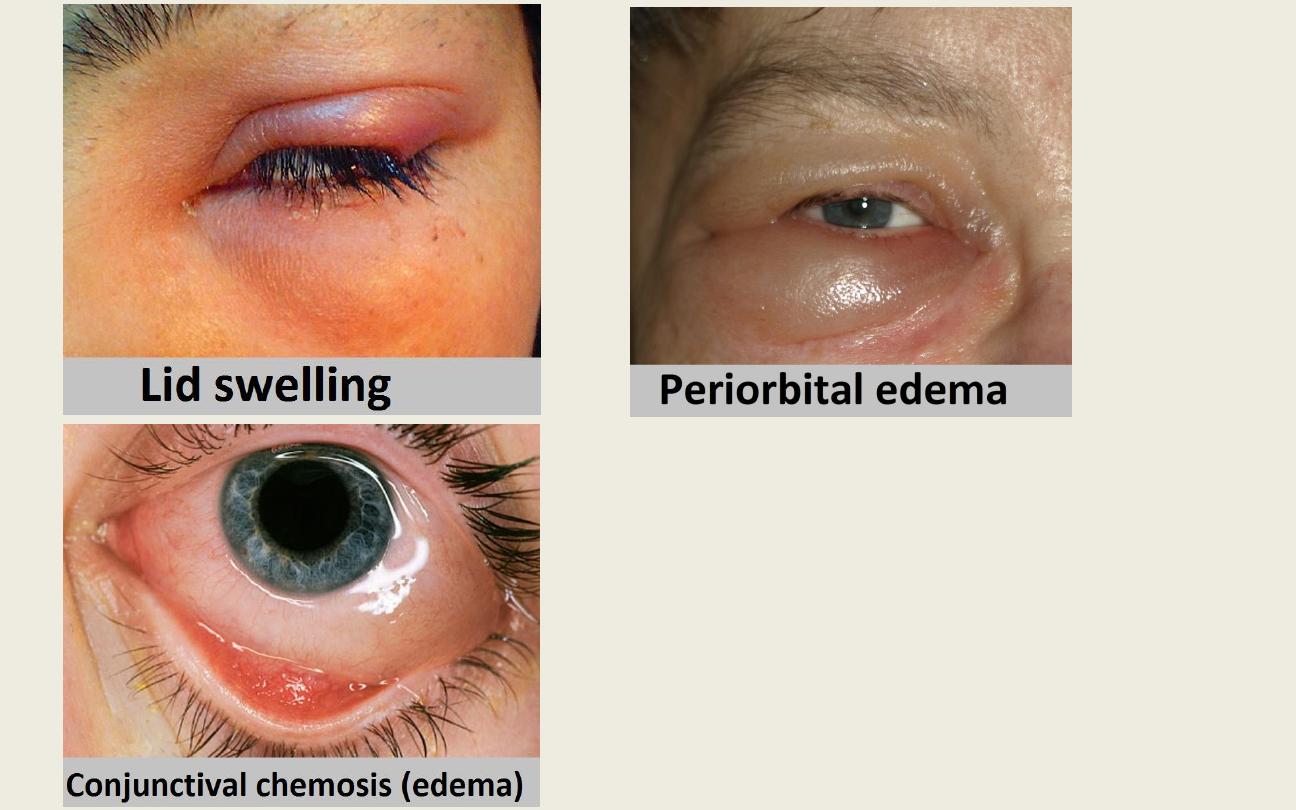
Soft tissue involvement
• Signs:
Lid & periorbital edema
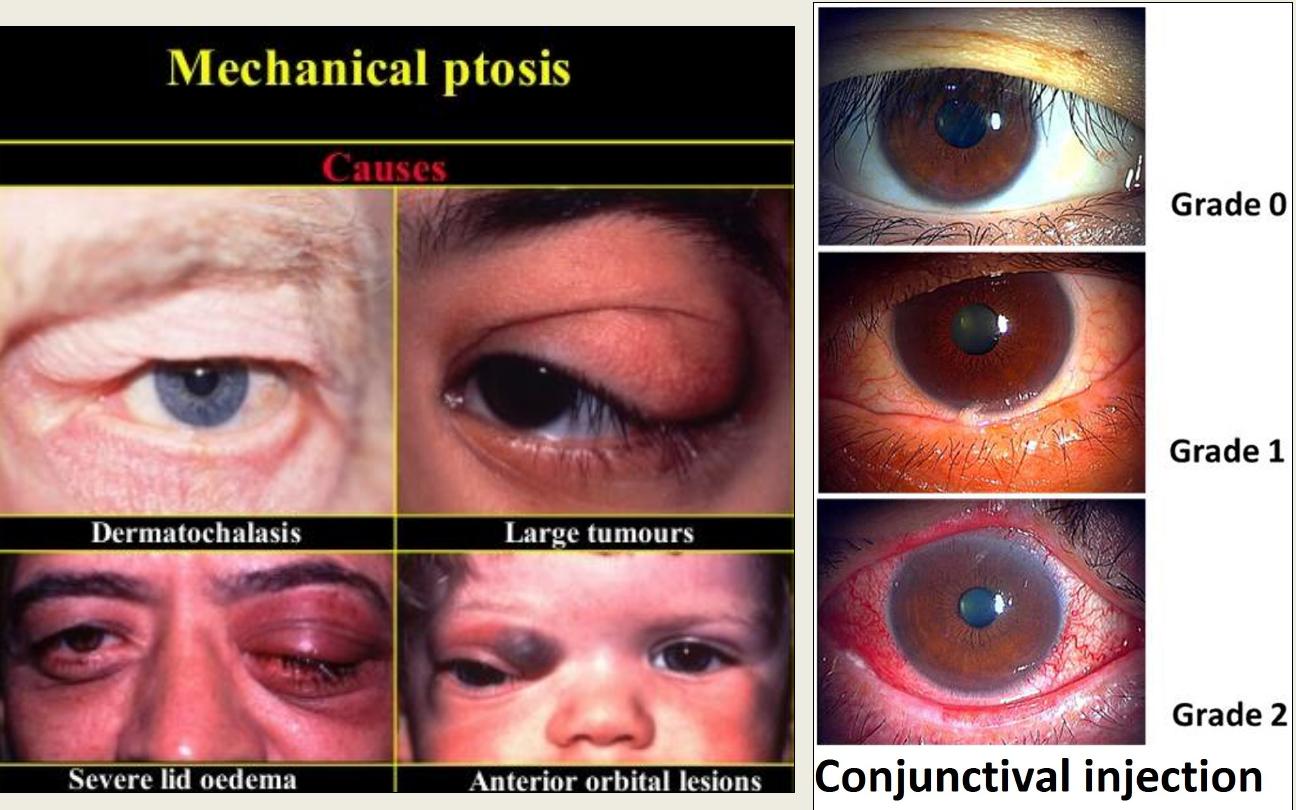
Ptosis: Mechanical ptosis due to swelling of lid.
Conjunctival chemosis (edema) & conjunctival injection.
• Causes:
Thyroid eye disease
Orbital swelling
Inflammatory orbital disease
Arterio-venous shunts.
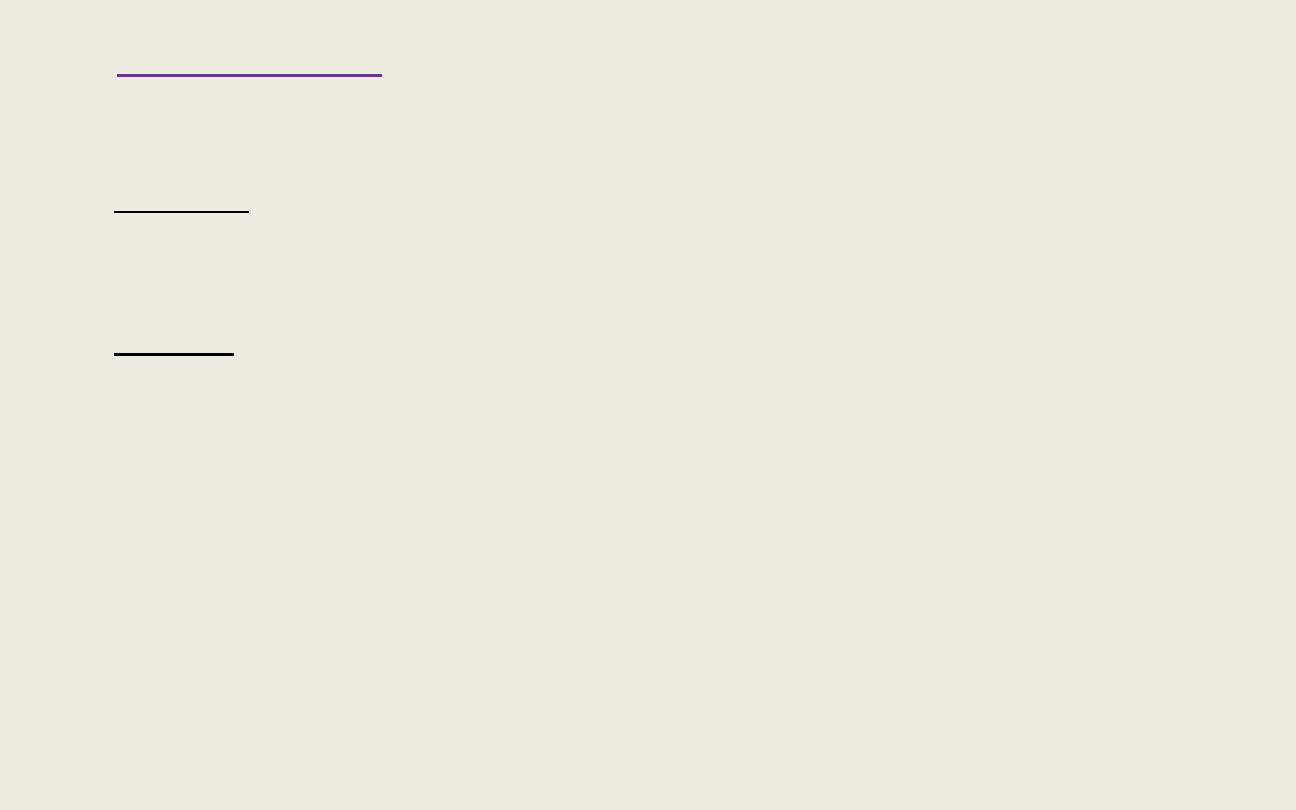
Proptosis:
• Abnormal forward displacement of the globe caused by retrobulbar lesion or less
frequently by shallow orbit which is usually congenital.
• Direction:
Axial
Eccentric: (upwards, downwards, medial or lateral)
• Severity: evaluated by simple plastic ruler (placed at the lateral margin to measure
the position of the apex of the cornea)
Normally: the apex of the cornea is up to 20 mm anterior to lateral orbital margin.
Mild: 21-23mm, Moderate: 24-27mm, Severe: > 28mm.
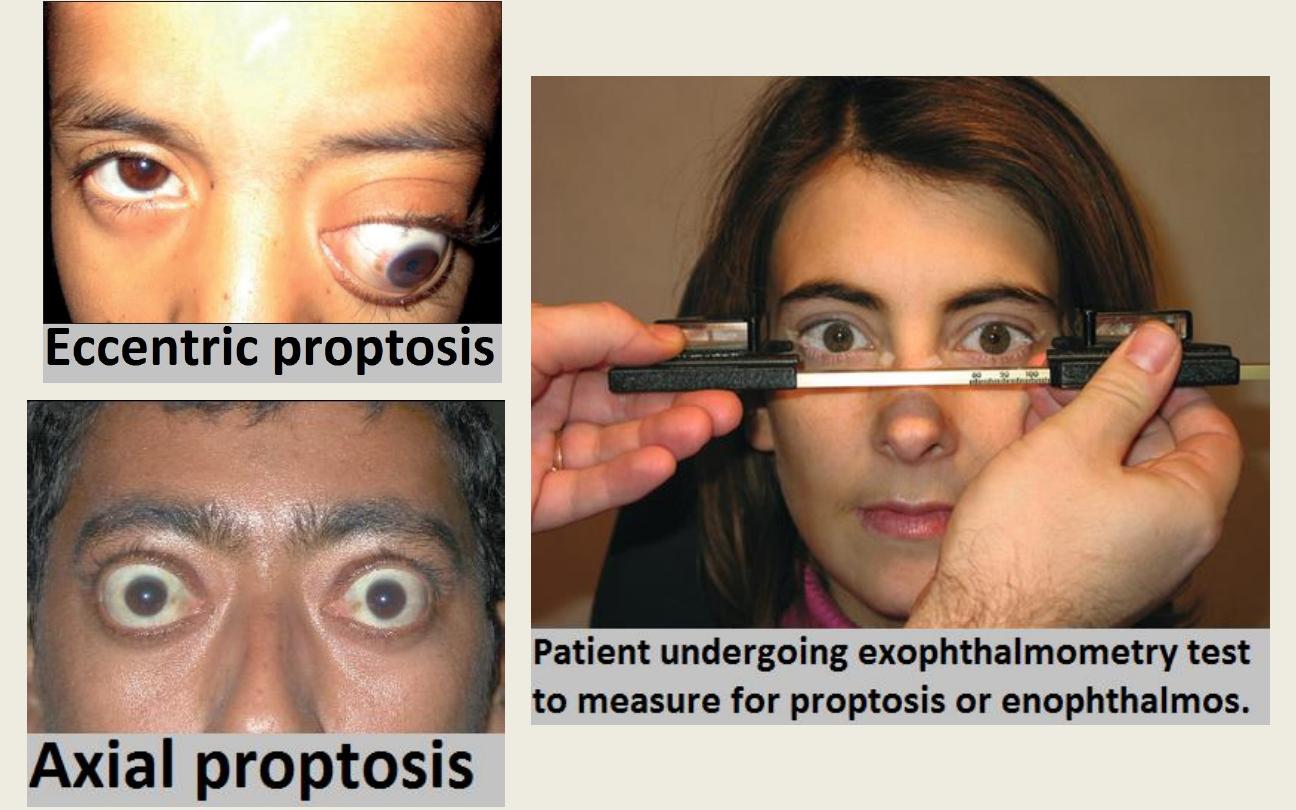
Enophthalmos:
• The globe is recessed within the orbit.
• Causes:
Small globe, congenital anomaly.
Structural bony abnormalities, blowout
fracture of floor.
Atrophy of orbital contents, after
radiotherapy
Cicatrizing orbital lesions, such as
chronic sclerosing inflammatory orbital
disease, secondary malignancy or
carcinoma of orbit causing fibrosis of
intraorbital structure & traction of
eyeball.
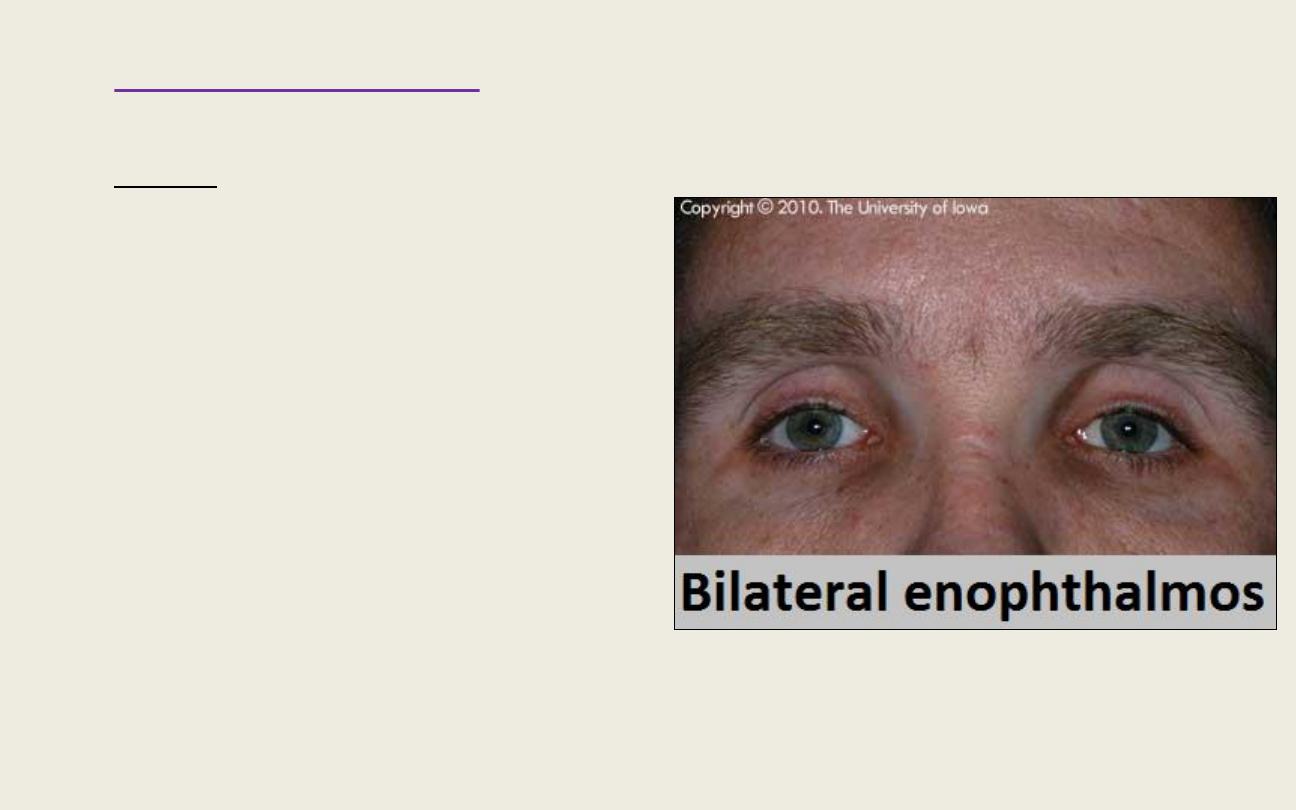
Ophthalmoplegia:
• Defective ocular motility, caused by:
Thyroid eye disease
Intraorbital eye disease
Tethering of the muscle
(ocular trauma)
Optic sheath meningioma
Visual
dysfunction
(reduced visual
acuity):
• Exposure keratopathy
• Compressive optic
neuropathy
• Choroidal folds at macula
Orbital infection
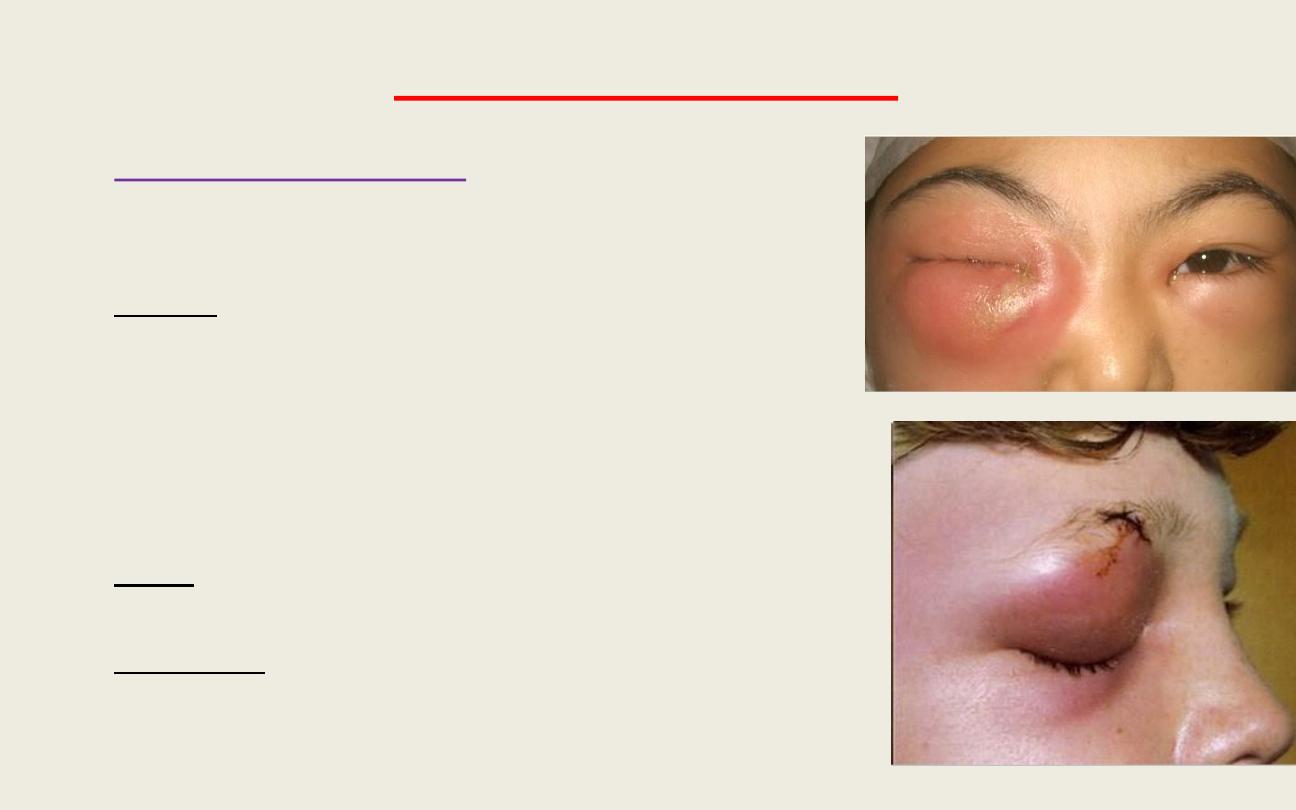
Preseptal cellulitis:
• infection of subcutaneous tissue anterior to the orbital
septum.
• Causes:
Skin trauma, lacerations or insect bites
Spread of local infection; such as dacrocystitis & acute
hordeolum
From remote infection; of the URTI or middle ear
infection by haematogenous spread.
• Signs: unilateral, tender, red periorbital & lid swelling. Ct
show opacification anterior to the orbital septum.
• Treatment: Oral co-amoxiclav. Severe infection require IV
antibiotics.
Bacterial orbital cellulitis:
• Polymicrobial infection of soft tissues behind the orbital septum, occur commonly in
children under 5 years. Causes:
Sinus-related: most common ethmoidal sinusitis & Extention of preseptal cellulitis.
Spread from adjacent dacrocystitis, mid-facial & dental infection
Post-traumatic & postsurgical & Haematogenous spread
• Presentation: severe malaise, fever, pain & visual impairment.
• Signs:
Swollen, tender, red & warm lids (unilateral) & Proptosis
Painful ophthalmoplegia (may cause diplopia)
Signs of optic nerve dysfunction (in advanced cases)
CT opacification posterior to orbital septum
• Complications:
Ocular: exposure keratopathy, ↑ IOP, central retinal vein or artery occlusion, optic neuritis
Intracranial: meningitis, brain abscess & cavernous sinus thrombosis & Orbital abscess
• Treatment: hospitalization, antibiotics & surgical intervention in some cases.
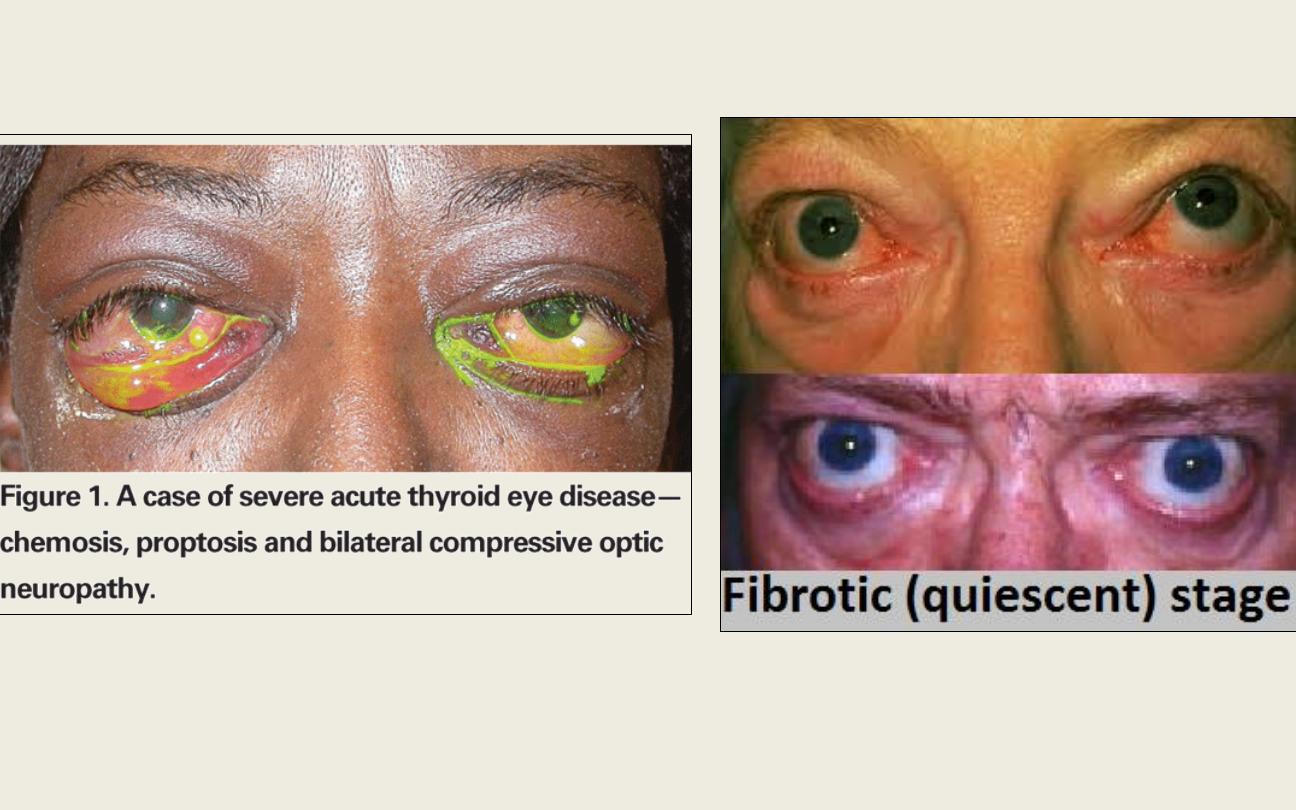
Thyroid eye disease (thyrotoxicosis;
Graves’ disease)
• Stages:
1) Congestive (inflammatory or acute) stage: eyes are red & painful. This stage
leads to remission within 3 years.
2) Fibrotic (quiescent) stage: eyes are white & motility defects are present.
• Clinical manifestations: soft tissue involvement, lid retraction, proptosis, optic
neuropathy & restrictive myopathy.
• Lid retraction: upper lid margin is either at level or above the superior limbus
(allowing the sclera to be visible)
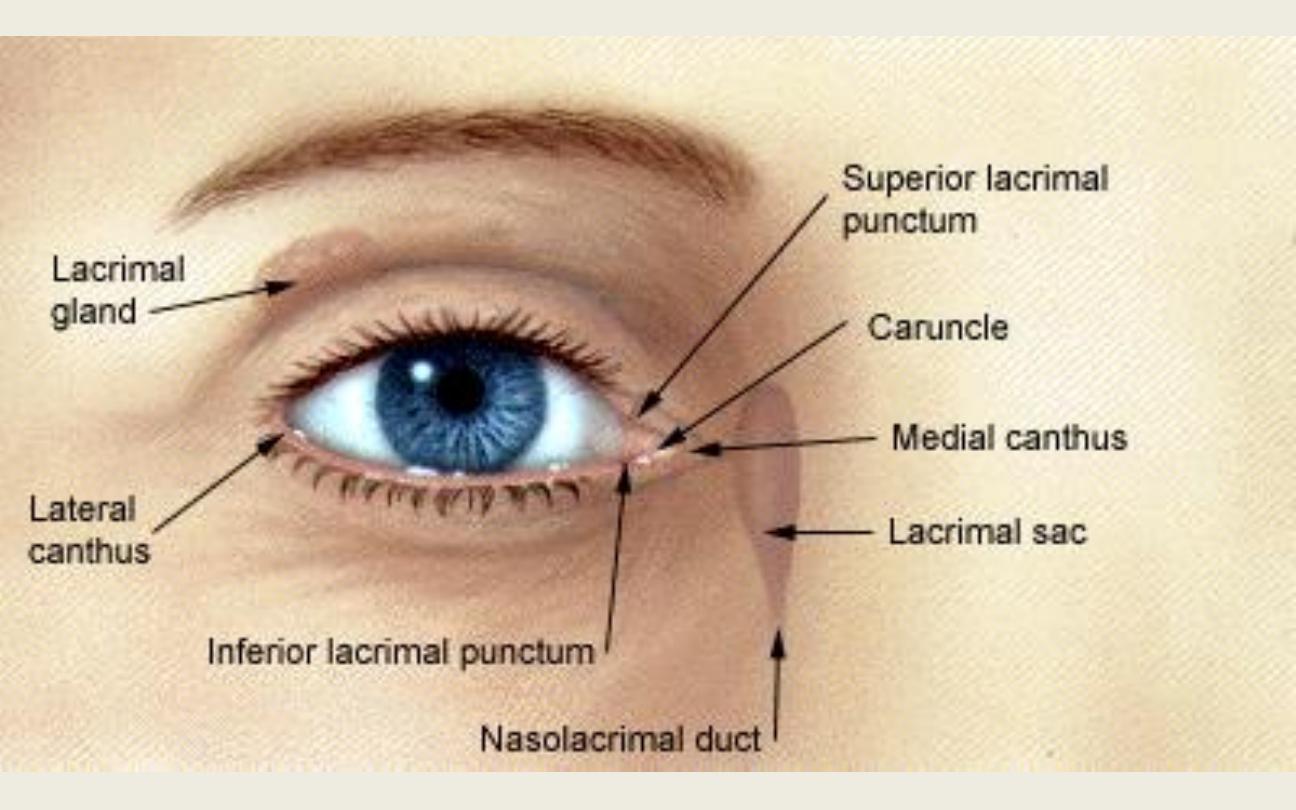
“Lacrimal
apparatus”
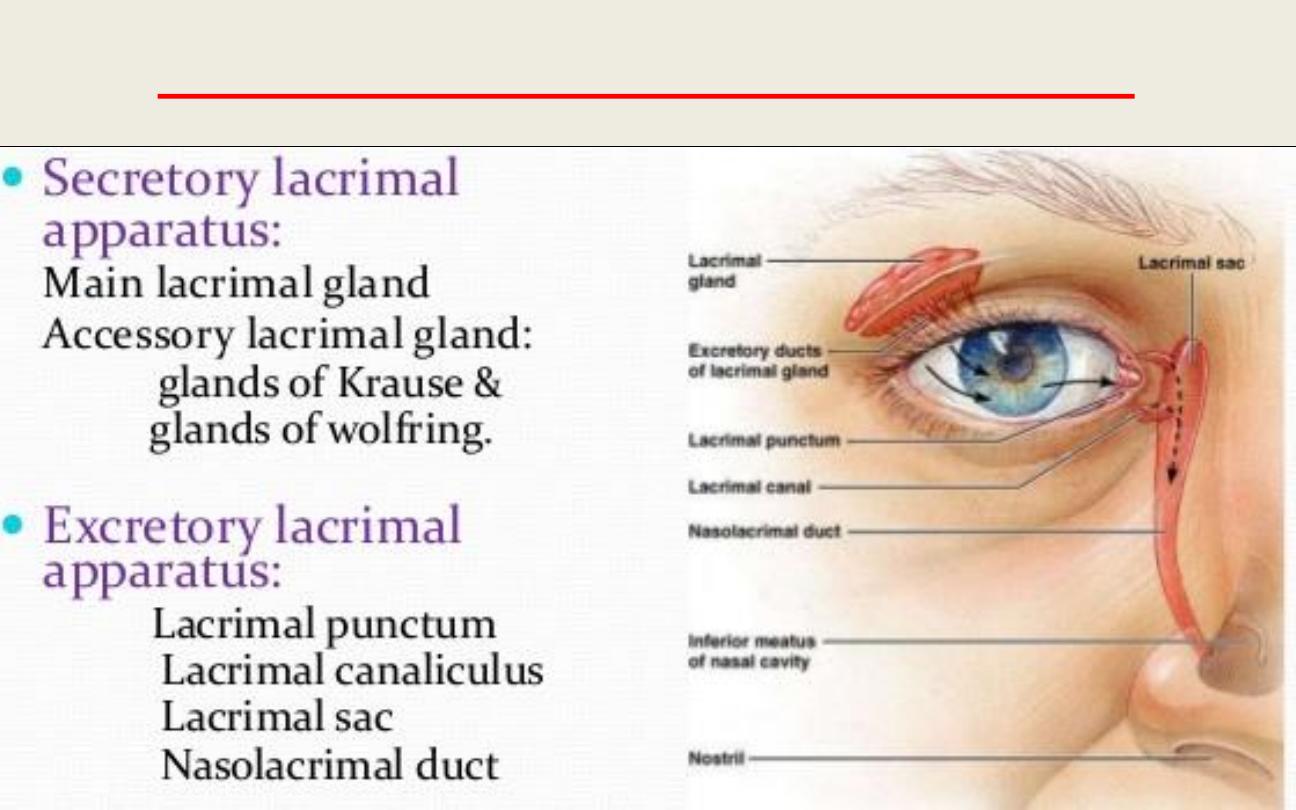
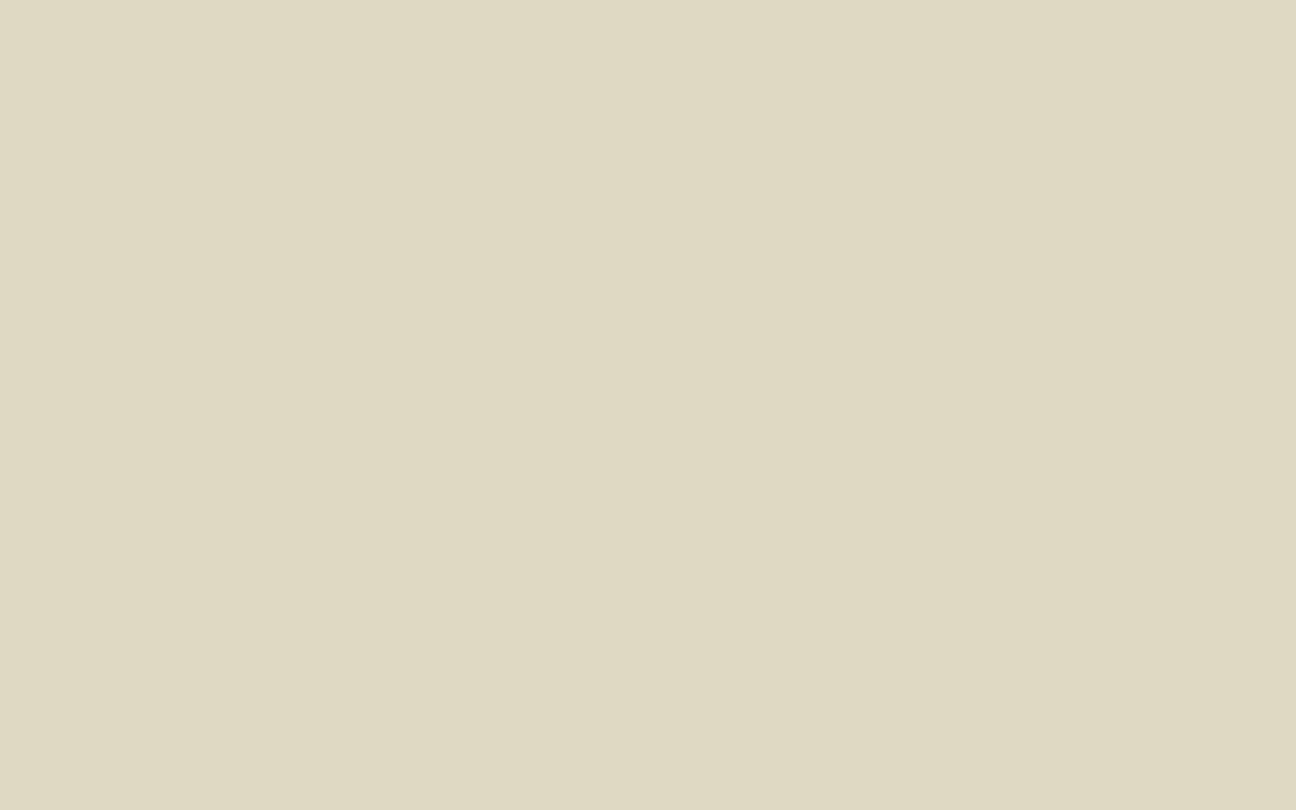
Anatomy of lacrimal apparatus
Diseases of lacrimal glands
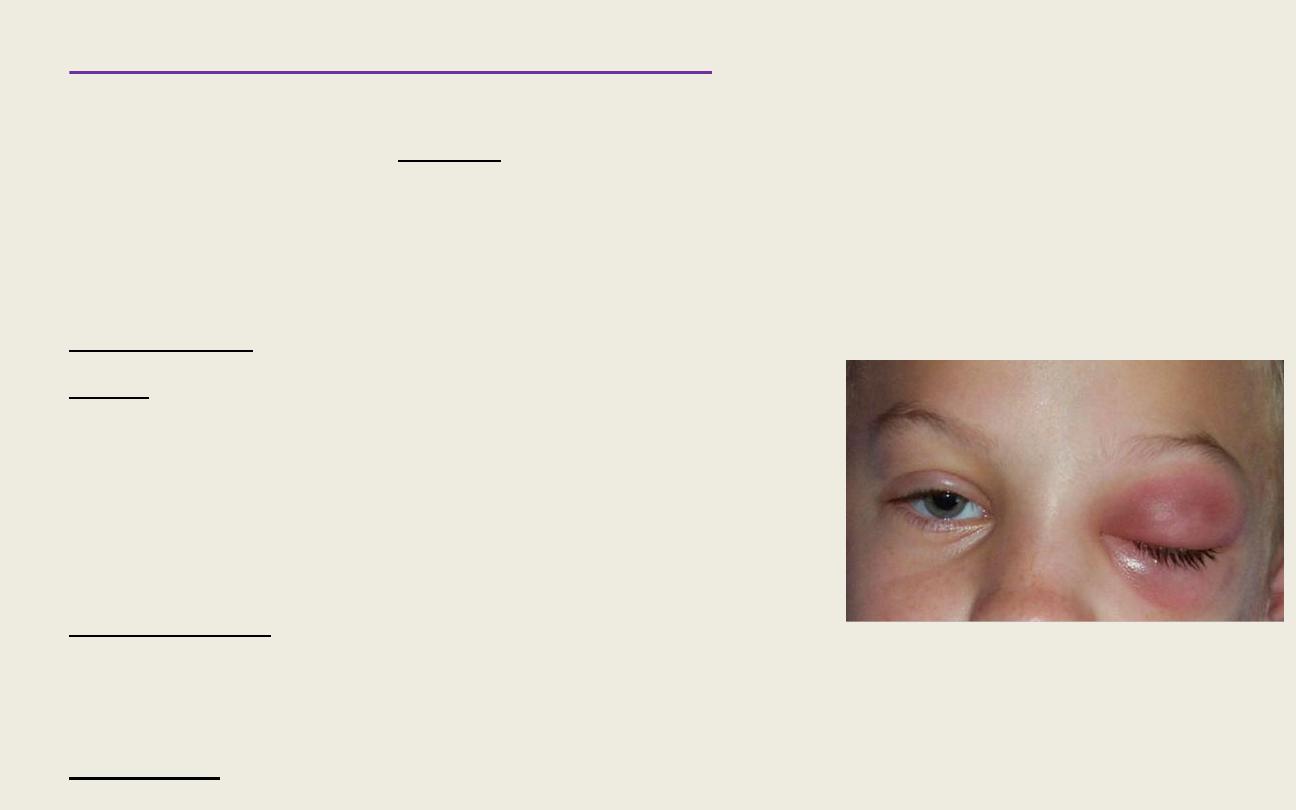
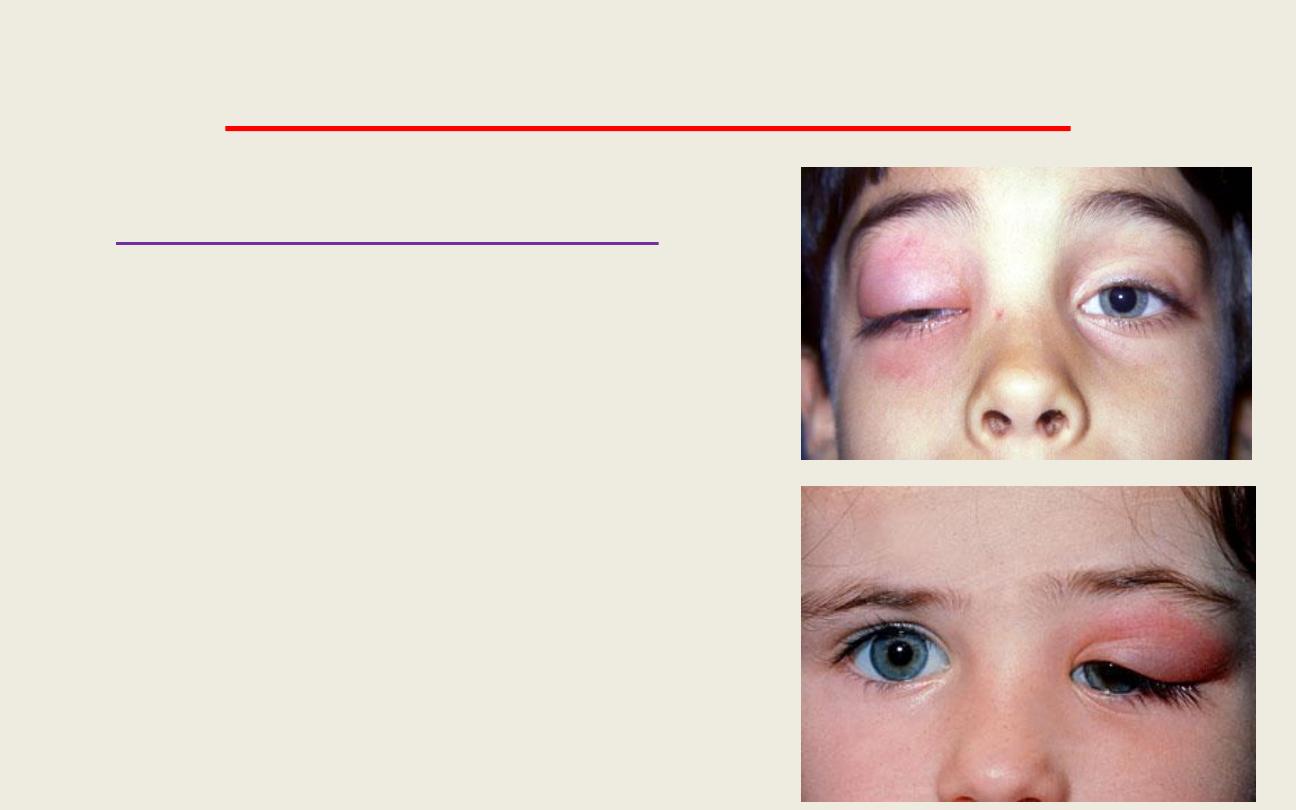
Acute dacryoadenitis:
• Uncommon inflammation of the lacrimal
gland that usually accompanies systemic
disease (mumps & infectious
mononucleosis)
• Signs:
Pain & dicomfort
Mechanical blepharoptosis
Swollen & reddened gland
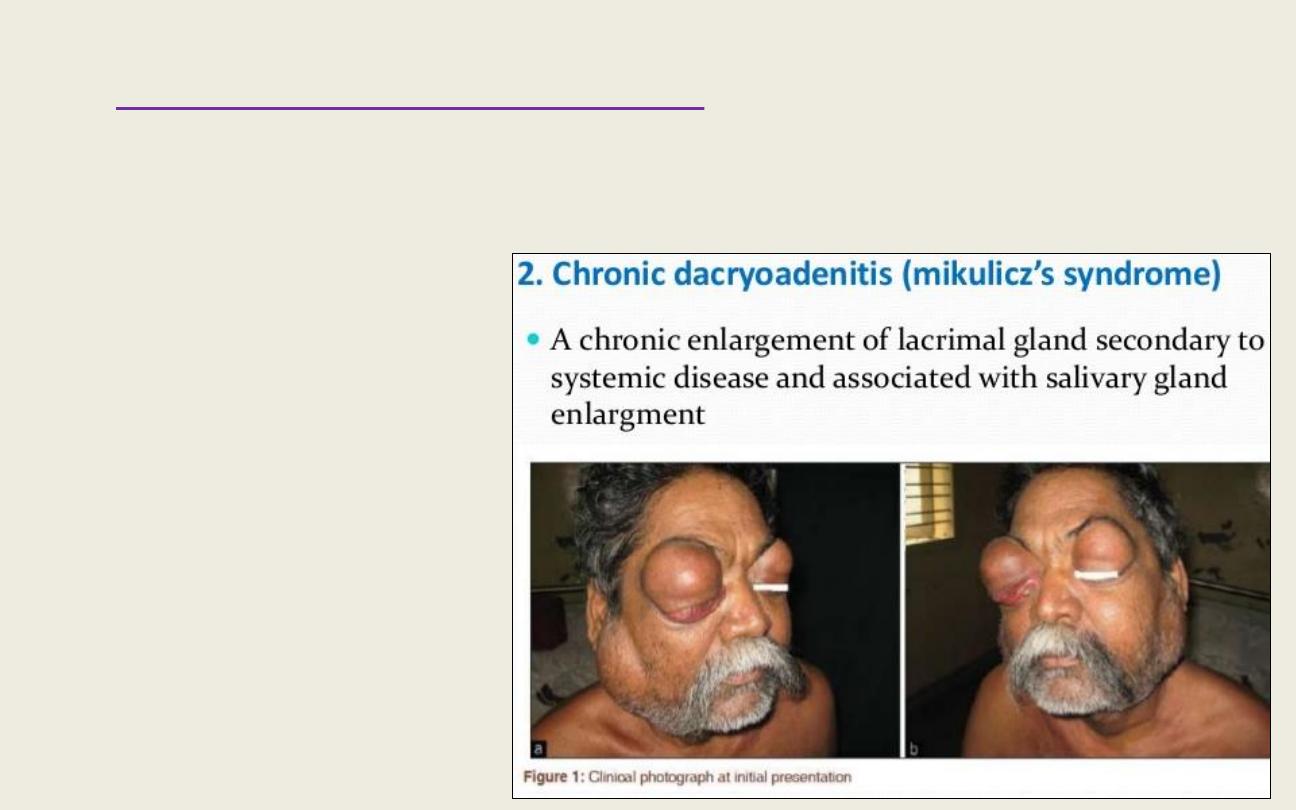
Chronic dacryoadenitis:
• Proliferative inflammation of the lacrimal gland that occurs in a variety of
disorders (sarcoidosis, sjorgen’s syndrome, leukemia, lymphoma, amyloidosis, Tb,
syphilis & foreign body granuloma)
• Signs & symptoms:
Painless enlargement of the
lacrimal gland
No congestion & no redness.
Disease of the lacrimal passages
Dacrocystitis
• Inflammation of the lacrimal sac. The cause is obstruction of the lacrimal sac or
nasolacrimal duct followed by microbial infection.
1) Acute dacrocystitis
• Suppurative inflammation of the lacrimal sac associated with cellulitis of the
overlying tissues (tissues medial to the medial canthus).
• Signs & Symptoms: painful swelling, sac tenderness, widespread cellulitis &
associated constitutional symptoms.
2) Chronic dacrocystitis
• Occurs due to obstruction of nasolacrimal duct & it is seen most frequently in
middle life.
• Sings & symptoms: Epiphora, painless swelling at the inner canthus & pressure
over the sac results in reflux of mucopurulent material through the canaliculi.

Lacrimal drainage obstruction
1) Punuctal stenosis with epiphora
• Causes:
Idiopathic (most common cause, usually in elderly),
herpes simplex lid infection,
trachoma,
irritation &
Ciactricial conjunctivitis.

2) Canalicular obstruction
• Causes:
Idiopathic fibrosis (most common),
chronic dacrocystitis,
herpes simplex lid infection,
cicatricial conjunctivitis,
systemic use of 5-fluorouricil
3) Acquired nasolacrimal obstruction
• Causes:
Idiopathic stenosis (most common),
Naso-orbital trauma,
wegener’s granulomatosis,
irradiation &
nasopharyngeal tumor.
4) Congenital nasolacrimal obstruction
• At birth, the lower end of the nasolacrimal duct is frequently non-canalized
(near the valve of hasner), nut this is of no clinical significance in most
neonates because it canalizes spontaneously soon after birth. Sometimes,
the occlusion continues & result in:
Epiphora
Gentle pressure of the lacrimal sac causes reflux of purulent material from
the puncti.
Occasionally, acute dacrocystitis might result.
Causes of excessive watering
1)
Lacrimation
2)
Obstructive epiphora
3)
Lacrimal pump failure
• Differential diagnosis of watery eye (lacrimation & epiphora)
Congenital drainage system obstruction.
Ophthalmianeonatrum (neonatal conjunctivitis)
Congenital glaucoma
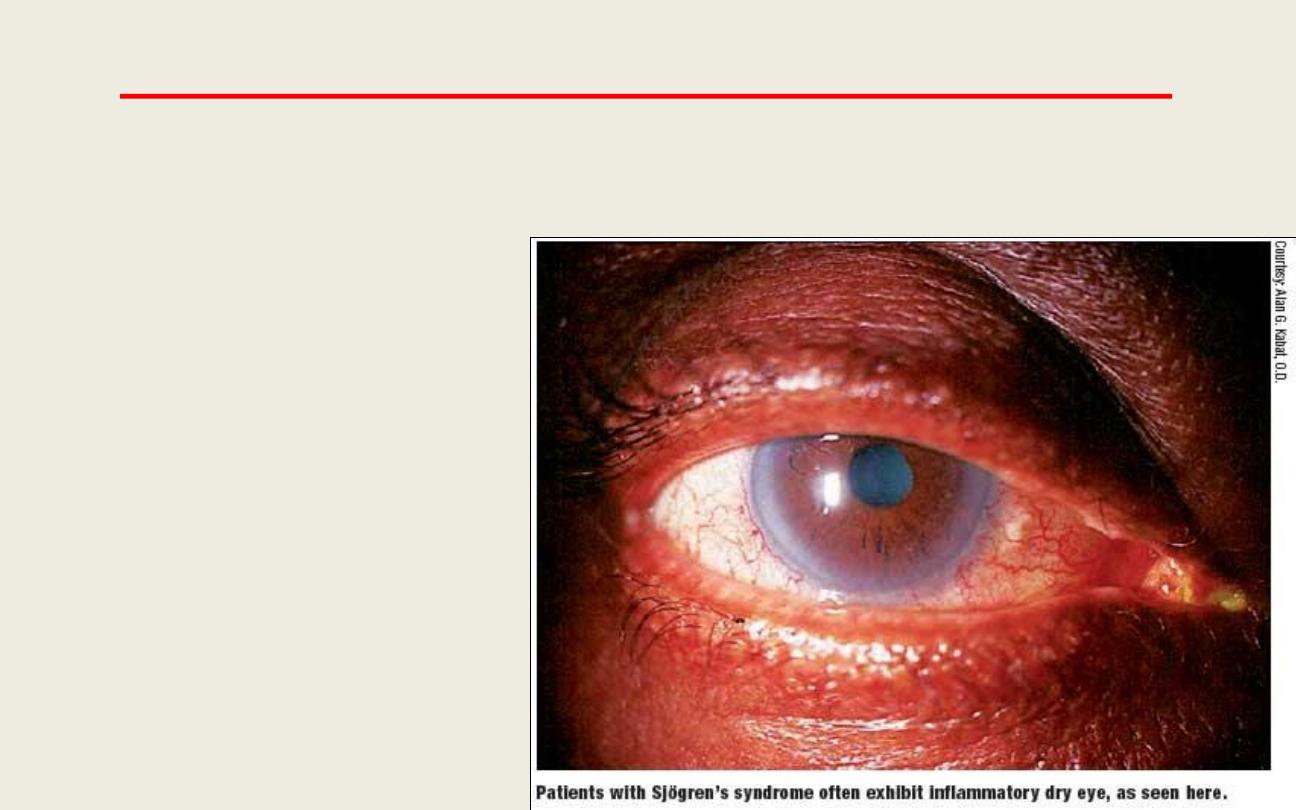
Dry eye (Keratoconjunctivitis sica)
• Absent or reduced tears causes keratinization of corneal & conjunctival epithelium
& possibly marked corneal scarring & opacification, usually both eyes are affected.
• Symptoms:
Burning sensation
Feeling of dryness
Continuous foreign
body sensation
Mucus discharge (as the
aqueous par affected)
Transient blurring of vision
Itching
Photophobia
• Causes of dry eyes:
Atrophy & fibrosis of lacrimal gland tissue as a result of a destructive infiltration
by mononuclear cells, usually associated with systemic diseases.
o Primary KCS: involving lacrimal gland alone (dry eye only & nothing else)
o Primary sjorgen’s syndrome: dry eye associated with dry mouth.
o Secondary sjorgen;s syndrome: dry eye & mouth associated with systemic disease,
most common one is rheumatoid arthritis, and other disease are SLE, systemic
sclerosis, hishimoto thyroiditis & primary biliary cirrhosis.
Miscellaneous causes:
o Destruction of lacrimal tissue by tumors, sarcoidosis.
o Meibomian gland dysfunction.
o Absence of lacrimal gland (Congenital or by surgical
removal)
o Blockage of the excretory ductules (due to burns,
drugs, diseases .. Etc, that cause blockage of these
excretory duct)

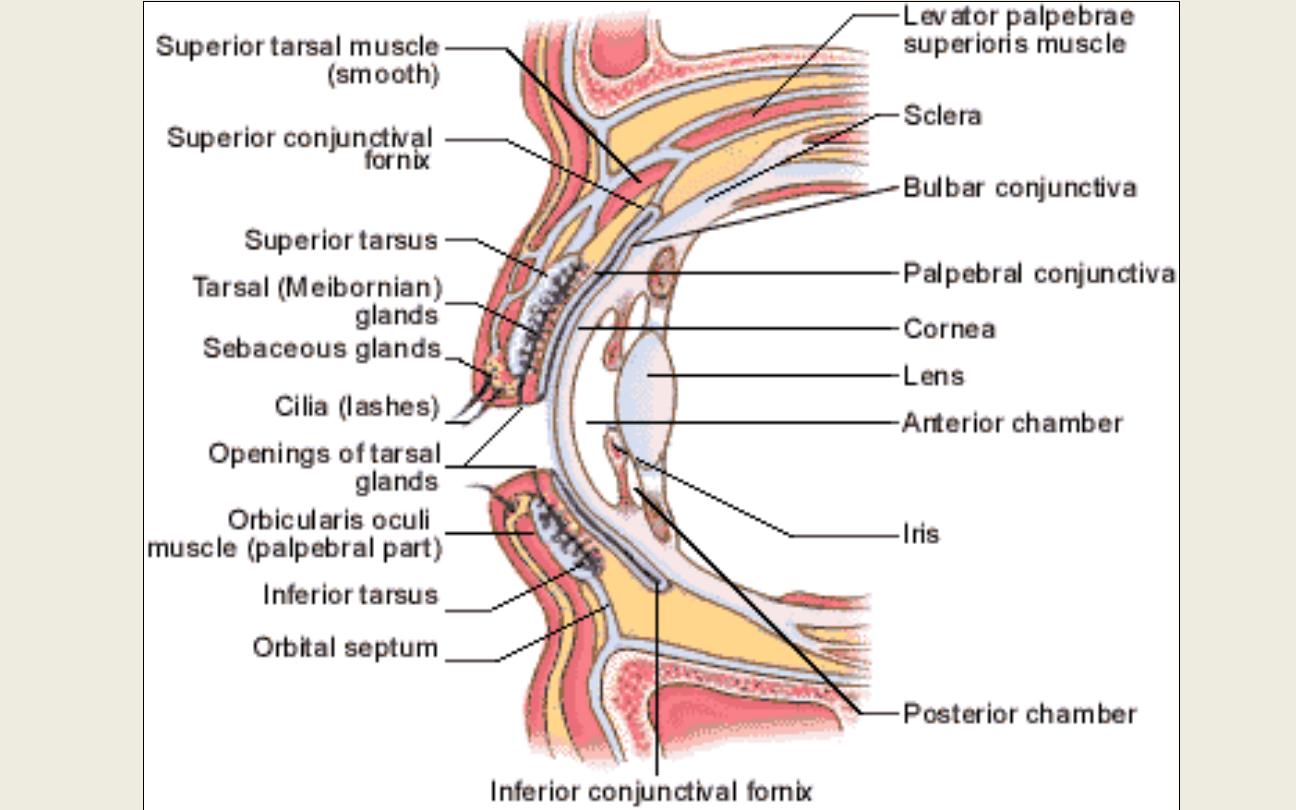
“Eyelid”
Anatomy of the eyelid
Congenital anomalies of the eyelid
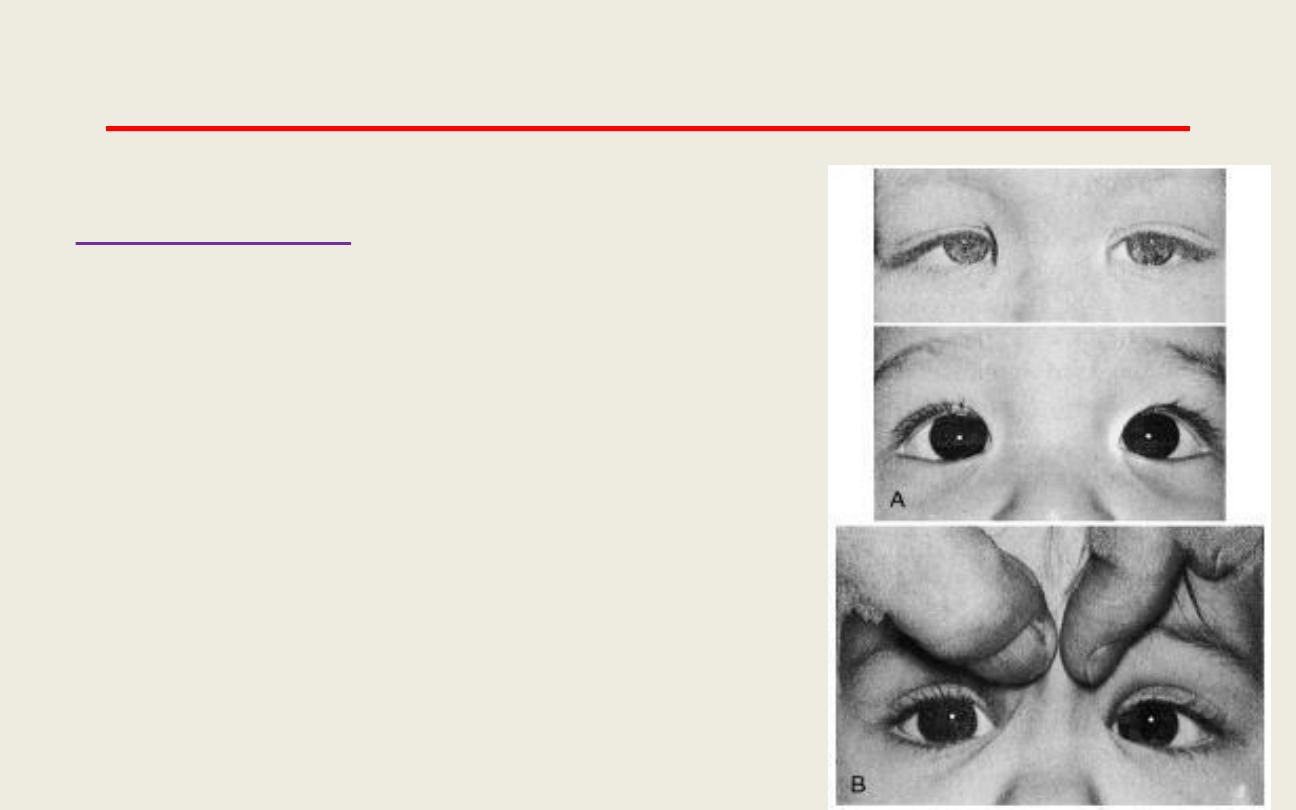
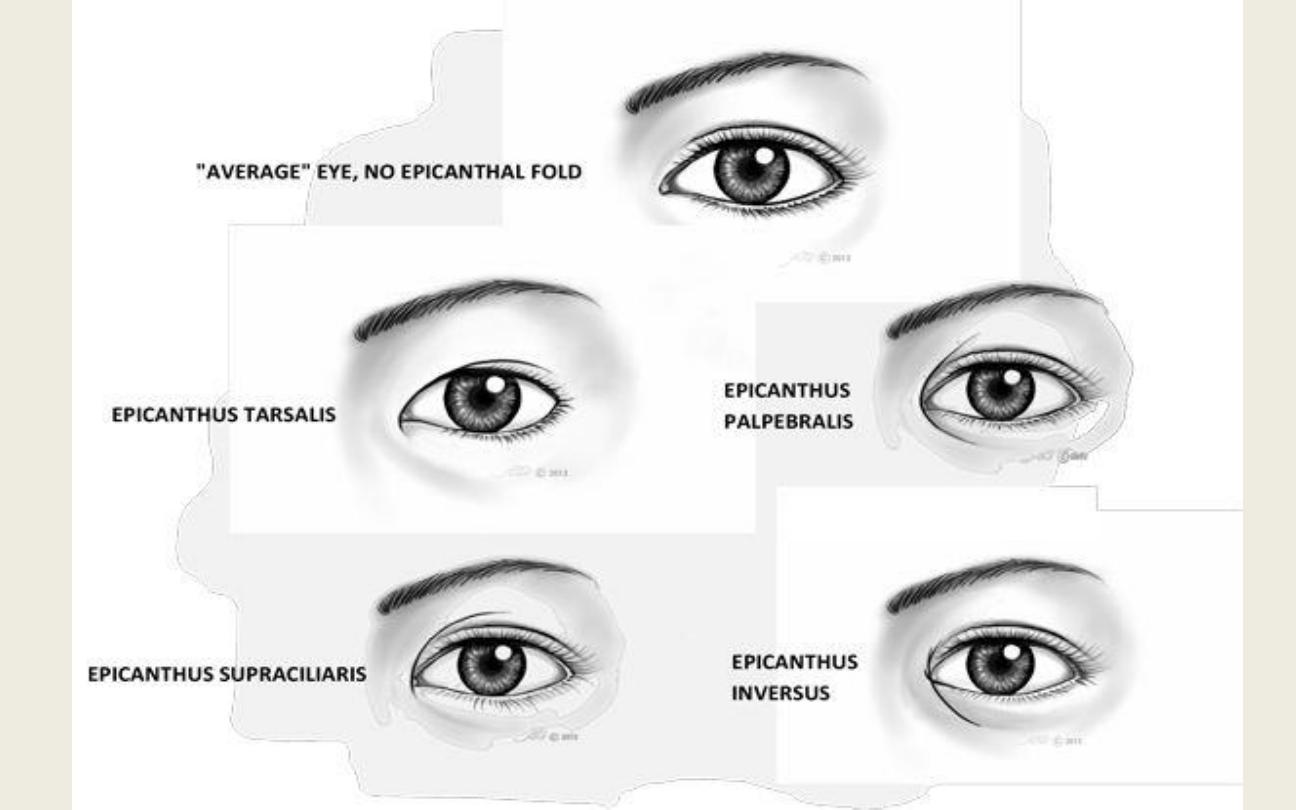
Epicanthus
Common anomaly, there is accessary fold of skin
extending from the nose to the inner end of the eye
brow which conceals the medium angle & caruncle
giving a picture stimulates convergent sequence
(pseudosequint).
Eyelid Coboloma
Failure of a portion of the lid to develop leading to notch in the lid margin.
Ablepharon
Absence of the eyelid
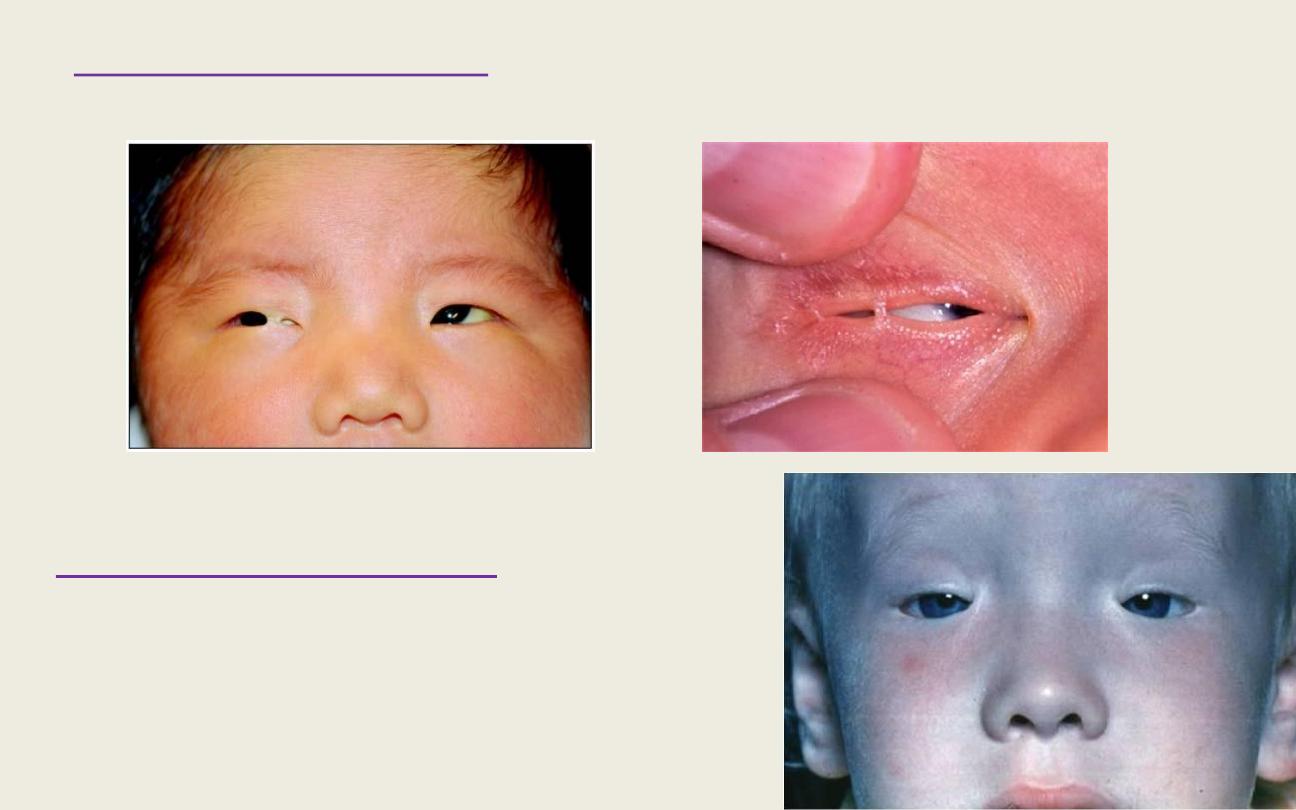
Ankyloblepharon
Imperfect separation of the eyelid
Blepharophimosis
Narrowing of the palpebral fissure usually
associated with congenital ptosis & epicanthus.
Abnormalities in shape & position
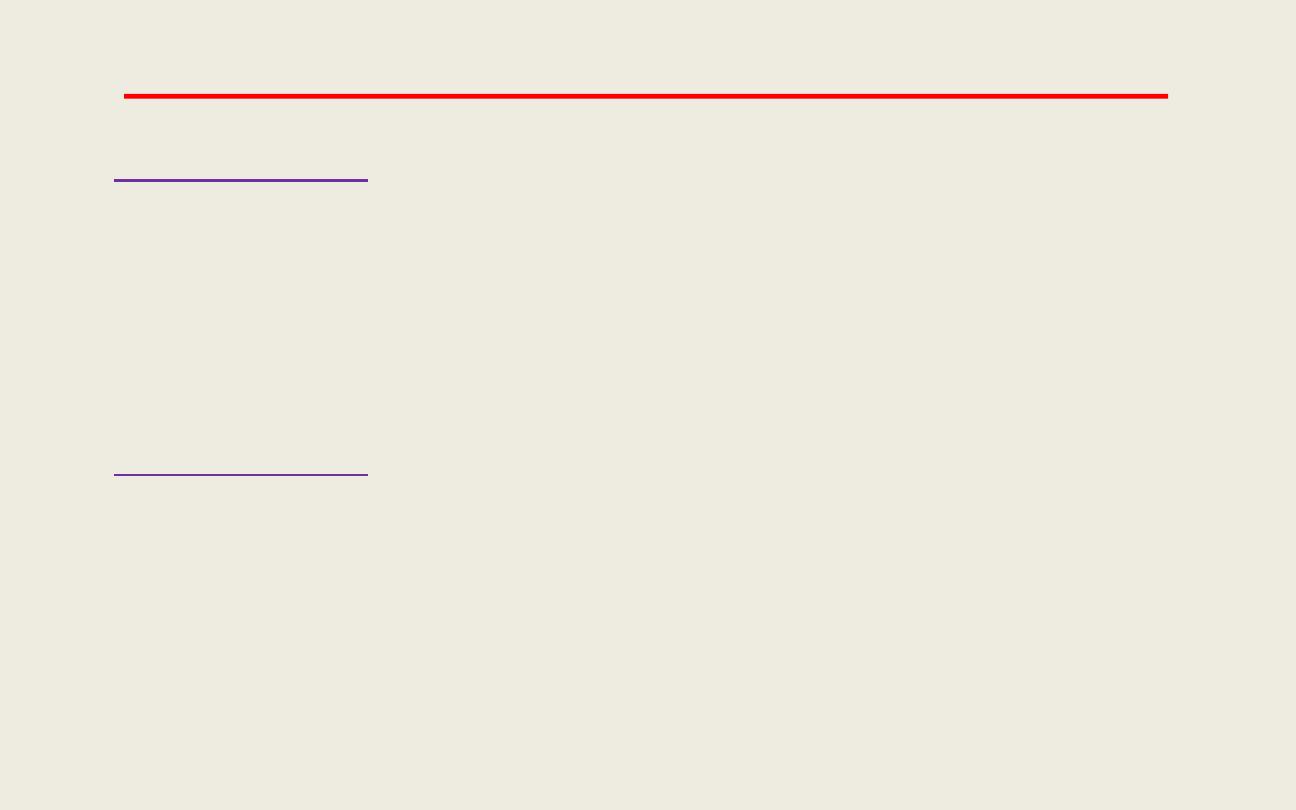
Entropion:
• Rolling of the eyelid inward continuous rubbing of the cornea.
• Causes: Cicatrial (fibrotic), Involutional (senile), Spastic & Congenital.
• Clinical picture: foreign body sensation, photophobia, lacrimation, blepharospasm.
• Complications: chronic (mechanical) conjunctivitis, conjunctival ulcer, superficial
vascularization & ulceration of the cornea.
Ectropion:
• Rolling of the eyelid outward (more common in lower lid)
• Causes: Cicatrial, Involutional, paralytic, mechanical & Congenital.
• Clinical picture: bad cosmetic appearance, exposure of the conjunctiva leads to
exposure conjunctivitis, exposure keratitis, watery eye, redness, crusting &
dermatitis of the skin.
• Complications: keratinization of the conjunctiva, ulceration & opacification of the
cornea.
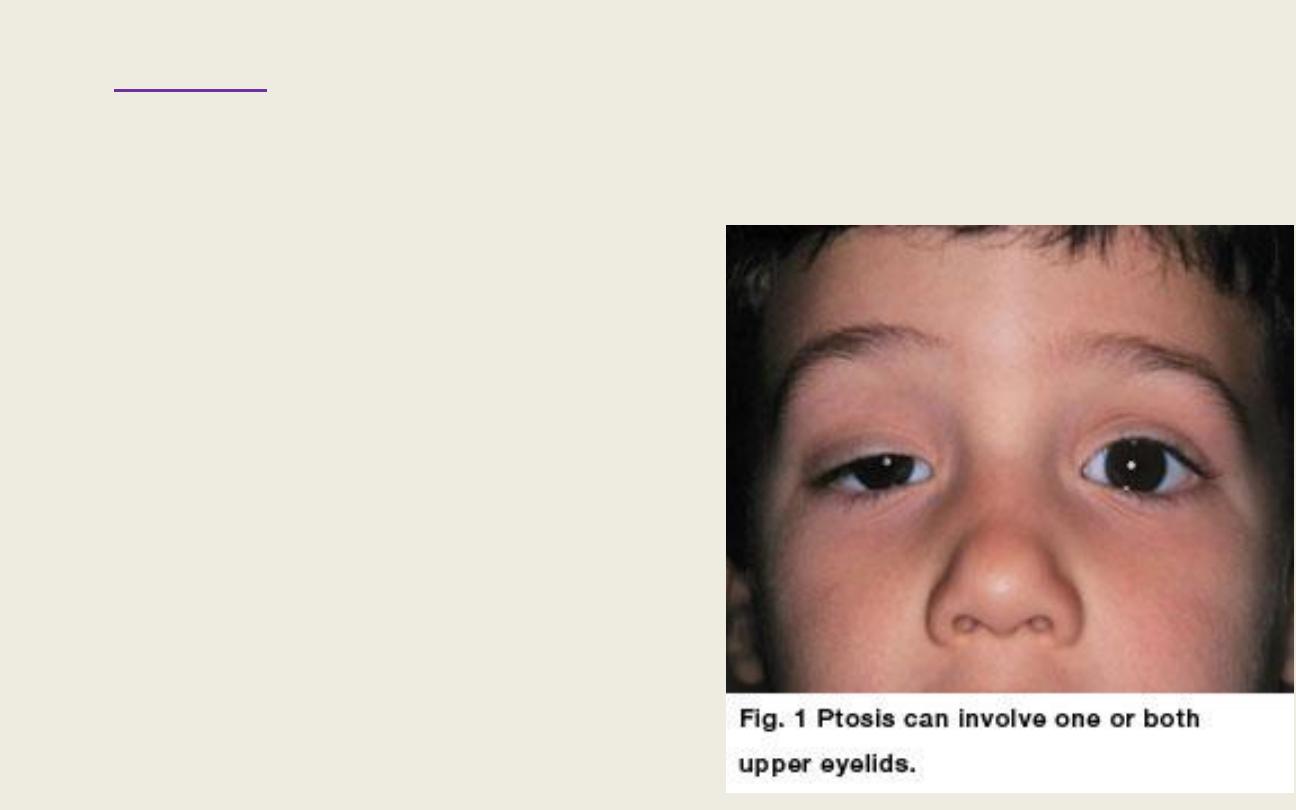
Ptosis
• Drooping of the upper lid that normally covers the upper 2mm of the cornea.
• Etiology: Neurogenic, myogenic, aponeurotic & mechanical.
• Causes:
Trachoma, VKC & lid tumor
Cicatricial (due to LPS & SR muscle fibrosis)
Trauma (collection of fluid)
Iatrogenic by surgeons.
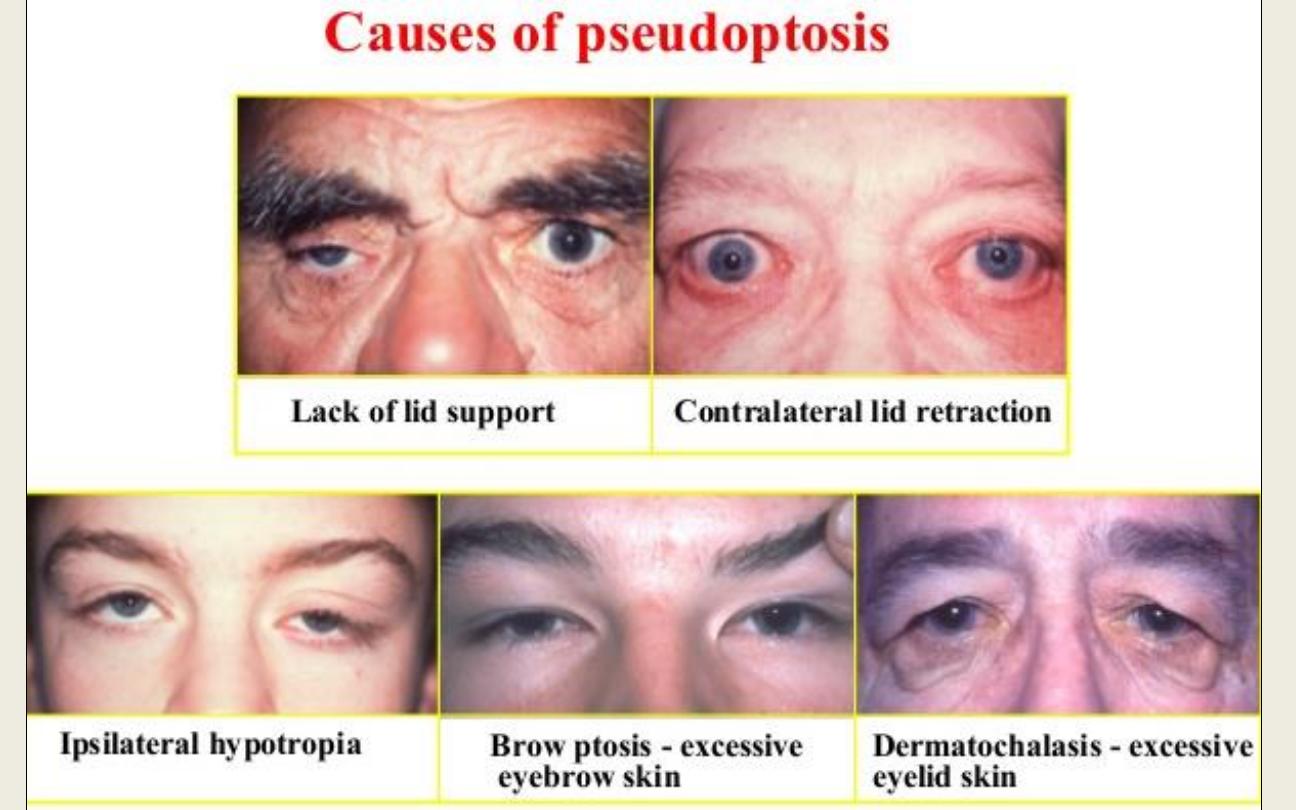
Pseudoptosis: occurs due to loss of support
e.g. enophthalmos.
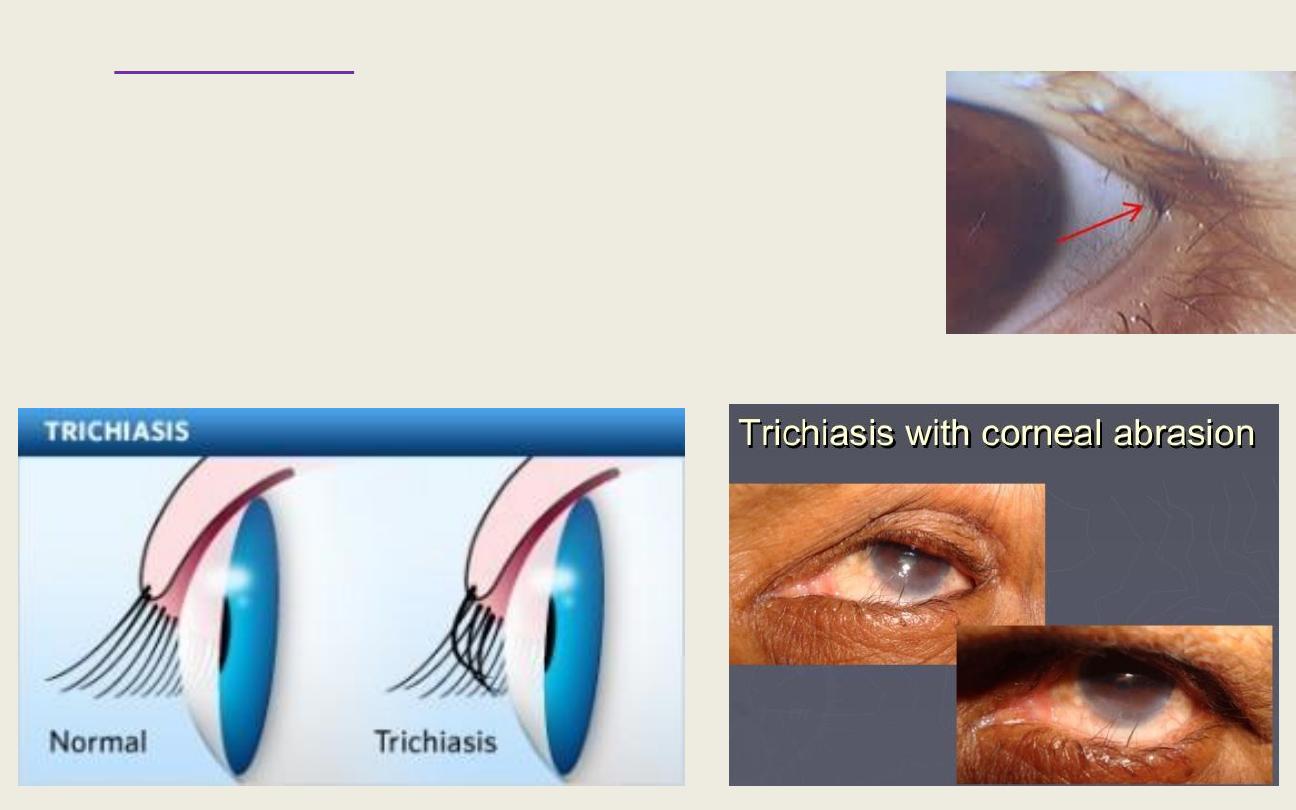
Trichiasis
• Posterior misdirection of lashes arising from normal site of
origin, it should not be mistaken for pseudotrichiasis which
occurs secondary to entropion.
1. Isolated
2. Secondary to scaring of the lid margin due to chronic
blepharitis herpes zoster ophthalmic & trachoma.

Madrosis
• Decrease in number or complete loss of lashes
• Causes:
Local: chronic blepharitis, burn, radiation, & infiltrating lid tumor.
Systemic: SLE, generalized alopecia, syphilis, leprosy, psoriasis.
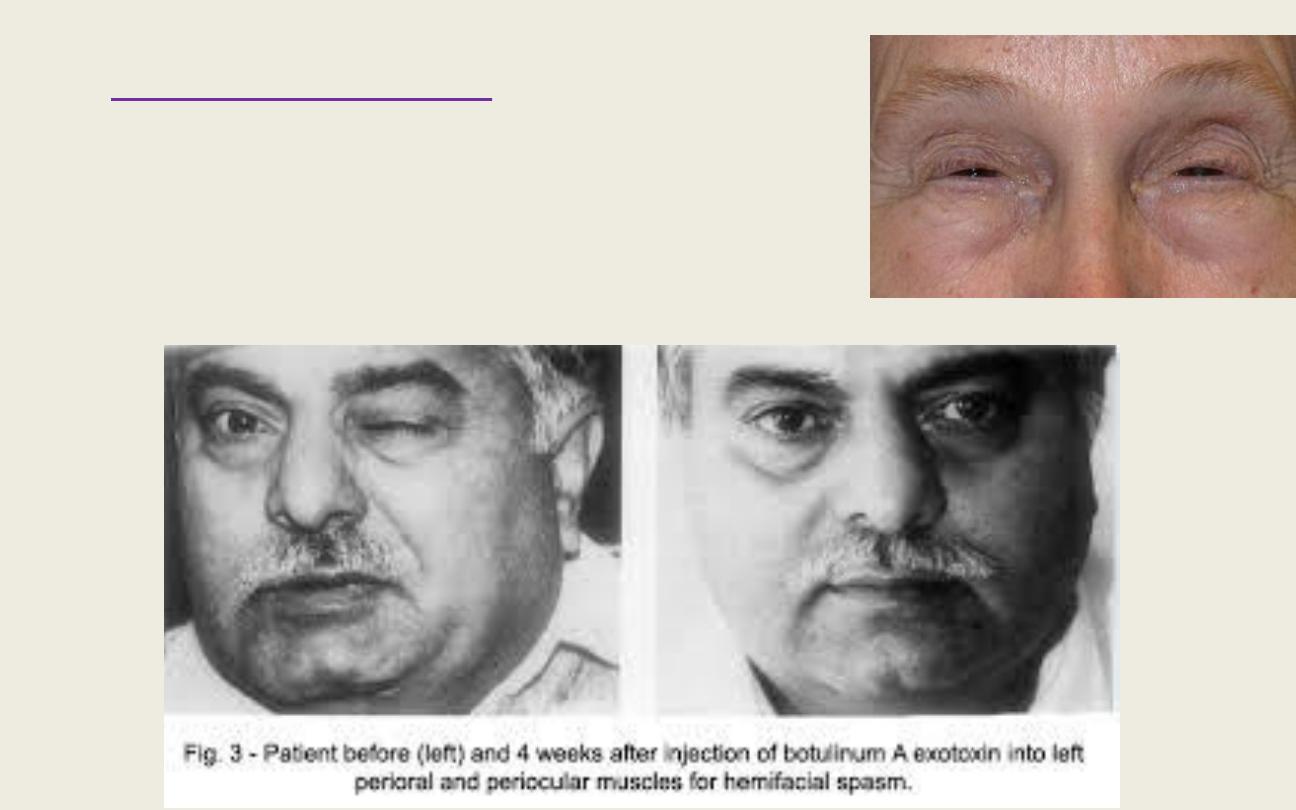
Blepharospasm
• Involuntary sustained closure of the eyelids which
occurs spontaneously (essential) or by sensory stimuli
(reflex).
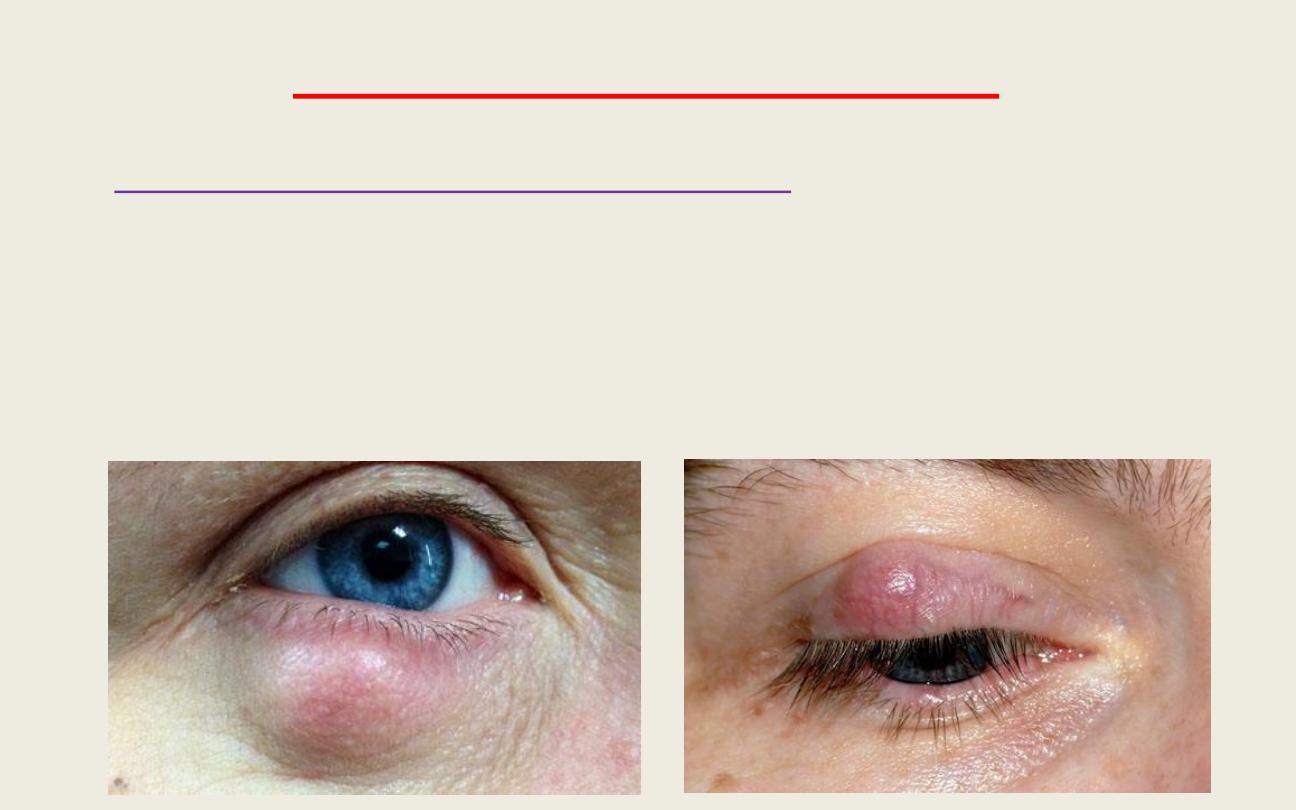
Benign nodules & cysts
Chalazion (Meibomian cyst)
• Chronic lipgranulomatous inflammatory lesion caused by blockage of meiboman
gland orifices & stagnation of sebaceous secretion, there is no infection
• It is more frequent & multiple in patients with acne, rosacea or seborrheic
dermatitis.
• Presentation: painless nodule & occasionally blurred vision.
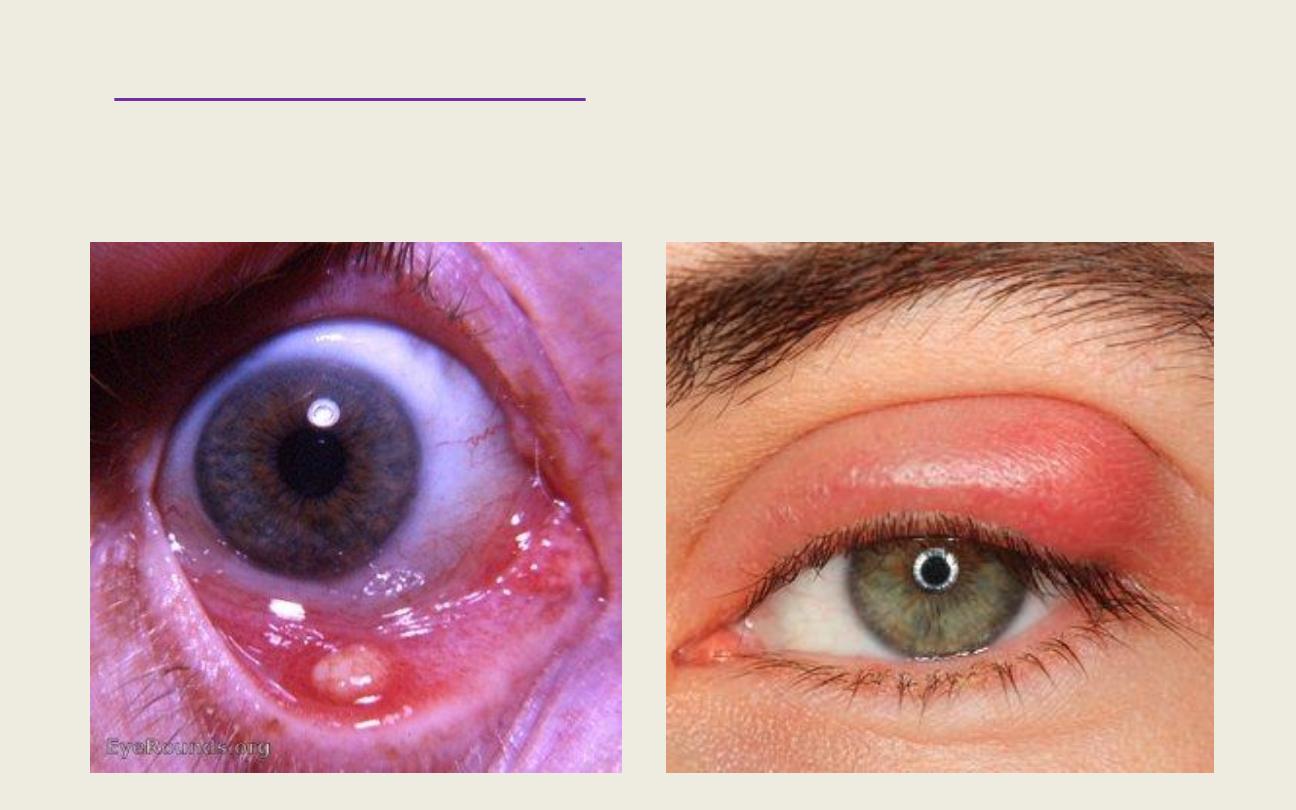
Internal hardeolum
• Small abscess caused by acute staphylococcal infection of meibomian glands.
• Signs: tender, inflamed swelling within tarsal plate.
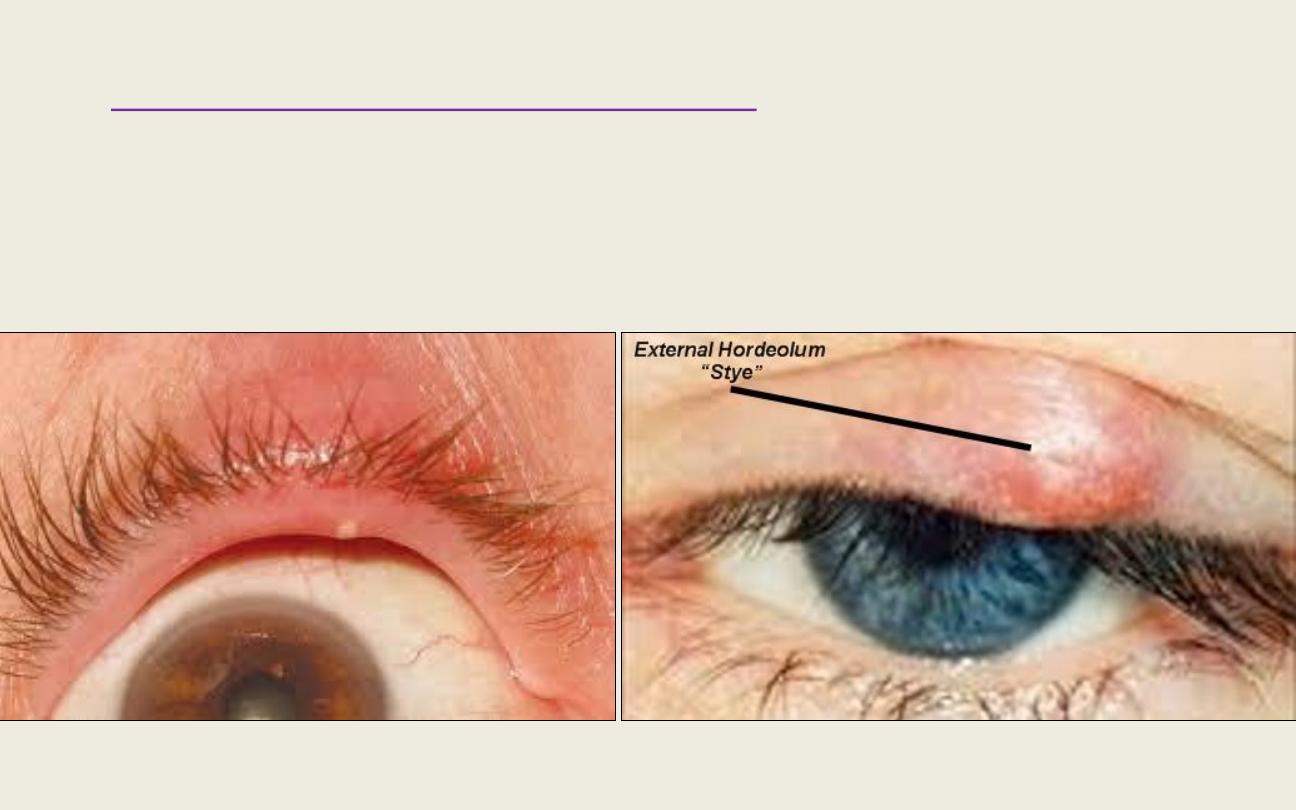
External hardeolum (Stye)
• Acute small staphylococcal abscess of lash follicle & its associated glands of Zeis.
• Signs: tender, inflamed swelling in the lid margin, which points anteriorly through
the skin. More than one lesion may present & occasionally minute abscess may
involve the entire margin.
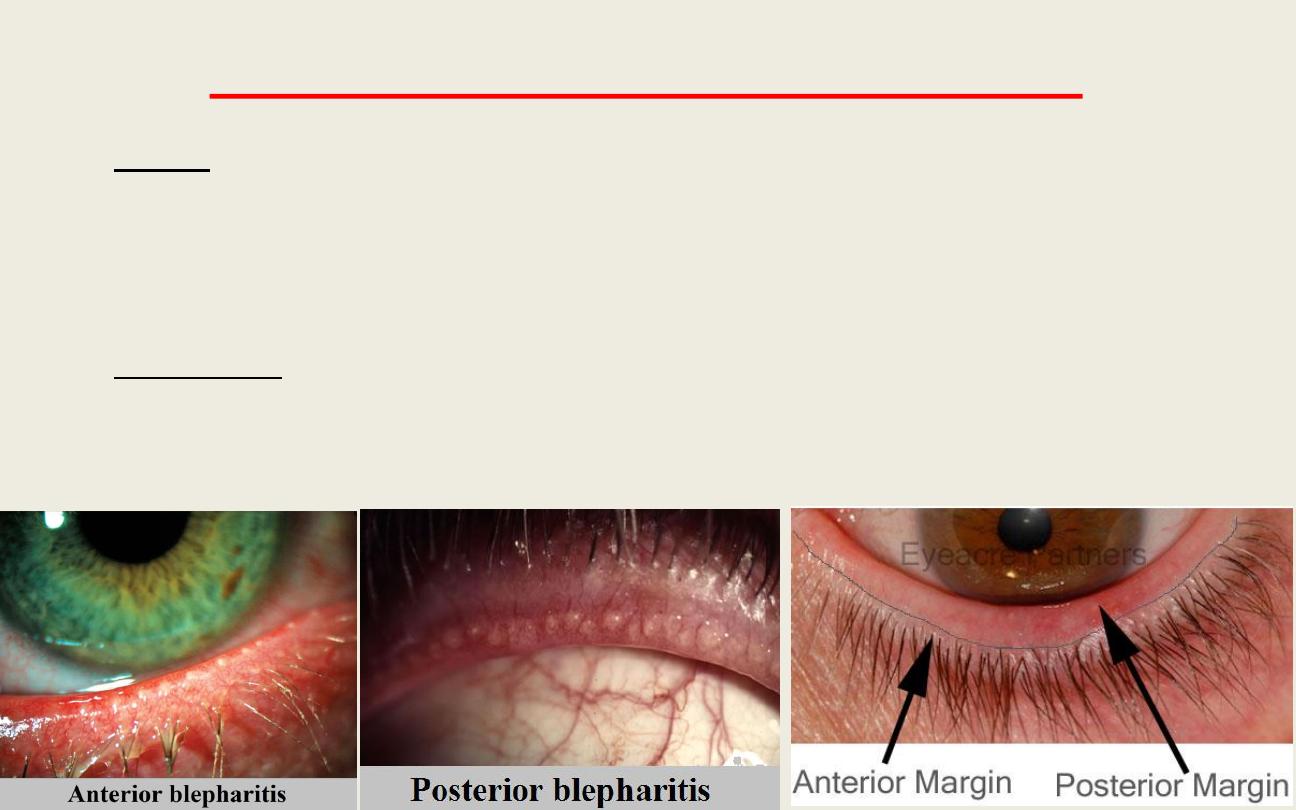
Marginal chronic blepharitis
• Types:
Anterior: Staphylococcus infection, seborrheic dysfunction or mixed.
Posterior: Meibomiantitis & Meibomian Seborrhea.
Mixed (any one of the anterior type plus any one of the posterior).
• Symptoms: burning, grittiness, mils photophobia ,and crusting & redness of
the lid margin. The symptoms are characterized by remissions &
exacerbations. Symptoms worse in mornings.
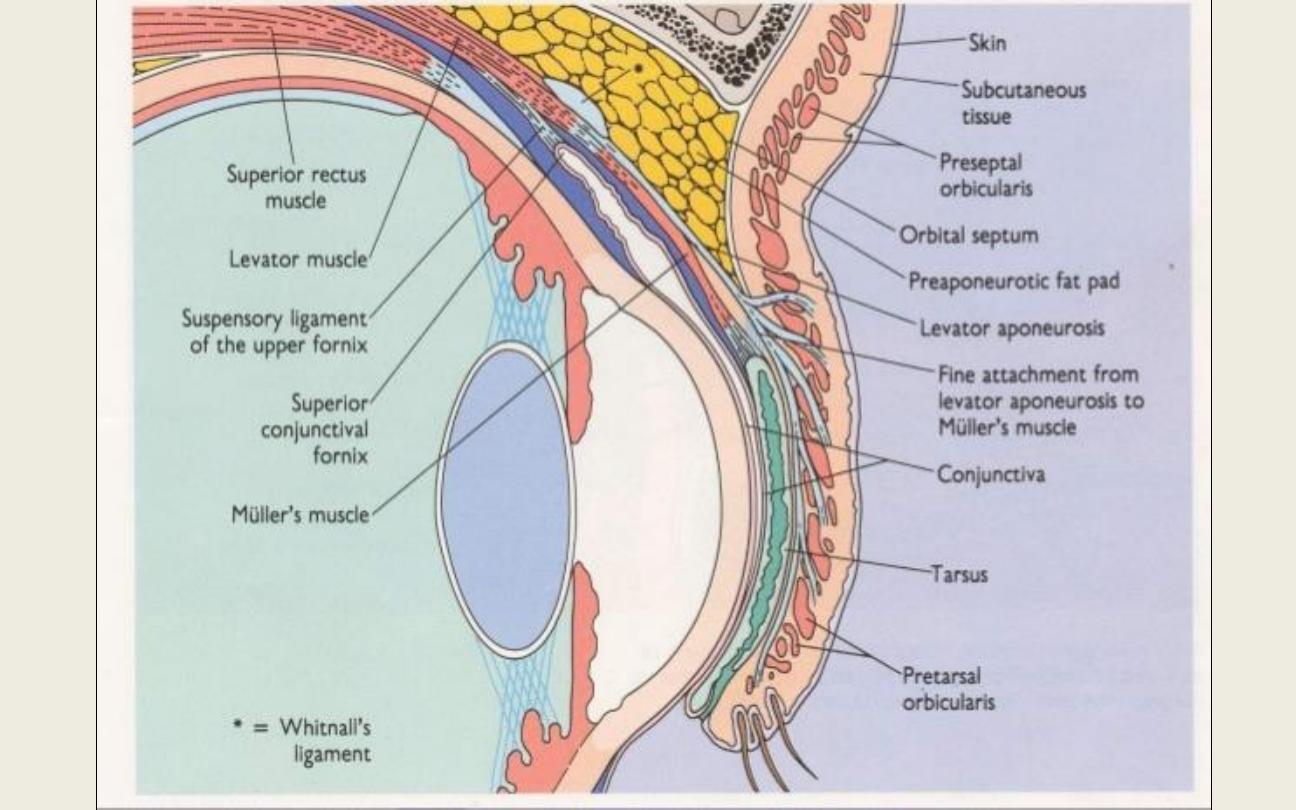
“Conjunctiva”
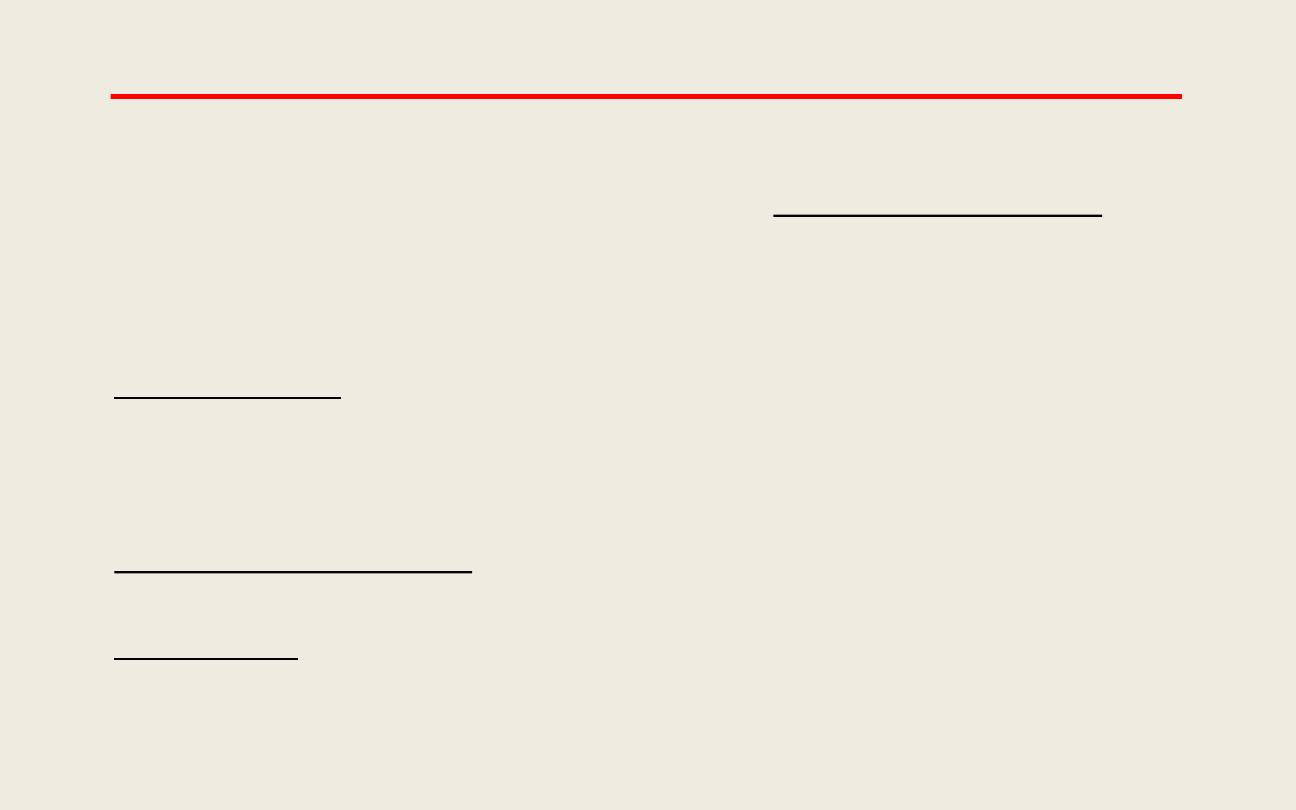
Applied anatomy of the conjuctiva
• Conjunctiva is a translucent mucous membrane cover the anterior sclera till the
limbus and lining the inner surface of the eyelid . It consists of two layers:
1) Epithelium: 2-5 cell layers.
2) Stroma (substantia propria): It is a richly vascularized connective tissue. Stroma
is made of 2 layers: a- superficial adenoid layer b- Deep thicker fibrous tissue.
• Mucin secretors: They are of three types: a- Goblet cells. b- Crypts of Henle:
Found at upper part of tarsal plate. c- Glands of Manz. Function: Lubrication.
Destructive disorders e.g. (cicatricial pamphygoid) causes decrease in number of
cells, while chronic inflammatory disorders increases the number of the cell.
• Accessory lacrimal glands: a- Krause. b- Wolfring.
They are found deep in stroma mainly at fornices.
• Clinical parts:
a- Palpebral: starts at the mucocutaneous junction, it is firmly adherent to the
tarsal plate. b- Forniceal: loose, redundant part, it swells easily.
c- Bulbar: it covers the anterior surface of sclera.
Clinical Evaluation of conjunctival
inflammation:
The differential diagnosis of conjunctival inflammation depends on:
1) Symptoms:
• Conjunctivitis has non-specific symptom such as:
lacrimation, irritation, stinging, burning.
(visual acuity is not affected as conjunctivitis is away from visual axis).
• If it is associated with keratitis, there will be
pain, photophobia & marked foreign body sensation and
sometimes blurred vision (as cornea is affected).
• In allergic conditions,
the hallmark is itching, which also occurs in blepharitis (inflammation of lid
margin) and
keratoconjunctivitis sicca.
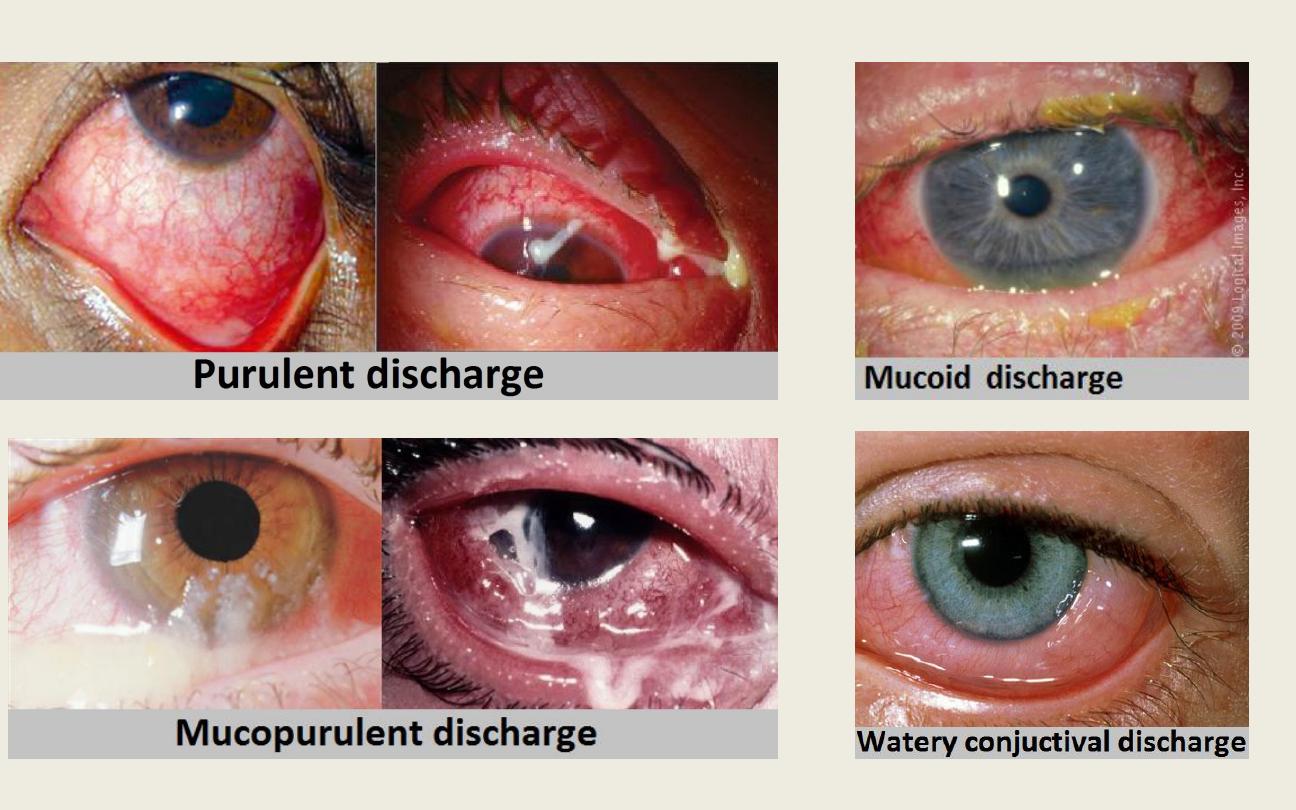
2) Discharge:
• It is exudates filtered through conjunctival epithelium from dilated blood vessels
with additional epithelial debris, mucus and tear.
a) Watery: Serous exudates and reflexly secreted tear. Associated with: - Acute viral
conjunctivitis. - Allergic conjunctivitis.
b) Mucoid: Associated with: - Vernal conjunctivitis. - Keratoconjunctivitis sicca.
c) Purulent: Severe acute bacterial conjunctivitis.(Gc conjunctivitis)
d) Mucopurulent: - Mild bacterial conjunctivitis. - Chlamydial infections.
3) Conjunctival Appearance:
a) Conjunctival injection:
• Can give a clue in diagnosis although it is a non-specific feature, in which, the
beefy-red conjunctiva suggests a bacterial cause (especially in the inferior fornix).
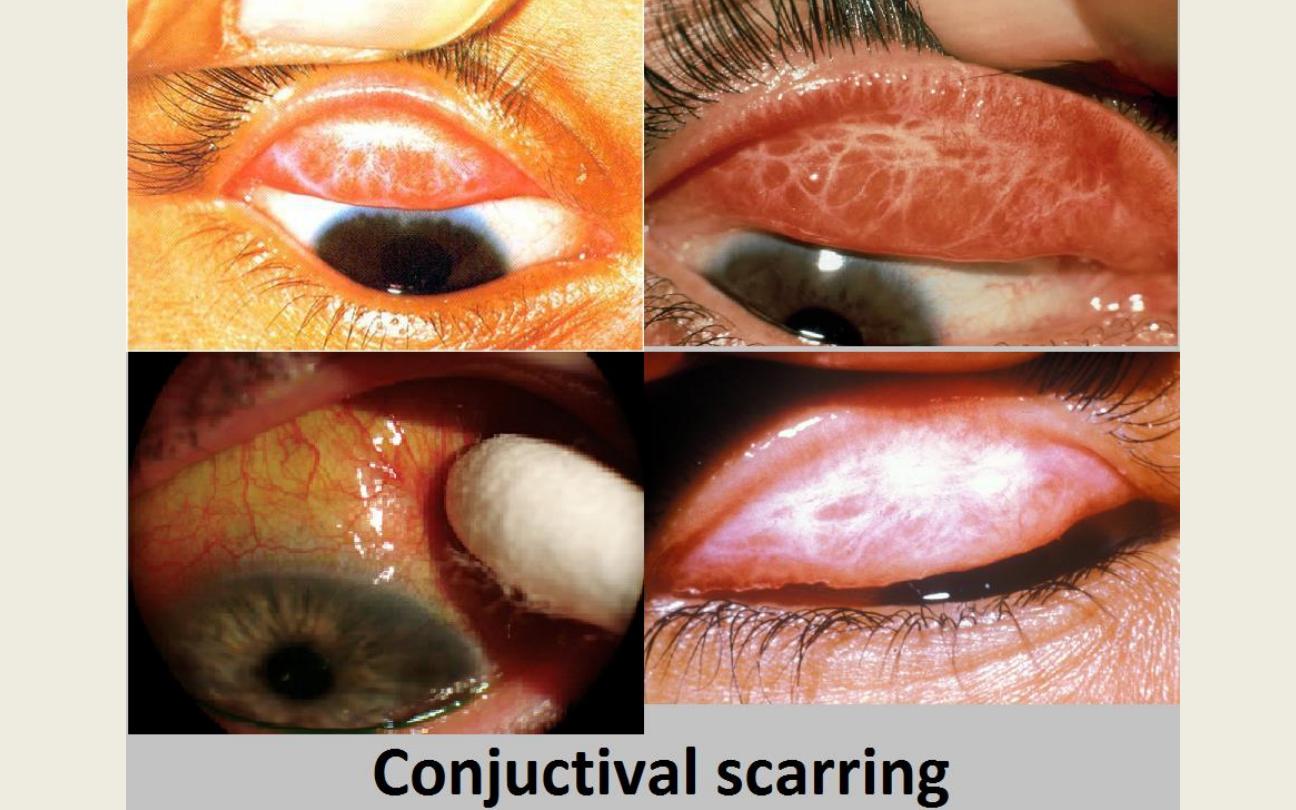
b) Subconjunctival haemorrhages:
• Mostly associated with:
Viral infection, e.g.: Adenovirus, Acute haemorrhagic conjunctivitis.
Bacterial infection, e.g. Streptococcus pneumoniae.
c) Follicular reaction:
• It is seen by magnification by slit-lamp, consists of hyperplasia of lymphoid tissue
within the stroma, commonly occurs in (inferior) forniceal conjunctiva.
• Clinically: It is seen as multiple, discrete, slightly elevated lesions, reminiscent of
small grains of rice, each follicle is encircled (surrounded) by a tiny blood vessels.
• The main causes are (differential diagnosis): - Viral infections. - Chlamydial
infections. - Parinaud oculoglandular syndrome. - Hypersensitivity to topical
medications.
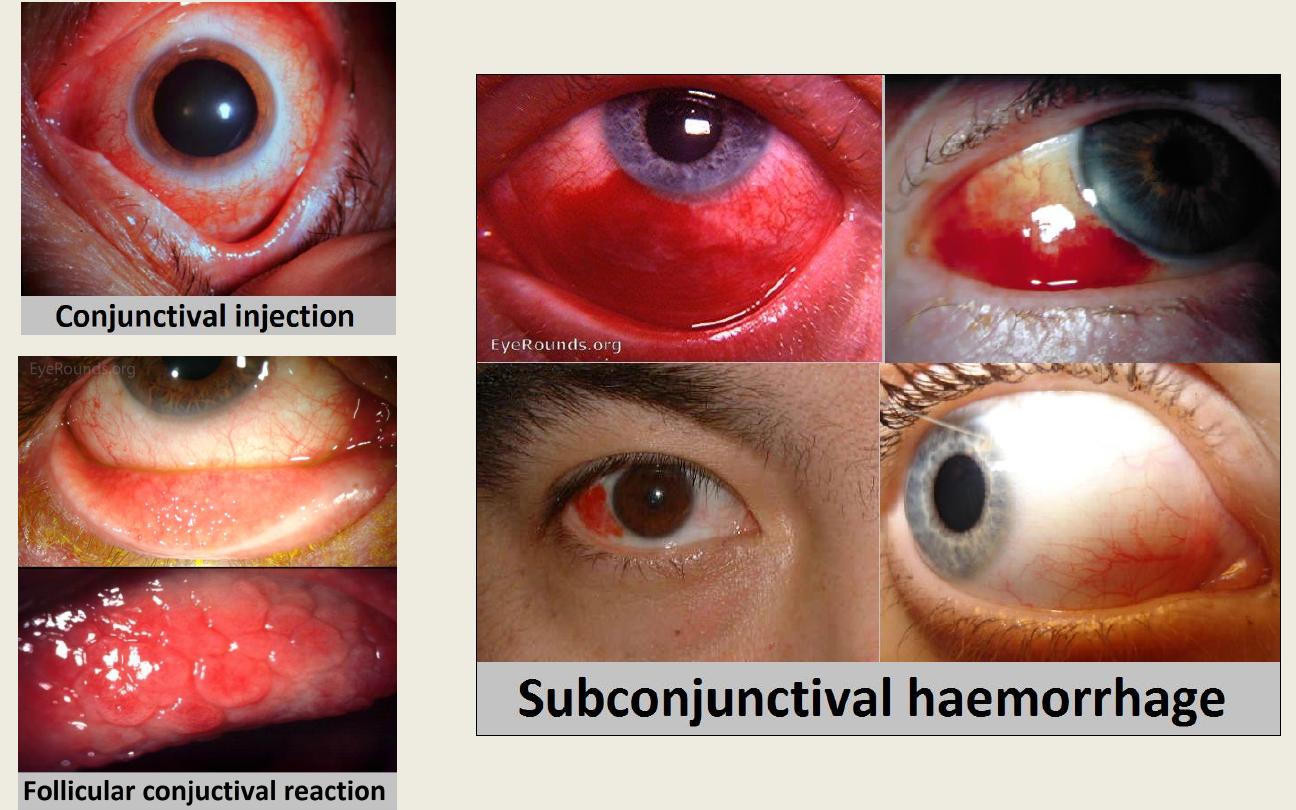
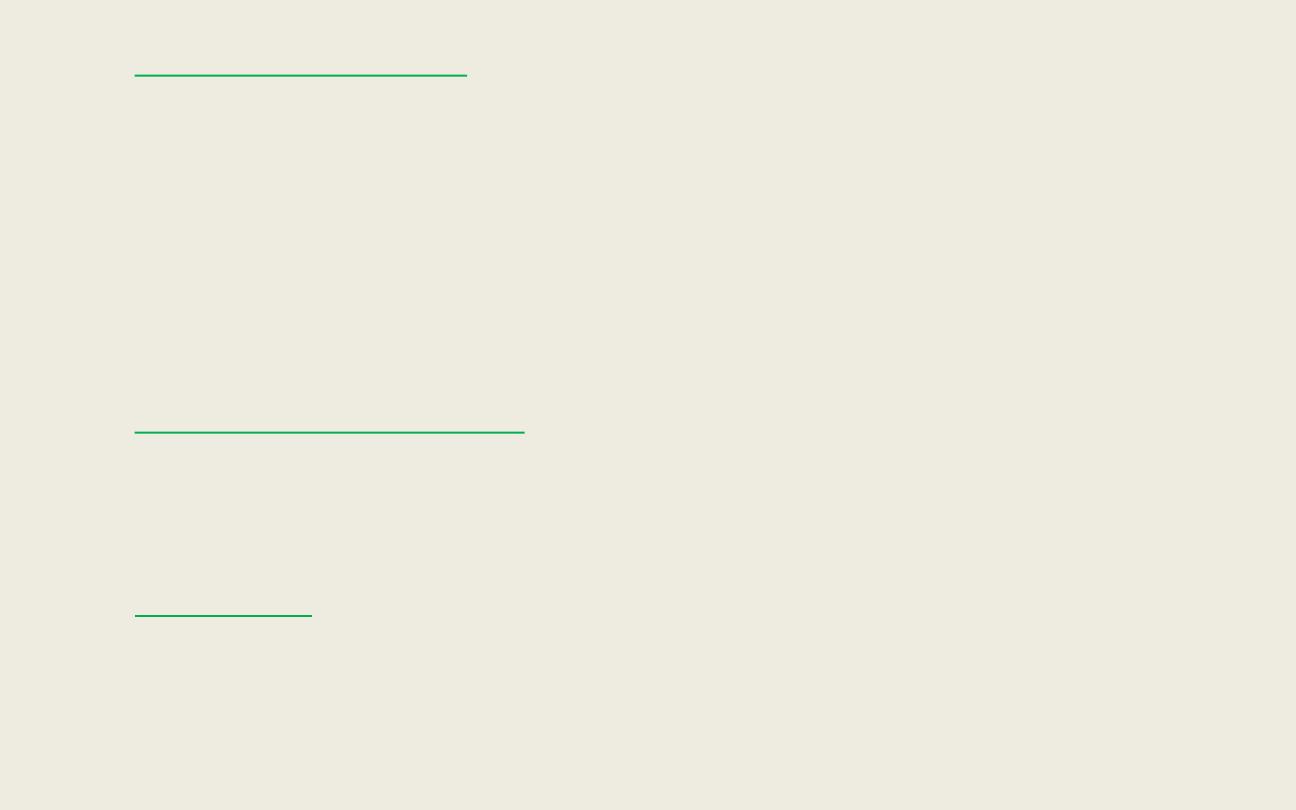
d) Papillary reaction:
• It is of less diagnostic value than follicular reaction. It is hyperplasia of conjunctival
epithelium (surrounding a core of blood vessels) thrown into numerous folds or
projections. Commonly occurs in the upper palpebral conjunctiva.
• Clinically seen as a fine mosaic-like pattern of elevated polygonal hyperemic areas
separated by paler channels.
• Main causes are: - Chronic blepharitis - Allergic conjunctivitis
- Bacterial conjunctivitis. - Contact lens-related problems.
e) Oedema (chemosis):
• Whenever the conjunctiva is severely inflamed. It is transudation of fibrin and
protein-rich fluid through the walls of the damaged blood vessels producing a
translucent swelling of the conjunctiva.
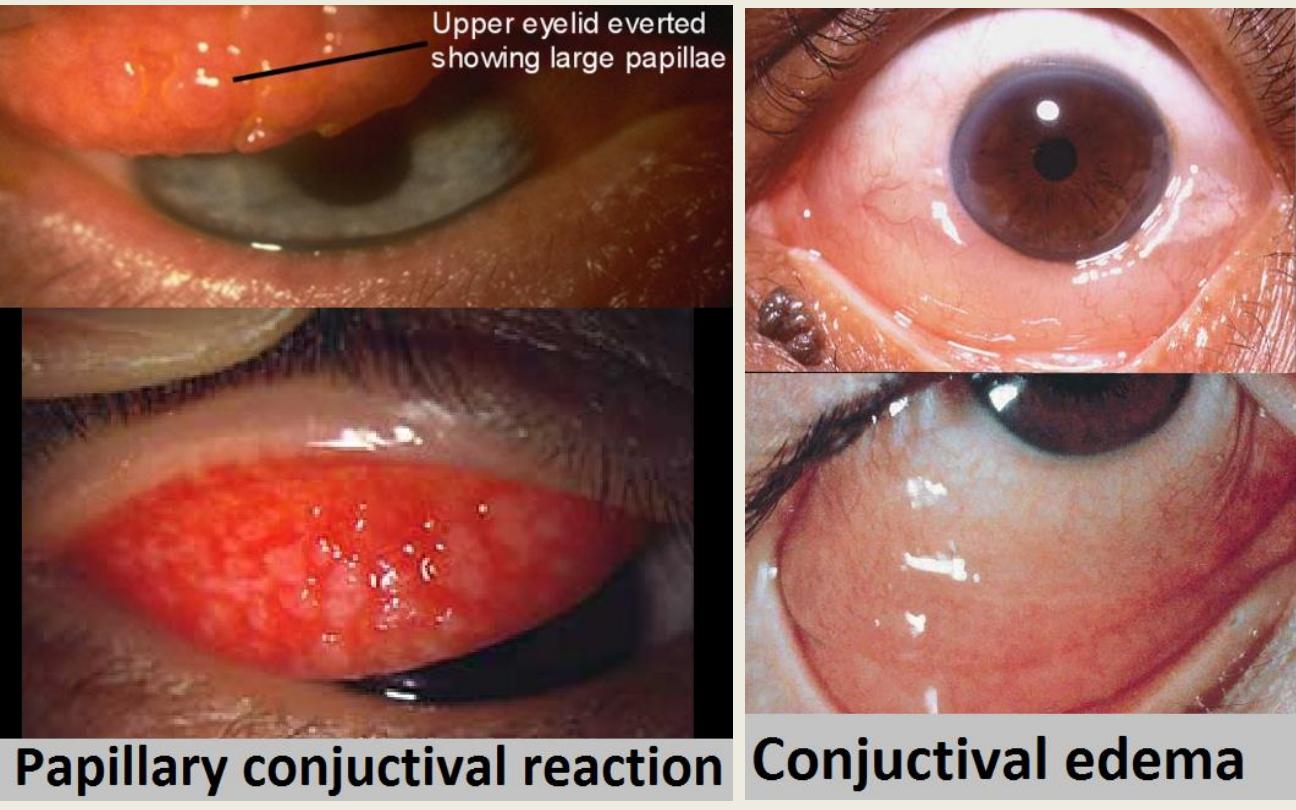
e) Scarring:
• its causes are: - Trachoma. - Ocular cicatricial pemphigoid.
- Atopic conjunctivitis. - Prolonged use of topical medications.
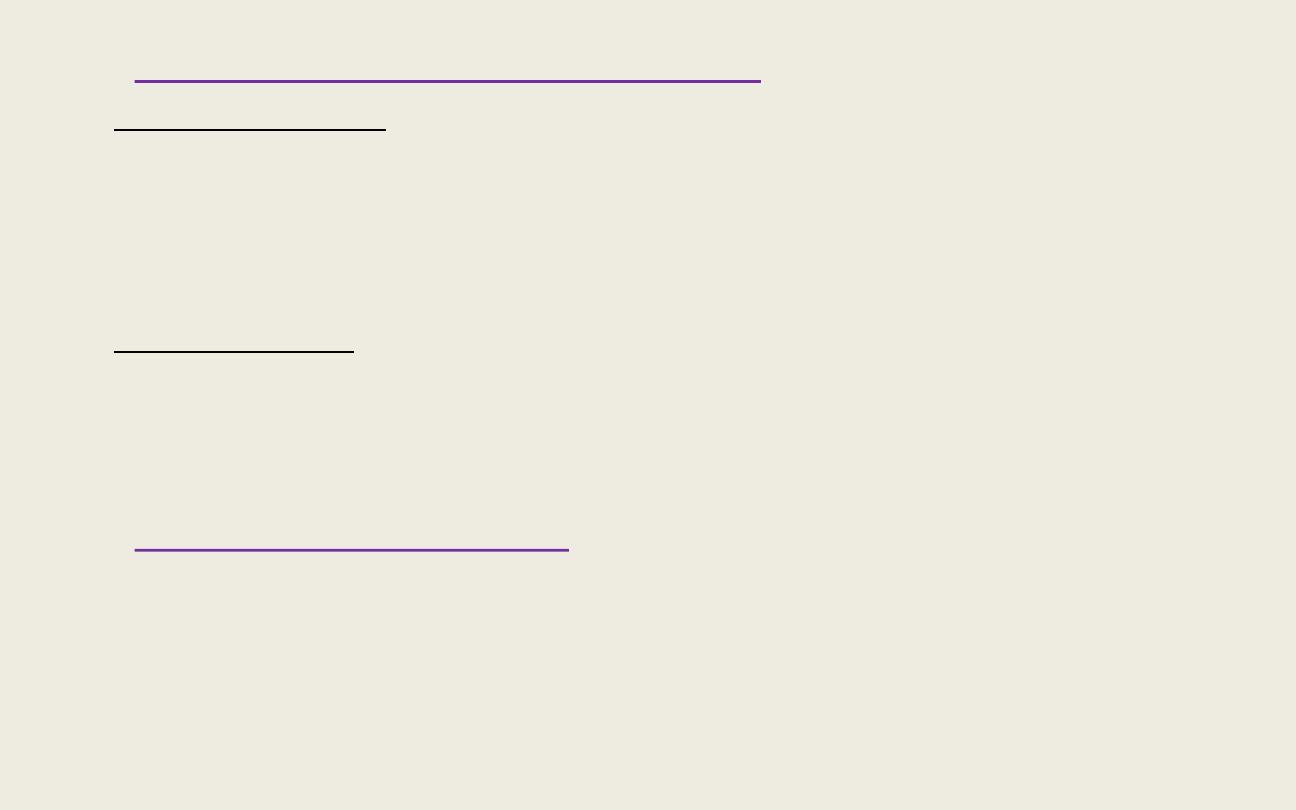
4) Conjunctival membranes:
• Pseudomembranes:
Coagulated exudates adherent to the inflamed conjunctival epithelium, peeled off
leaving the epithelium intact (or healthy).
- Severe adenoviral infection. - Gonococcal conjunctivitis.
- Steve-Johnson syndrome. - Ligneous conjunctivitis.
• True membranes:
When inflammatory exudates permeates the conjunctival epithelium. Removal of
membranes may be accompanied tearing of the epithelium and bleeding.
- Beta-haemolytic Streptococci. - Diphtheria.
5) Lymphadenpathy:
• The upper and lower lids with eyeball and other structures drains to the
preauricular and submandiblar lymph nodes.
• These lymph nodes are swollen in these cases: - Viral infections. - Chlamydial
infections. - Severe Gonoccocal infections. - Parinaud syndrome.
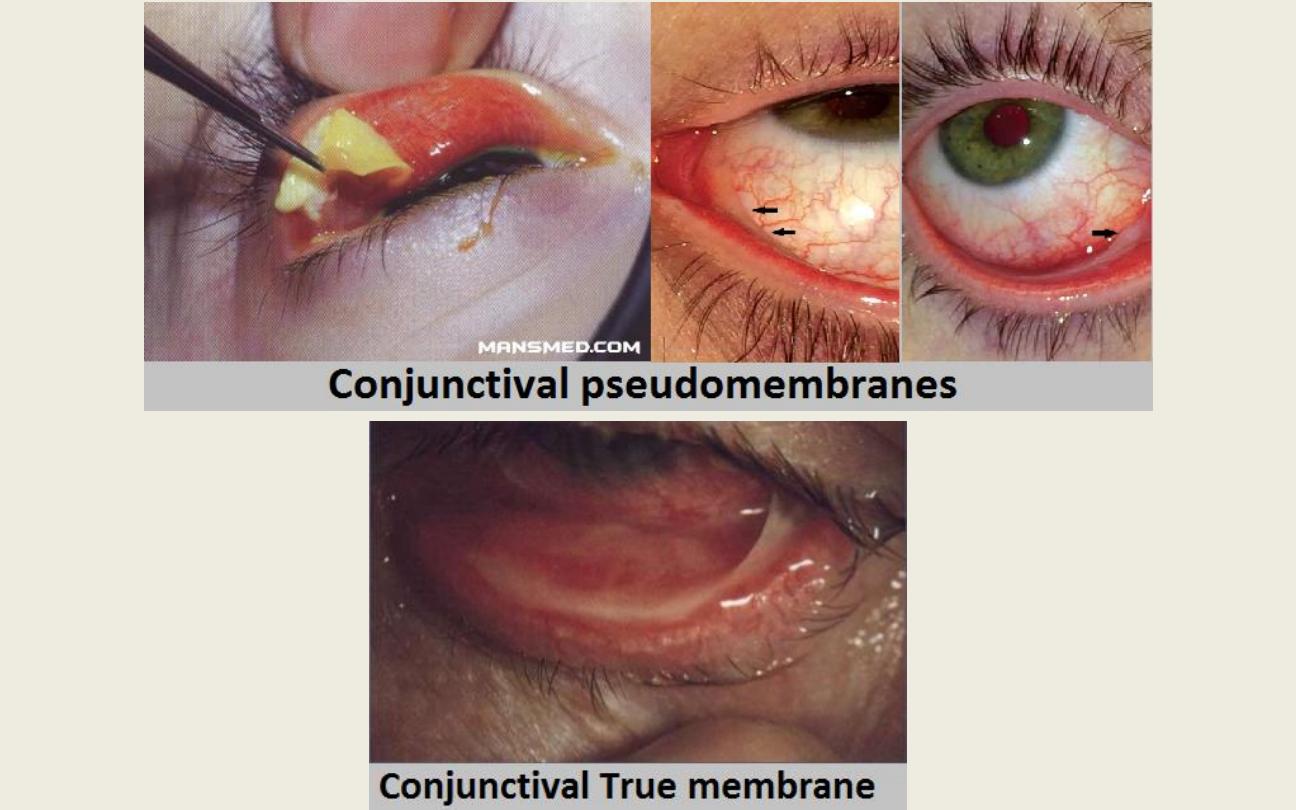
Bacterial Conjunctivitis
Simple bacterial conjunctivitis:
• Symptoms: - Acute onset of redness - Grittines - Burning.
- Discharge - On morning, eyelids are stuck together due to
accumulation of exudates during the night.
- Both eyes are usually involved.
• Signs: - The eyelids are crusted and oedematous (mild oedema).
- Mucopurulent discharge. - Beefy-red injection, maximally in the fornices.
- Membranes in severe cases. - Corneal involvement is uncommon.
- Blurred vision may occur due to mucus not due to corneal involvement.
• Treatment:
Usually resolves within 10-14 days. - Bathe all discharge away.
Topical drops (Antibiotics): Chloramphenicol, ciprofloxacin, ofloxacin, gentamicin,
neomycin, tobramycin.
Antibiotic ointments: chloramphenicol, gentamicin, tetracydine, framycetin.
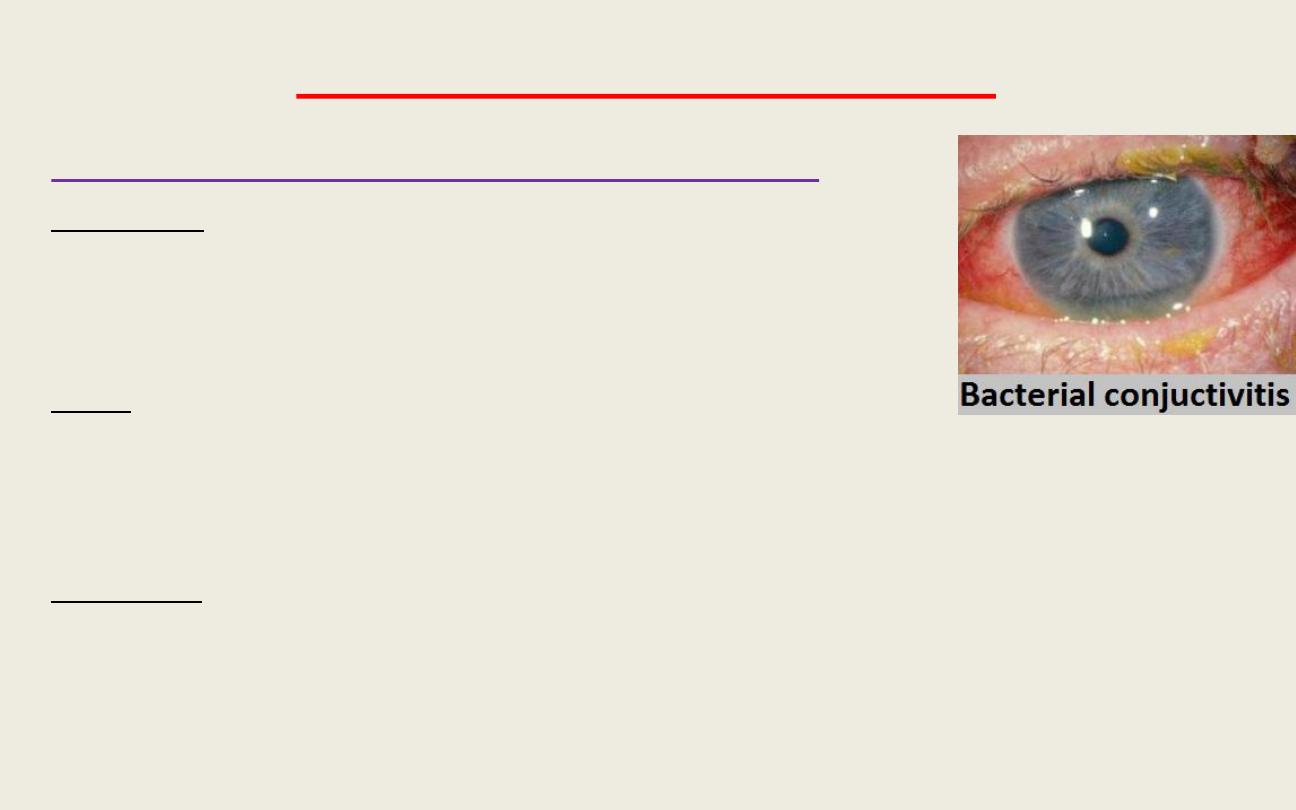
Adult gonococcal
keratoconjunctivitis:
• Symptoms: - Hyperacute presentation. - Profuse and thick
creamy (purulent) pus.
• Signs:
* Eyelids are oedematous and tender. - Discharge is
profuse & purulent. * Intense hyperaemia (conjunctival
injection), chemosis and pseudomembranes format.
* Preauricular lymphadenopathy & sometimes suppuration
of nodes. * Keratitis may occur in severe cases
• Treatment:
Hospitalization (we should admit this patient to hospital).
Cultures (means all investigations).
Eye irrigation with saline (frequent)
Antibiotics: i- Systemic antibiotics: Cefoxitin or cefotaxime.
Spectinomycin in penicillin-resistant cases.
ii- Topical Antibiotics: Gentamicin, or Bacitracin.
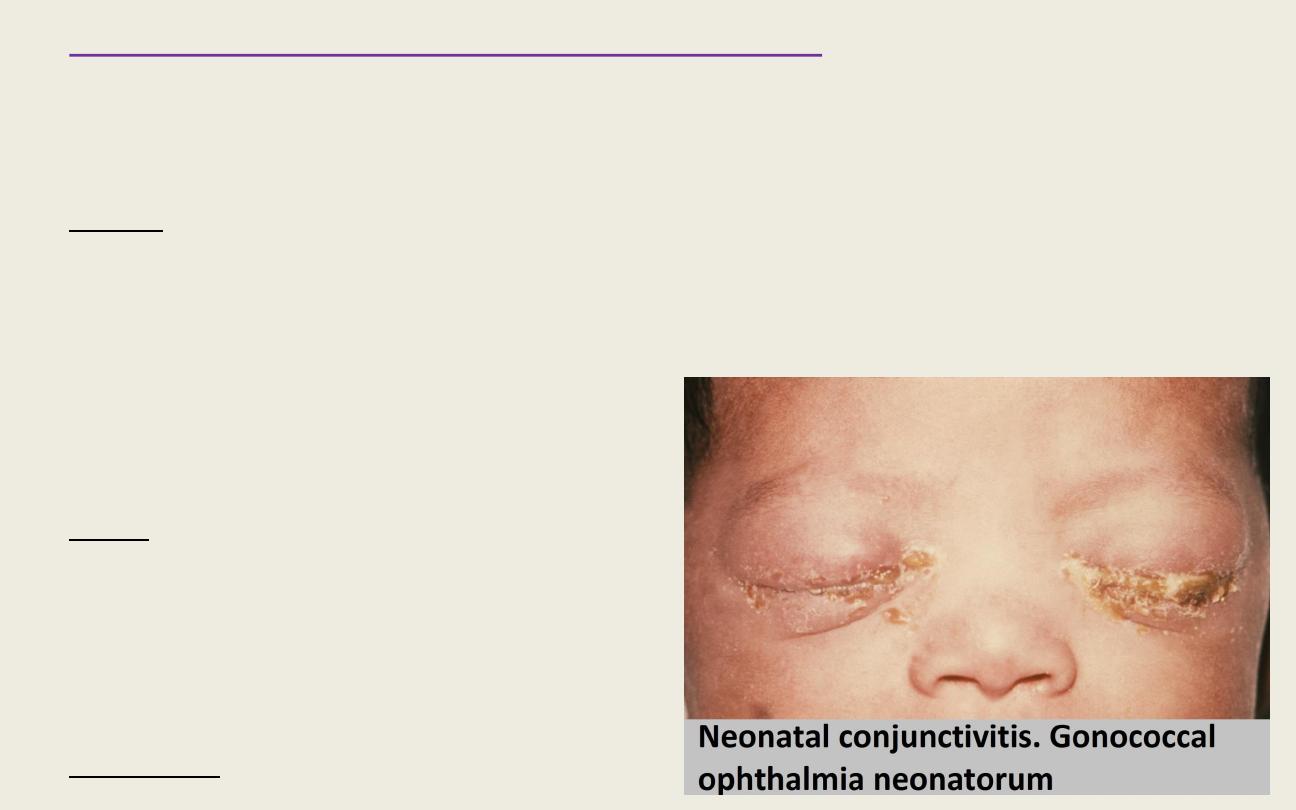
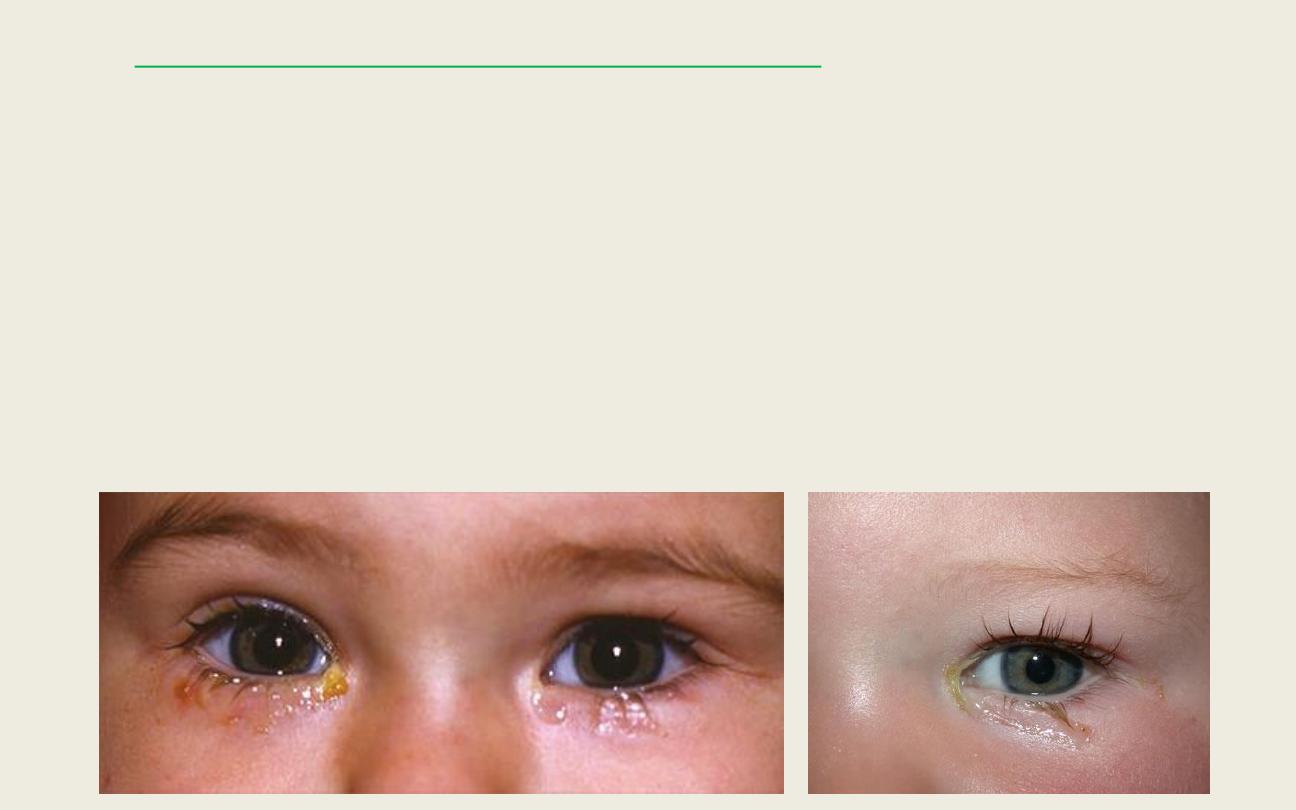
Neonatal Keratoconjunctivitis:
• Ophthalmia neonatorum is any infection of the eye within
one month from birth. Often transmitted infection from
mother to infant.
• Causes;
C.trachomatus, N.gonorrhea, occasionally HSV2,
Staphylococcus, strept., H.influenza & other G.-ve bacteria.
Chemical irritation by topical preparation used as
prophylaxis against infection.
Congenital NLD obstruction: can produce
recurrent mild bacterial conjunctivitis.
• Signs:
Hyperacute presentation.
Chemosis.
Pseudomembranes.
Corneal involvement.
• Treatment: Systemic and topical antibiotics.
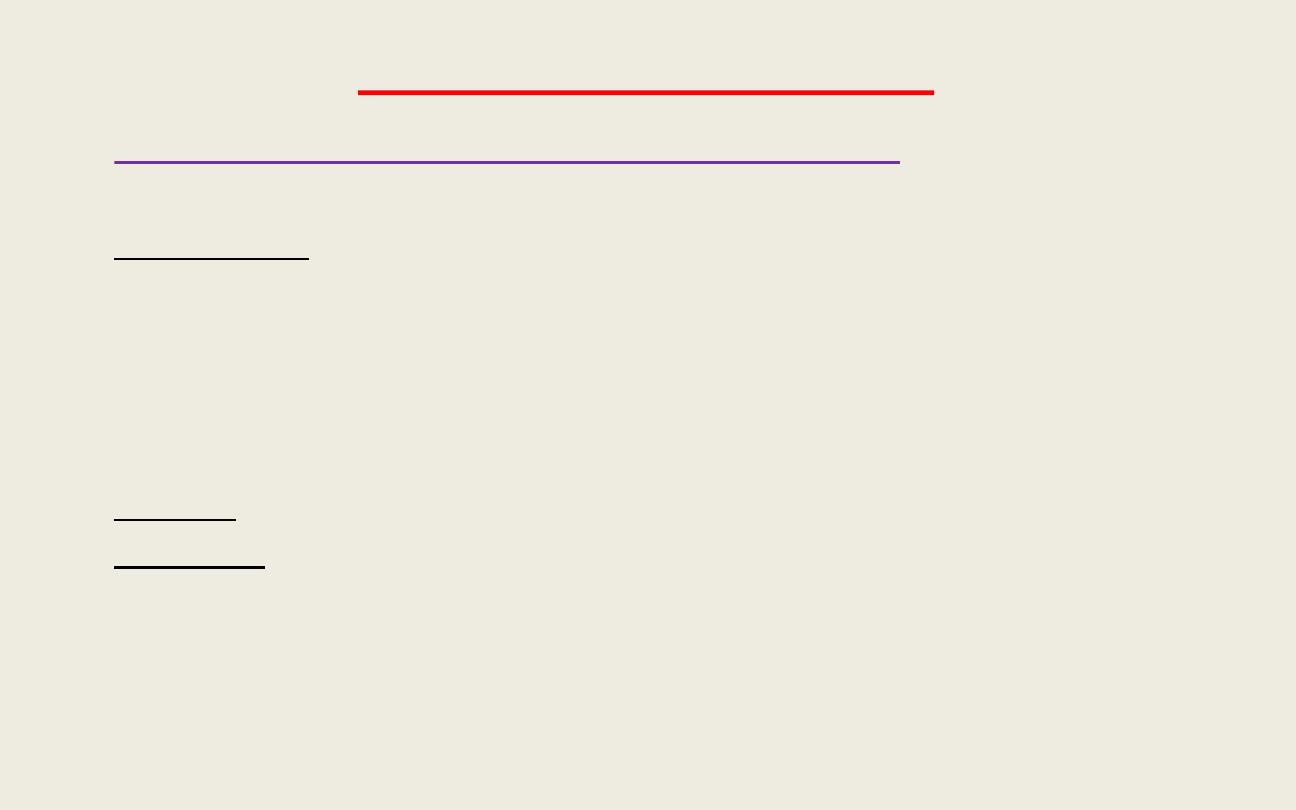
Viral Conjunctivitis
Adenoviral keratoconjunctivitis:
• highly contagious virus. - Transmission is via respiratory or ocular secretion.
• Conjunctivitis:
Presentation: acute onset of watery discharge, redness, discomfort and
photophobia, both eyes are affected in 60% of cases.
Signs: - Eyelids are oedematous. - Watery discharge. - Mild chemosis to moderate.
- Follicular reaction. - Subconjunctival haemorrhages. - Pseudomembranes.
- Lymphadenopathy is tender.
• Keratitis: Corneal sub epithelial infiltration and opacification.
• Treatment:
Avoid transmission following examination of patients:
o Washing of hands.
o Meticulous disinfection of ophthalmologic instruments.
o Infected hospital personnel should not be in contact with patients.
Medications:
o For conjunctivitis:
Spontaneous resolution occurs within 2 wks
Antiviral agents are ineffective (has no role).
Topical steroids are indicated only in very
severe inflammations and when Herpes
simplex infection has been excluded. The
treatment with steroids is symptomatic and
supportive (not used routinely).
o For keratitis:
Topical steroids, which are indicated only if
the eye is uncomfortable or there is
diminishing of the visual acuity by corneal
sub epithelial infiltrates and opacifications,
Steroids should not be used till exclusion of
Herpes simplex infection.
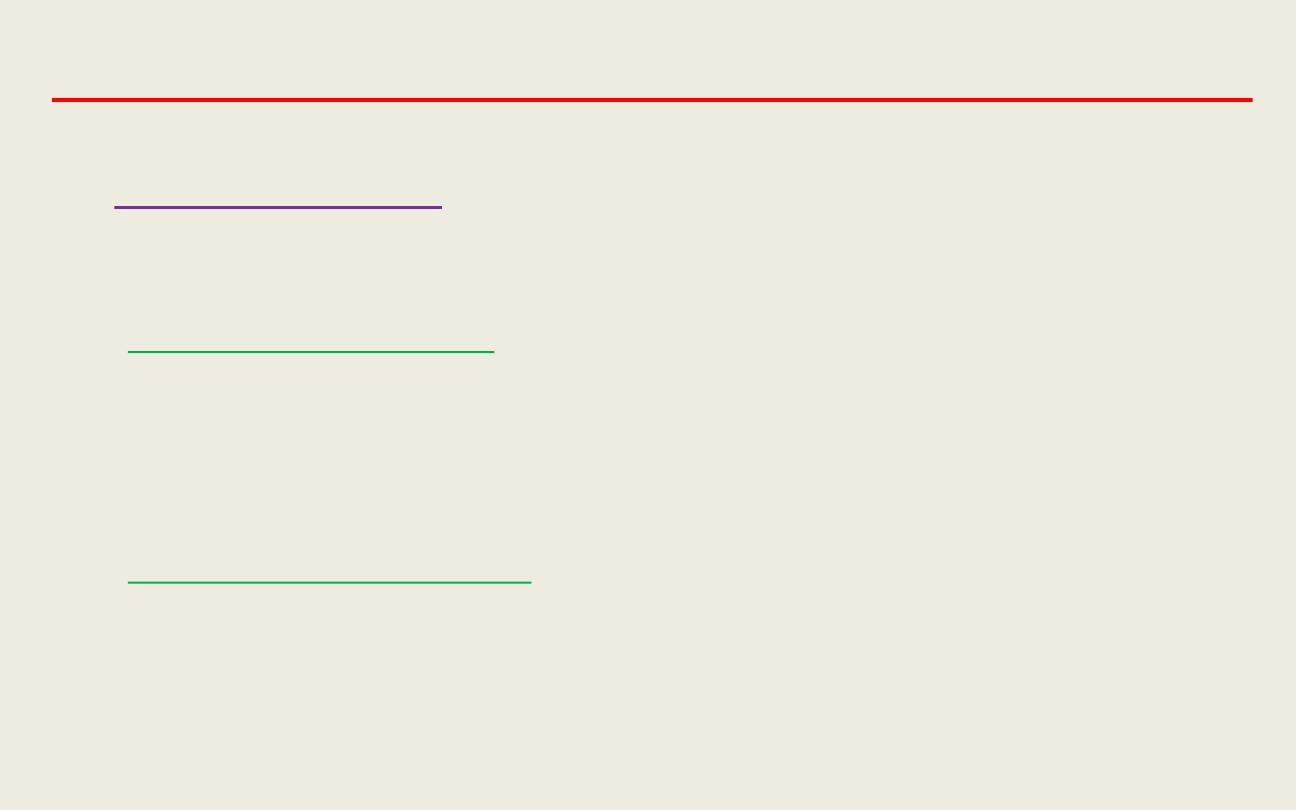
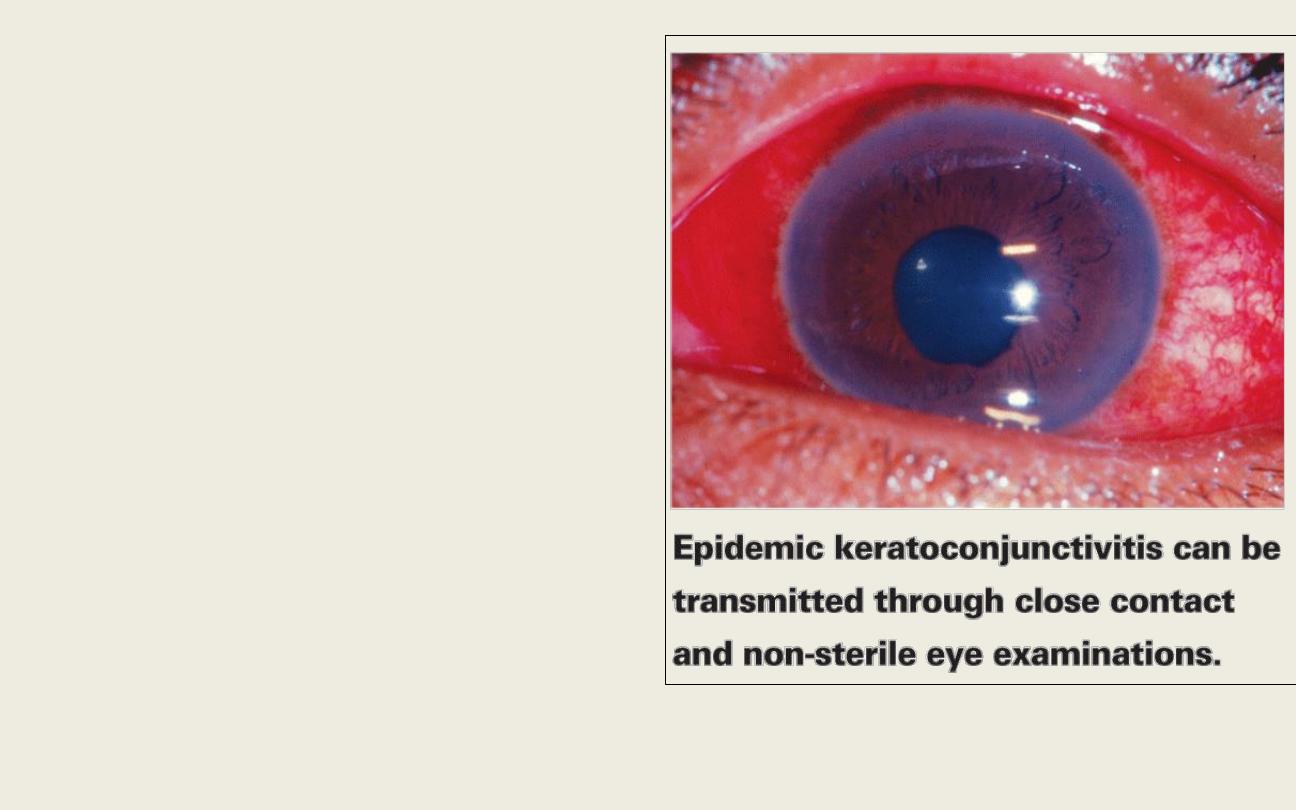
Herpes simplex conjunctivitis:
• Conjunctivitis may occur in patients with primary Herpes simplex infection.
• Signs:
The eyelids and periorbital skin show unilateral herpetic vesicles, which may be
associated with edema.
Watery discharge.
Ipsilateral follicular reaction.
Lymphadenopathy is tender.
Keratitis is uncommon.
Herpes simplex infection is very severe and it
can lead to dendritic ulcer of the cornea.
No subconjunctival hemorrhage.
• Treatment:
Antiviral agent (as Acyclovir "Zovirax™") for
21 days to prevent keratitis.
Chlamydial Conjunctivitis
Adult chlamydial Keratoconjunctivitis:
• It is a sexually transmitted disease caused by the obligate intracellular bacterium
Chlamydia trachomatis. Mode of transmission: - Autoinoculated from genital
secretions. - Eye to eye spread is rare.
• Presentation: Subacute onset of unilateral or bilateral mucopurulent discharge.
Chronic infection if not treated
• Signs:
- Eyelids are lightly oedematous. - Mucopurulent discharge.
- Large follicles are formed at the inferior fornix. - Lymphadenopathy.
- Keratitis is uncommon, if it occurs: Epithelial Keratitis, Subepithelial keratitis
(opacities), Marginal infiltrates & Conjunctival scarring + Pannus
• Treatment:
a- Topical therapy: Tetracycline ointment
b- Systemic therapy: One of: i- Doxycycline: ii- Tetracyclinec. Azithromycine
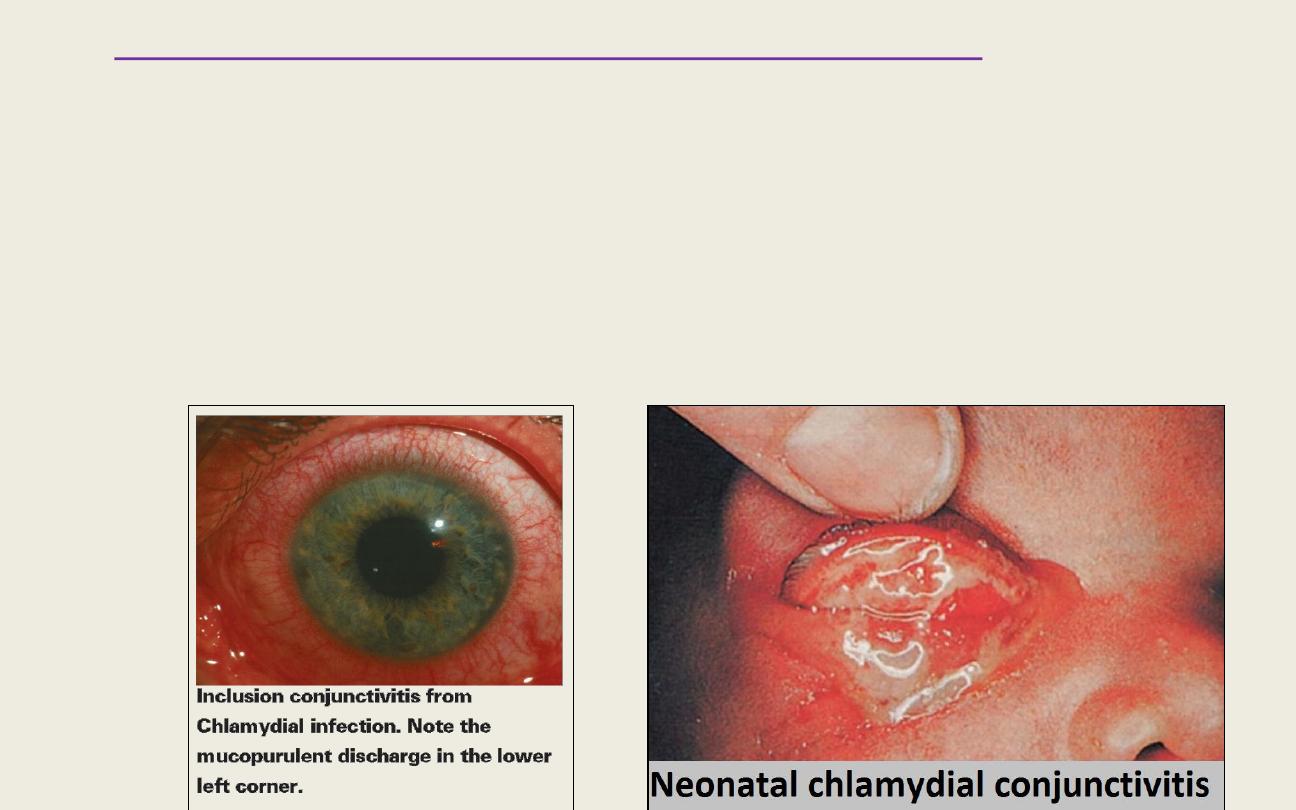
Neonatal chlamydial conjunctivitis:
• The most common cause of neonatal conjunctivitis (ophthalmia Neonatorum).
• It is transmitted from the mother genital tract during delivery.
• Presentation: The child is usually presented between 5 & 19 days after birth.
• Signs: - Papillary conjunctivitis (there is no follicular reaction as the lymphoid
tissue develops 3 months after delivery). - Mucopurulent discharge.
• Complications (if not treated): Conjunctival scarring & superior corneal pannus.
• Treatment: a- Topical Erythromycin. b- Oral Erythromycin.
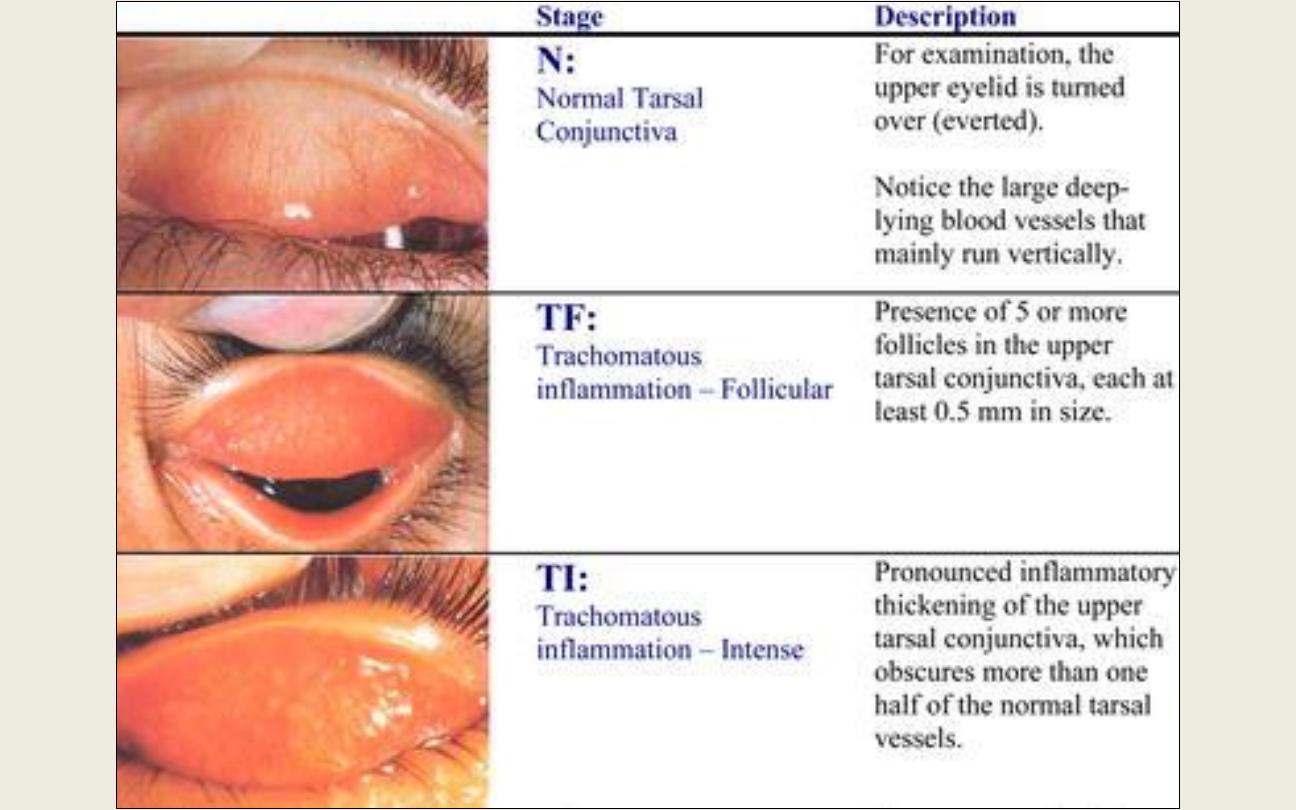
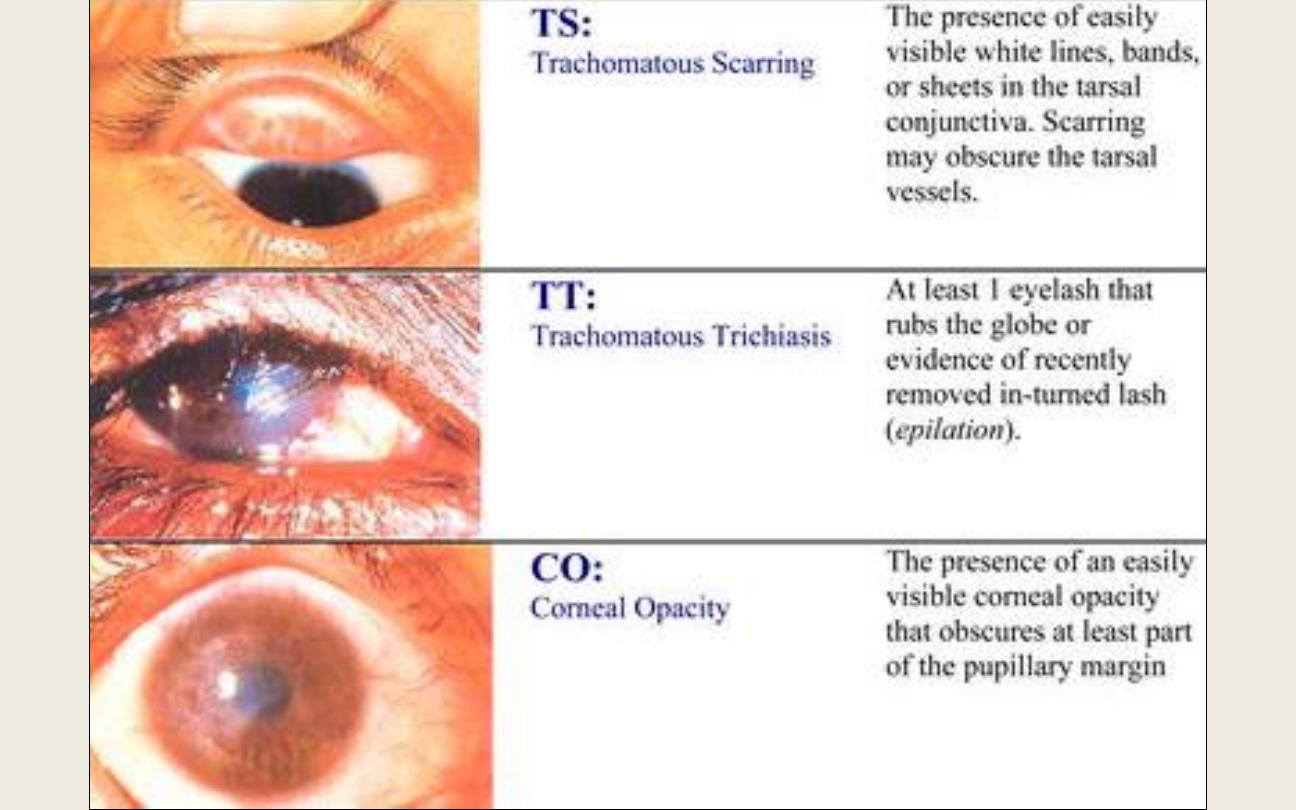
Trachoma:
• infection caused by Chlamydia trachomatis. Transmission: Common fly is the major
vector, currently it is the leading cause of preventable blindness in the world.
• Presentation: is usually during childhood.
• Signs: 1- Follicular reaction.
2- Chronic conjunctival inflammation causes conjunctival scarring that involves the
entire conjunctiva but most prominent on the upper tarsus.
3- Keratitis: either * Superficial epithelial keratitis.
* Anterior stromal inflammation and pannus formation.
4- Progressive conjunctival scarring: if it is severe lead to:* Destruction of lids.
* Trichiasis: * Entropion * Dry eyes 5- End-stage trachoma: * Corneal ulceration
• Treatment of trachoma:
Indicated for stages I & II (TF & TI) only, as there is no benefit from treating stages
III, IV &V (there is no active inflammation).
Preventive measures: strict personal hygiene, especially washing the face of young
children (single face wash at the morning is enough to prevent the infection).
Topical Tetracycline or Erythromycin eye ointment plus Single dose of systemic
azithromycine.
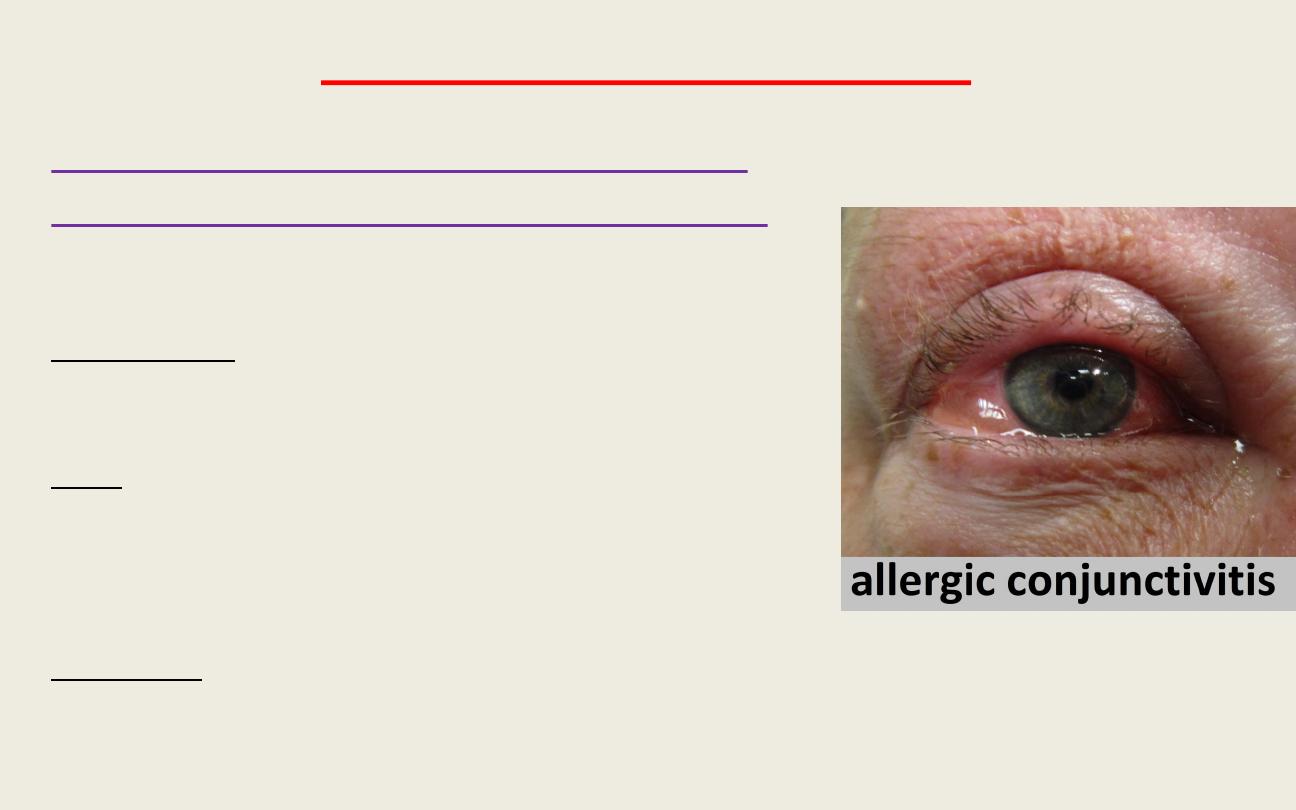
Allergic conjunctivitis
Acute allergic conjunctivitis
(Allergic rhinoconjunctivitis):
• The most common type of eye allergy. Usually there is
associating nasal symptoms
• Presentation: Acute, transient attacks of slightly red, itchy
and watery eyes associated with sneezing and a water
nasal discharge.
• Signs: Mild to moderate lids oedema
Periorbital oedema in severe cases.
Milky or pinkish appearance of conjunctiva.
Mild papillary reaction in the upper tarsal conjunctiva.
• Treatment: Either topical mast cell stabilizer e.g. nedocromil & lodoxamide, or topical
antihistamine e.g. levocabastine & azelastine.
Only in very rare and severe cases we need topical steroids.
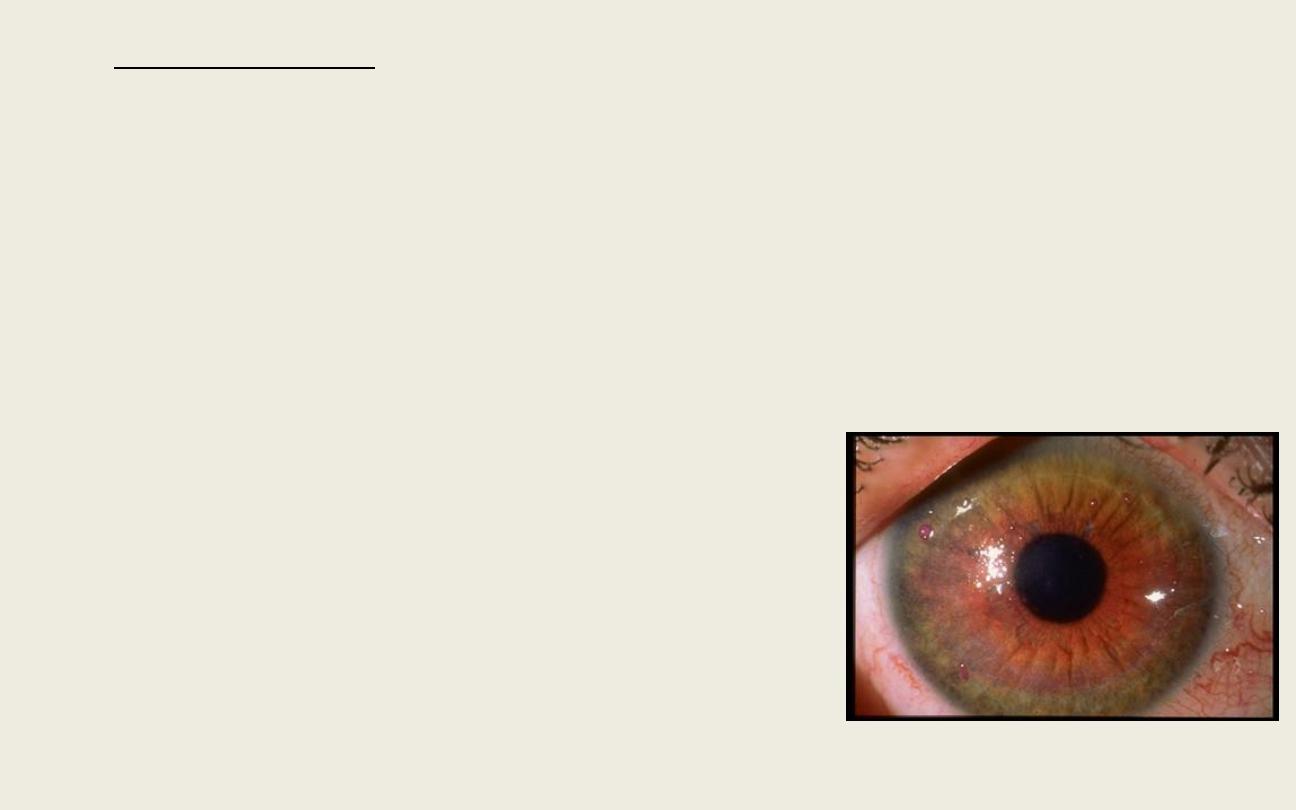
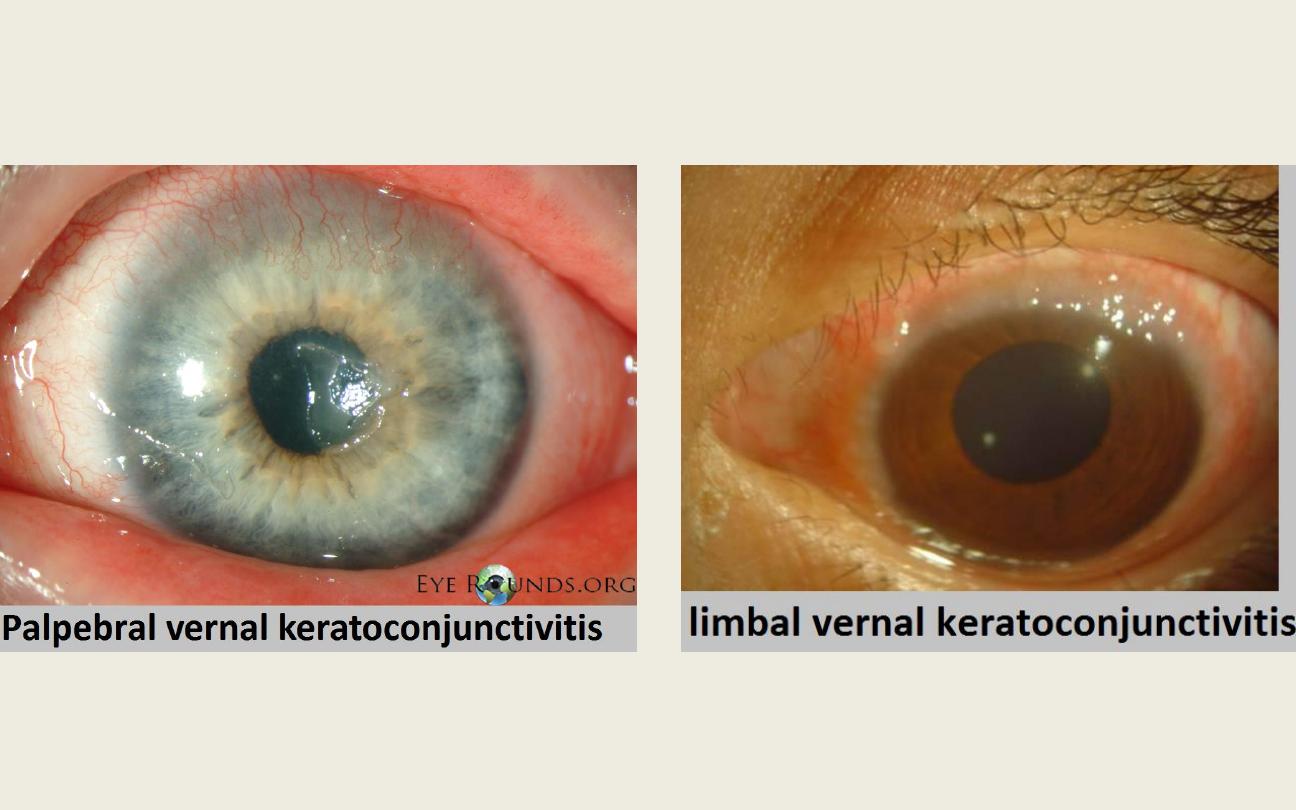
Vernal keratoconjunctivitis (spring catarrh):
• Clinical features: Intense ocular itching, Lacrimation, Photophobia, Foreign body
sensation, Burning, Thick mucus discharge and mechanical Ptosis
• There are three main types: a- Palpebral, b- Limbal and c- mixed.
• Signs:
For conjunctivitis:
o For palpebral vernal keratoconjunctivitis, the signs in chronological order:
Conjunctival hyperaemia.
Diffuse papillary hypertrophy mostly on the superior tarsus (tarsal conjunctiva).
Enlarged of papillae ends in flat-topped polygonal appearance reminiscent of
cobblestones.
In severe cases, the connective tissue septa rupture, giving rise to giant papillae.
o For limbal vernal keratoconjunctivitis:
mucoid nodules that have a smooth round surface.
Discrete white superficial spots (Trantas dots);
o For mixed vernal keratoconjunctivitis: papillary reactions and Trantas dots.
For keratitis: (in chronological fashion)
o Punctate keratopathy: earliest finding.
o Macro erosions .
o Plaque
o Subepithelial scarring
o Pseudogerontoxon
• Treatment:
1) Topical steroids: (its use is mandatory). It should be of short course.
2) Mast cell stabilizers: nedocromil or lodoxomide or sodium cromoglycate
3) Topical Acetylcyseine (mucolytic).
4) Topical cyclosporin A: used in steroids resistant cases.
5) Debridement: of early mucus plaques.
6) Lamellar keratectomy: For densely adherent plaques or subepithelial scarring,
and sometimes we may need corneal replacement (corneal graft).
7) Supratarsal injection of steroids: for severe disease & Giant tarsal papillae.
Conjunctival Degenerations
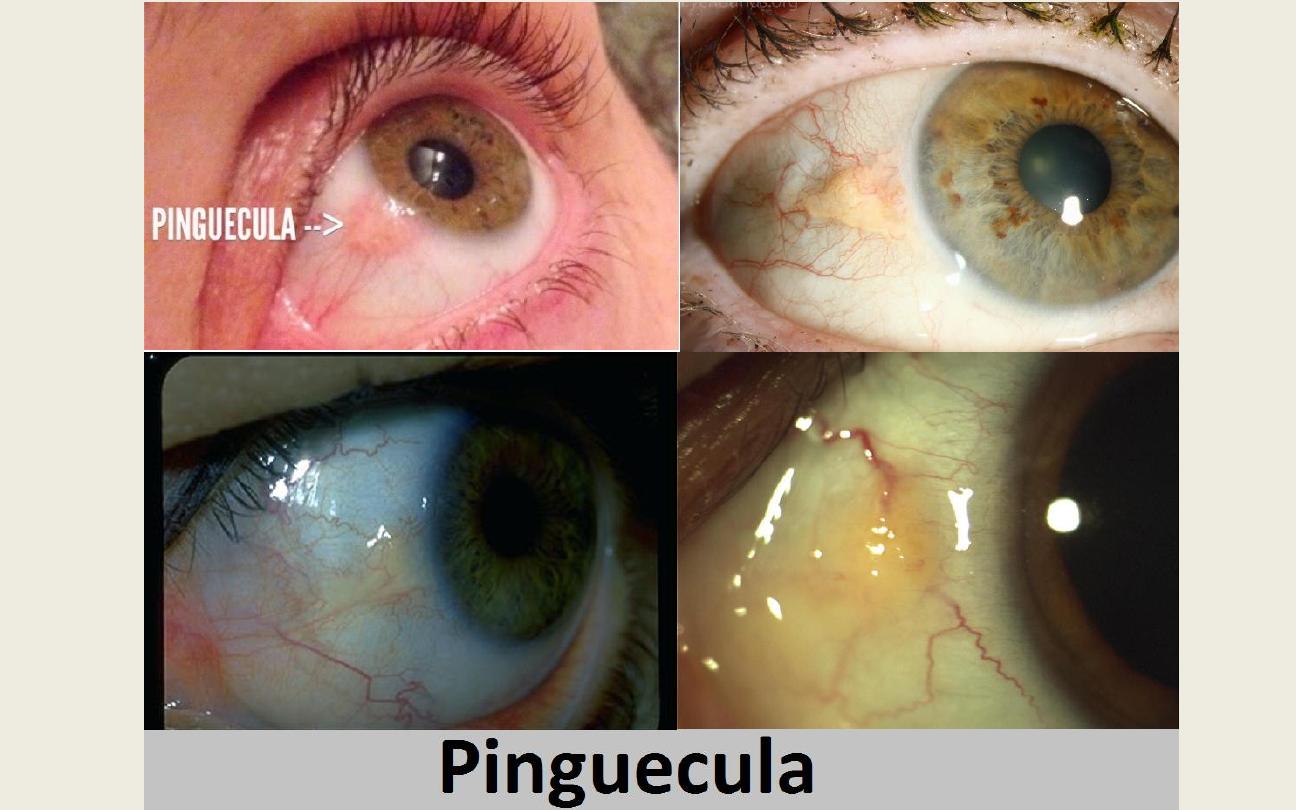
Pinguecula:
• It is an extremely common lesion which consists of a yellow-white deposit on the
bulbar conjunctiva adjacent to the nasal or temporal aspect of the limbus and it is
usually asymptomatic.
• Surgical excision is seldom required. (usually, it need no treatment)
Concretions:
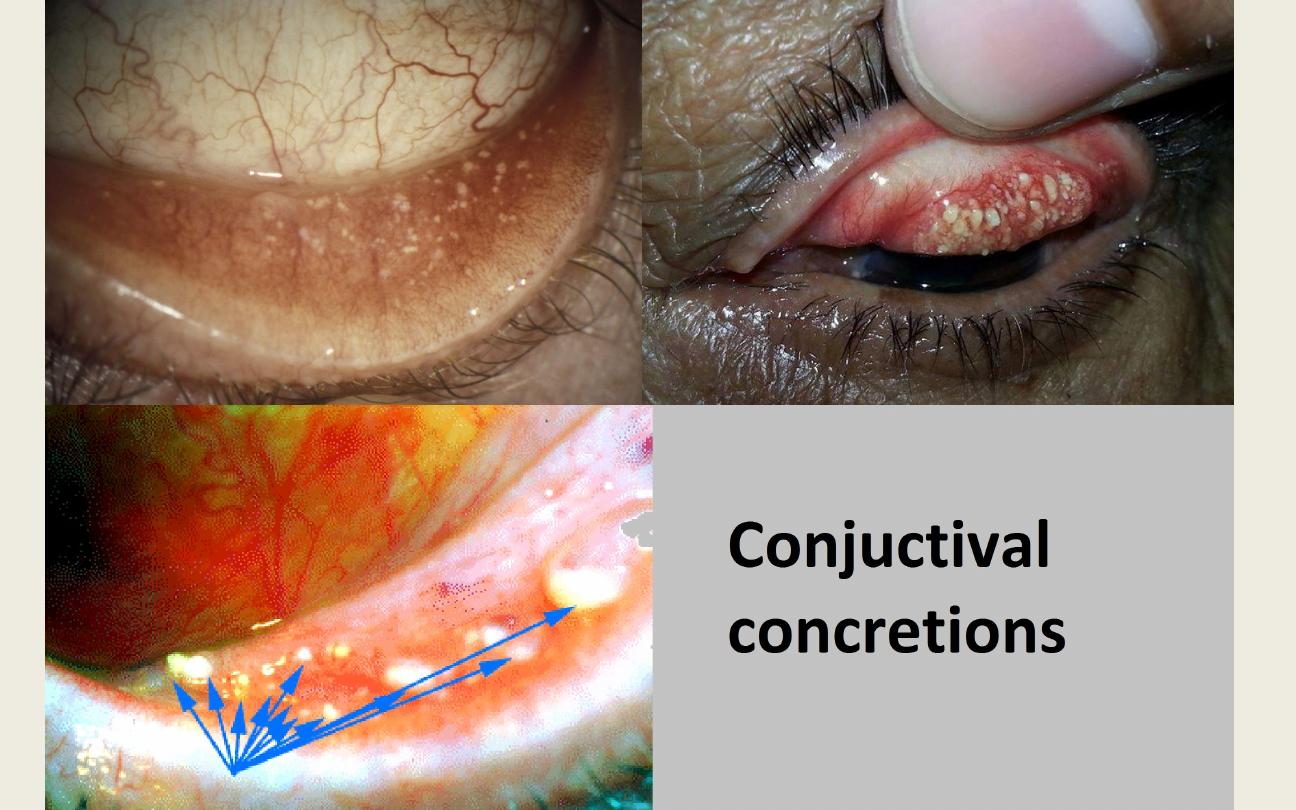
• They are small yellow-white deposits. Commonly present in the palpebral
conjunctiva of the elderly. Also in patients with chronic meibomian gland disease.
• Usually asymptomatic, but occasionally causes foreign body sensation when erode
through the epithelium.
• Treatment: They can be easily removed with a needle.
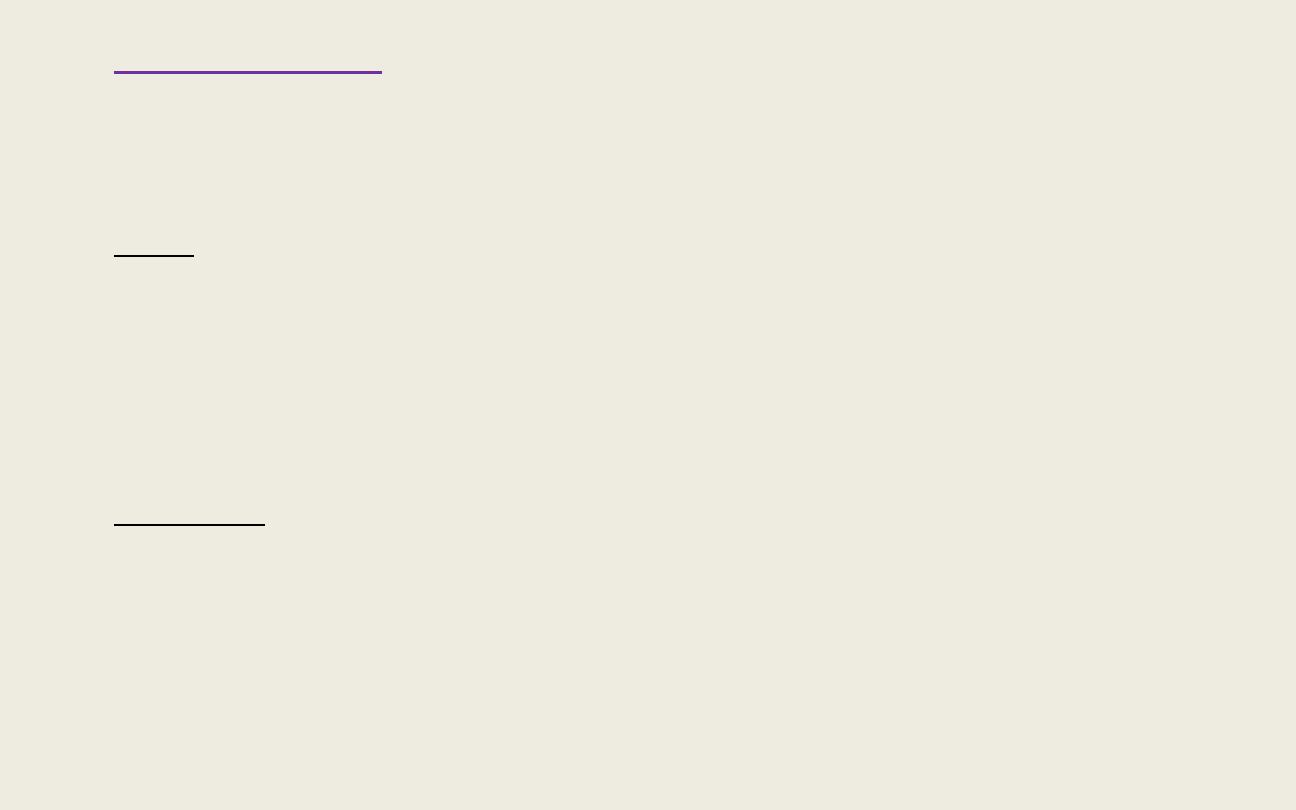
Pterygium:
• It is a triangular sheet of conjunctival fibrovascular tissue invades the cornea.
• Occurs in patients who have been living in outdoor, hot climates. May represent a
response to chronic dryness and exposure to the sun. Usually asymptomatic.
• Signs:
a- Small, grey, corneal opacities near the nasal limbus.
b- Then, the conjunctiva overgrows these opacities and progressively invades onto
the cornea in a triangular fashion.
c- A deposit of iron (Stocker line) may be present in the corneal epithelium
anterior to the advancing head of the pterygium.
• Treatment:
a- Surgical excision: needed only (indicated only) in the following cases: i- If it is
threatening the visual axis. ii- Severe irritation. iii- For cosmetic reason.
b-Lamellar keratoplasty: required if the visual axis is affected by opacification.
Surgical excision, it is an easy procedure but should be avoided unless there is
indication because the recurrent rate is high (about 40%) and the recurrent
ptrygium is uglier,
“Sclera &
Episclera”
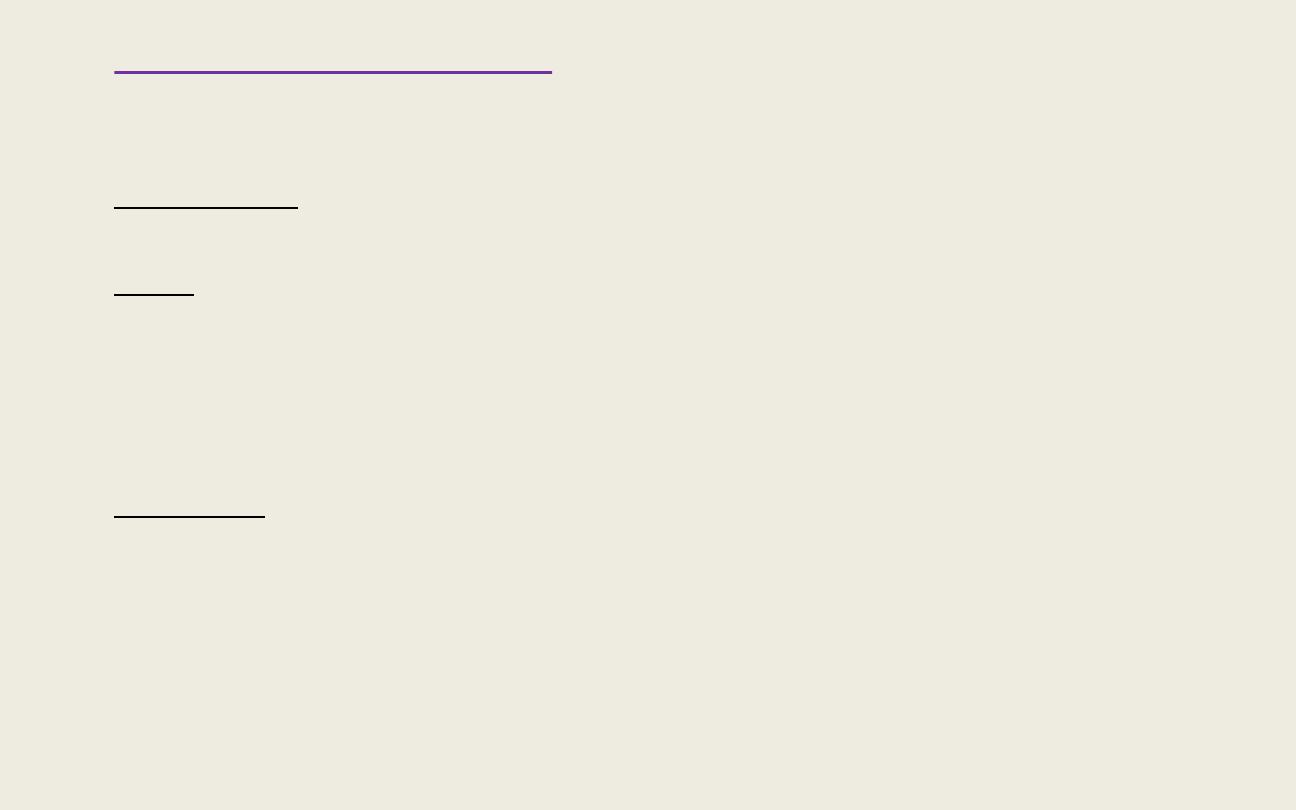
Episclerritis
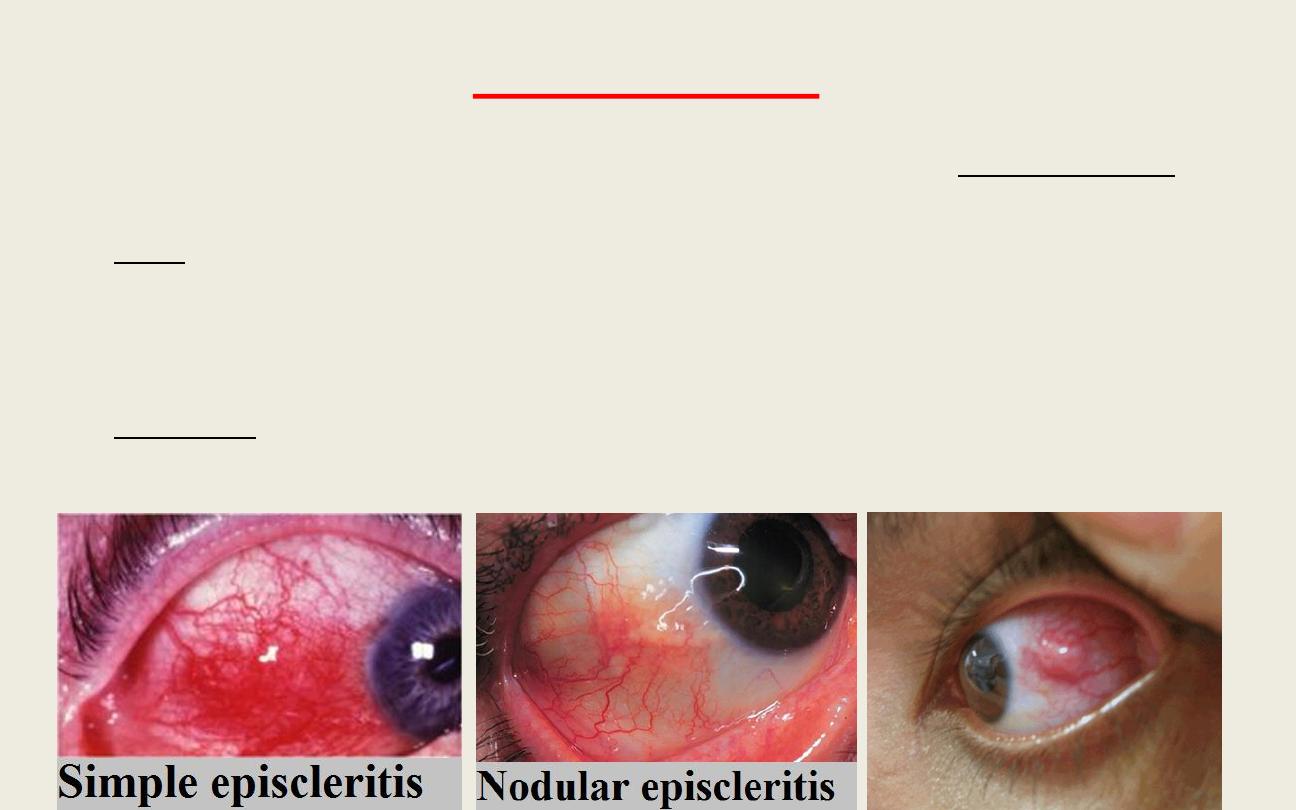
• Common, benign, self-limiting & frequently recurrent disorder. Presented with:
unilateral redness associated with mild discomfort, tenderness & watering eye.
• Signs: 1) Simple episcleritis: commonest type, characterized by sectoral or less
commonly diffuse redness that resolves spontaneously within 1-2 weeks.
2) Nodular seclerosis: characterized by a localized, raised congested nodule which
take longer time (> 1-2 weeks) to resolve.
• Treatment:
Simple lubricants or vasoconstrictors: suffice in most mild cases.
Oral NSAIDs: Flurbiprofen. Topical steroids: Helpful, but increase recurrence rate
Scleritis
• Characterized by edema & cellular infiltration of the entire thickness of the sclera.
• Causes & associations:
Systemic associations (50%): RA (most common), wegener’s granulomatosis,
relapsing polychondritis & polyarteritis nodosa.
Surgically induced: follows eye surgery e.g. retinal reattachment surgery
Infectious: from corneal ulcer, after trauma or follows excision of a pterygium.
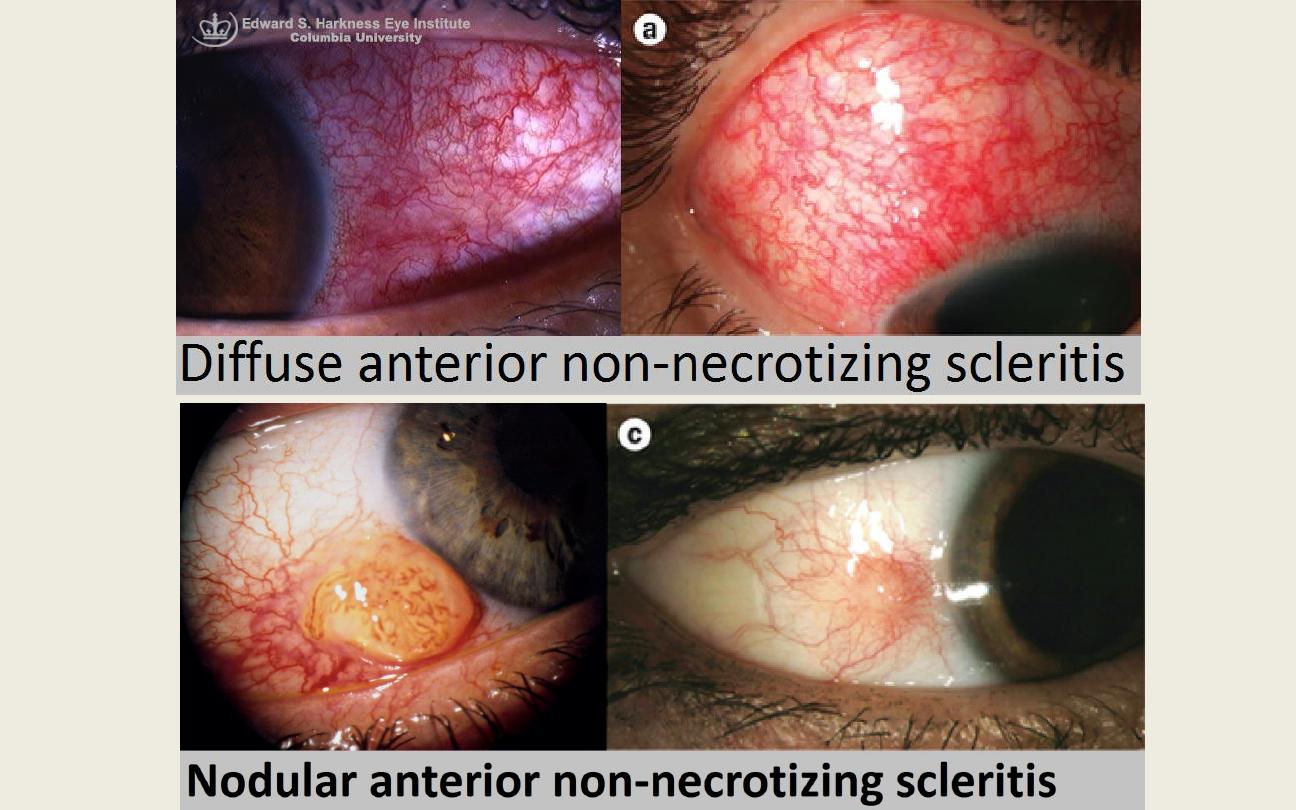
• Anatomical classification:
Anterior (98%):
o Non-necrotizing (85%): diffuse & nodular
o Necrotizing (13%): with inflammation or without inflammation
Posterior (2%)
Anterior non-necrotizing scleritis
• Presentation: similar to episcleritis although discomfort may be severe.
• Signs:
Diffuse scleritis: widespread inflammation involving a sector or entire anterior
scleritis.
Nodular scleritis: more severe & resemble nodular episcleritis, but the nodule
can’t be moved over the underlying tissue.
• Treatment:
Oral NSAIDs: such as Flubiprofen
Oral prednisolone: resistent or intolerant to NSAIDs.
Combined therapy: NSAIDs+low dose steroid, when response is inadequte to
either drug alone.
Sub Tenon’s steroid injection: Triamcinolone acetonide alternative to systemic
treatment.
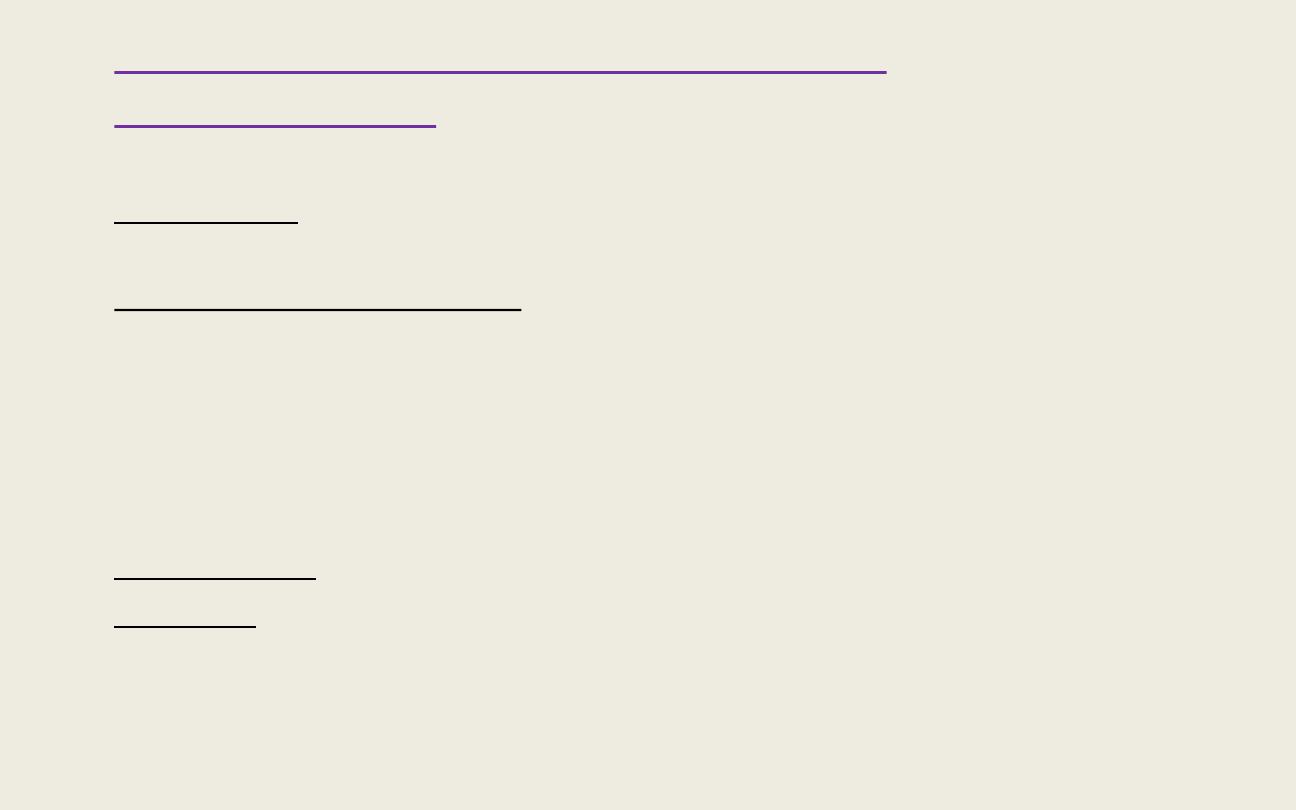
Acute necrotizing scleritis with
inflammation
• Most severe & distressing form of scleritis, Visual prognosis is poor.
• Presentation: Gradual pain & localized redness. The pain becomes severe &
persistent and radiates to the temple, brow or jaw.
• Signs (In chronological order): Congestion of the deep vascular plexus.
Distortion & occlusion of blood vessels producing avascular patches.
Scleral necrosis. Spreading of scleral necrosis.
Upon resolution; a bluish tinge appears secondary to scleral thinning (the sclera
becomes transparent so that the underlying choroidal pigment becomes visible
when viewed in daylight).
• Complications: Staphyloma formation & Anterior uveitis.
• Treatment: Oral prednisolone: indicated in active disease
Immunosuppressive agents: cyclophosphamide, azathioprine or cyclosporine in
steroid resistant cases.
Combined therapy: Pulsed IV methylprednisolone & cyclophosphamide. Used in
failure of oral treatment & established scleral necrosis.
Acute necrotizing
scleritis with
inflammation
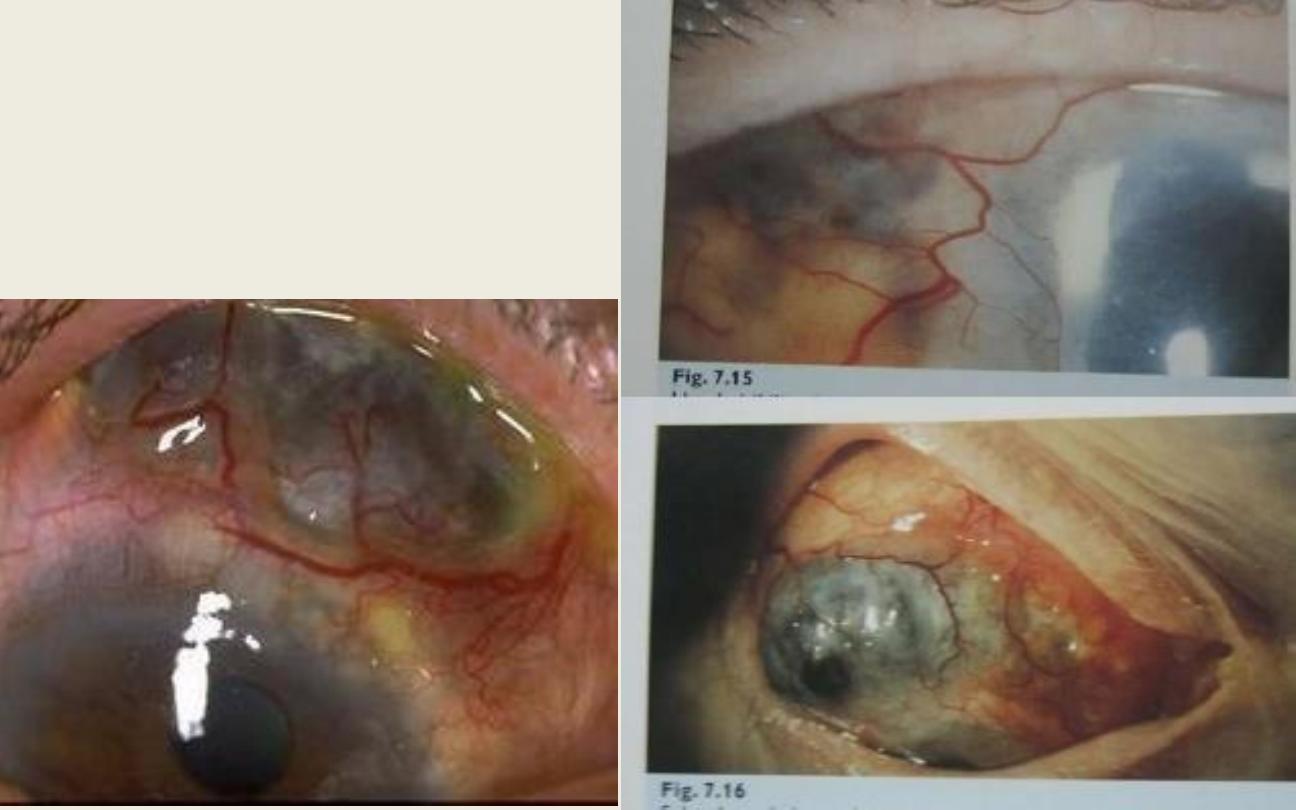
Acute necrotizing scleritis without
inflammation (Scleromalacia perforans)
• Typically occurs in women with longstanding RA & is usually bilateral.
• Signs (In chronological order):
Asymptomatic: yellow necrotic scleral patches in uninflamed sclera.
Enlargement of necrosis & spreading.
Scleral thinning & exposure of underlying uvea.
Staphyloma formation but perforation is rare unless the IOP is elevated.
• Treatment: is ineffective.
Posterior scleritis
• Uncommon & often misdiagnosed because it may confused with other
inflammatory & neoplastic condition.
• Presentation: Pain & decreased visual acuity (vision is affected more than that in
anterior scleritis)
• Signs:
External signs: Lid edema, proptosis & ophthalmoplegia associated anterior
scleritis.
Fundus findings: Disc swelling, macular edema, choroids folds, exudative retinal
detachments & subretinal lipid exudation.
• Treatment:
In young patients: without systemic disease, usually respond to NSAIDs.
In elderly patients: with associated systemic disease iis as for anterior necrotizing
scleritis.
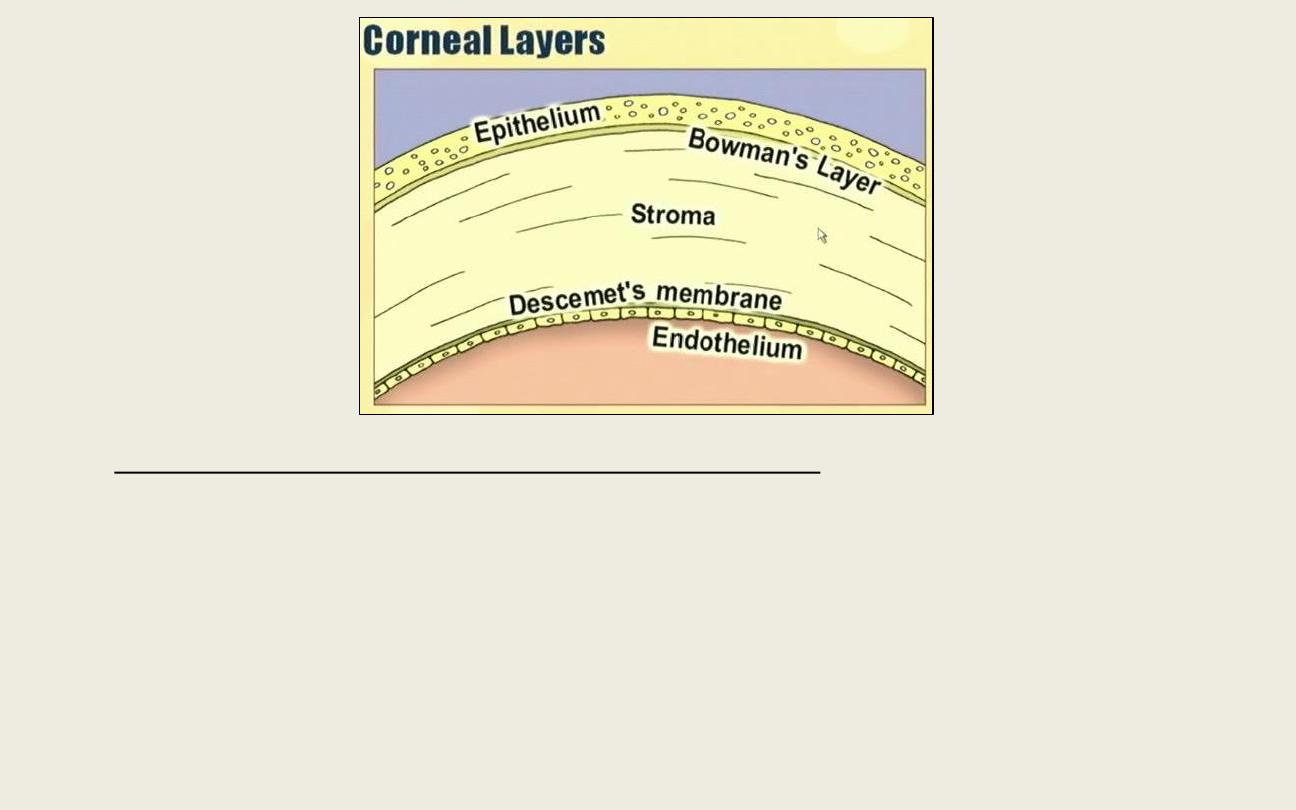
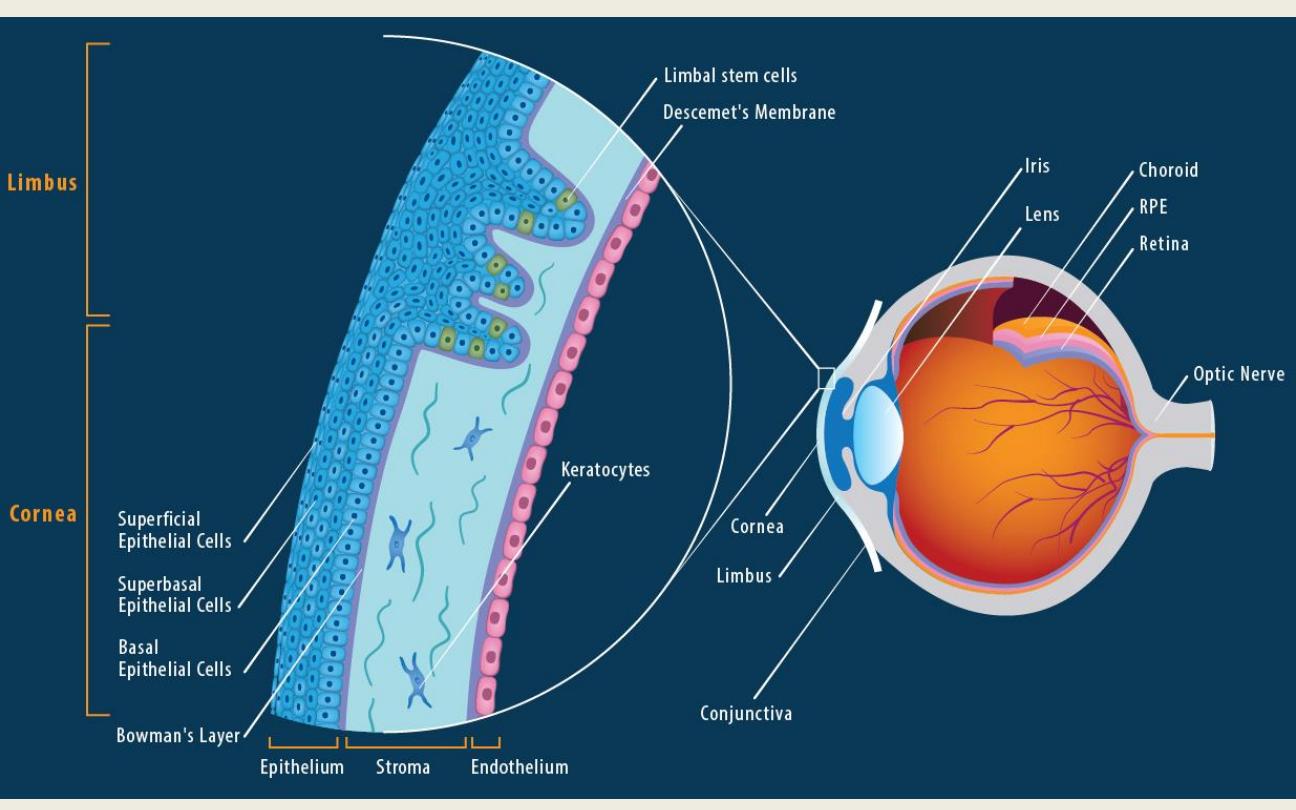
“The cornea”
Gross Anatomy
• The cornea is the anterior continuation of the sclera; it forms 1/6 of the outer
layer of eyeball.
• It is a transparent structure;
• its function is facilitating entrance and focusing the light rays on the retina. It
represents the most important refractive organ in the eye.
• The cornea consists of the five following layers: (from anterior to posterior or
from external to internal)
1) The epithelium
2) Bowman's layer
3) The stroma: makes up 90% of the corneal thickness.
4) Descemet's membrane
5) The endothelium
• The cornea is transparent for the following reasons:
1) The epithelium is not keratinized.
2) The stroma is regularly oriented. (Maurice theory)
3) The endothelium has active pump, it pushes the fluid into aqueous and it acts as
barrier to prevent entrance of aqueous inside the cornea.
4) The corneal nerves are unmylinated.
5) It contains NO blood vessels.
6) It contains NO pigments (as melanin).
Signs of corneal diseases
Epithelial signs:
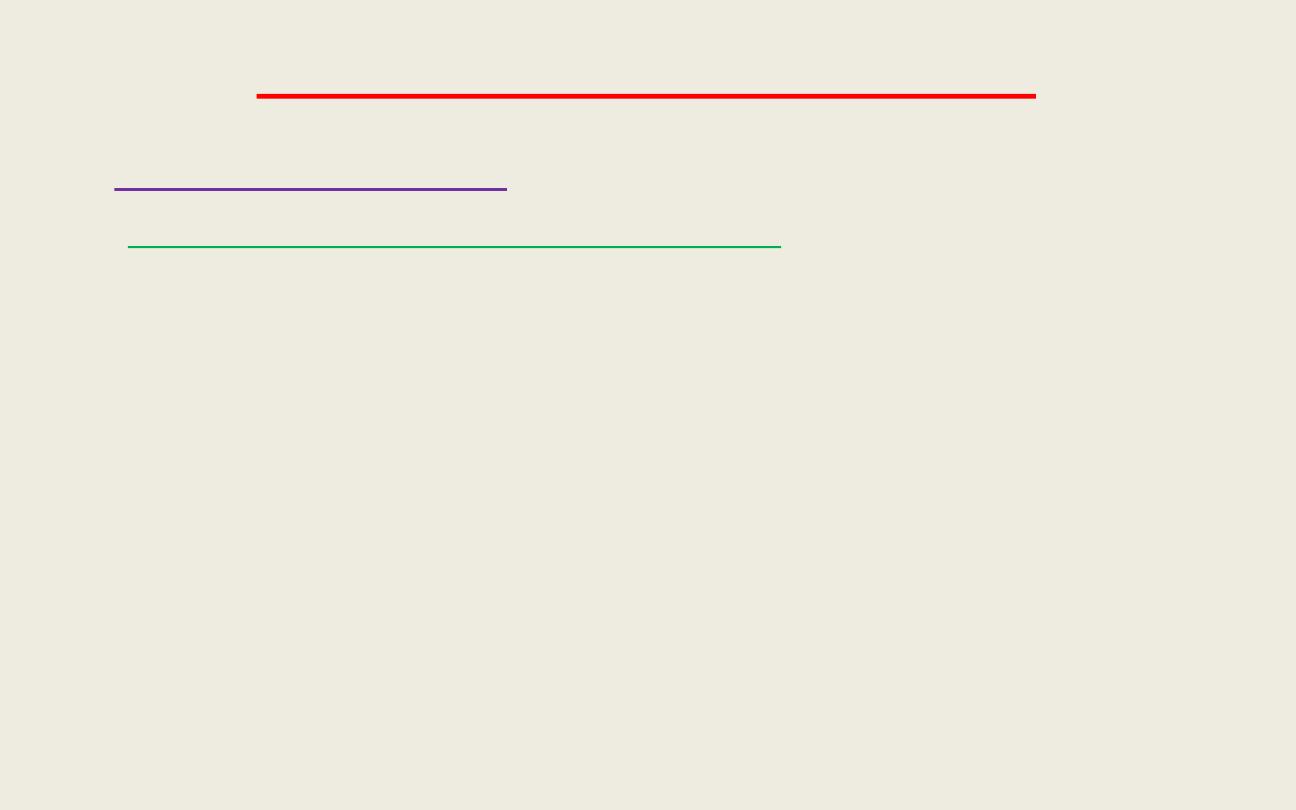
1) Punctate epithelial erosions (PEE):
• Are tiny, slightly depressed, epithelial defects (micro-ulcers seen by slit-lamp),
which stain with fluorescein.
• Note: Fluorescein is vital extracellular stain. It stains living tissue e.g. the base of
ulcer, while Rose-Bengal is non vital intracellular stain. It stains dead cells and
mucus at the margin of ulcer.
• Causes: vernal keratoconjunctivitis, poorly fitting contact lens, dry eyes, decreases
corneal sensation (as in trigeminal nerve palsy or after herpes simplex viral
keratitis), exposure to ultraviolet, corneal exposure and toxicity from drops (e.g.
Aminoglycosides).
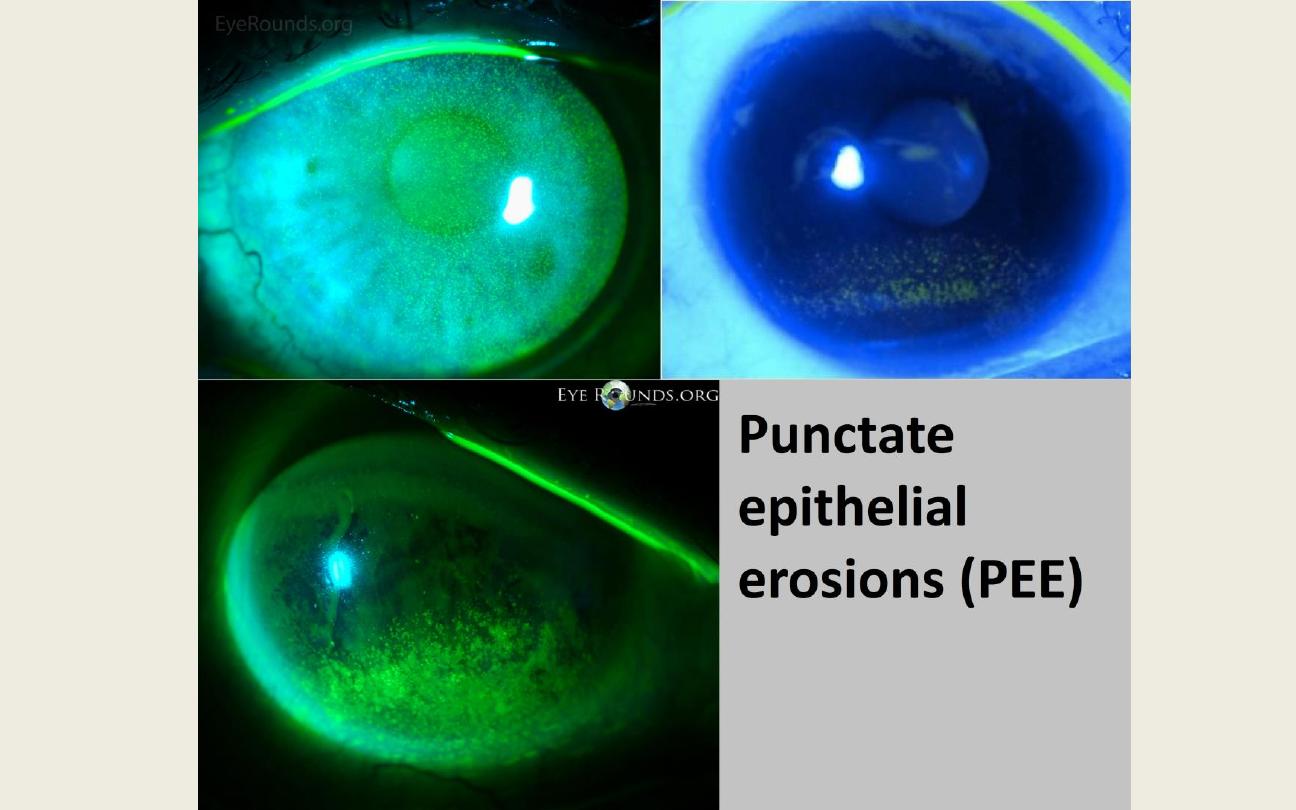
2) Punctate epithelial keratitis (PEK):
• Is the hallmark of viral infections, it is characterized by granular, opalescent,
swollen epithelial cells stained with rose Bengal stain but not fluorescein (why?).
3) Epithelial oedema:
• It is a sign of endothelial decompensation or severe and sudden elevation of
intraocular pressure (as that occurring in acute glaucoma as IOP is raised leading
to oedema that affects the vision).
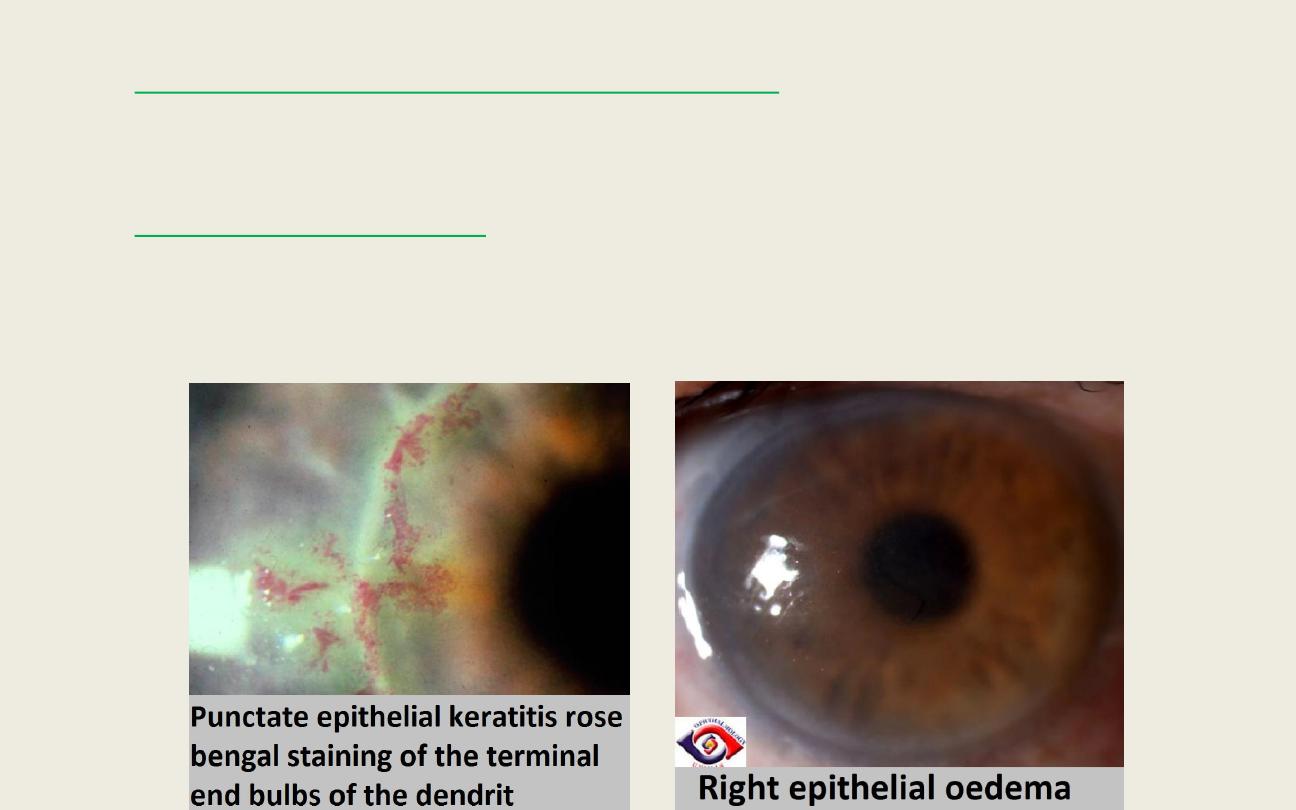
4) Filaments:
• Small, comma-shaped mucus strands lined with epithelium (one end attached to
the epithelial cornea & the other is free), which stain well with Rose-Bengal stains.
• Causes: KC sicca, recurrent erosion syndrome, prolong eye patching, corneal
exposure, diminished corneal sensation & herpes zoster ophthalmicus.
5) Pannus:
• inflammatory or degenerative sub-epithelial ingrowths of fibrovascular tissue from
limbus.
Stromal signs:
1) Stromal infiltration:
• Focal areas of active stromal inflammation composed of accumulations leucocytes
and cellular debris. These focal areas are granular, gray-white opacities within the
stroma.
• Causes:
i- Non-infectious (Antigen sensitivity): e.g. contact lens wear & marginal keratitis.
ii- Infectious keratitis: e.g. bacteria, viruses, fungi and protozoa.
2) Stromal oedema:
• It affects optically empty spaces between stromal lamellae associated with
increase corneal thickness and decreased its transparency.
• Causes: Fuch's dystrophy (Hereditary abnormal endothelium or decreased
number of cells) and surgical damage to the corneal endothelium.
3) Vascularization:
• Causes: Wide variety of corneal disorders, e.g. microbial keratitis, chemical burns,
trauma, TB, syphilis and autoimmune Keratoconjunctivitis (Cicatricial Pemphigoid
and Stevens Johnson syndrome).
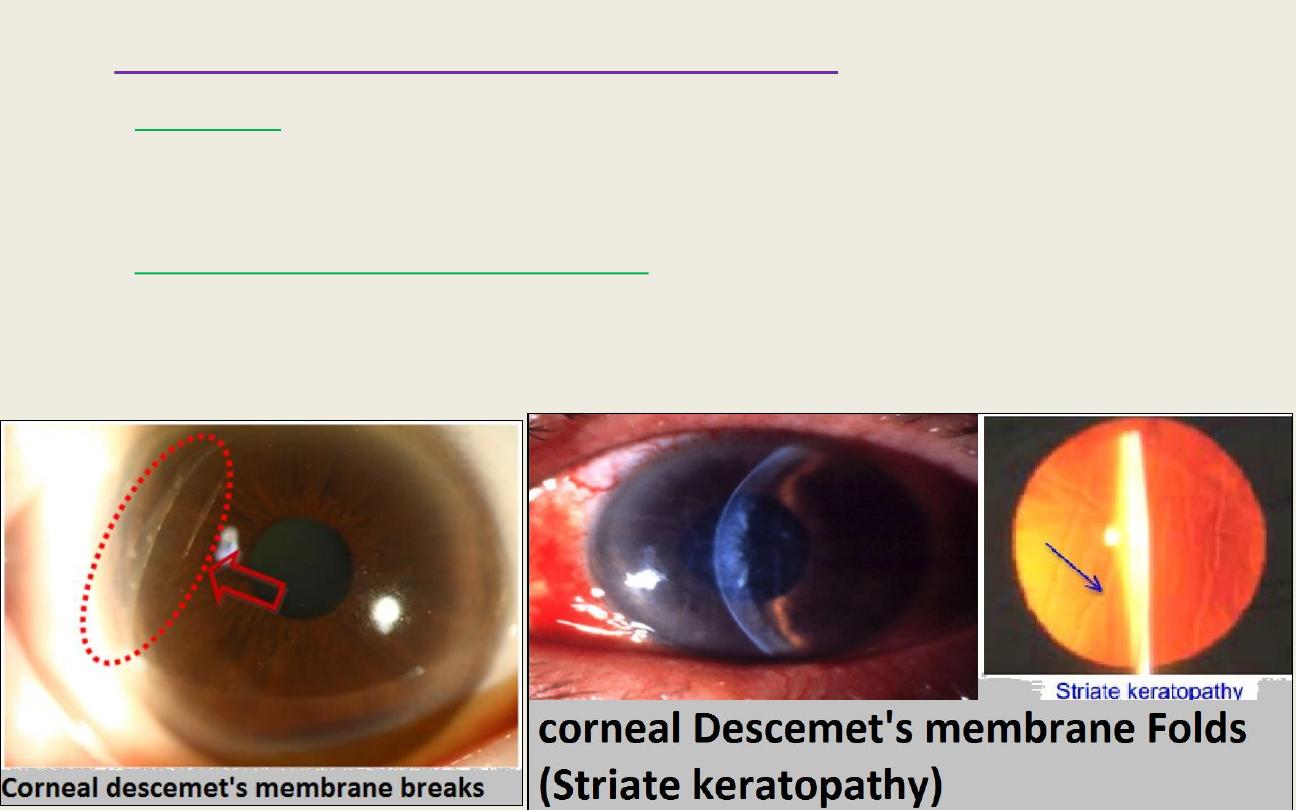
Descemet's membrane signs:
1) Breaks:
• Causes: Corneal enlargement e.g. congenital glaucoma, birth trauma and
keratoconus. It leads to influx of aqueous causing stromal oedema.
2) Folds (Striate keratopathy):
• Causes: Surgical trauma, ocular hypotony, stromal inflammation and oedema.
• Normal IOP is 10-21 mm Hg, if it is less than 6 mm Hg then it is hypotony.
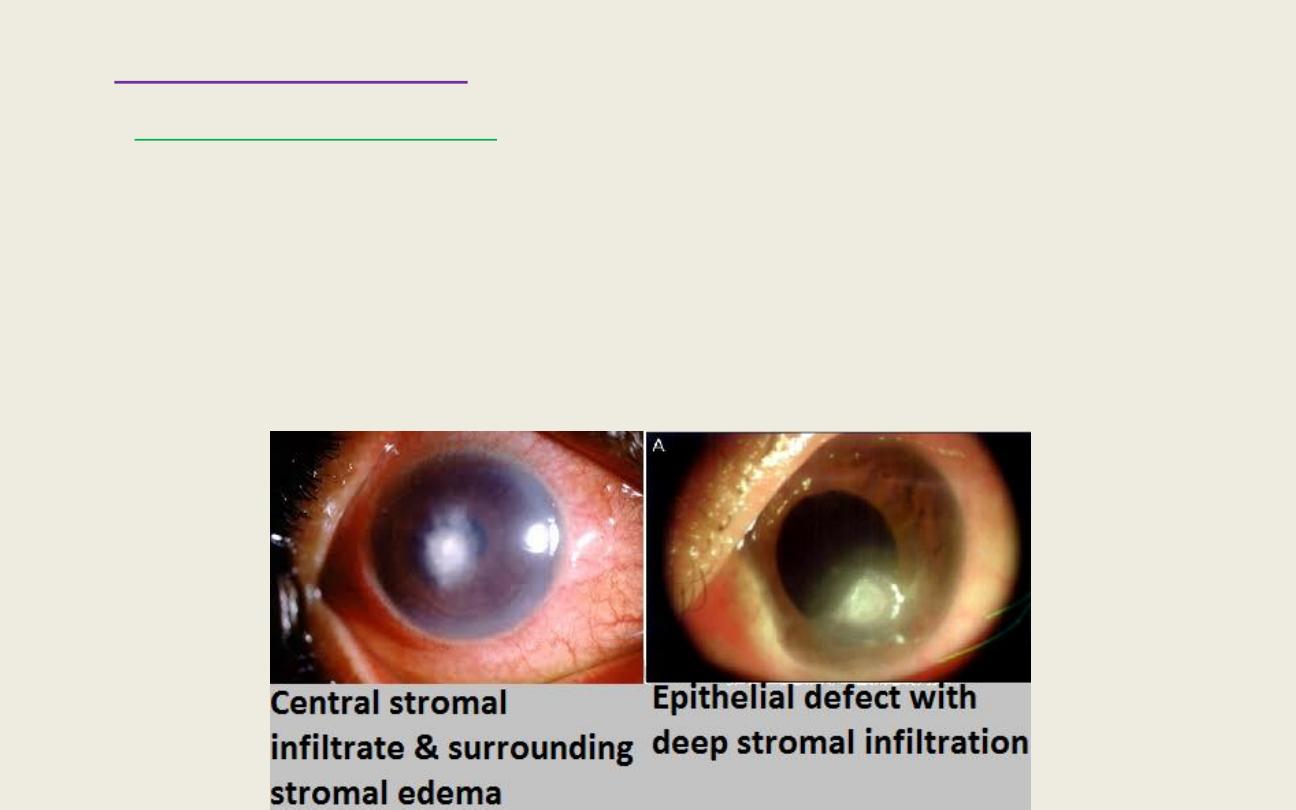
Microbial keratitis
Bacterial Keratitis:
• Symptoms: foreign body sensation, photophobia, blurring of vision, pain, eyelid
oedema and discharge.
• Signs:
Conjunctival and circumcorneal injection (almost always some sort of anterior
uveitis is associated with Keratitis).
Epithelial defects associated with an infiltrate around the margin and base.
Enlargement of the infiltrate associated with stromal oedema.
Secondary sterile anterior uveitis with hypopyon.
Progressive ulceration may lead to corneal perforation and bacterial
endophthalmitis (involvement of all intraocular tissues).
• Treatment:
Corneal scraping: may not be required for small eccentric infiltrate
Hospital admission: should considered for aggressive disease
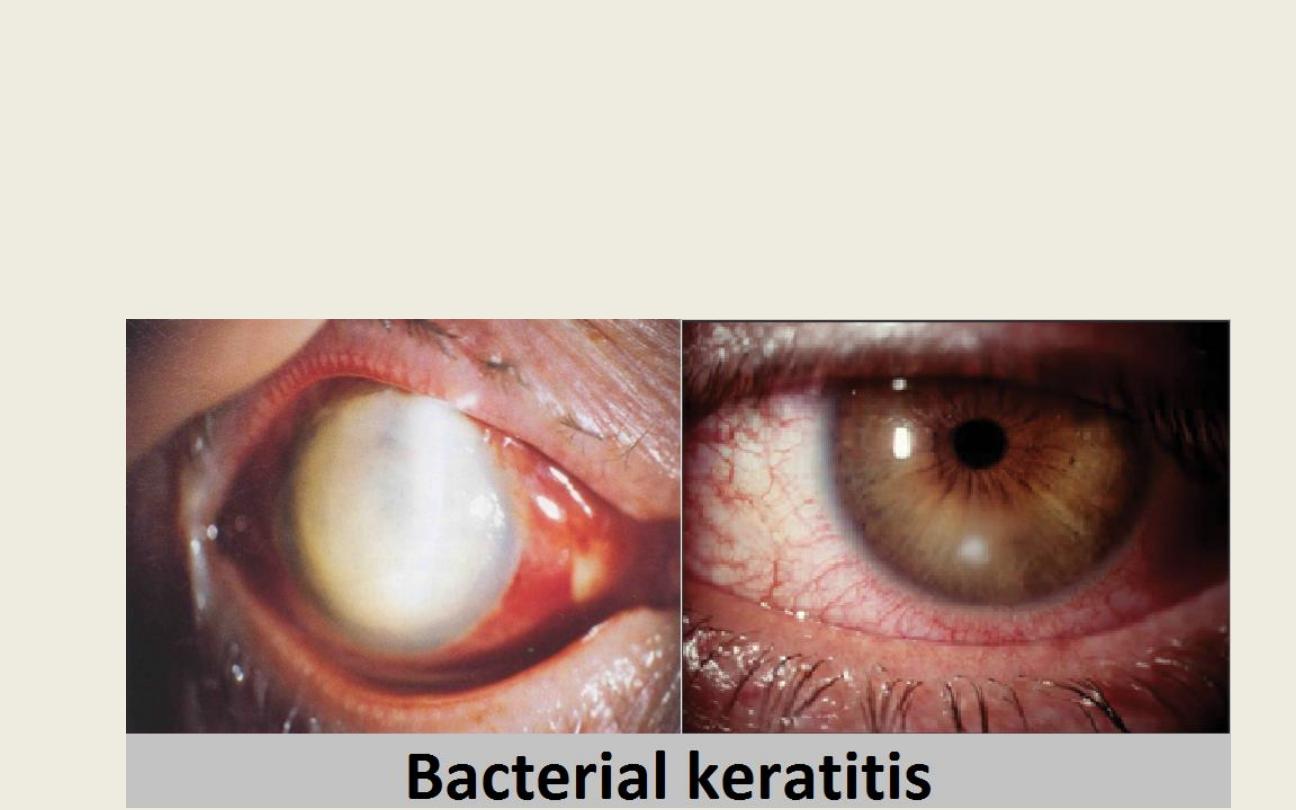
a- Topical antibiotics: Initial instillation of empirical fortified antibiotic (topical)
started before microscopy result available.(empirical duo therapy usually
cephalosporin and aminoglycoside)
b- Oral ciprofloxacin
c- Atropine
d- Steroid therapy: It is contravesial.
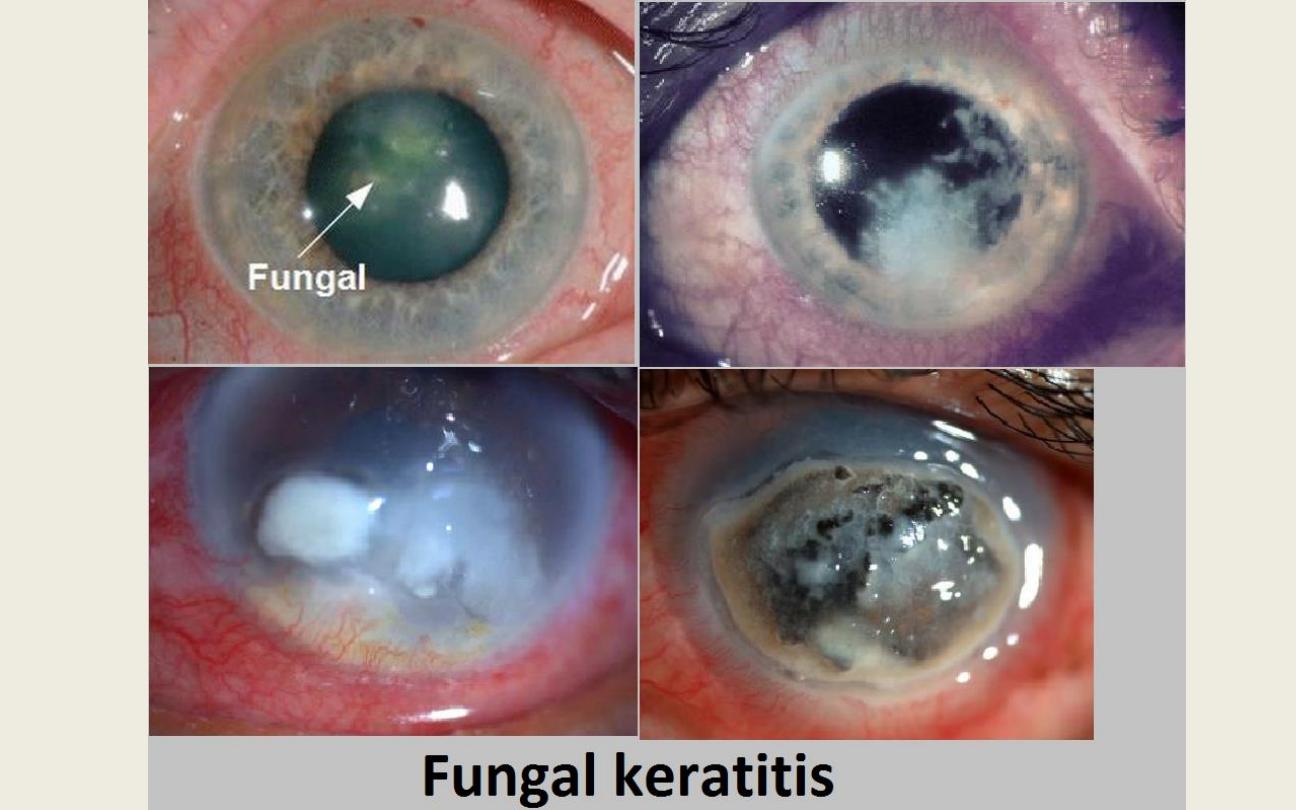
Fungal keratitis:
• Symptoms: Gradual onset of foreign body sensation, Photophobia, Blurred vision
and discharge (mucopurulent). Progression is much slower and less painful than
in bacterial keratitis.
• Signs:
Filamentous keratitis:
o A grayish, stromal infiltration with indistinct margin.
o Surrounding, satellite, feathery, finger-like lesions (extensions).
o Hypopyon (pus in the anterior chamber).
o There is always some sort of iritis associating keratitis.
Candida keratitis: A yellow-white, stromal infiltration associated with dense
suppuration similar to bacterial keratitis.
• Treatment:
a- Topical treatment: Filamentous: Natamycin, and may add Amphotericin.
Candida: Imidazole or Flucytosine.
b- Systemic antimycotics: e.g. Ketoconazole (tablets) or Itraconazole.
c- Therapeutic penetrating keratopathy: In unresponsive cases.
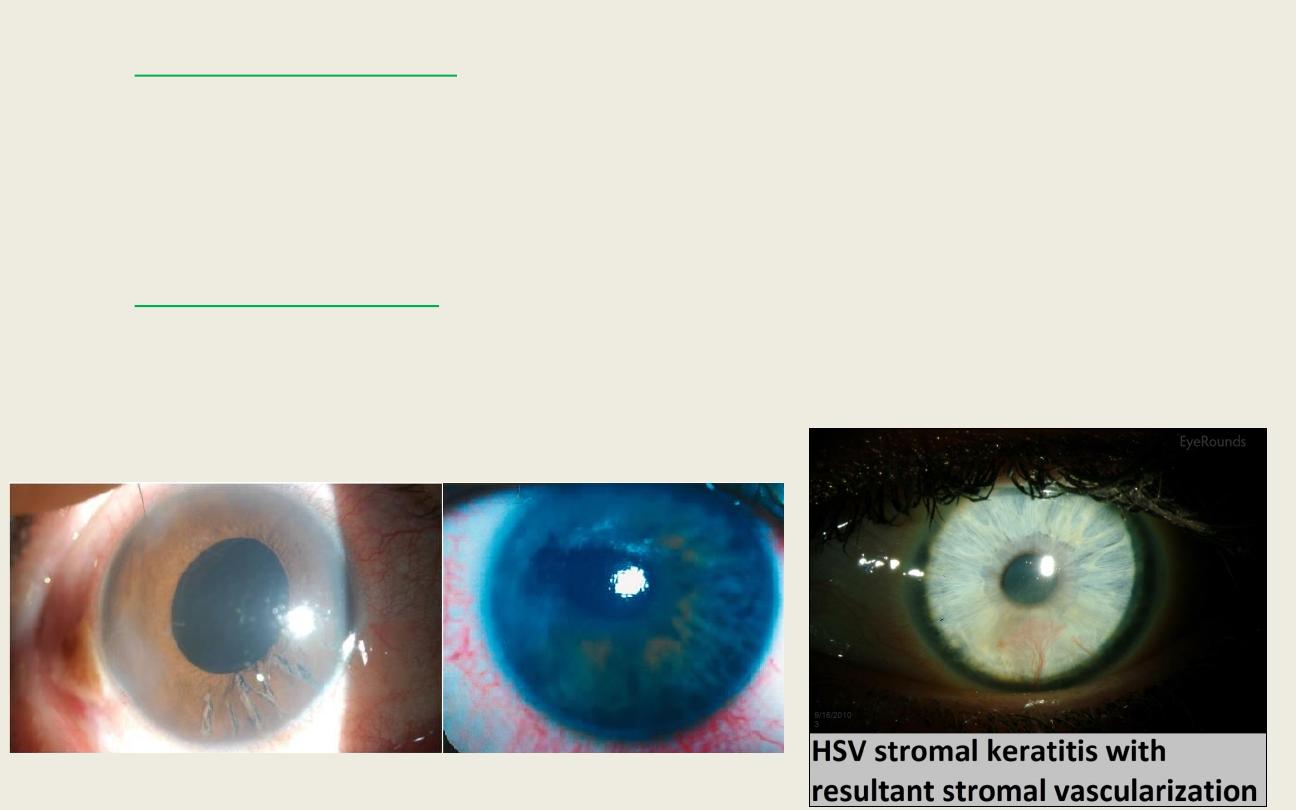
Viral keratitis:
1) Herpes simplex keratitis:
Primary ocular infection:
• Signs:
Skin vesicles typically involve the lids and periorbital area.
Acute, unilateral, follicular conjunctivitis associated with tender lymphadenopathy.
Secondary canalicular obstruction may occur (the infection by itself causes
lacrimation, but if it is complicated by secondary canalicular obstruction this will
cause epiphora).
Keratitis is uncommon.
• Treatment: Aciclovir (Zovirax
®
) eye ointment.
Recurrent ocular disease (Epithelial keratitis):
• Presentation: Mild discomfort. - Watering eye. - Blurring of vision.
• Signs: (in chronological)
Opaque epithelial cells or punctuate epithelial keratitis (coarse punctuate or
stellate pattern).
Central desquamation results in a linear-branching (dendritic) ulcer.
Decreased corneal sensation (as it involves the nerves).
Anterior stromal infiltration under the ulcer.
Progressive centrifugal (from the center outwards) enlargement may result in a
large epithelial defect with a geographical or amoeboid configuration, especially in
the context of injudicious topical steroid therapy.
Following healing, there are persistent linear-branching shapes, which represent
waves of healing epithelial cells.
• Treatment of Herpes simplex epithelial keratitis:
Topical: without treatment, 50% resolves spontaneously, with treatment, the cure
rate is 95%. i- Aciclovir 3% ointment. ii- Ganciclovir (Virgan) gel
iii- Trifluorothymidine drops: like Aciclovir, cure rate of 95%, but it is more toxic.
Debridement: Which is used in dendritic but not geographic ulcers in patients who
are: non-compliant, allergic to drugs, when antiviral agents are not available and
resistant cases. Drugs are ideally used after debridement. Cure rate is above 50%
and below 95%.


2) Herpes Zoster ophthalmicus (HZO):
• Caused by Varicella Zoster virus (VZV). Chickenpox (Varicella) and Zoster are
different conditions caused by the same virus. If we have crust lesion at the tip of
the nose "Hutchinson sign", it indicates ocular involvement (Because the
distribution of the ophthalmic division of the trigeminal nerve)
• Ocular Features: Keratitis, conjunctivitis, episcleritis, scleritis and anterior uveitis.
• Treatment:
Systemic: Valaciclovir 1g t.i.d for 7 days Or Famciclovir 250mg t.i.d for 7 days.
Topical: Eye: Herpetic ulcer Aciclovir ointment.
Autoimmune Topical steroid. Sometimes, both of them are used.
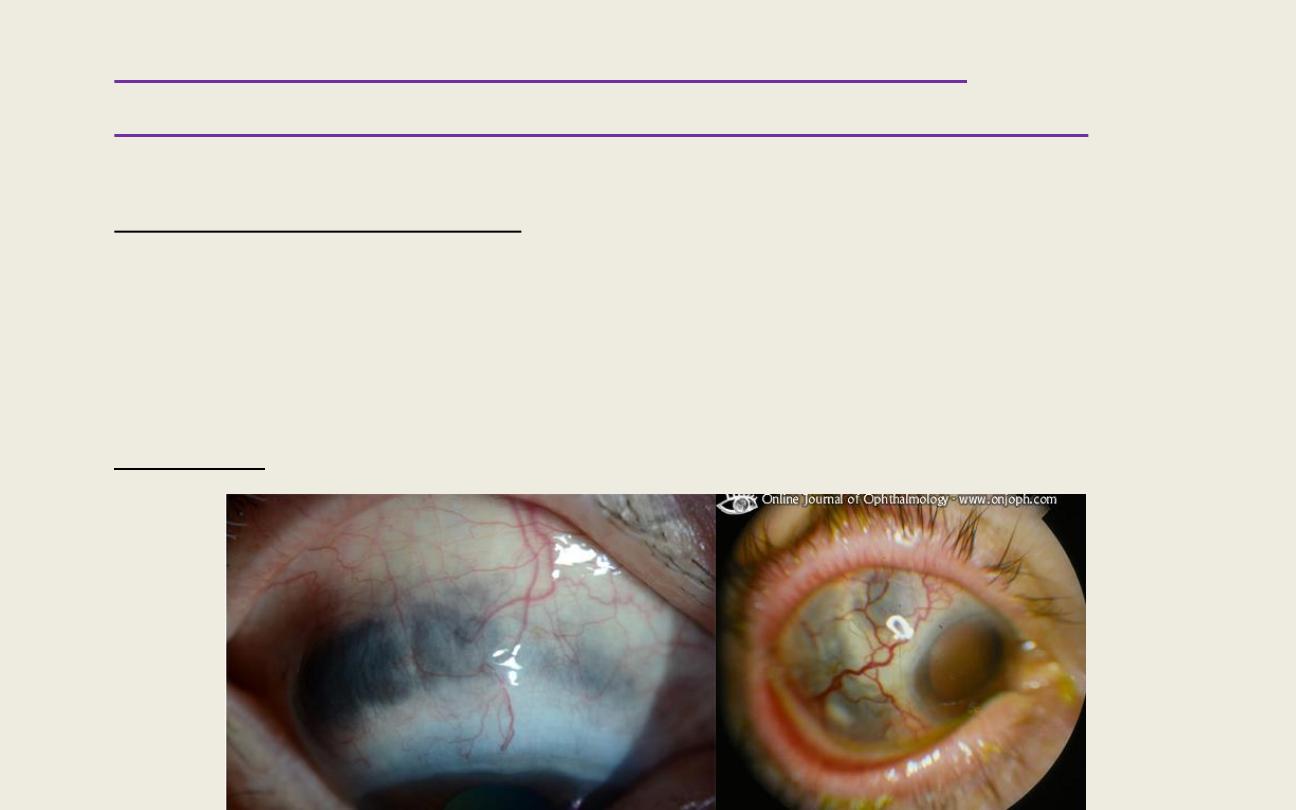
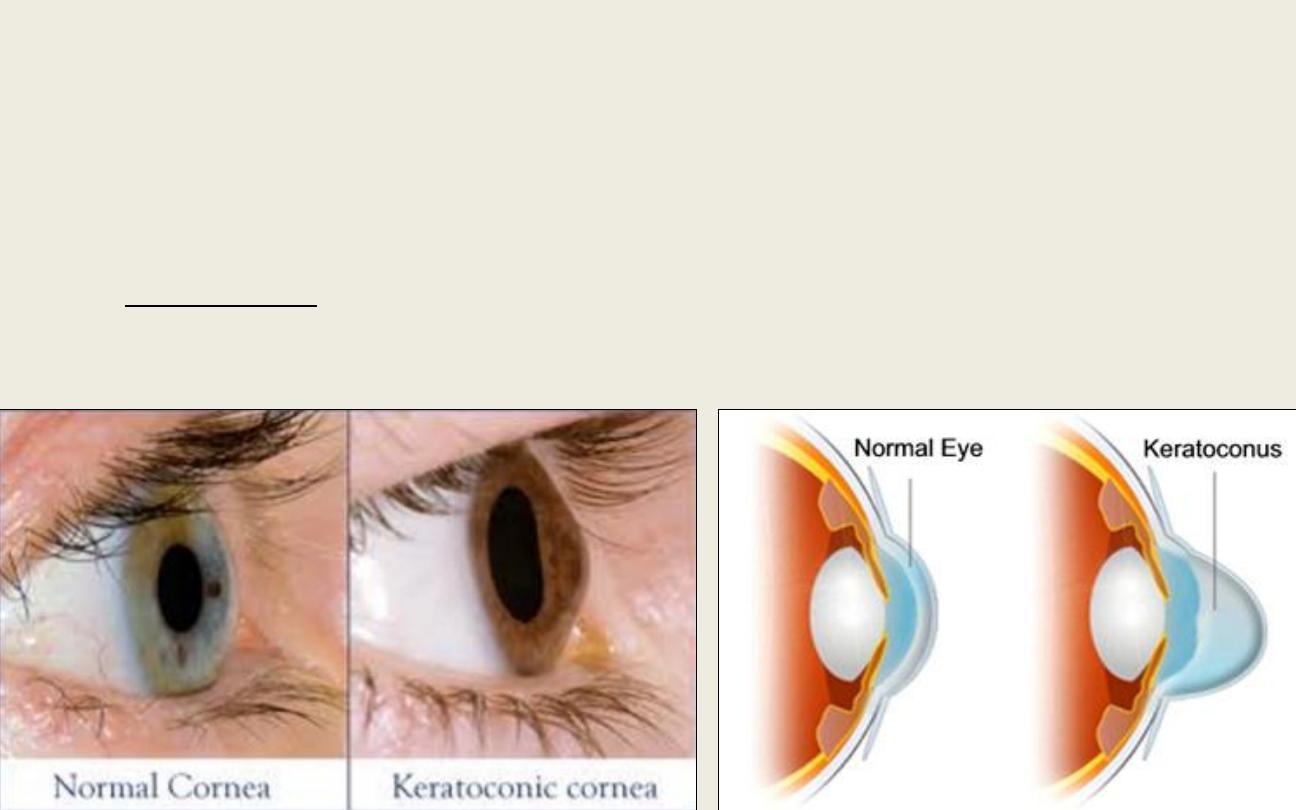
Keratoconus
• there is progressive and irregular changes in the cornea making it more convex
and make it have a more conical shape, also there is severe thinning of the cornea
that the cornea may reach 1/3 its original thickness (about 0.16mm). These
deformities will affect the visual acuity (as the cornea is the most important
focusing power) leading to myopia and irregular astigmatism.
• Presentation: Unilateral impairment of vision
Frequent changes in spectacle prescription or decrease tolerance to contact lens
The fellow eye usually has normal vision with negligible astigmatism at
presentation
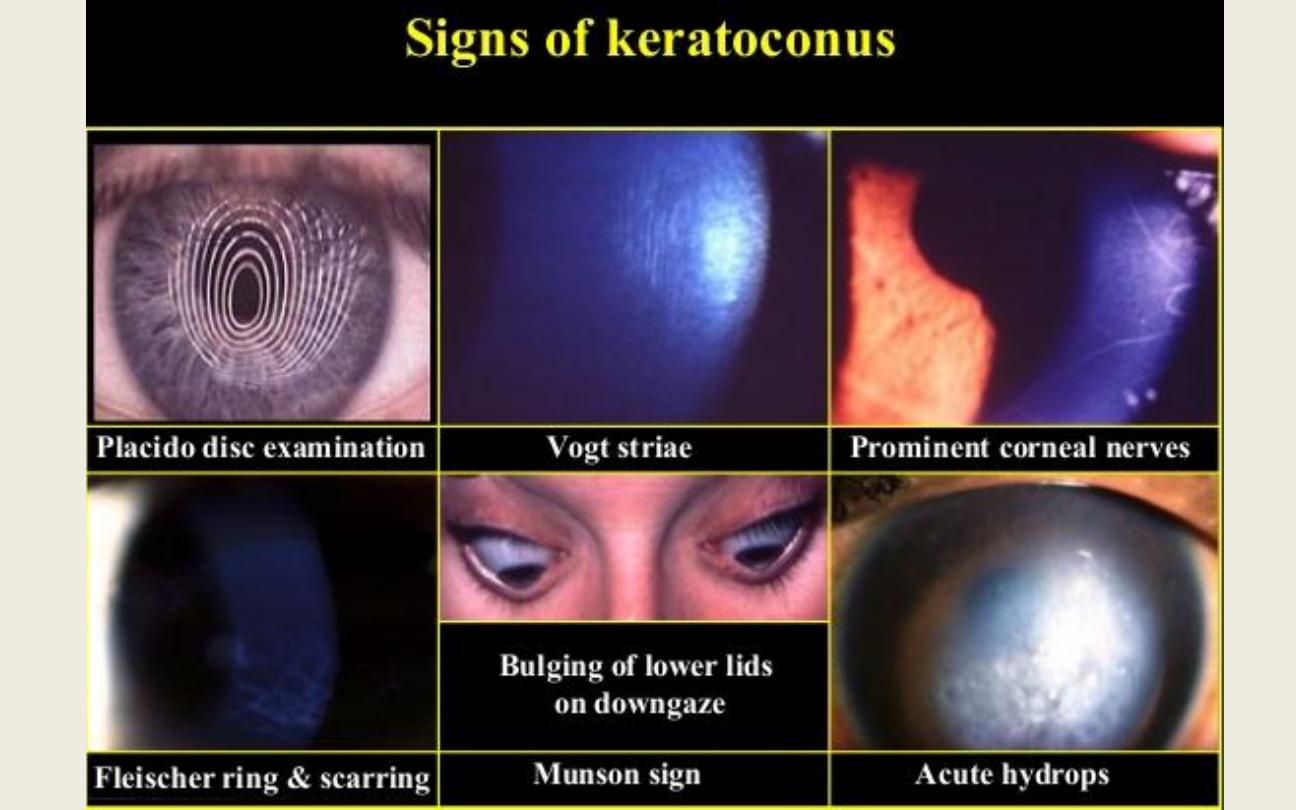
• Signs of keratoconus:
The hallmarks are: 1- Central or paracentral stromal thinning. 2- Apical protrusion.
3- Irregular astigmatism.
1) Direct ophthalmoscope from a distance of one foot shows an oil droplet reflex.
2) Retinoscpoy (used for diagnosis of refraction errors) shows an irregular reflex.
3) Slit-lamp shows very fine, vertical, deep stromal striae "Vogt's lines" due to
protrusion of cornea.
3) Later, there is progressive corneal thinning as little as one third of normal
thickness, associated with poor visual acuity (irregular myopic astigmatism).
4) Bulging of the lower lid in down gaze "Munson sign".
5) Acute hydrops: It is an acute influx of aqueous into the cornea as a result of a
rupture in Descemet's membrane sudden decrease in visual acuity associated
with discomfort and watering (lacrimation).
• Management:
1- Spectacles: 2- Rigid contact lenses: 3. Corneal collagen cross-linking 4. Corneal
ring implantation 5- Keratoplasty
“Uveal tract (Iris,
Ciliary body and
choroid)”
Anatomy
Uveitis
• Definition: inflammation of the uveal tract & adjacent structures, most probably
the retina.
Classification
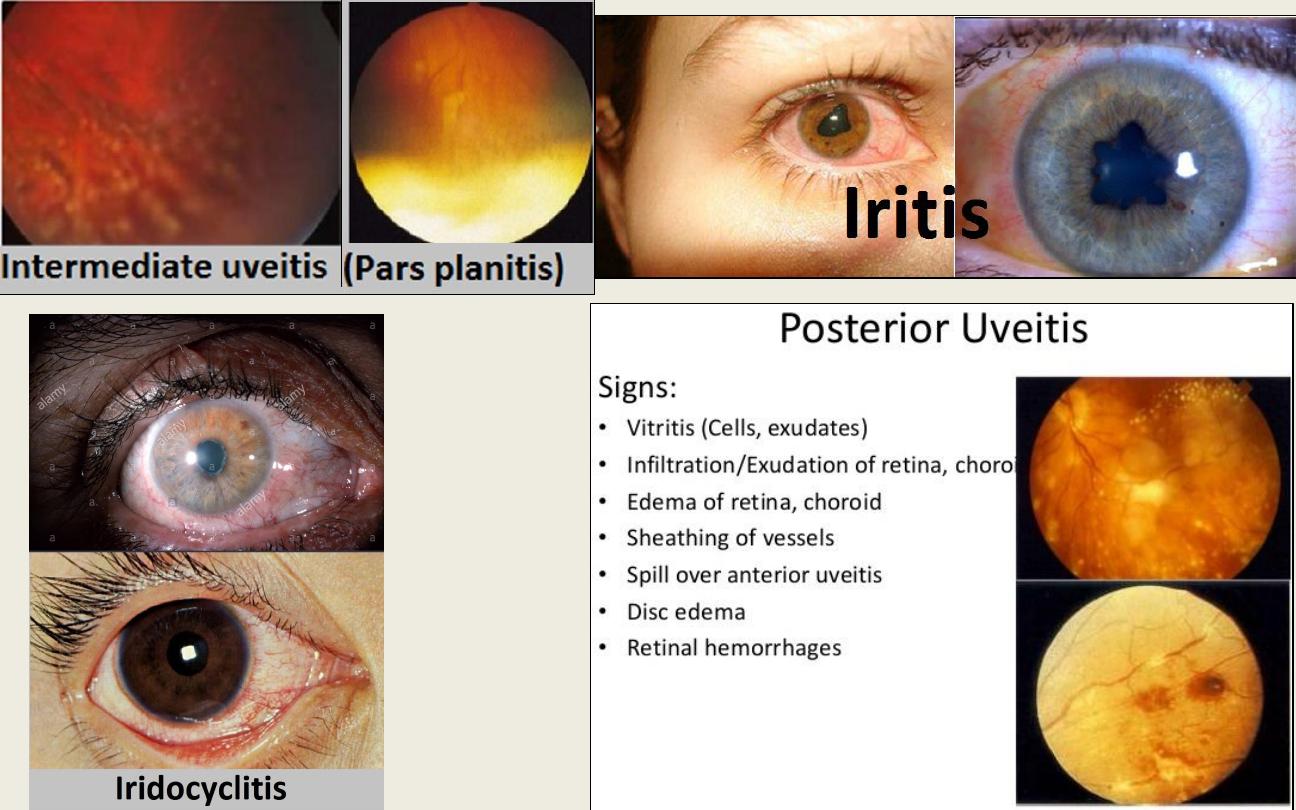
1) Anatomical Classification:
• Anterior uveitis: which is subdivided into: a- Iritis b- Iridocyclitis: iris & anterior
part of the ciliary body (pars plicata) are equally involved.
• Intermediate uveitis: posterior part of the ciliary body (pars plana), periphery of
the retina and the vitreous.
• Posterior uveitis: involve the fundus posterior to the vitreous base:
a) retinitis with primary focus in the retina
b) choroiditis with primary focus in the choroid
c) vasculitis which arteries and /or veins.
• Panuveitis: Involvement of the entire uveal tract.
2) Clinical classification:
• Acute uveitis: sudden, symptomatic onset and persists for up to 3 months.
• Chronic uveitis: insidious and may be asymptomatic, persists for > 3 months.
3) Aetiological classification:
• Idiopathic: more than 50% of cases.
• Associated with a systemic disease, e.g.:
a- Spondyloarthopathies: ankylosing spodylitis, Reiter's syndrome, psoriatic
arthritis and chronic juvenile arthritis.
b- Inflammatory bowel disease: ulcerative colitis, Crohn's disease, Whipple's
disease. c- Nephritis.
d- Non-infectious multi-system disease: sarcoidosis, Behçet's disease.
e- Infectious systemic disease: e.g. TB, syphilis f- Diabetes.
• Infections: a- Bacterial: tb b- Fungal: Candidiasis c- Viral: Herpes Zoster
• Infestations: a- Protozoa: Toxoplasmosis. b- Nematodes: Toxocariasis.
Note: endophthalmitis mean inflammation often purulent involve all intra ocular
tissues except sclera.
Clinical Features:
1) Anterior uveitis
• Symptoms: Acute: Photophobia, pain, redness, decreased visual acuity & lacrimation.
Chronic: many patients asymptomatic until development of complications occasionally give
rise to mild redness so usually the eye white .
• Signs: 1) Circumcorneal injection 2) Keratic precipitates
3) Cells: Aqueous cells & Anterior vitreous cells. 4) Aqueous flare: It is graded from 1 to 4
according to its haziness or obscuration to the details of iris. 5) Iris nodule:
• Complications of anterior uveitis:
1- Posterior synechiae: ends with secondary angle closure glaucoma.
2- Cataract. 3- Glaucoma: inflammatory or secondary angle closure glaucoma.
4- Cyclitic membrane formation which leads to phthisis bulbi.
2) Intermediate Uveitis
• Symptoms: Initially, floaters and later, decreased visual acuity.
• Signs: Cellular infiltration of vitreous (vitritis).
• Complications: 1- Cystoid macular oedema. 2- Cyclitic membrane and phthisis bulbi.
3- Cataract. 4- Tractional retinal detachment.
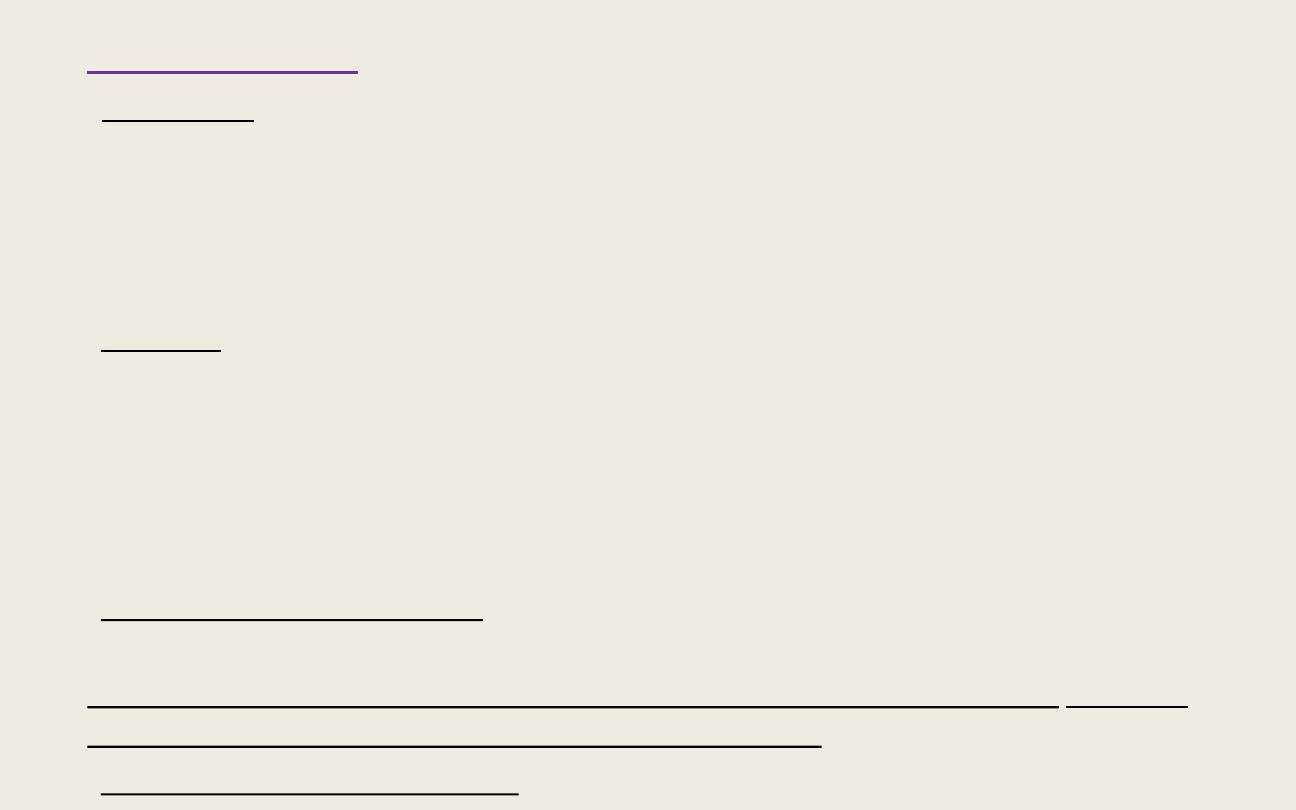
3) Posterior uveitis
• Symptoms:
1) Floaters.
2) Impairment of visual acuity.
• Signs:
1) Cells, flare, opacities & posterior vitreous detachment.
2) Retinitis
3) Vsculitis
4) chorioditis
• Complications:
1) Cystoid macular oedema.
2) Macular ischaemia.
3) Epiretinal membrane formation.
4) Vascular occlusion.
5) Retinal detachment (tractional).
6) Consecutive optic neuropathy
Treatment:
1) Mydriatics:
Short acting: Tropicamide, Cyclopentolate. Both have mydriatic & cycloplegic effects
Phenylnephrine (sympathetic agonist) has no cycloplegic effect.
Long acting: Atropine most powerful cycloplegic and mydriatic, its duration of action
is 2 weeks. Homatropin: had duration up to 2days
2) Steroids:
Topical steroids: Only for anterior uveitis. Potent steroids are: prednisolone acetate,
Dexamethasone and betamethasone. Periocular injection of steroids
Intravitreal injection of steroids: Injection of triamcinolone acetonide
Systemic steroids: Either orally: prednisolone tablets Or as injections: intravenous
infusion of methylpredinsolon.
3) Immunosuppressive agents: Either Antimetabolites (cytotoxic) as Azathioprine and
Methotrexate, Or T-cell inhibitors as ciclosporin.
• 1, 2 and 3 are used to treat cases with undetected etiology (idiopathic). But if we
find a cause, so the treatment is by 1, 2 in addition to:
4) Treatment of underling cause. e.g. TB, syphilis, toxoplasmosis, toxocariasis, ect.
“Lens”
Anatomy of the lens
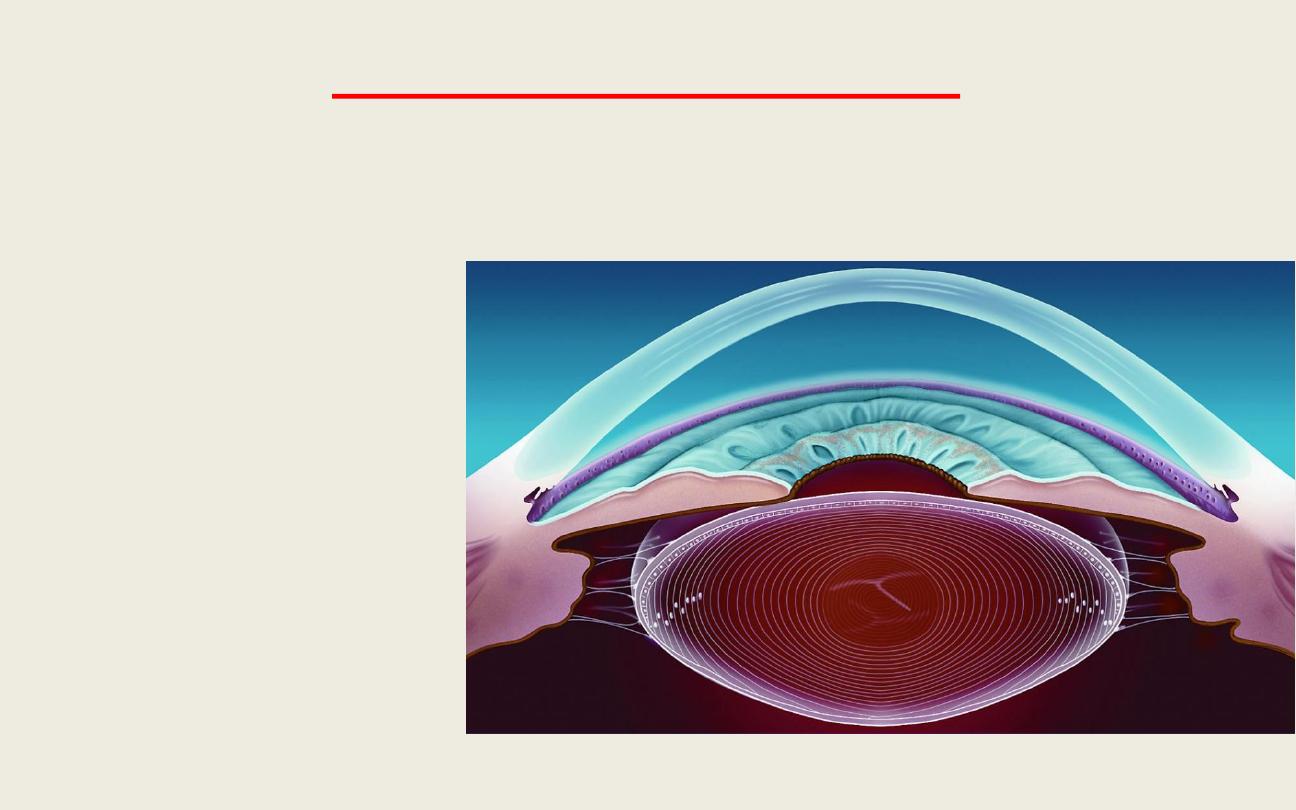
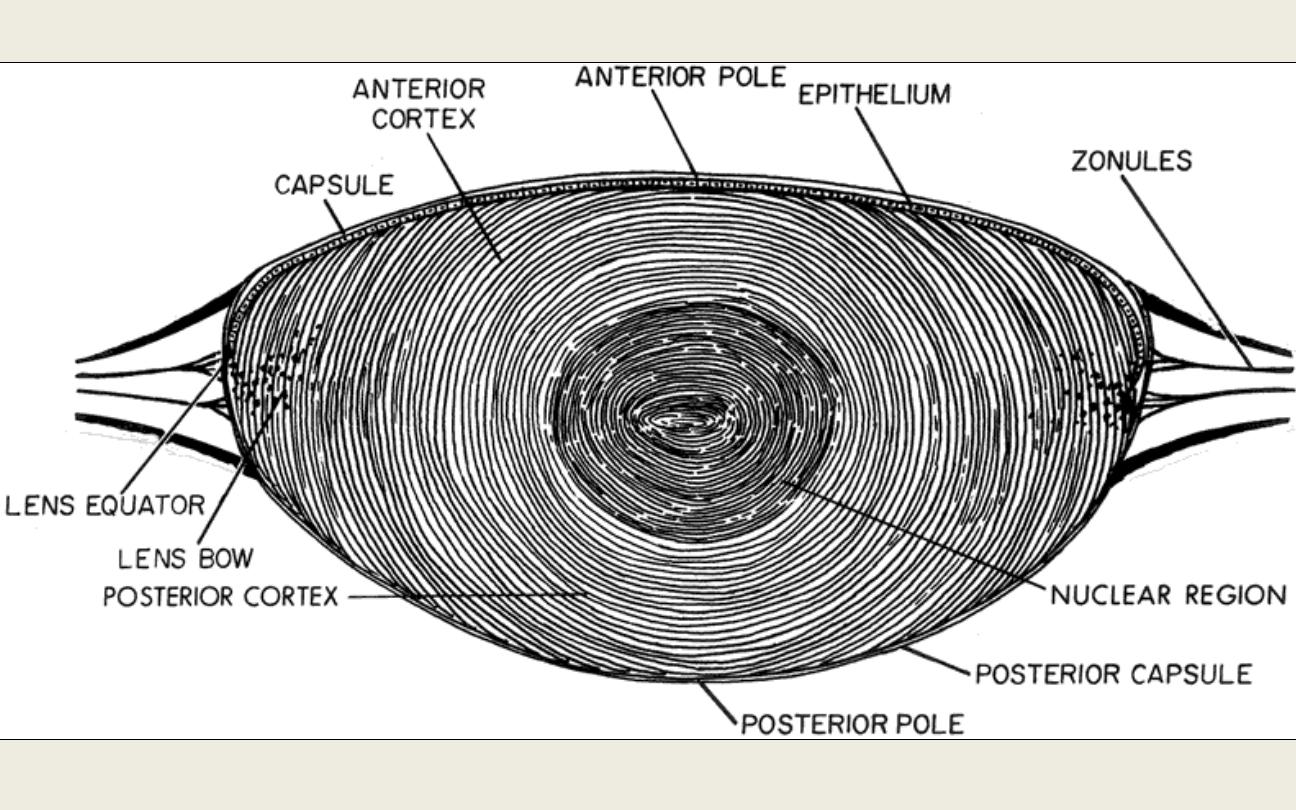
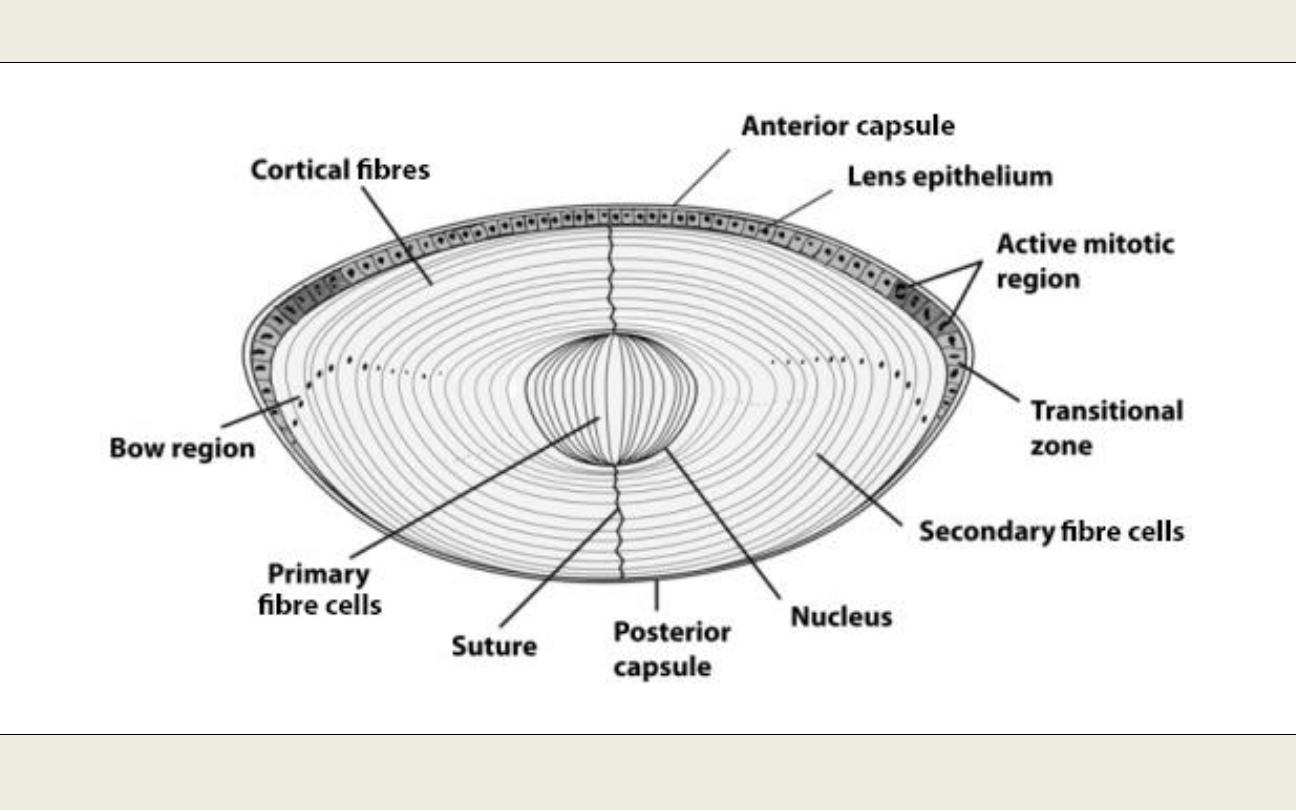
• The crystalline lens is a biconvex, avascular transparent structure enclosed by a
capsule.
• The lens consists of:
1) Nucleus: represents the
older lens fibers formed
during intrauterine life
and early years of life.
2) Cortex: represents the
newly formed epithelial
cells,
3) The capsule: which is
the thickest basement
membrane in the body.
Symptoms & signs of diseases of lens
1) Cataract: lead to painless impairment visual acuity.
2) Presbyopia: decrease in accommodation (due to decreased elasticity) leading
impairment of near vision.
3) Nuclear sclerosis: lead to increase the difference between the refractive indices
of the nucleus and cortex causes "index (lenticular) myopia".
4) Monocular diplopia: due to opacification or tilting of lens producing two images
in the same eye due to diffraction of light.
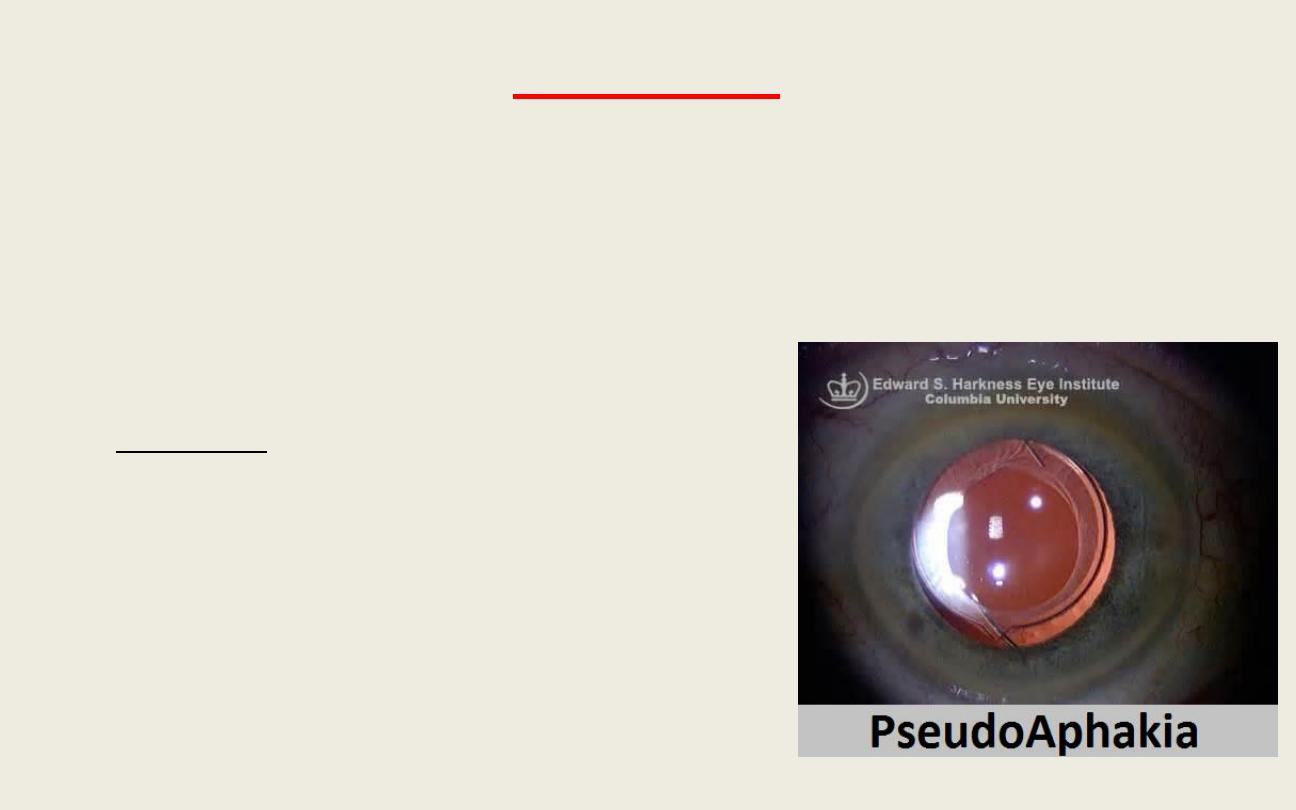
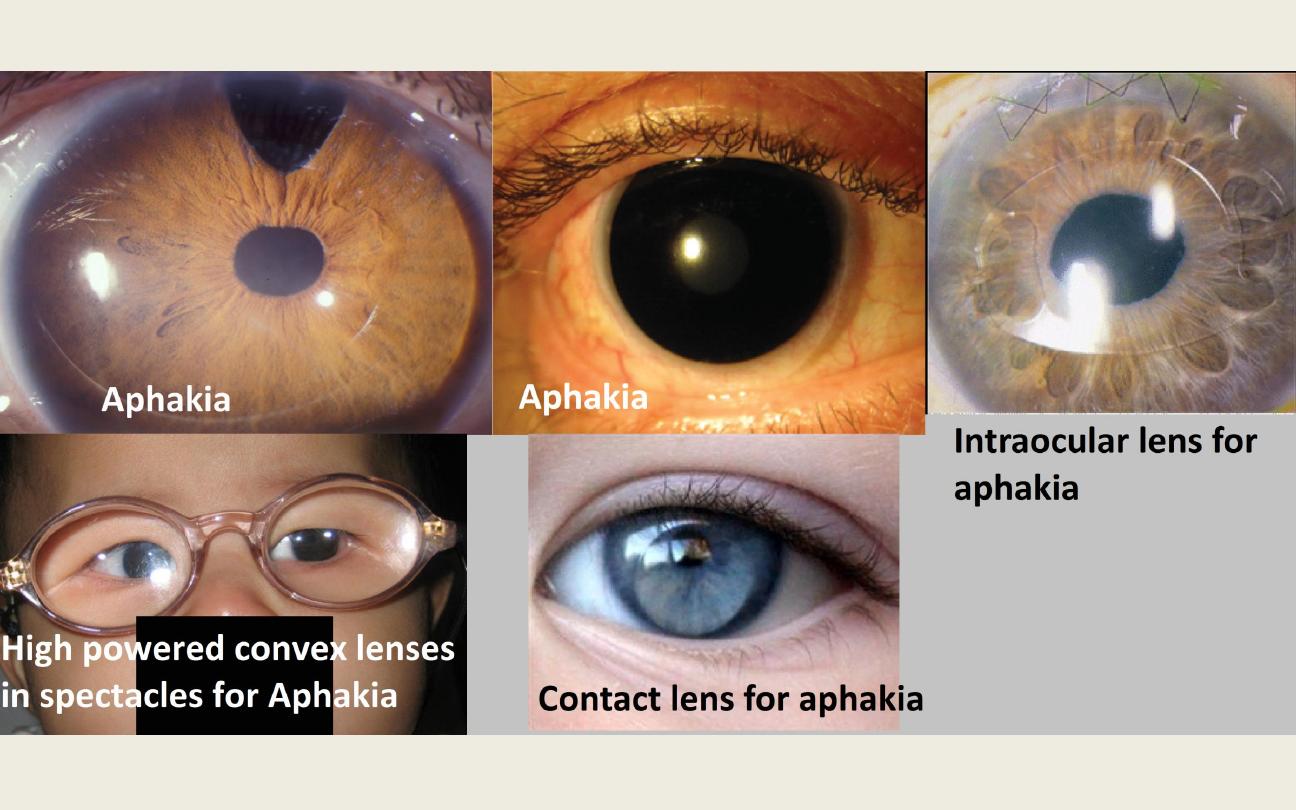
Aphakia
• Congenital or acquired absence of the lens from the eye, or its absence from the
pupillary area (luxated).
• An aphakic eye is usually strongly hypermetropic where parallel rays of light are
brought to a focus behind the retina.
• All accommodation is abolished.
• Treatment:
High powered convex lenses in spectacles:
Contact lens (1% magnification). This is can be
used without diplopia in aphakic eye if the other
eye is phakic or pseudophakic.
IOL (intraocular lens): is the best way of
correction as there is no magnification at all.
Cataract
• Any congenital or acquired opacity in the lens or its capsule, irrespective to the
effect on vision, is a cataract.
• Types of cataract:
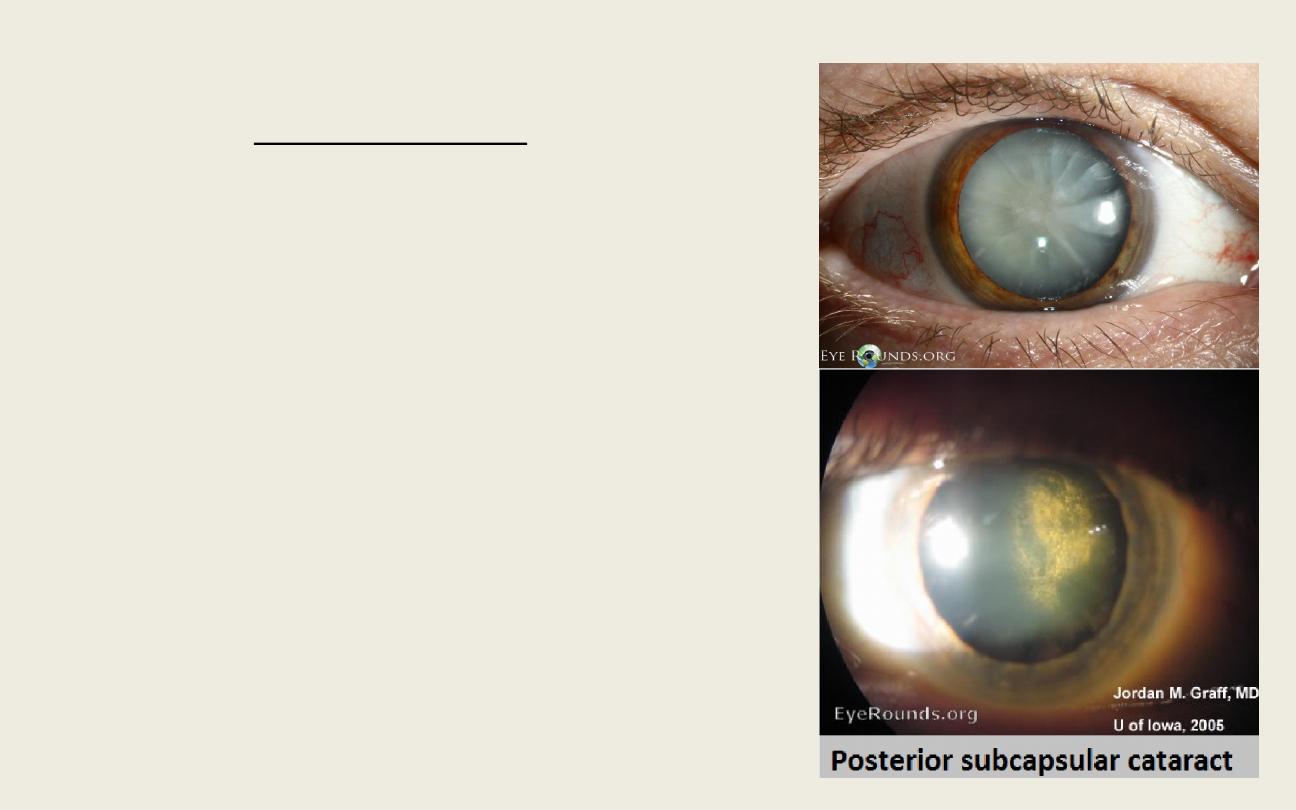
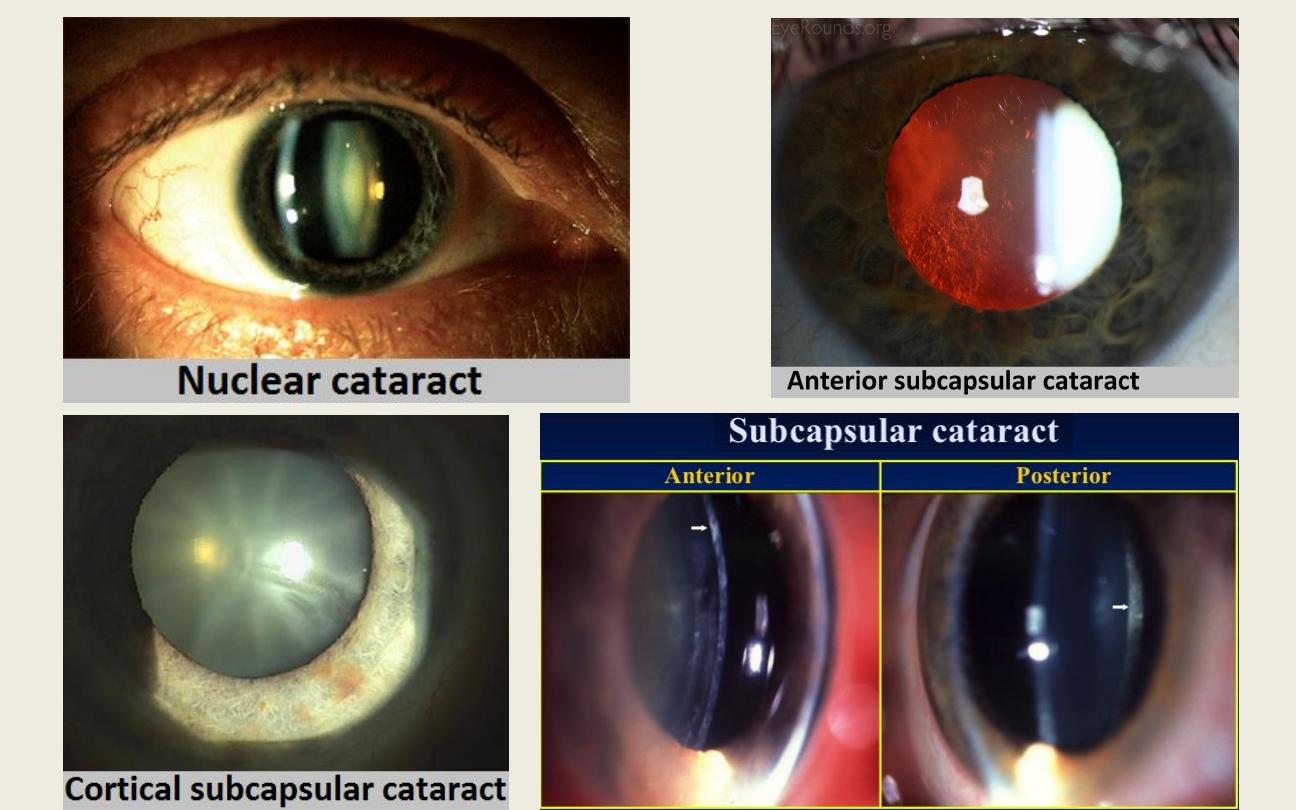
1) According to its site within the lens:
a- Posterior subcapsular: just anterior to the posterior capsule.
b- Anterior subcapsular: just posterior to the anterior capsule.
c- Cortical: cataract involving the cortex.
d- Nuclear: cataract involving the nucleus.
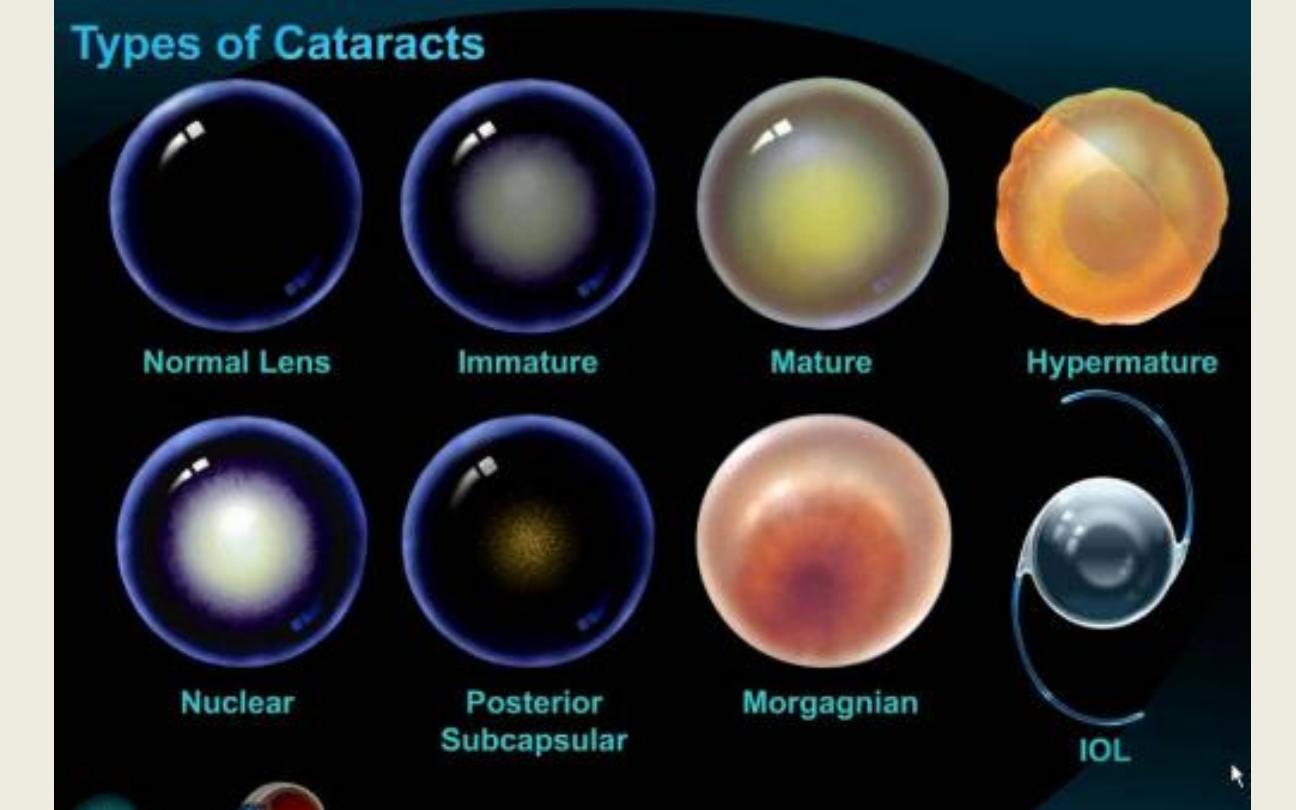
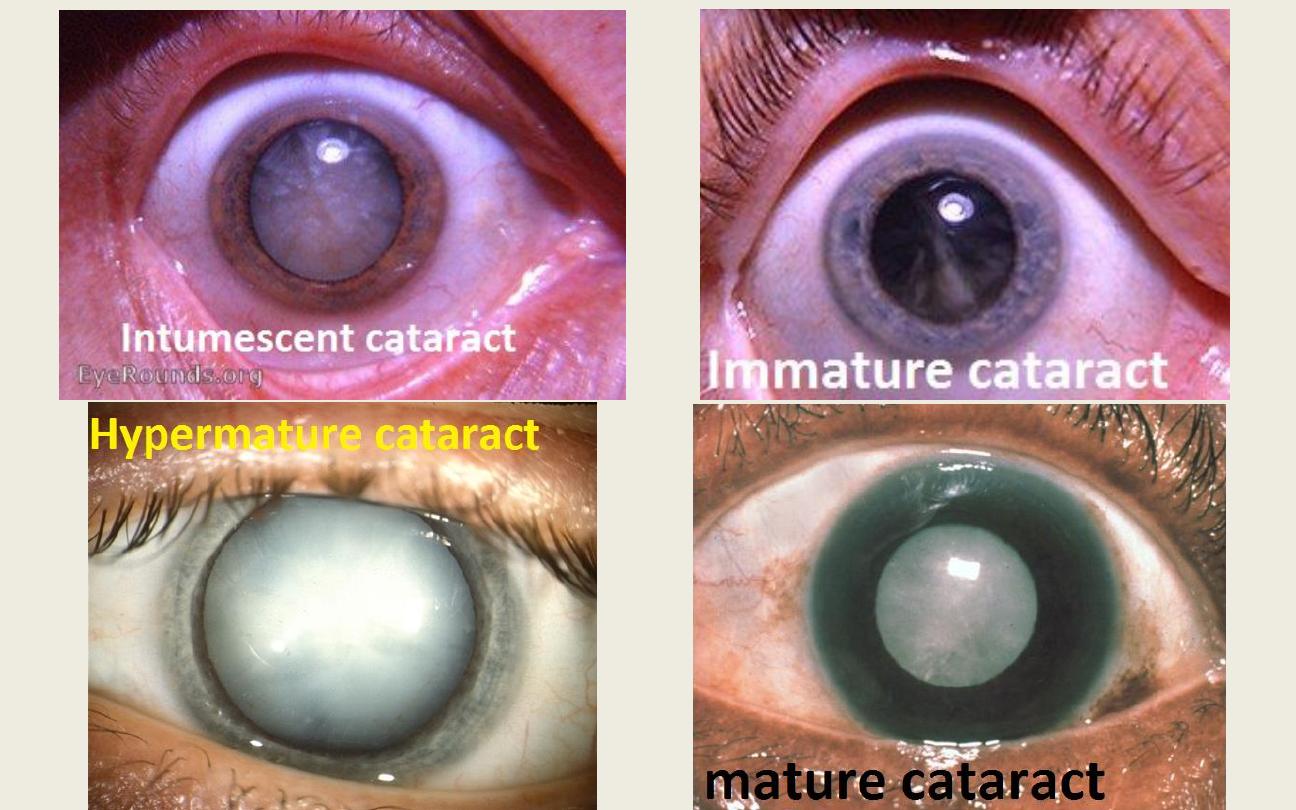
2) According to maturation:
a- Immature: if there is involvement of part of lens (any part), and other parts are
transparent.
b- Mature: complete opacification of the entire lens.
c- Hypermature Cataract: which is a mature cataract liquefaction, leakage of fluids
from the lens towards aqueous humor, shrinkage of lens and folding of capsule.
d- Intumescent Cataract (phacomorphic cataract):
In case of immature or mature cataract, if there is
influx of fluids from aqueous humor towards lens
lead to swelling of the lens. Some time, this
swelling will progress to a level sufficient to
occlude the angle of AC results in "Intumescent
Glaucoma".
3) According to its onset: either acquired or
congenital.
• Cataract can be detected by slit-lamp, direct
ophthalmoscope (where we have black dots in the
red reflex or total loss of red reflex) and B-scan
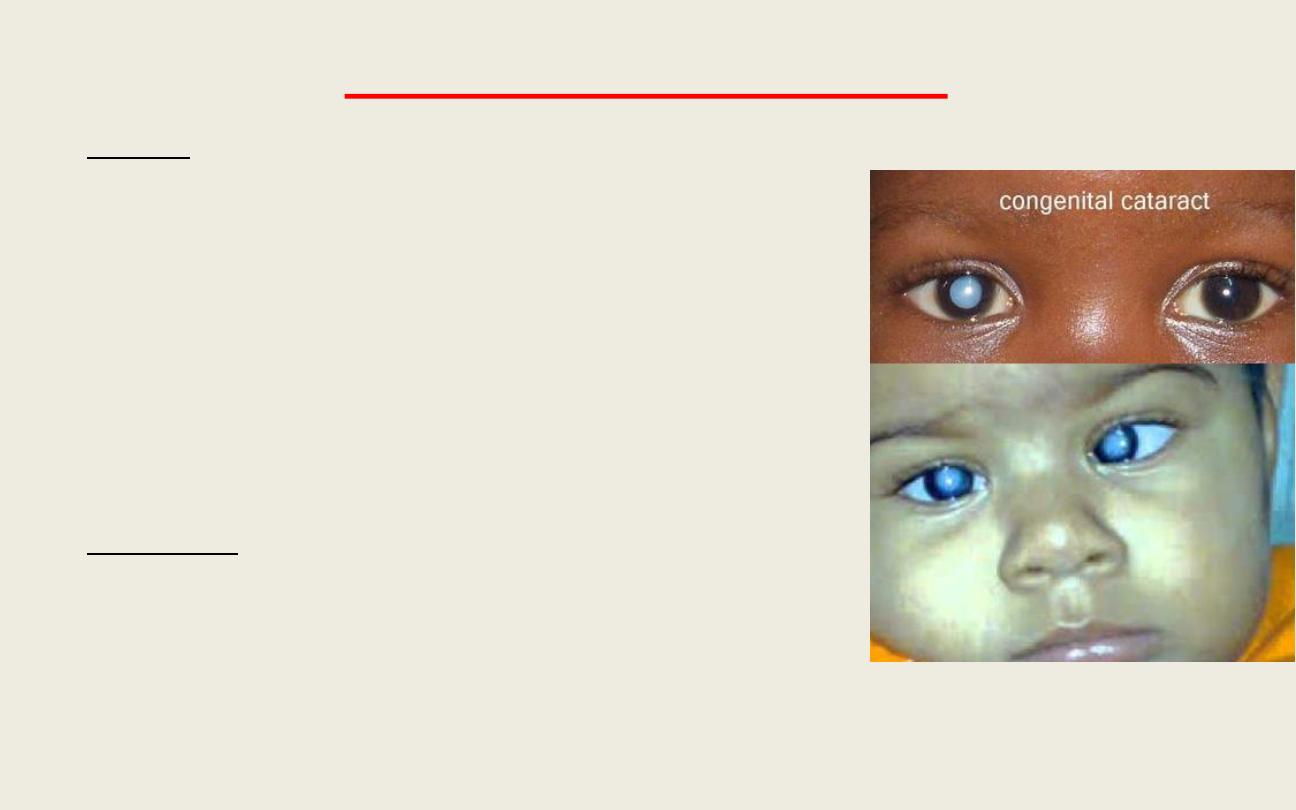
Congenital cataract
• Causes:
Isolated hereditary cataracts.
Metabolic cataract: a- galactosaemia b- Lowe's
(oculocerebral) syndrome
Prenatal infections: a- Congenital Rubella b- Others:
Cytomegalovirus, Herpes simplex and Varicella.
Chromosomal abnormalities: a- Down syndrome
(Triosomy 21). b- Other: Patau syndrome (Triosomy 13),
Edward syndrome
• Treatment:
If the cataract is so dense, visualization of retina is difficult
or impossible then surgery is urgently indicated.
Correction of aphakia in congenital cataract:
1- Unilateral aphakia: either IOL or contact lens (NO role
for glasses) 2- Bilateral aphakia: in addition to IOL &
contact lens, it can be corrected by spectacles.
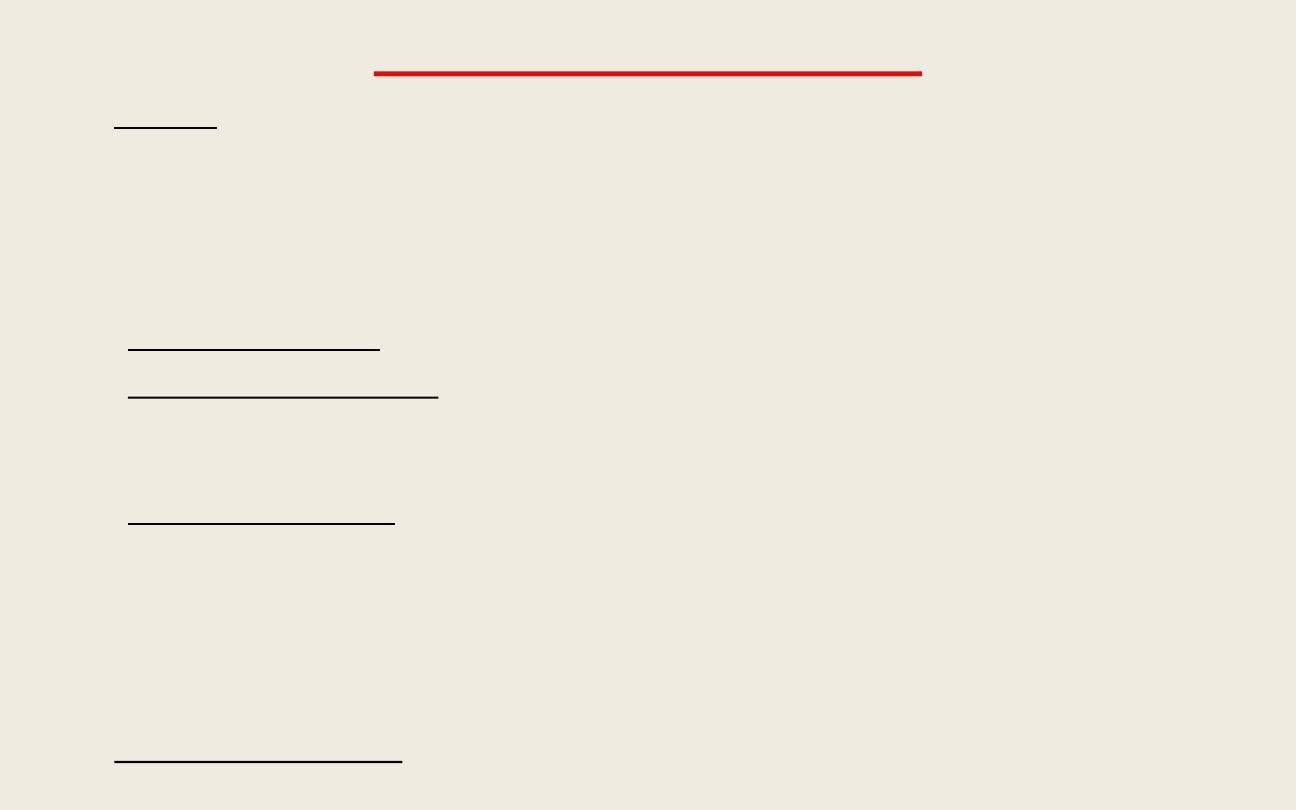
Acquired cataract
• Causes:
1) Age-related cataract: usually develops after the age of 60.
2) Pre-senile cataract: develops before the age of 60 in the following conditions:
a- Diabetes Mellitus b- Myotonic dystrophy c- Atopic dermatitis
d- Neurofibromatosis type 2.
3) Traumatic cataract
4) Drug-induced cataract: a- Steroids: both systemic & topical b- Chlorpromazine.
c- Amiodarone (anti-arrhythmic). d- Gold.
e- Allopurinol: used in hyperuricaemia and chronic gout.
5) Secondary cataract as a result of some other primary ocular disease:
a- Chronic anterior uveitis: most common cause of secondary cataract.
b- Acute congestive angle-closure glaucoma.
c- High (pathological) myopia.
d- Hereditary fundus dystrophies, such as retinitis pigmentosa.
• Treatment of catract: Surgery there is NO effective medical treatment
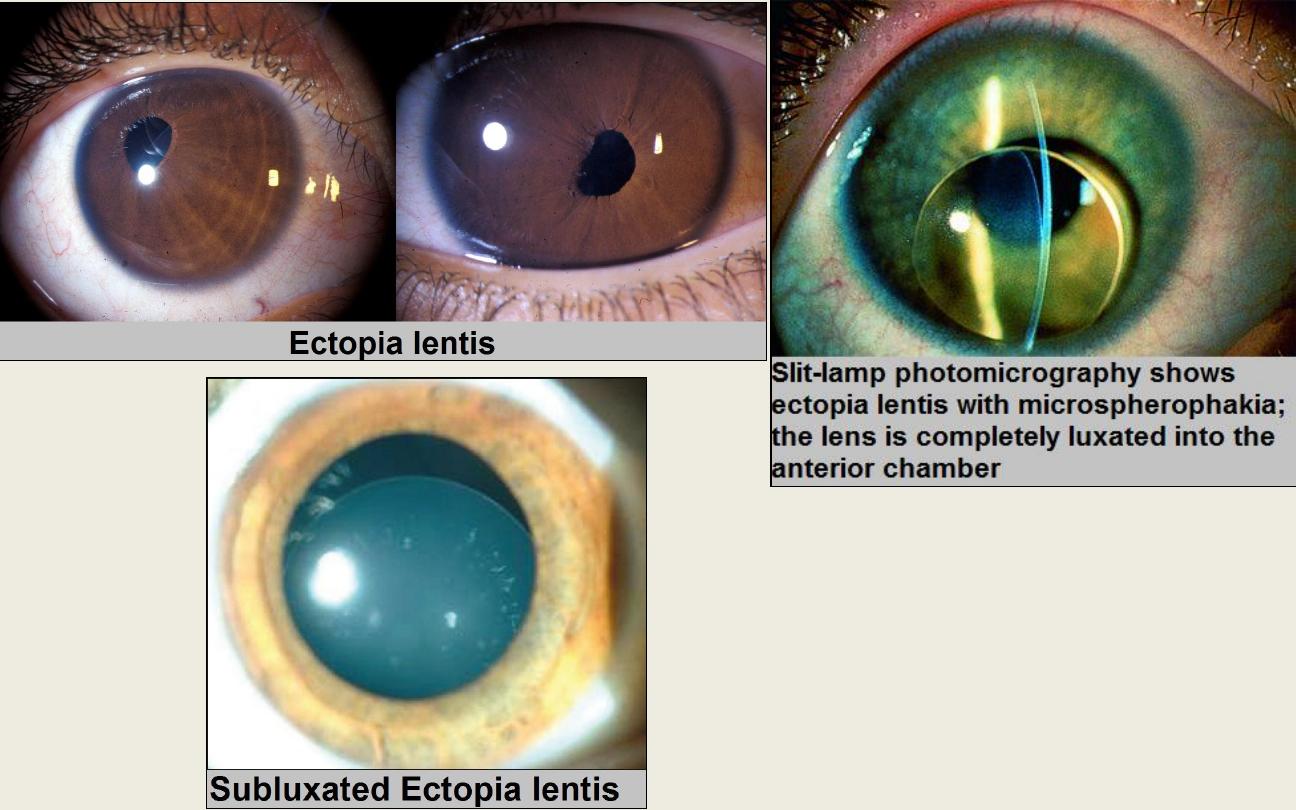
Ectopia lentis
• displacement of the lens from its normal position which may be completely
dislocated "Luxated" (complete destruction or cut of zonules) or partially
dislocated "Subluxated".
• Causes:
1) Acquired: - Trauma. - Large eye {high myopia, buphthalmus (congenital
glaucoma)}. - Anterior uveal tumour - Hypermature cataract.
2) Congenital: a- Without systemic association: AD, AR or associated with aniridia
(congenital absence of iris) b-With systemic association: e.g., Marfan's syndrome,
Weill-Marchesani syndrome, homocystinuria, Ehlers-Danlos syndrome.
• Complications of ectopia lentis:
1- Refractive errors: myopia and astigmatism 2- Glaucoma
3- Endothelial touch: damage to endothelium of cornea. 4- Lens induced uveitis
• Indications of treatment:
1- Refractive error 2- Glaucoma
3- Endothelial touch 4- Lens induced uveitis (which is chronic)
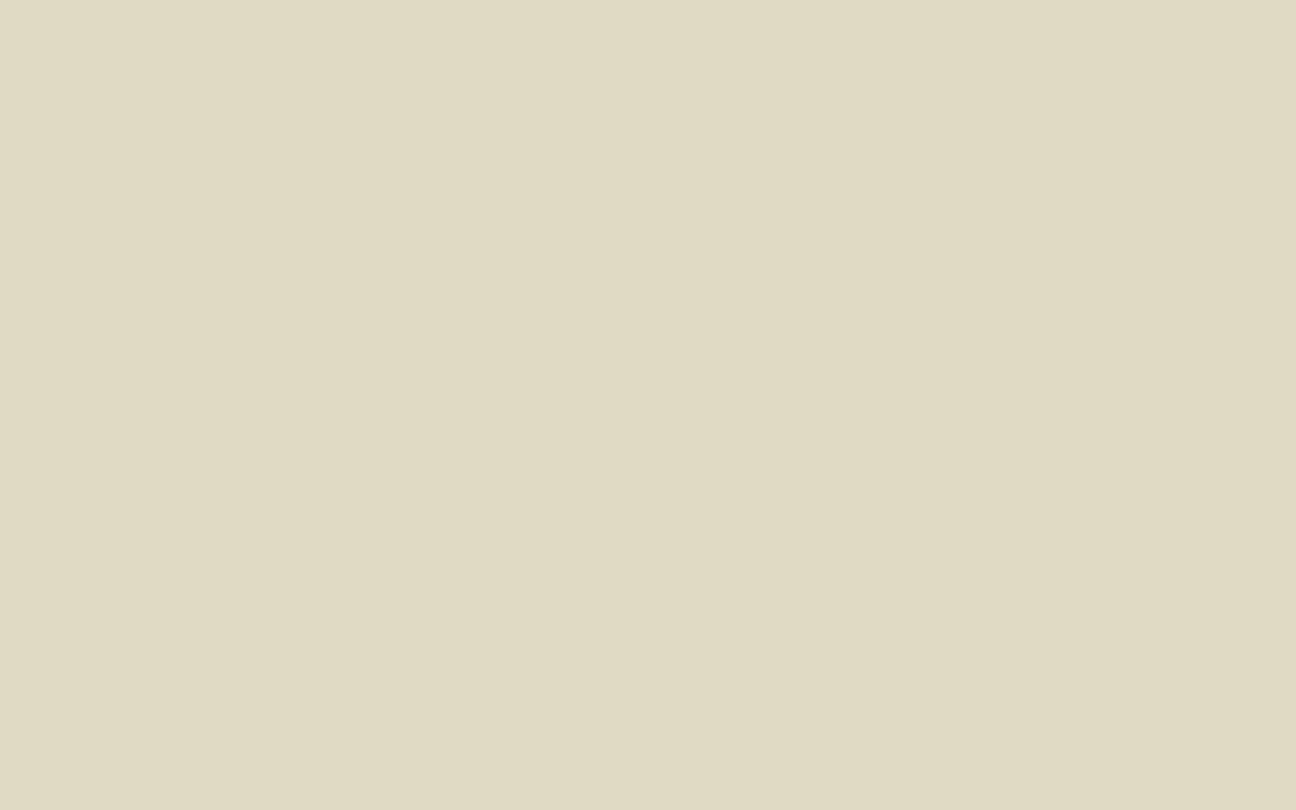
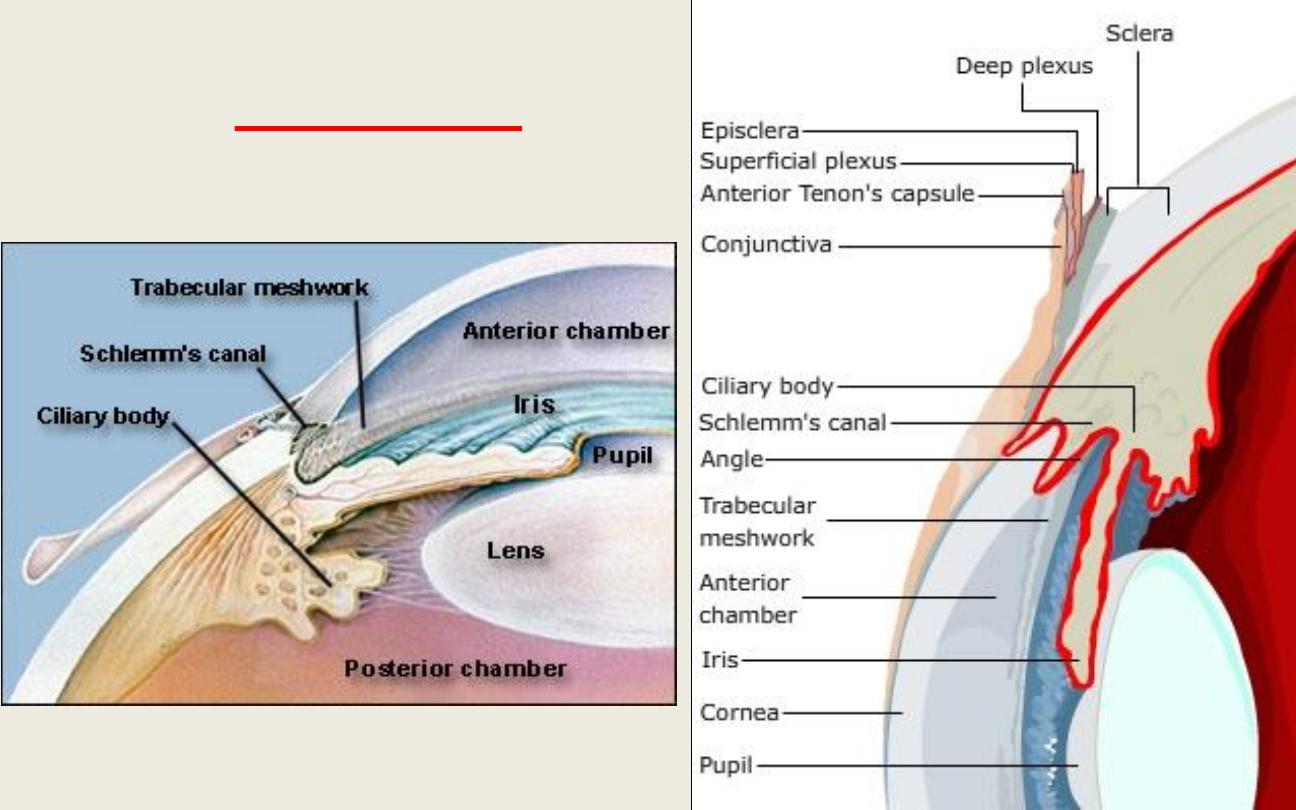
“Raised
intraocular
pressure (IOP)”
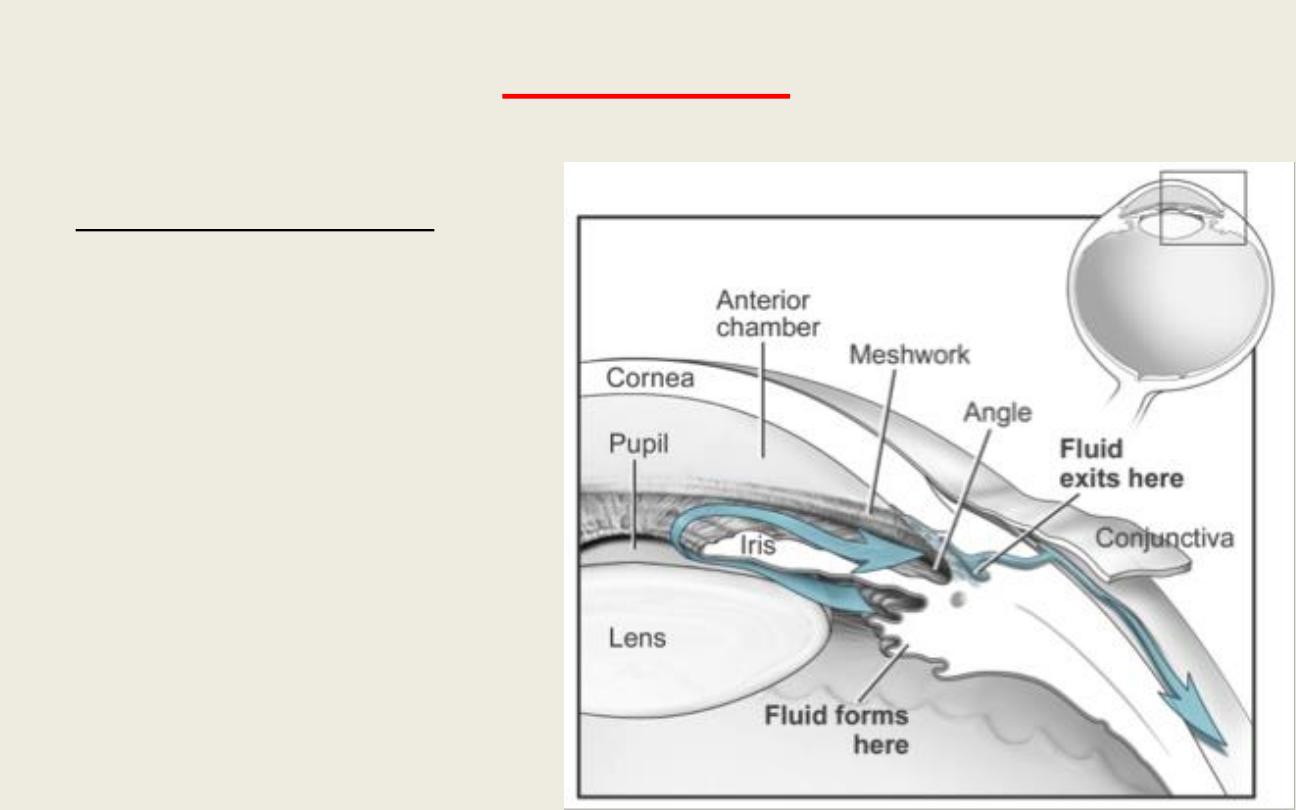
Anatomy
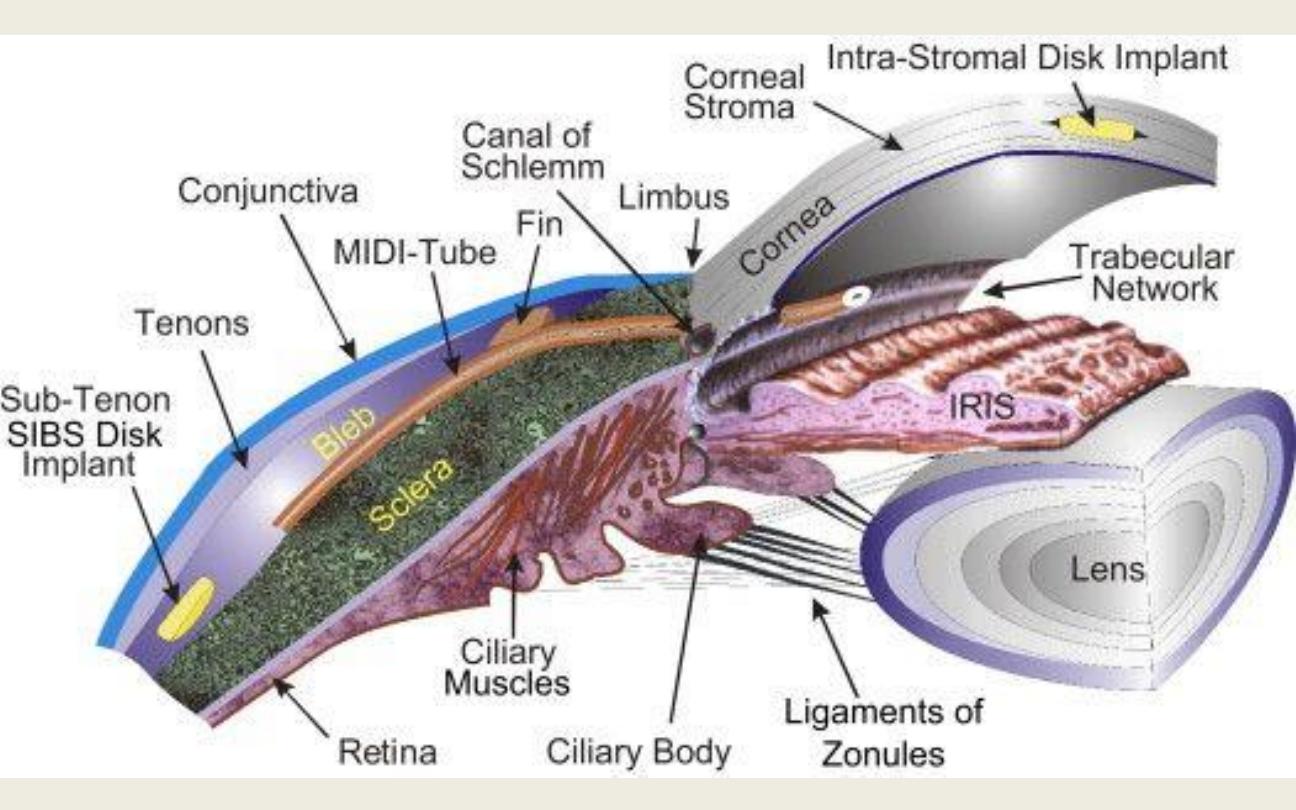
The trabecular meshwork: It is a
sieve-like structure at the angle of
the anterior chamber through
which 90% of the aqueous humour
leaves the eye.
Ocular hypertension
• ‘Normal' IOP range of 11-21 mm Hg..
• It is estimated that about 7% of the population over age of 40 years have IOPs >
21 mm Hg without glaucomatous damage on standard clinical tests. These
individuals are referred to as ocular hypertensive or glaucoma suspects.
Glaucoma
• It is an optic neuropathy with characteristic appearance of the optic disc and
specific pattern of visual field defect that is associated frequently but not
invariably with raised intraocular pressure (IOP)
• Classification of glaucoma: 1) Congenital (developmental).
2) Acquired: divided into: a- Open angle: this is either primary (raised IOP not
associated with other ocular disorders) or secondary.
b- Angle closure: also either primary or secondary.
• We use gonioscopy to determine the type of glaucoma, so if we see the structures
of the angle, then it is open angle glaucoma, while if we do not see some or all of
these structures, then the angle is closed or occludable. The structures seen
normally by gonioscopy (using goniolens) in the angle are; (anterio-posteriorly)
schwalbe's line, trabecular meshwork, scleral spur & anterior face of ciliary body.
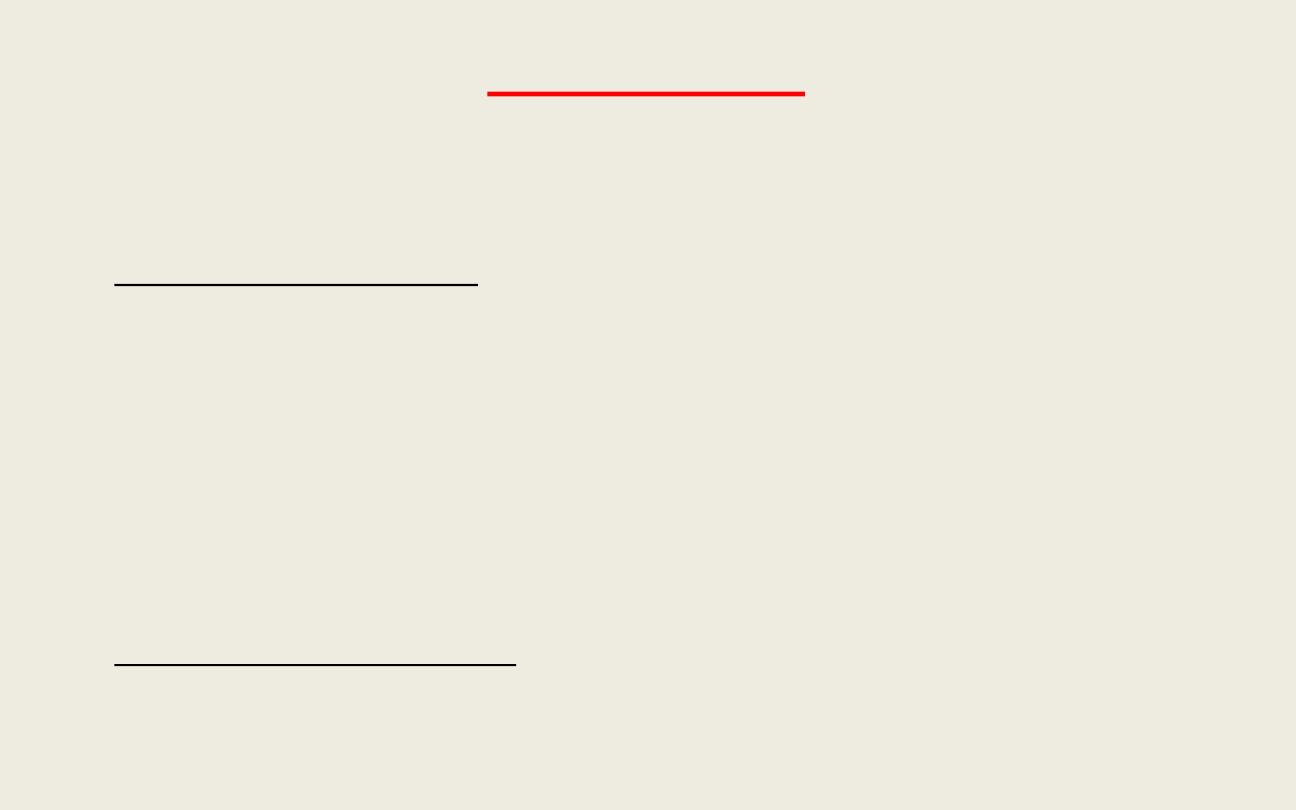
• The cup:disc ratio (C/D ratio):
Should be measured in both vertical (more important) & horizontal meridian.
Most normal eyes have a vertical C/D ratio of 0.3 or less (<30%). So C/D ratio > 0.3
or difference of 0.2 (20%) between the 2 eyes should be regarded with suspicion.
About 2% of population have CD ratio more than 0.3 and may even reach 0.7 and
they are really normal, and to consider it glaucoma we have to have either raised
IOP or optic neuropathy (we must have two of three of the diagnostic criteria of
glaucoma to say this is glaucoma).
C/D ratio assessed and calculated by:
o Clinical fundal examination and fundus photograph. (crude method)
o Now a day we use very sophisticated method of imaging technique called
Heidelberg retinal tomography (HRT). The imaging technique is used in diagnosis
and follows up of patients with glaucoma.
o Ocular coherent tomography (OCT) which is work in the similar way of
ultrasonography but instead of using reflected sound, reflected light is used. It give
accurate measurement of nerve fibers layer changes and C\D ratio assessment.
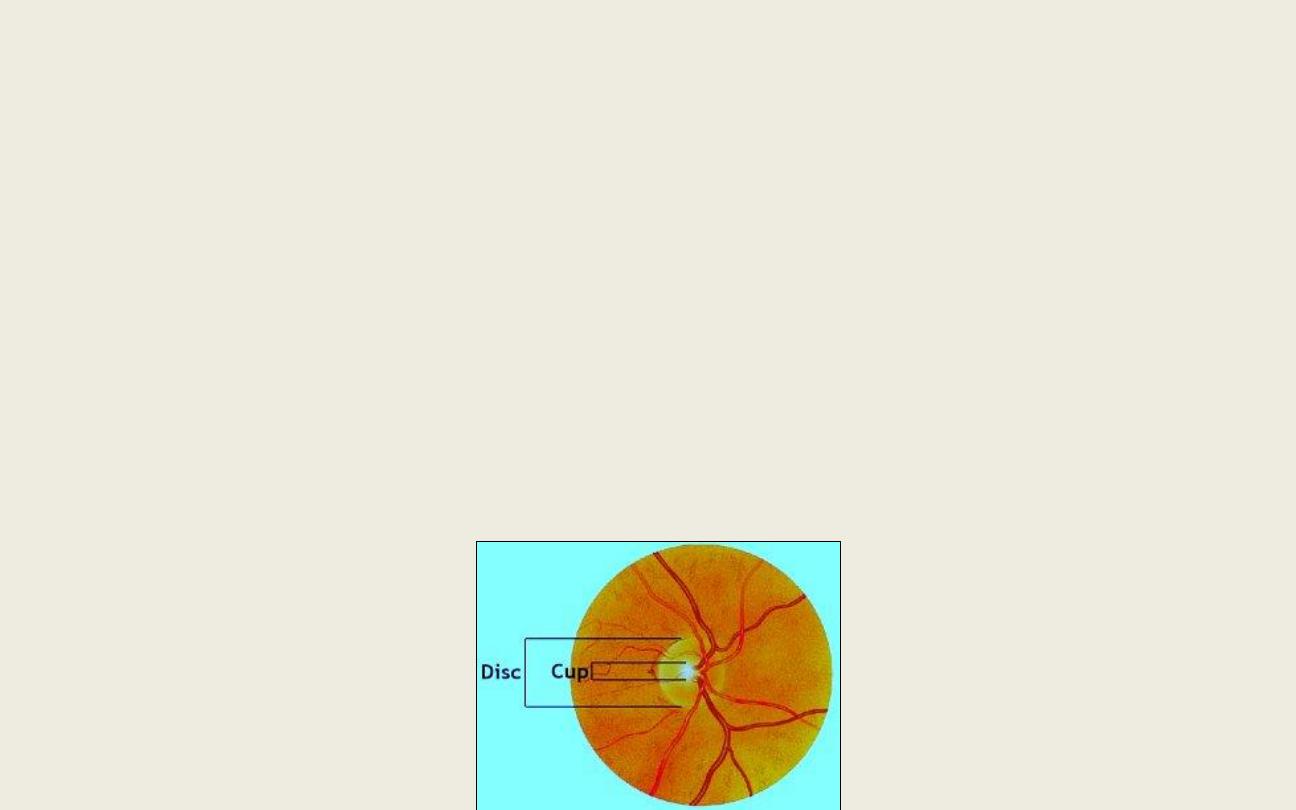
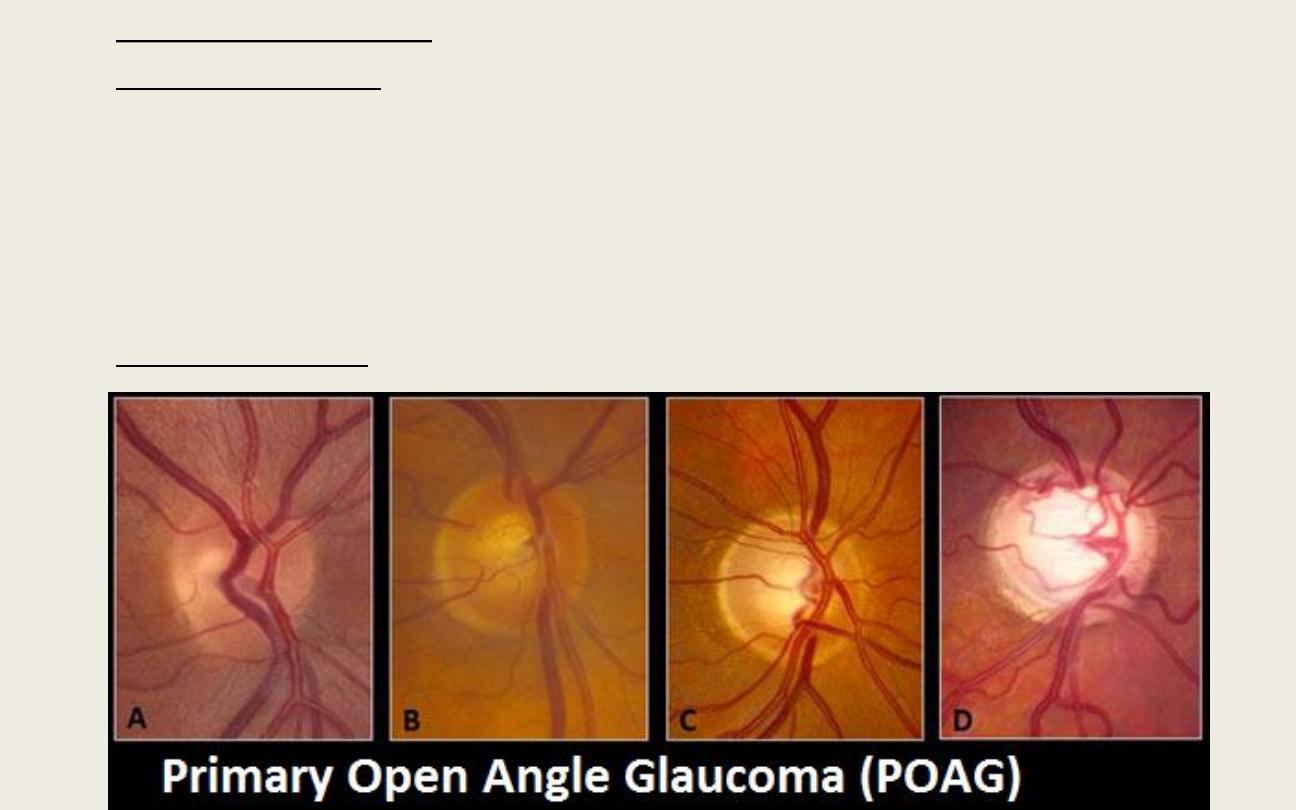
Primary Open Angle Glaucoma (POAG)
• Definition: a bilateral disease (in general) although not necessarily a symmetrical
disease. In POAG, the trabecular meshwork is exposed (angle is open) but the pores
are occluded (sclerosis of trabecular meshwork for unknown etiology).
• Clinical features: (of POAG): Insidious (gradual), asymptomatic until late in the
course of the disease due to significant loss of visual field.
• Signs of POAG:
1- Raised IOP. 2- Fluctuation in IOP In glaucoma (> 5 mm Hg).
3- Optic disc changes, increased C/D ratio > 0.3 or asymmetry of it (difference > 0.2
between both eyes). 4- Glaucomatous field change.
5- Gonioscopy, show open angle with no any abnormality (e.g. no new blood
vessels or inflammatory cells occluding the angle)
• Visual field changes: 1- Generalize constriction of peripheral VF (not specific sign).
2- Paracentral scotoma: (central VF change which is specific sign).
3- Arcuate scotoma (central VF change).
4- Temporal (crescent) or central island of vision only (both are end-stage glaucoma)
• Management of POAG:
Medical treatment: Drugs used:
o Beta blockers: betaxolol is cardio-selective
o Dorzolamide is a carbonic anhydrase inhibitor.
o Brimonidine is an alpha-2 agonist. Latanoprost is a prostaglandin agonist.
o Parasympathomimetics (e.g. Pilocarbine) act on ciliary and specifically on its
longitudinal muscles which are inserted in scleral spur.
Surgical treatment
Primary Angle Closure Glaucoma (PACG)
• Definition: is a condition in which there is obstruction to aqueous outflow due to
partial or complete closure of the angle by peripheral iris.
• Unlike POAG, the diagnosis is by examination of anterior segment and gonioscopy.
• Classification of PACG:
1) Latent PACG: the asymptomatic phase of PACG.
• Signs:
Slit-lamp examination: a- Shallow AC. b- Convex-shaped iris-lens diaphragm.
c- Close proximity of iris to cornea. d- Normal IOP.
Gonioscopy: shows an occludable angle (grades 1 ,2 ,0).
• Management: Prophylactic bilateral YAG laser PI (peripheral iridotomy).
2) Intermittent (sub-acute) PACG:
• Clinical features: - Transient obscuration of vision. - Halos around light due to
corneal edema. - Eye ache. - Frontal headache. - Recurrent attacks
• Treatment: YAG laser PI to the affected eye and prophylactic PI to the fellow eye.
3) Acute congestive angle-closure glaucoma:
• This condition is caused by a sudden total closure of the angle.
• Clinical features:
Symptoms:
a- Rapidly progressive impairment of visual acuity, due to corneal oedema.
b- Periocular pain + congestion.
c- Nausea and vomiting in severe cases.
Signs seen with slit-lamp:
a- Ciliary flush due to injection of limbal and conjunctival blood vessels.
b- IOP severely elevated (>50mmHg).
c- Corneal oedema with epithelial vesicles.
d- Shallow AC + peripheral iridocorneal touch.
e- Aqueous humour flare (protein) + cells.
f- Pupil vertically oval + fixed in mid-dilated position, not reactive to light &
accommodation.
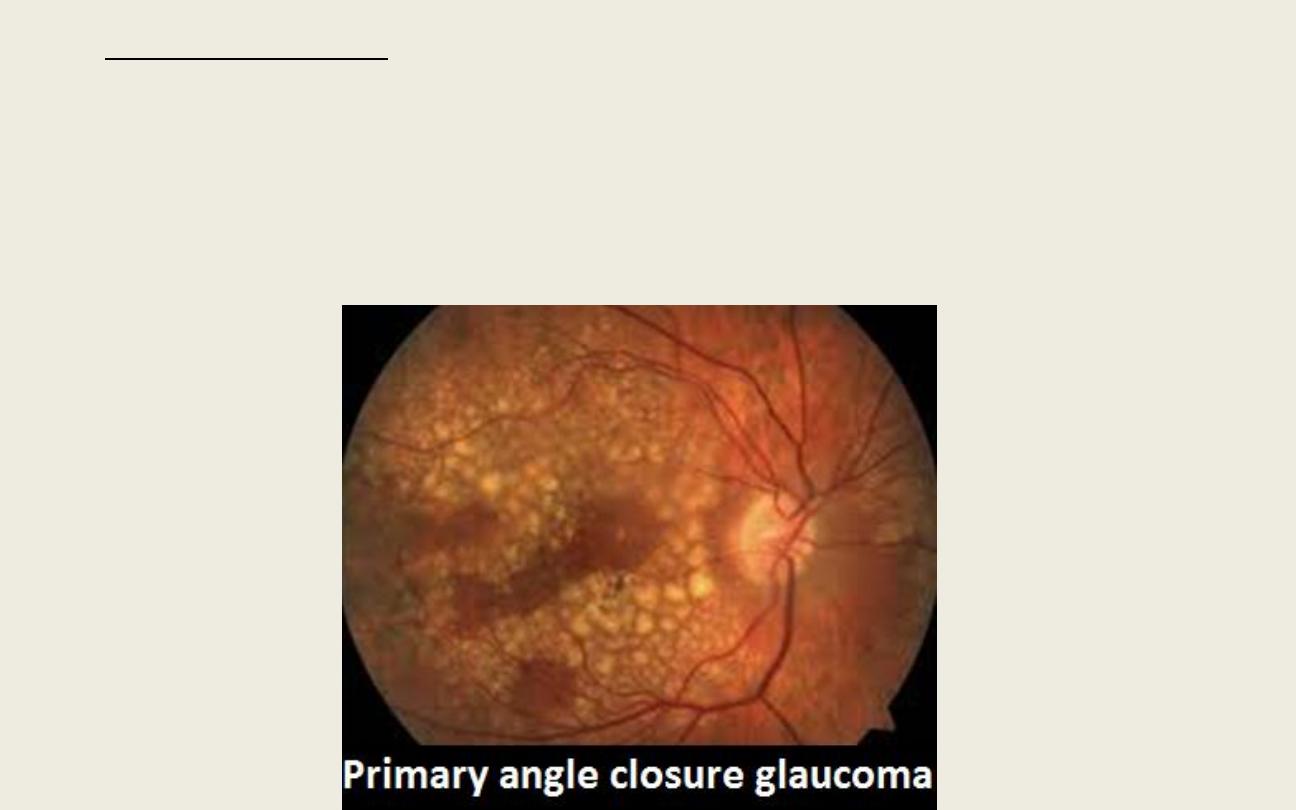
• Treatment is surgical: but initially we start medical treatment to control elevated
IOP which is by:
a- IV acetazolamide followed orally.
b- Hyperosmotic agents: - IV Mannitol. - Oral glycerol with lemon juice.
c- Topical therapy: i- Pilocarpine ii- Pilocarpine 1% x4 to unaffected eye (as
prophylaxis). iii- Beta-blocker. iv- Topical steroid.
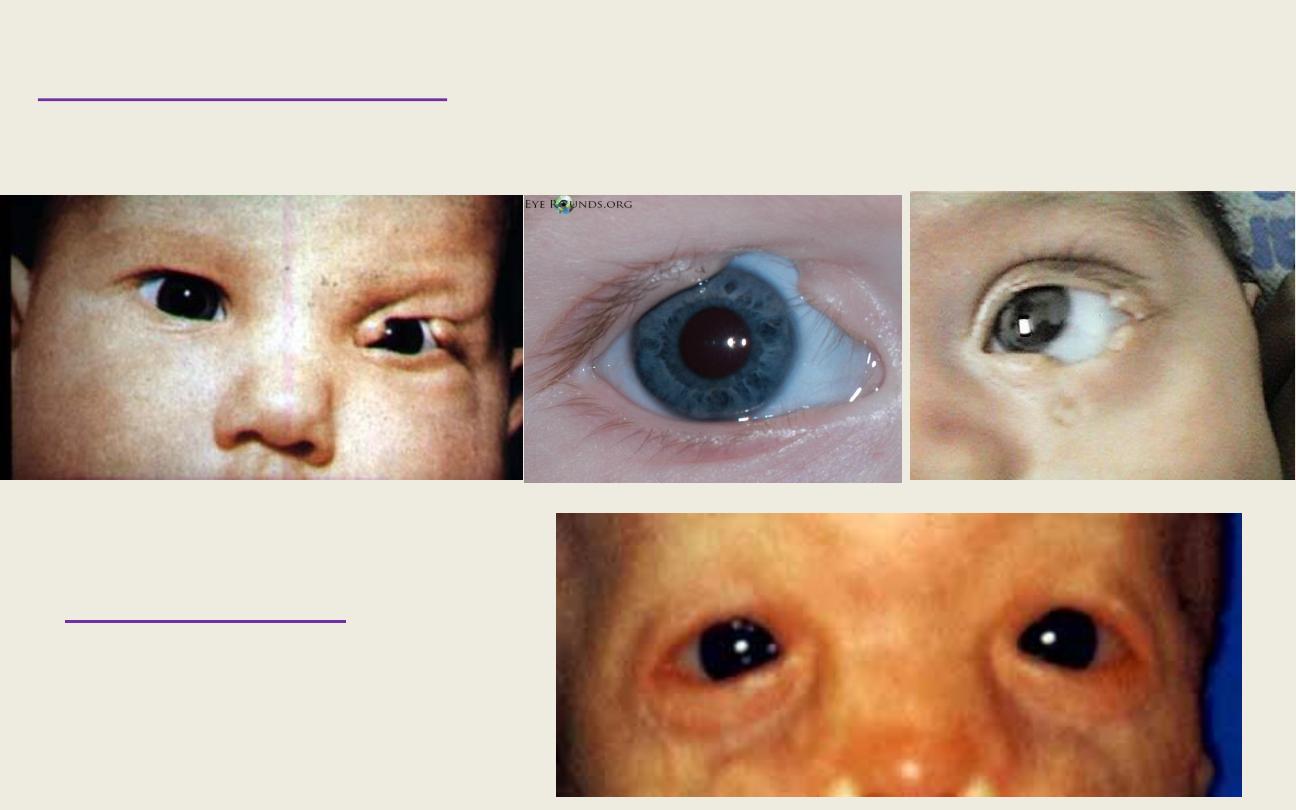
Congenital glaucomas
• Sever and potentially blinding disease.
• Types:
1) True congenital glaucoma: (40%), IOP is elevated during intra-uterine life.
2) Infantile glaucoma: (55%), manifested before 3 years age, patient born with
normal IOP.
3) Juvenile glaucoma: (5%), present after 3 years but before 16 years.
• Aetiology: Isolated trabeculodysgenesis without major ocular defect.
• Clinical Features:
1- Corneal haze (or opacity): first sign. 2- Photophobia, lacrimation and
blepharospasm.
3- Buphthalmus: a large eye. - Sclera also enlarges - Corneal enlargement.
- Ocular enlargement leads to axial myopia.
4- Breaks in descemet's membrane (due to stretching).
5- Optic disc cupping, C/D >0.3, it is not a reliable sign.
6- Visual field: cannot be done.
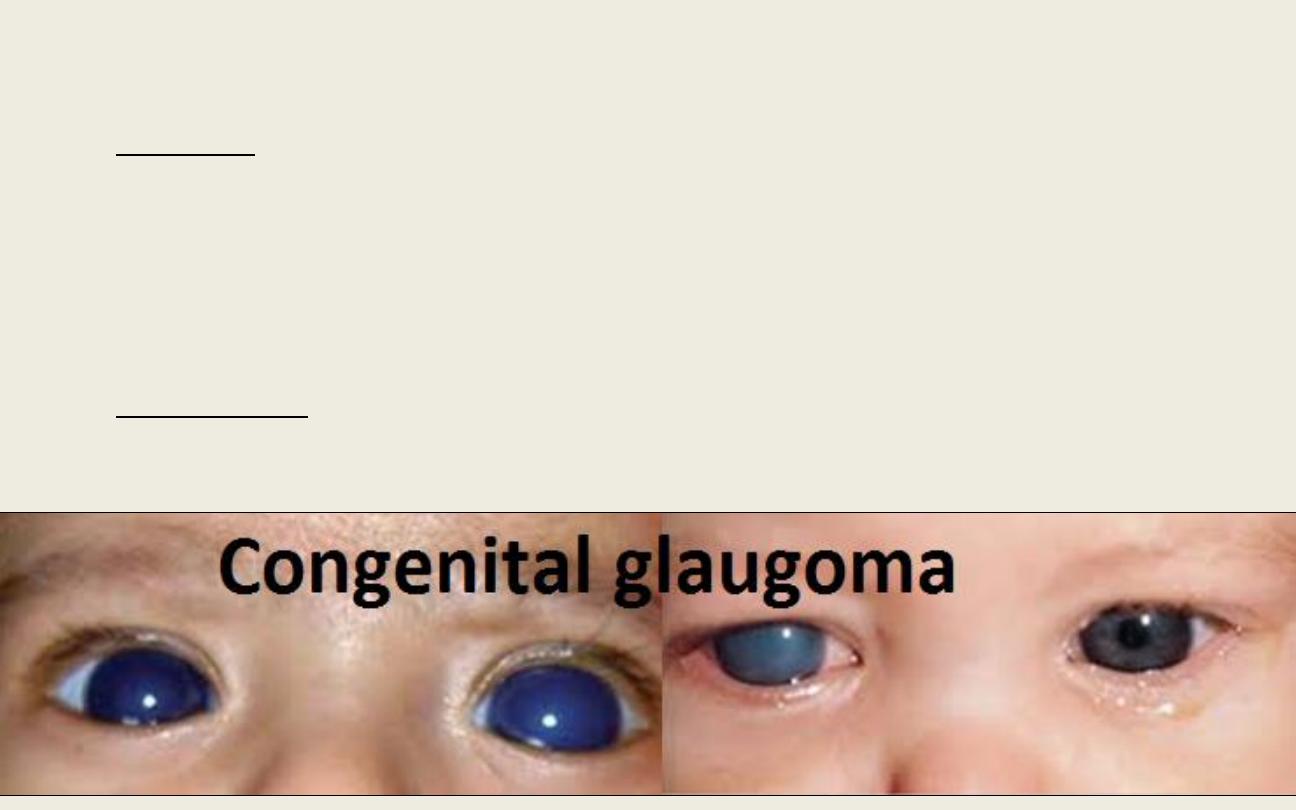
• The IOP should be check under general anesthesia by using Perkins hand-held
applanation tonometer or Schiøtz tonometer.
• Diagnosis:
1- Signs. 2- Checking IOP.
3- Corneal diameter: normally, corneal diameter at delivery is ≤ 10 mm, if corneal
diameter was > 12mm at age of 1 year, or 13mm at any age, then it is viewed with
suspicion. In children, corneal diameter is regarded as visual field assessment in
adults to follow patients with glaucoma.
• Management: is always surgical, and no role for medical treatment, and surgery
should be done as early as possible. (On day of delivery)
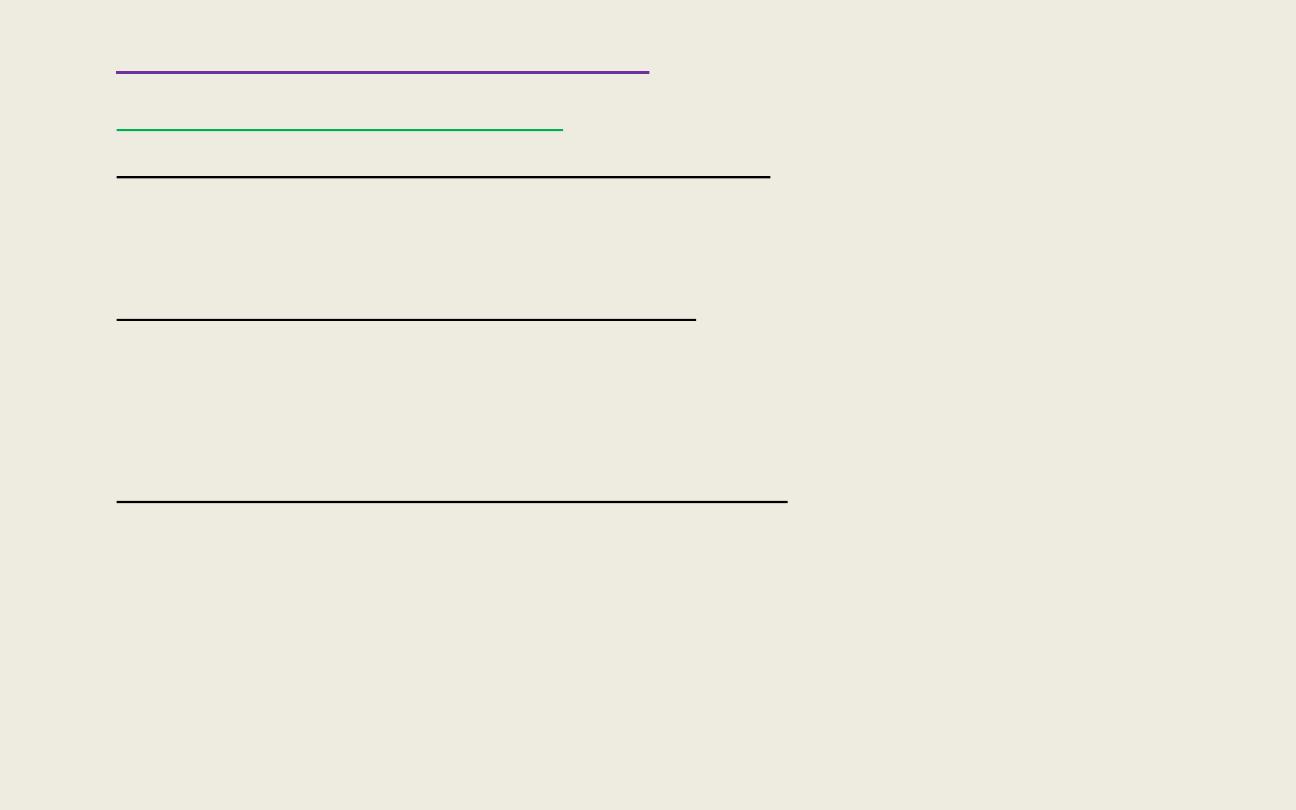
Secondary glaucoma:
Lens-related glaucoma:
a- Phacolytic glaucoma (lens protein glaucoma):
Is occur in association with hypermature cataract
Treatment: control IOP medically, then surgery (cataract extraction).
b- Phacomorphic (Intumescent) glaucoma:
Is acute secondary angle-closure glaucoma precipitated by an intumescent
cataractous lens.
Treatment: surgery (cataract extraction).
c- Phacoanaphylactic (phacoantigenic) glaucoma:
Is an autoimmune reaction to lens proteins occurring in an eye with a traumatic
ruptured anterior capsule.
Treatment: cataract extraction.
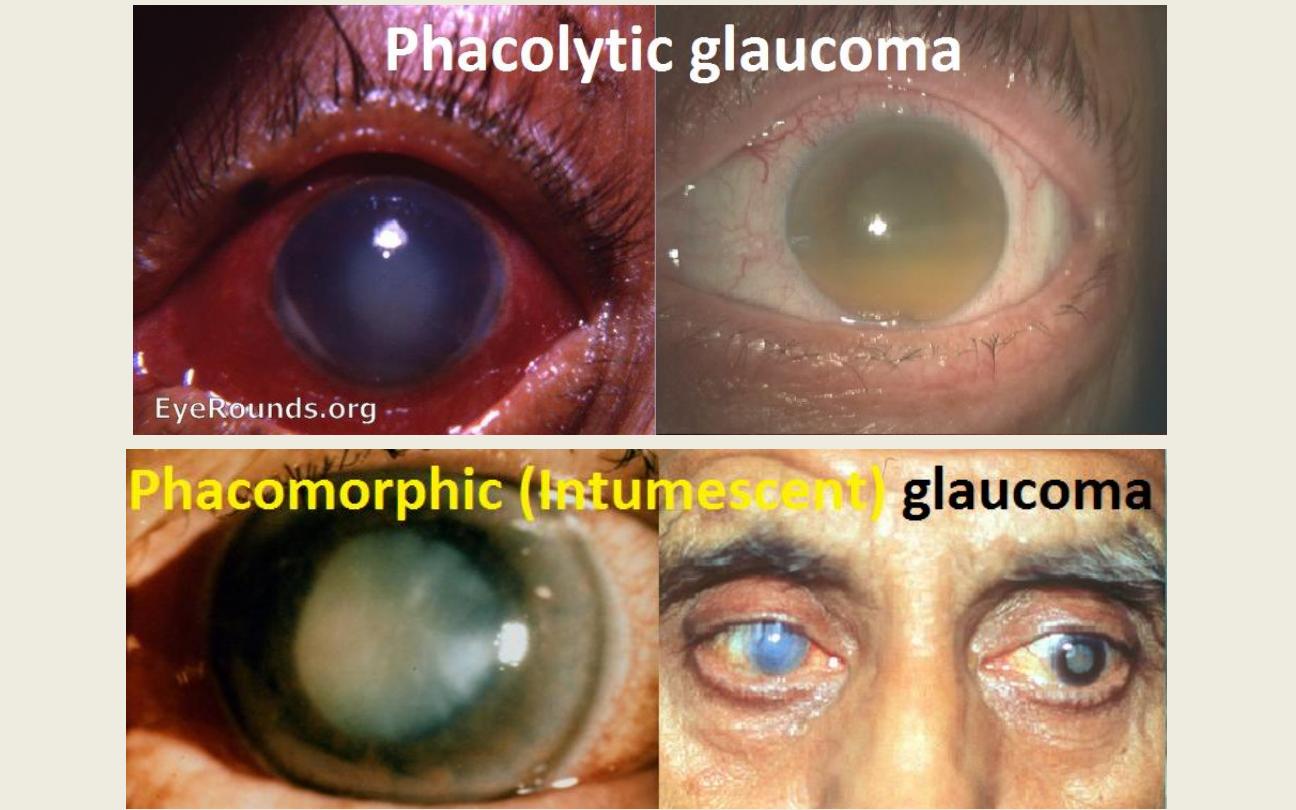
Neovascular glaucoma (NVG)
• Occurs as a result of iris neovascularization (Rubeosis iridis).
• The common aetiopathogenic factor is severe, diffuse & chronic retinal ischaemia.
• Causes of retinal ischaemia (causes of NVG):
a- Central retinal vein occlusion. (commonest cause)
b- Diabetes mellitus (proliferative diabetic retinopathy).
c- miscellaneous: - Carotid obstructive disease. - Central retinal artery occlusion.
- IO tumours - Long standing retinal detachment - Chronic IO inflammation.
• Treatment: Medical treatment is initially with topical β-blockers & acetazolamide.
Topical atropine &
steroids may decrease
inflammation and make
the eye more
comfortable and less
congested, even if IOP
remains high.
Surgical treatment
“Refractive error
(Ametropia)”
• Axial diameter: is the distance from tip of cornea to the center of macula, which is
normally 24mm.
• The most important two refractive surfaces are cornea and lens.
• The power of cornea and the lens depends on curvature of their surfaces,
so if we consider the cornea as a part of a sphere, it has a radius of curvature of
7.8 mm.
The radius of curvature of anterior capsule of lens is 10 mm.
The radius of curvature of posterior capsule of lens is 6 mm.
If the curvature of cornea or lens is increased, or in other word, the radius of
cornea or lens is decreased, then there is increase in refractive power of these
structures & vice versa.
For rays to come parallel, their source must be at distance of six meters and more
from the eye, and if the source of rays is at distance less than 6 meters, then the
rays will come divergent. The more close the source of rays to the eye, the more
divergent they are.
Emmetropia (normal refraction)
• It is an eye in which parallel rays (i.e. from infinity, 6 meters or more) of light come
to a focus directly on the retina when the eye is at rest {i.e. without
accommodation = the eye is using its normal power (60D) only}.
• Accommodation: contraction of Ciliary muscle in order to increase curvature of
lens (and so increase its refractive power more than 17D) to visualize objects
closer than 6 meters (near objects).
Ammetropia
A state of the eye when parallel light rayes cannot be focused on the retina .
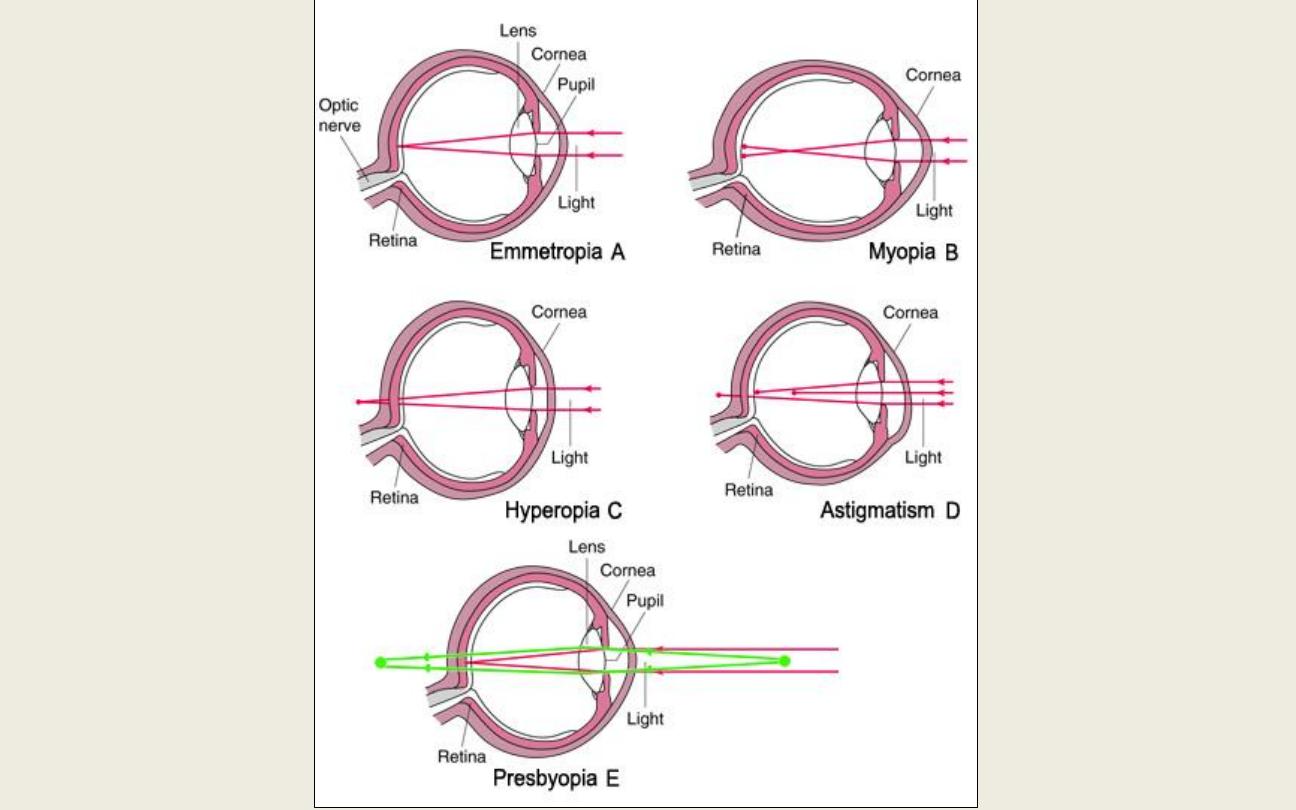
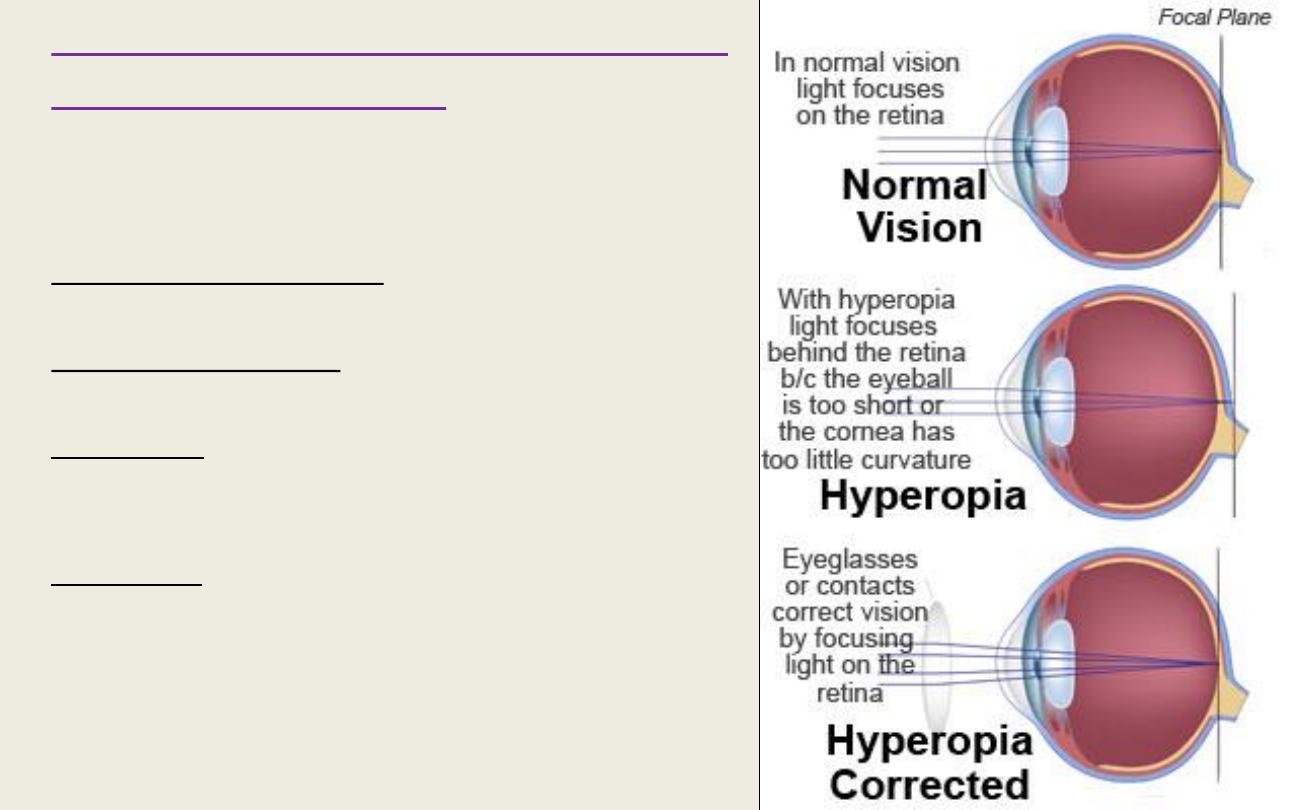
Hypermetropia (hyperopia),
far-sightedness:
• Is a type of refractive errors in which parallel rays of
light are brought to a focus some distance behind
the retina when the eye is at rest.
• Etiological classification: 1- Axial
2. Refractive: a- Curvature b- Index C-Aphakia
• Clinical classification: 1- Facultative 2- Absolute 3-
Manifest 4- Latent 5- Total
• Symptoms: 1- Blurred vision 2- Eye strain 3-
General symptoms like nausea and fatigue 4- can
present in child as squint.
• Treatment:
Convex lens in spectacles (+ve lenses to increase
refractive power).
Contact lenses.
LASER
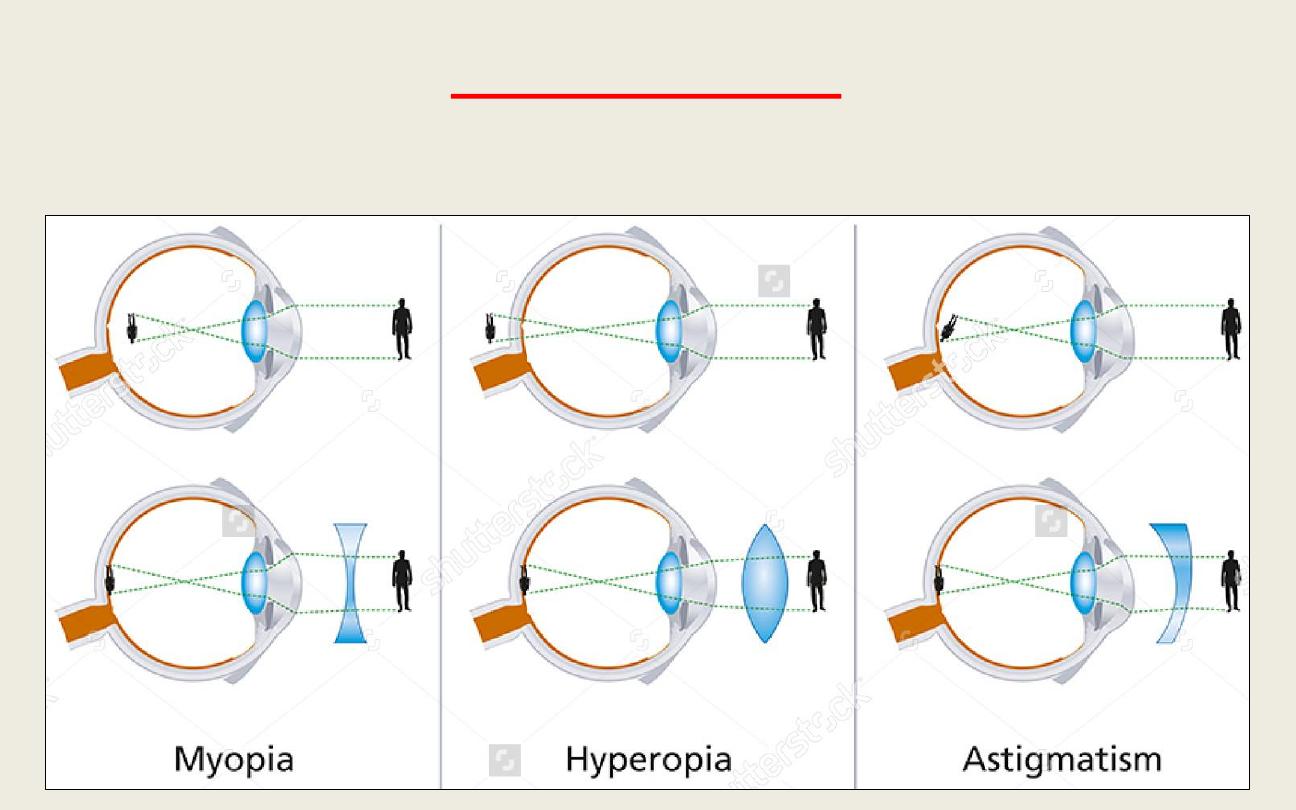
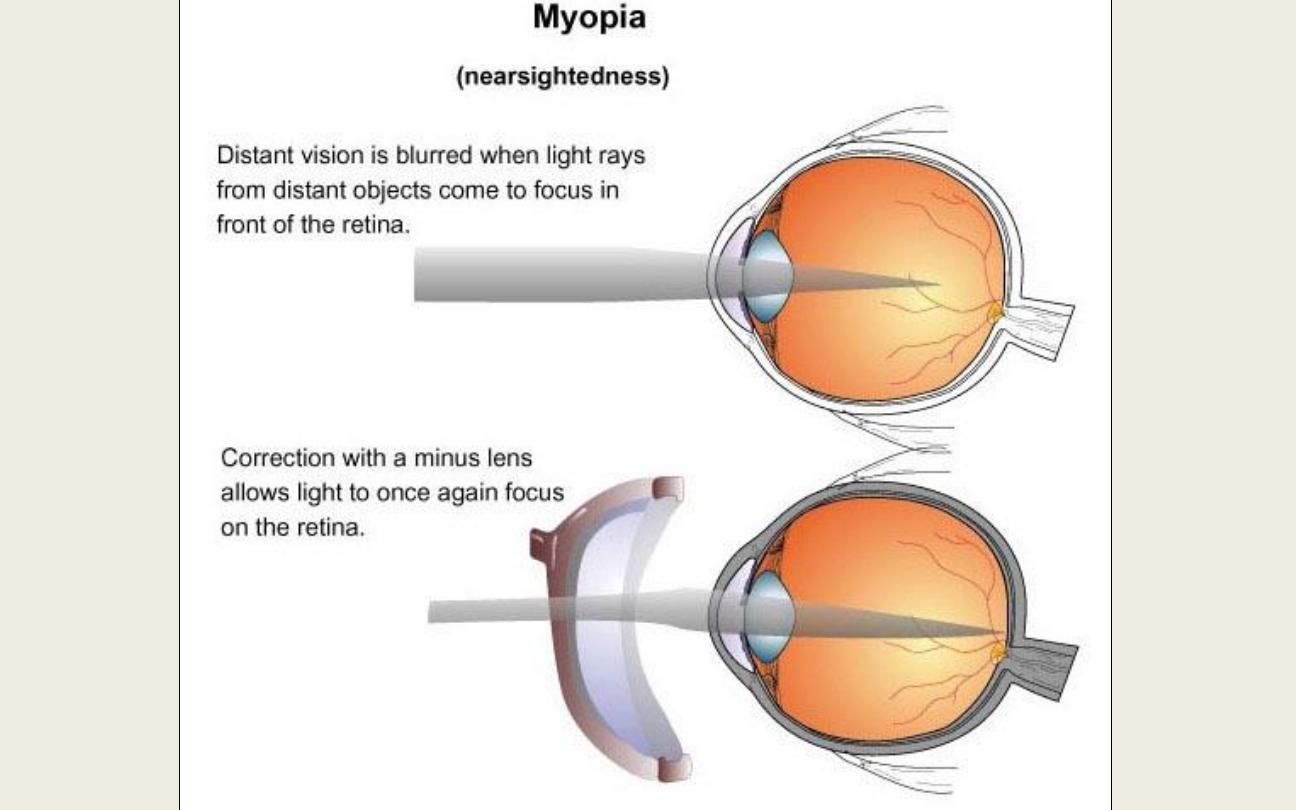
Myopia or short-sightedness:
• Parallel rays of light come to a focus in front of the retina when the eye is at rest.
• As there is increase in the refractive power of the eye, the near objects (closer
than 6m) will be seen normally, while far objects (whom rays come parallel) will be
focused in front of retina.
• Etiological classification: 1- Axial 2- Curvature 3- Index
• Clinical classification:
1- Simple (stationary): <6D
2- Pathological (progressive): >6D
• Symptoms:
1- Distance object "Blurred", near objects clear.
2- Headache, eye strain.
3- general symptoms like fatigue and nausea
• Treatment:
1- Concave lenses in spectacles. 2-Contact lens. 3- Surgical
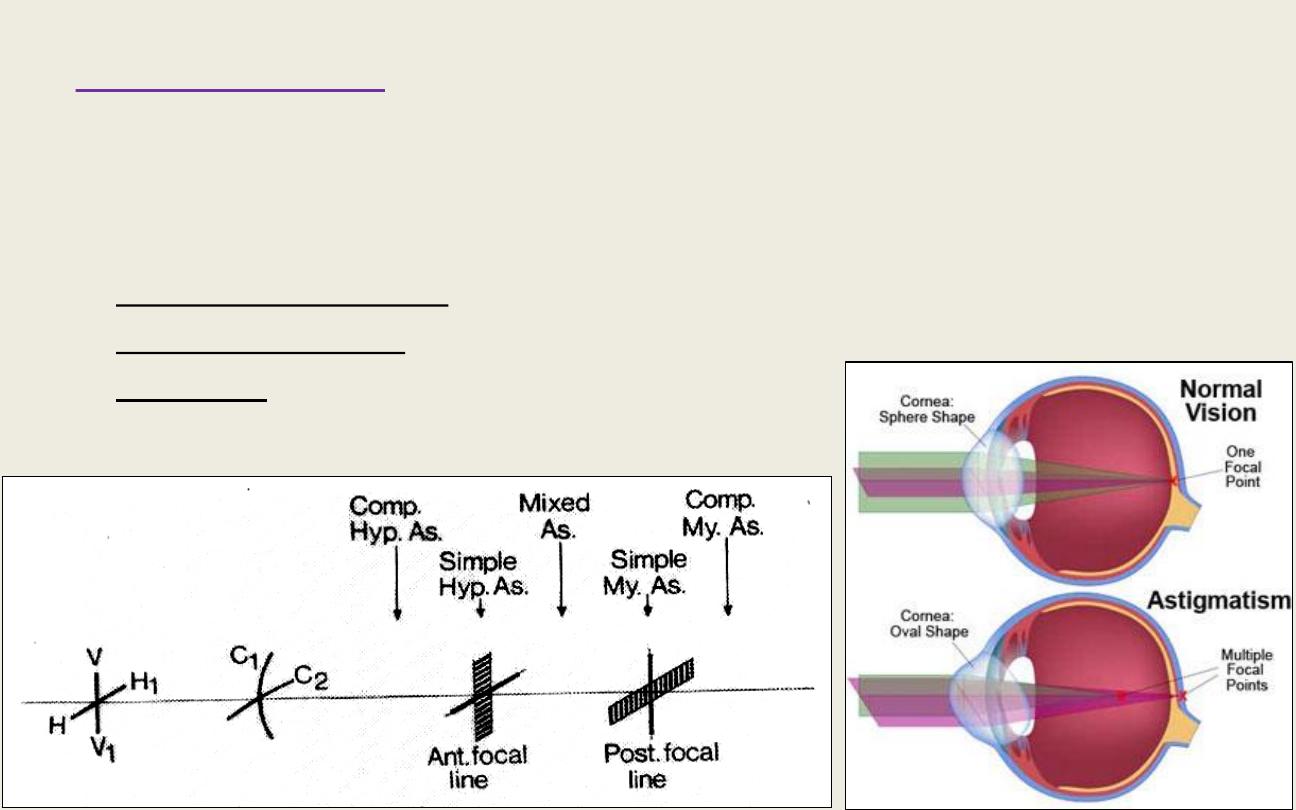
Astigmatism
• Astigmatism is that condition of refraction in which a point of focus of light cannot
be formed upon the retina. The optical condition is that instead of a single focal
point, there are two or more focal lines (depending on the type of astigmatism),
separated from each other by a focal interval.
• Etiological classification: 1- Curvature 2- Decentering 3- Index
• Clinical classification: 1- Regular: a- Simple b- Compound c- Mixed 2- Irregular
• Treatment: - Cylindrical lenses in spectacles
- Toric lens in spectacles - Contact lenses - Surgical
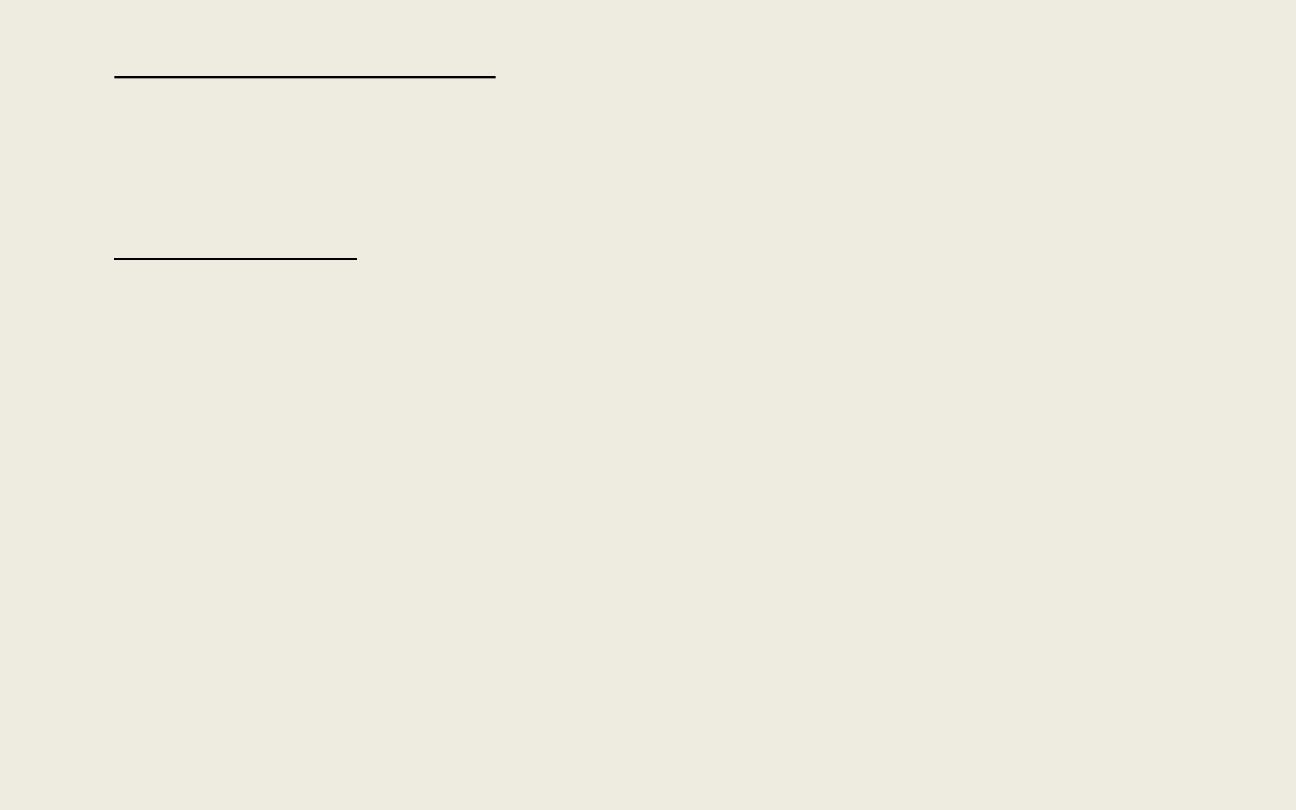
“The retina”
Anatomy
• The retina is divided into two major components:
1- Outer, pigmented monolayer known as Retinal Pigmented Epithelium (RPE).
2- Inner, multilayered (nine) lamina called the Neural Retinal (Sensory Retina).
• Blood supply:
The outer one third (1/3) of retina is supplied from choroidal blood vessels which
are formed by arborization of 10-20 ciliary arteries arising from ophthalmic artery
The inner 2/3 of retina is supplied by 2-3 levels of capillary network arising from
central retinal artery, which is a branch of ophthalmic artery.
The venous drainage of retina is through central retinal vein which also passing its
blood to the superior ophthalmic vein.
Both central retinal vein and artery are entering the eyeball with the optic nerve
through the scleral canal.
• Blood-Retinal Barrier (BRB): It is composed of two components:
1- Outer BRB: is formed by the tight junctions between RPE cells.
2-Inner BRB: is formed by the tight junctions between the endothelial cells of
retinal blood vessels.
• Applied anatomy:
The macula: it is a round area at the posterior pole, found temporal and inferior to
the optic disc. It contains xanthophylls (yellow) pigment (so it is called macula
lutea) and more than one layer of ganglion cells.
The fovea: it is a depression in the inner retinal surface at the center of the
macula (equal to optic disc diameter). By ophthalmoscope, it gives rise to oval
light reflex.
The foveola: it forms the central floor of the fovea. It is the thinnest part of retina.
In this area there is no ganglion cell layer and consists only of cones. It is
concerned with color and day vision. .
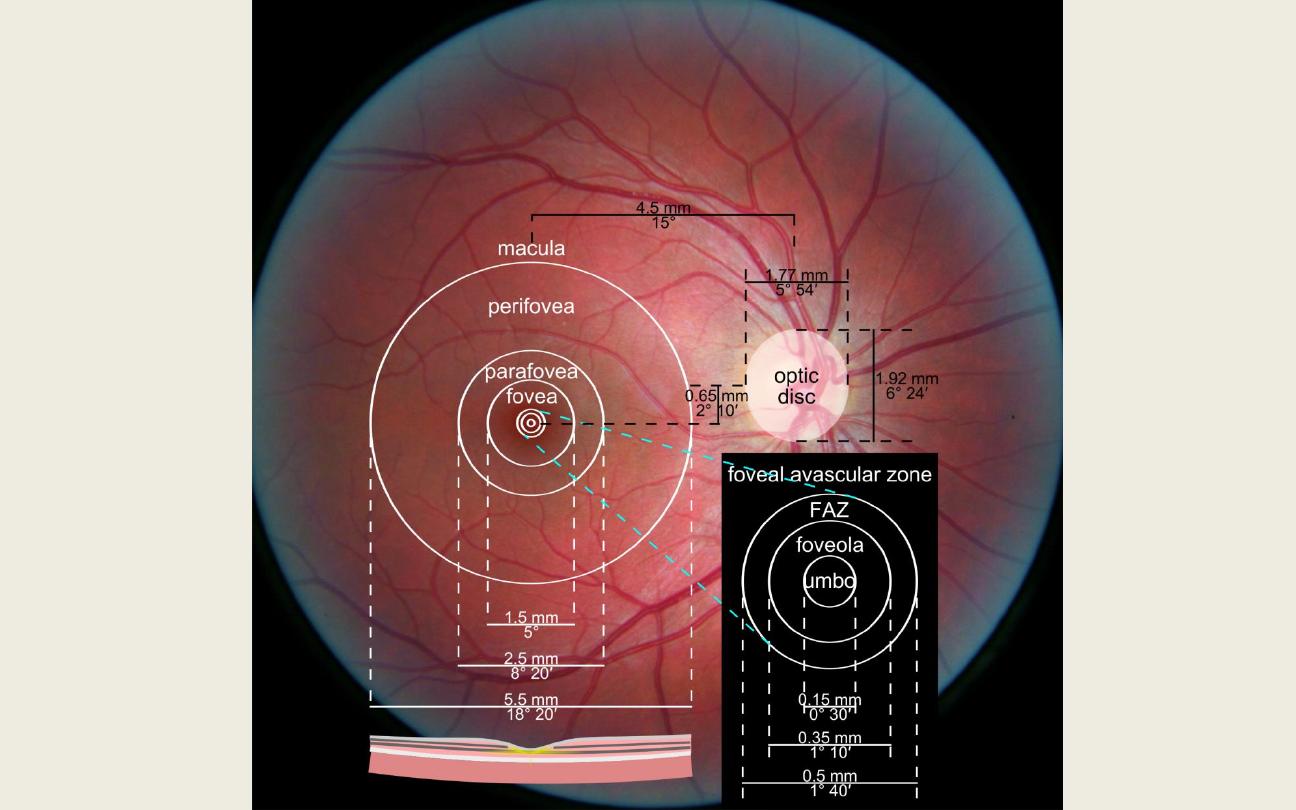
Retinal Detachment (RD)
• It is separation of the sensory retina from the RPE by subretinal fluid (SRF)
accumulated in SRS. Types of retinal detachment:
Rhegmatogenous RD: (Rhegma = break)
• occurs secondary to a full thickness defect (either a hole or tear) in the sensory
retina. Causes:
a- Idiopathic. b- Myopia c- Trauma. d- Intraocular surgery, e.g. cataract surgery.
e- Hereditary diseases of vitreous and retina, e.g. Stickler's syndrome.
f- In association with tractional RD.
• Symptoms:
a) Photopsia (flashes of light).
b) Floaters: are moving vitreous opacities perceived when they cast a shadow upon
the retina. Weiss ring which is pathognomonic for PVD.
(a) & (b) reported in 60% of patients with spontaneous rhegmatogenous RD, then
after a variable period the patient notice:
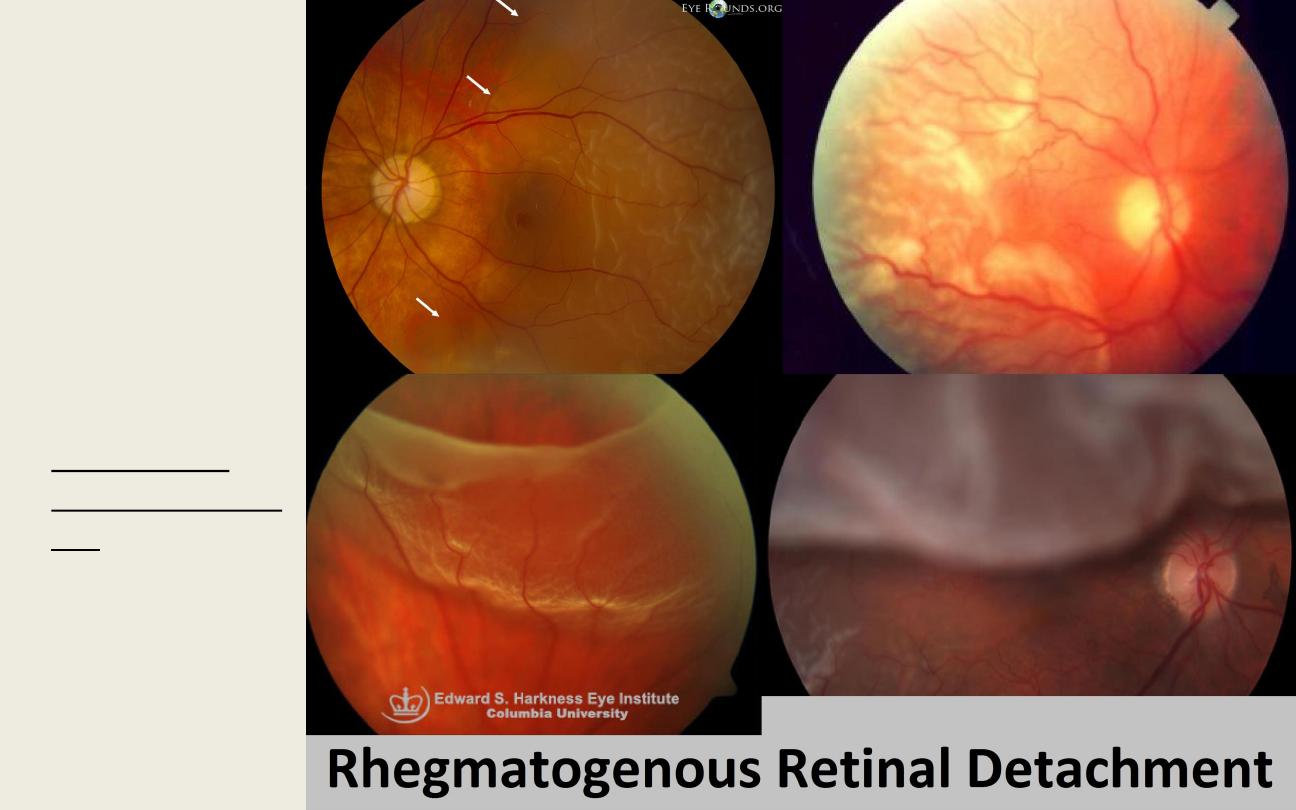
c) Peripheral visual
field defect
which progress
to:
d) Decreased
central visual
acuity (drop
vision): when
macula is
involved.
• Treatment of
rhegmatogenous
RD: is surgical
Non-rhegmatogenous RD:
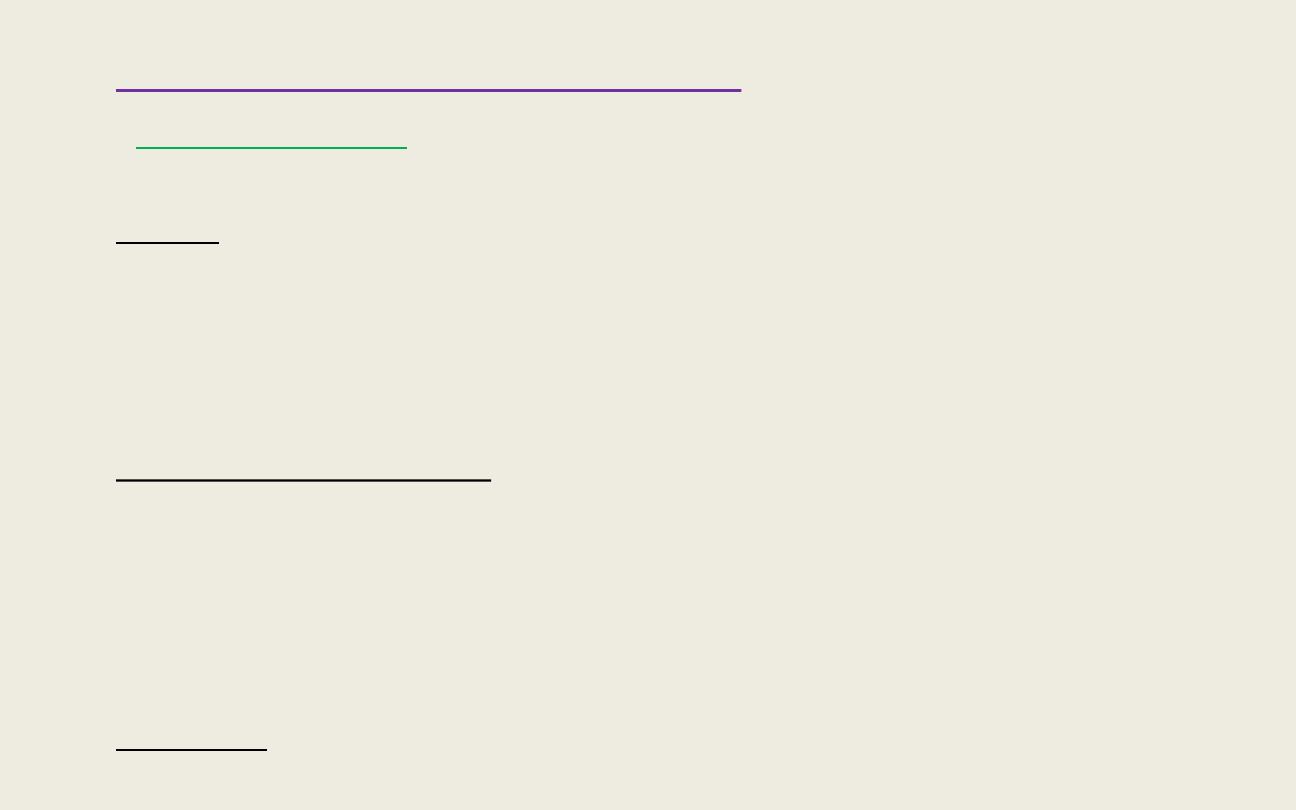
1) Tractional RD:
• In which, the sensory retina is pulled away from the RPE.
• Causes:
i- Advanced diabetic eye disease.
ii- Retinopathy of prematurity "ROP" (retrolental fibropathy or fibroplasia).
iii- Sickle cell retinopathy.
iv- Penetrating trauma.
• Symptoms of tractional RD:
Photopsia and floaters are usually absent.
i- Visual field defect: it is the main complaint, which progress slowly and may
become stationary for months or years.
ii- Decreased central visual acuity: if tractional detachment progress to involve
the macula.
• Treatment: surgery.
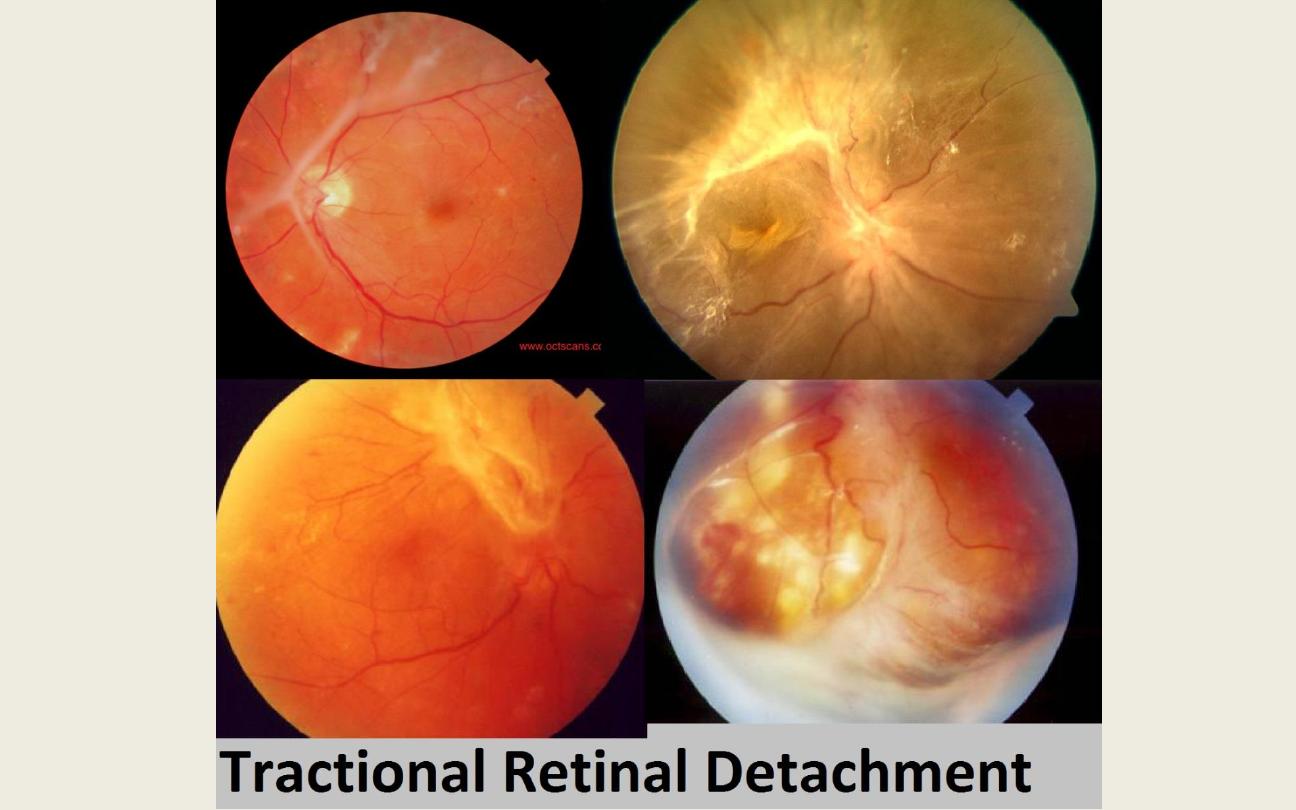
2) Exudative (serous) RD:
• Due to damaged RPE.
• Causes
Ocular causes: i- Choroidal tumours. ii- Retinoblastoma. iii- Uveitis (posterior
uveitis). iv- Posterior scleritis.
Systemic causes: i- Malignant hypertension. ii- Eclampsia. iii- Uremic patient.
• Symptoms:
Photopsiae is absent (no vitreoretinal traction).
Floaters may be present if it is associated with uveitis (vitritis).
Visual field defect develops suddenly & progress rapidly.
Bilateral eye involvement is possible.
• Treatment: towards the cause.
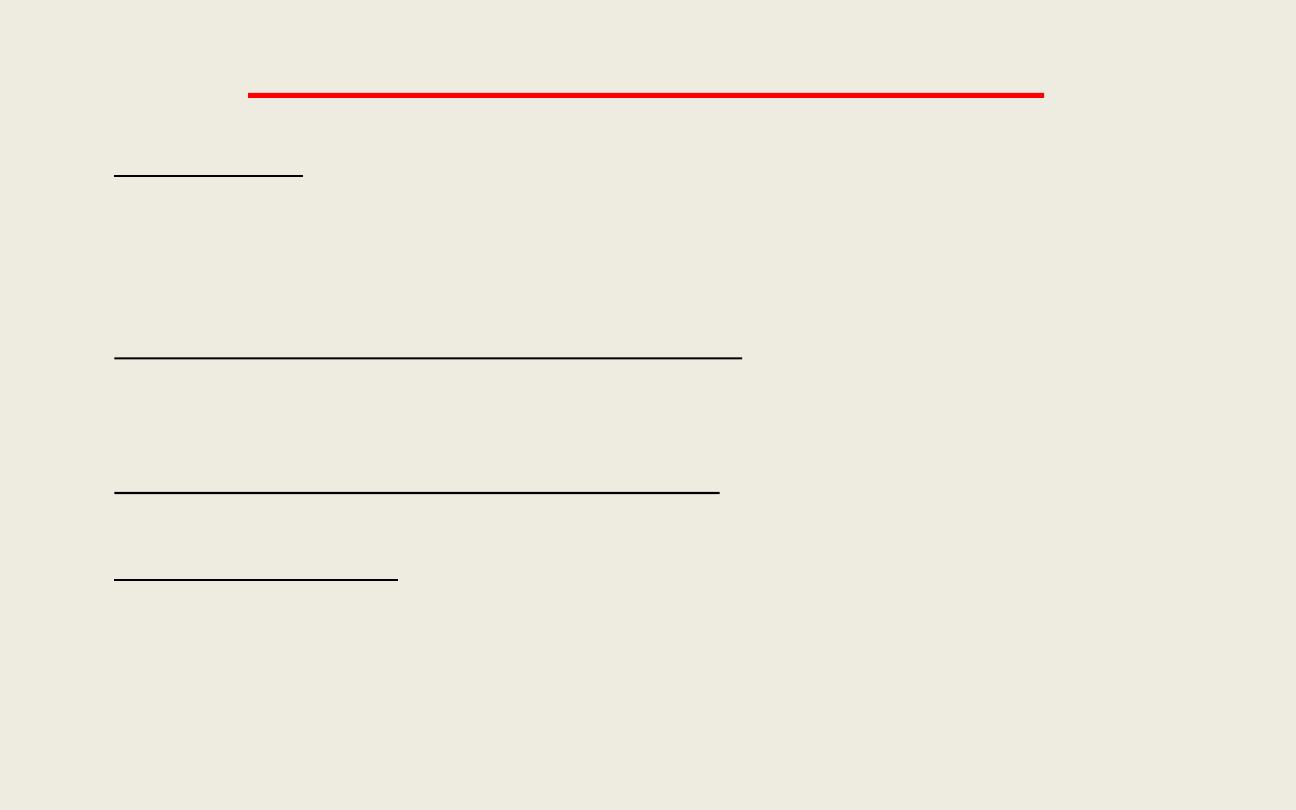
Diabetic Retinopathy (DR)
• Pathogenesis:
DR is a microangiopathy primarily affecting the arterioles, capillaries & post-
capillary venules, although large vessels may also be involved.
The main pathology in DR is: either microvascular occlusion. Or leakage.
• The consequences of microvascular occlusion:
retinal ischemia and hypoxia → "Neovascularization", formed at optic disc "NVD",
or elsewhere in the retina "NVE", and occasionally on the iris "Rubeosis Iridis".
• The consequences of Microvascular leakage and increased vascular permeability
include intraretinal haemorrahges and oedema.
• Clinically DR may be:
1- Background DR. 2- Pre-proliferative 3- Proliferative DR.
4- maculopathy, which associates (1), (2) or (3).
5- Advanced diabetic eye disease (ADED).
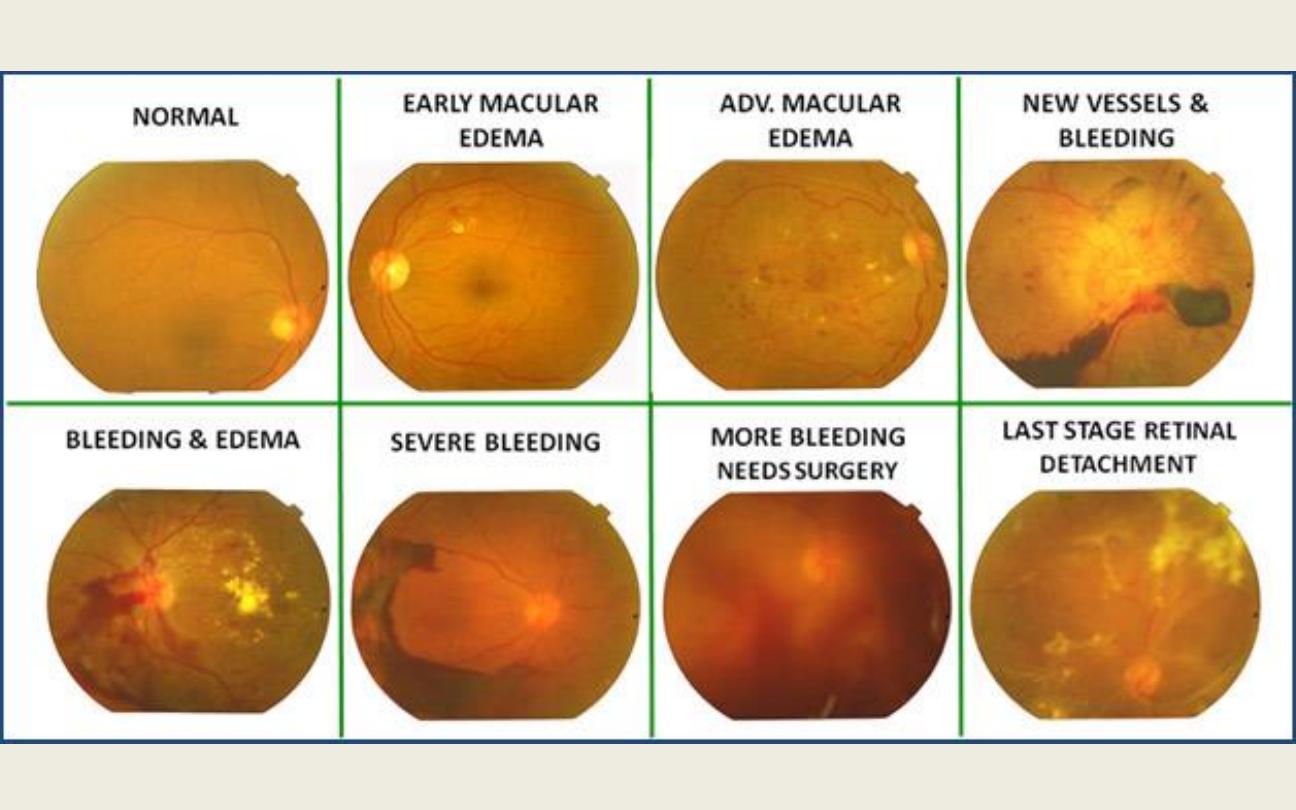
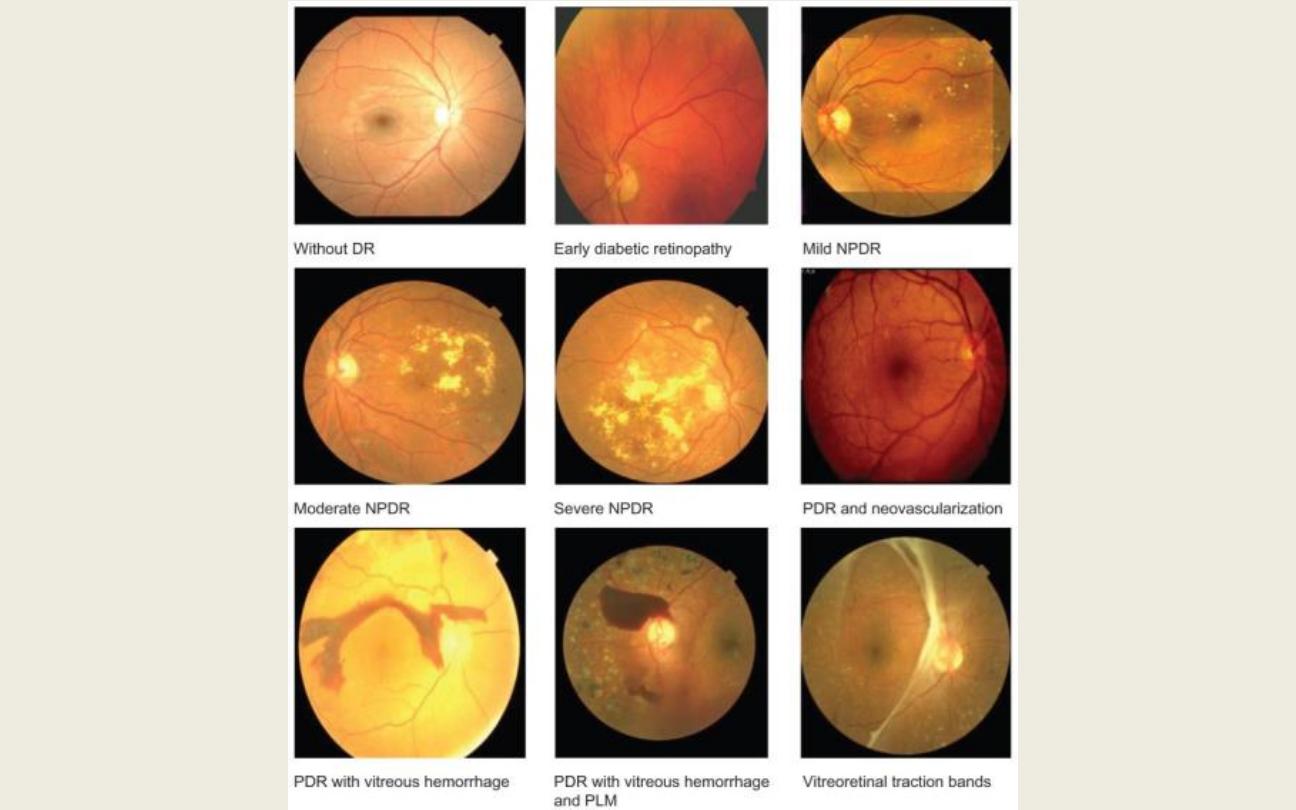
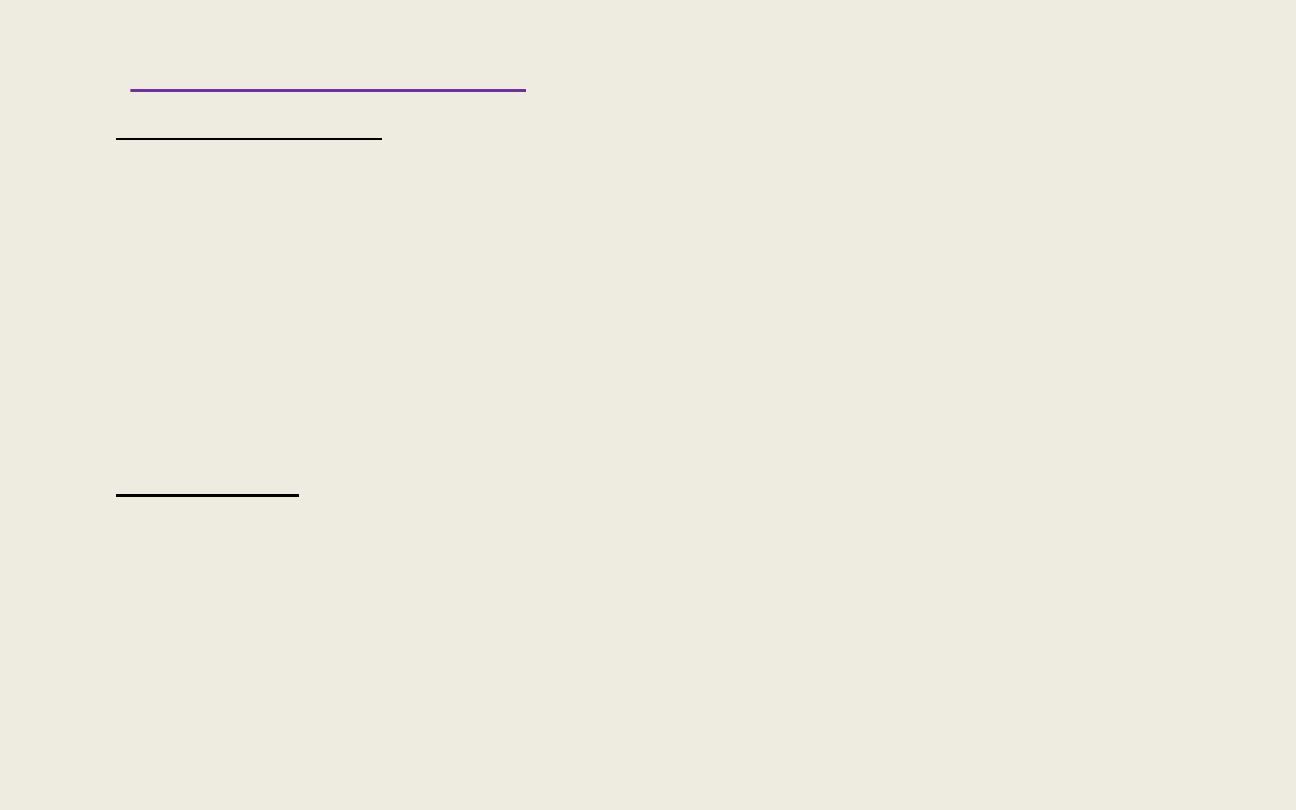
Background DR:
• Fundoscopy shows:
a- Microaneurysms (saccular dilatations).
b- Exudation (leakage of lipoprotein).
c- Retinal oedema.
d- Intaretinal Haemorrhages: Dot-blot haemorrhage or flame-shaped
haemorrhage at level of nerve fiber layer. Sometimes it is difficult to differentiate
intraretinal haemorrhages from microaneurysm, however, we can differentiate by
fluorescein angiography, as aneurysms will leak dye.
• Management: It requires NO treatment, but should be reviewed every 6 months.
In addition, patients need to control of diabetes and associating factors as
hypertension, anemia and renal failure.
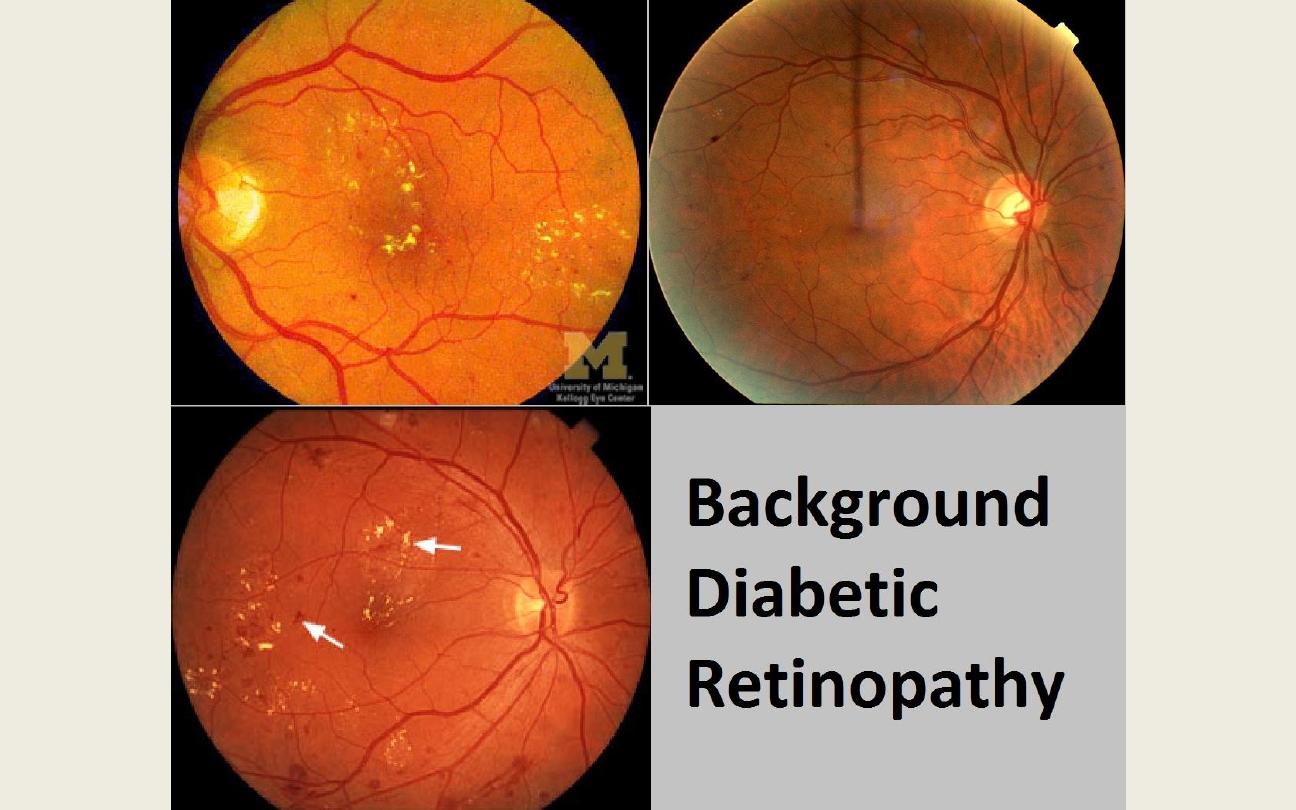
Pre-proliferative DR:
• Fundoscopy shows, in addition to all features of background DR, the following:
a- Cotton wool spots which represent focal infarction of retinal nerve fiber layer
due to occlusion of pre-capillary arterioles.
b- Intra Retinal Microvascular Abnormalities (IRMA), which represent shunts that
run from retinal arterioles to venules, bypassing the capillary bed.
• Management:
Should be watched closely every 3 months because of the risk of PDR
(Proliferative Diabetic Retinopathy) is high. Laser photocoagulation is usually not
needed unless:
a- Regular follow-up is not possible.
b- Vision in the fellow eye has been already lost due to PDR.
Also we need to control diabetes and associating factors.
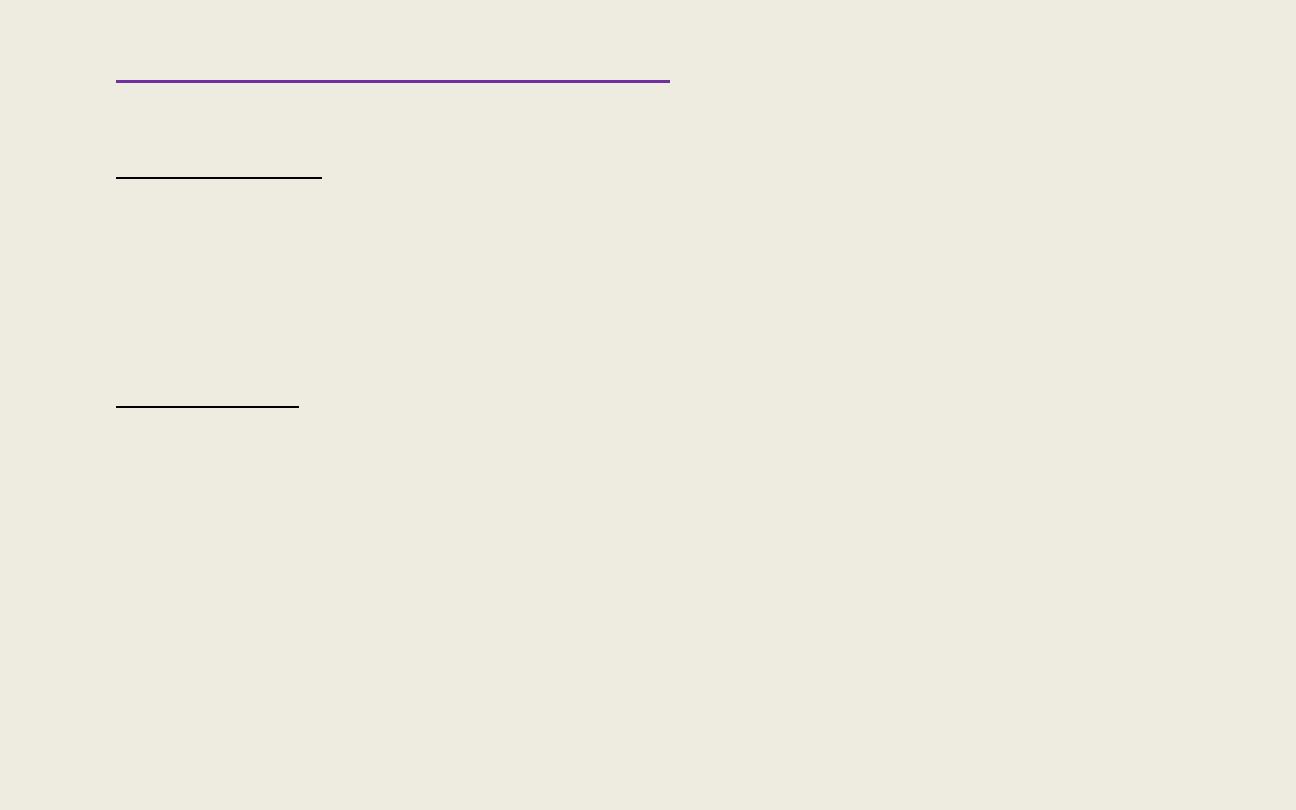
Proliferative DR (PDR):
• Type 1 diabetics are at particular risk.
• By fundoscopy,
Neovascularization is the hallmark of PDR, either at disc (NVD) or elsewhere (NVE)
Sometimes we can see pre-retinal haemorrhage or intravitreal haemorrhage & the
patient complains of sudden drop of vision.
Finally, tractional RD that may end with ADED.
• Management:
Pan-Retinal Photocoagulation (PRP), we destroy all normal retinal tissue around
the temporal arcades (temporal blood vessels) in order to decrease retinal
ischaemia by decreasing O
2
demand. Then the neovascularization resolves
spontaneously (no hypoxia → no growth factors).
If pre-retinal or intravitreal hemorrhage occur, it is impossible to do PRP until this
blood resolve spontaneously or remove by vitrectomy.
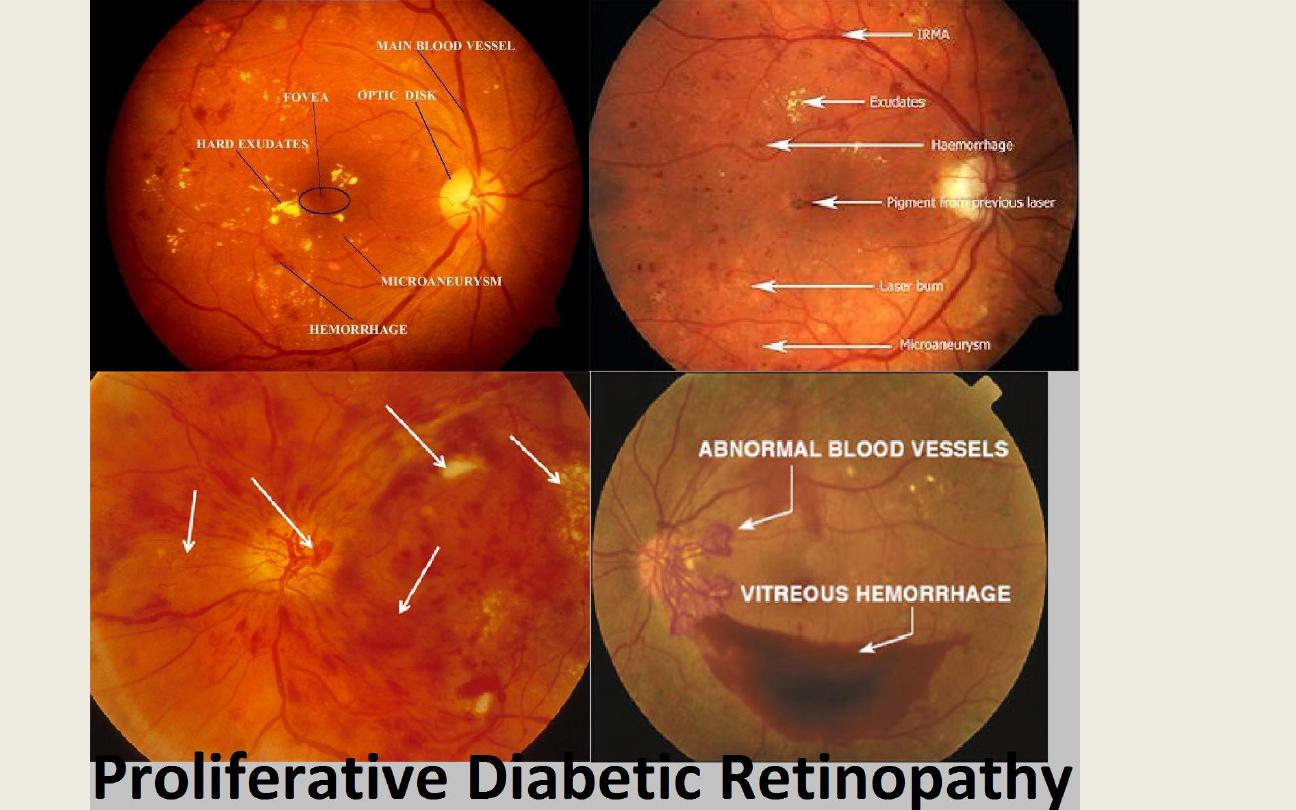
Maculopathy (macular DR)
• Is might be associated with: a- Background DR. b- Pre-proliferative DR.
c- Proliferative DR.
• It is the involvement of the fovea by oedema and exudates (leakage) or ischaemia
(occlusion).
• Diabetic maculopathy is the most common cause of visual impairment in diabetic
patients particularly those with type 2 diabetes.
• Management:
We should do fluorescein angiography to differentiate between leakage type
(edematous or exudative maculopathy) and ischaemic type (ischaemic
maculopathy) and to find the site of leakage in first type.
For exudative and edematous maculopathy, focal laser photocoagulation to
occlude the site of leakage.
For ischaemic maculopathy, no treatment available.
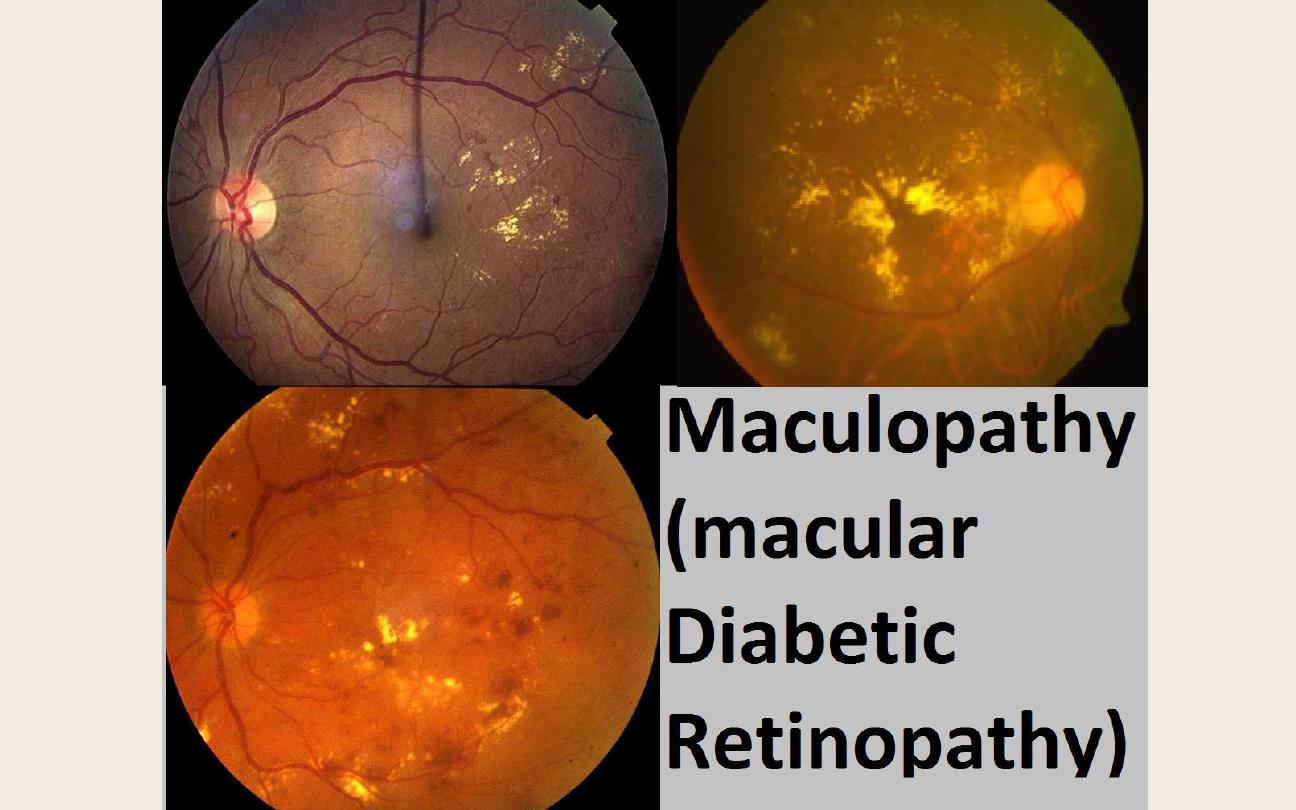
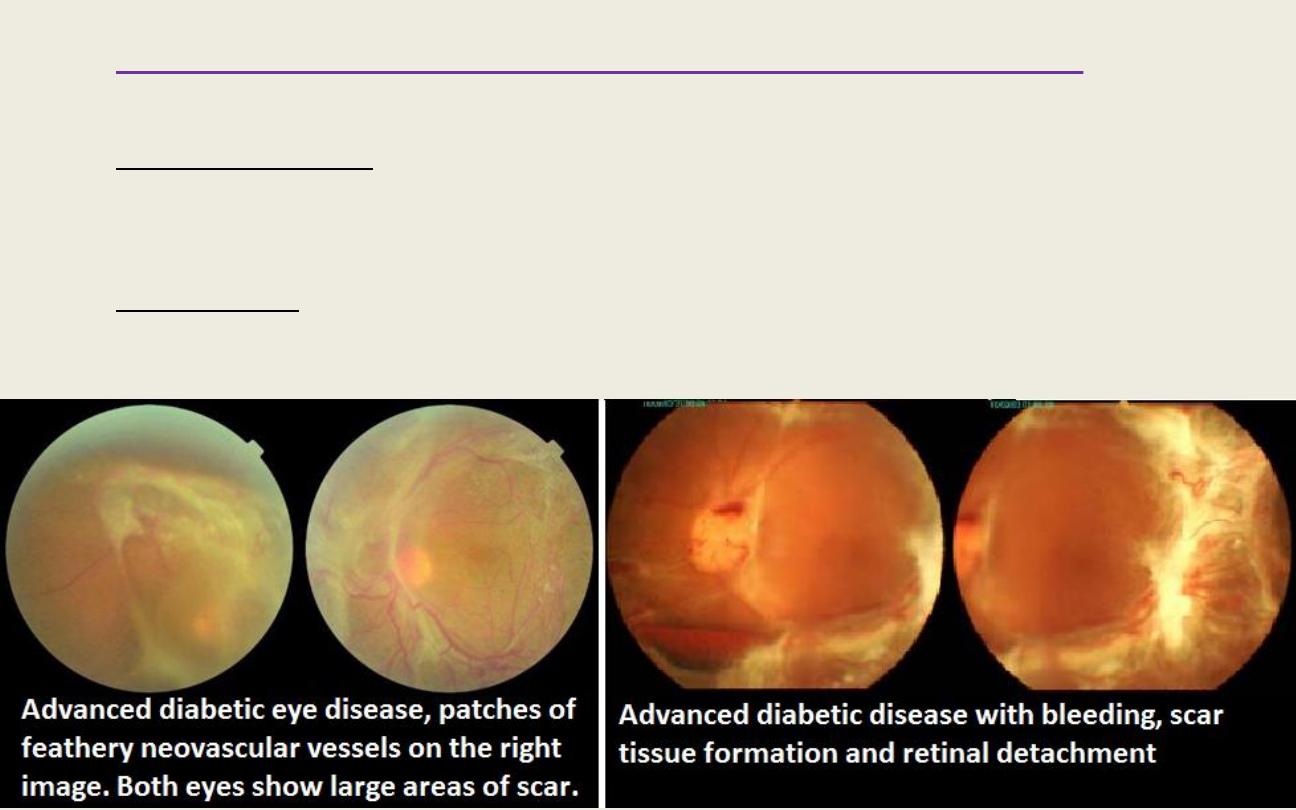
Advanced diabetic eye disease (ADED):
• Serious vision-threatening complication of diabetic retinopathy.
• Fundoscopy shows:
a- Hemorrhage. (pre-retinal or intravitreal).
b- Tractional RD.
• Management: Vitrectomy + Retinal reattachment surgery + Endolaser (PRP).
“Neuro-
ophthalmology”
Optic nerve
• Optic nerve can be subdivided into four segments:
1- Intra-ocular segment (optic disc, nerve head).
2- Intra-orbital segment: 3.0 cm, this part has S shape allowing the eye for
movement without nerve stretching
3- Intra-canalicular segment: 1cm.
4- Intra-cranial segment: 6-8 mm, joins the chiasm.
• The optic nerve is surrounded by pia, arachnoid and duramater, so the CSF
reaches up to the posterior sclera around the optic nerve.
• Axoplasmic transport:
Retinal cotton-wool spots are the result of accumulation of cytoplasmic
organelles due to interruption of axoplasmic flow between the retinal ganglion
cells & their terminal synapses.
Papilloedema is similarly caused by hold-up of axoplasmic flow at the lamina
cribrosa
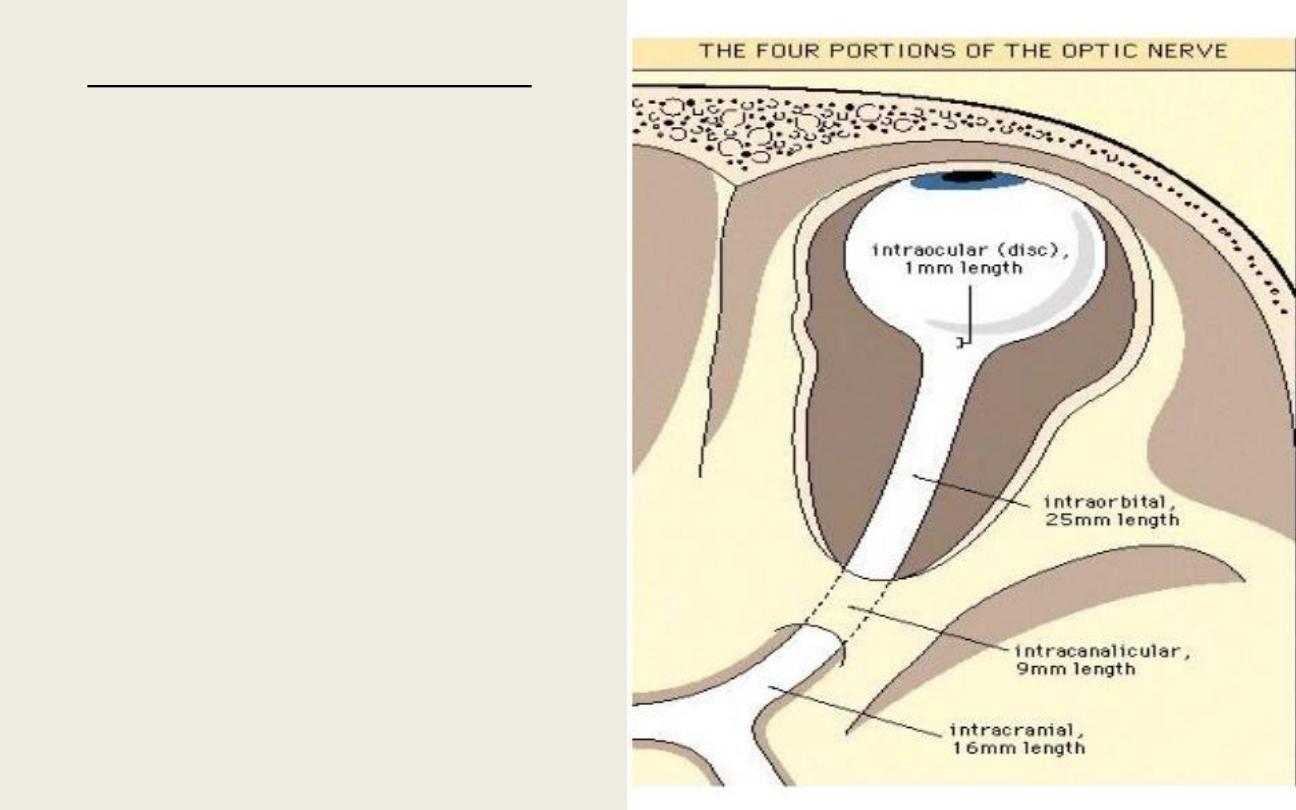
• Signs of optic nerve dysfunction:
1- Decreased visual acuity.
2- Diminish light pupillary reflex.
3- Dyschromatopsia (impairment of
color vision): affected eye sees the
colors less bright.
4- Diminished light brightness
sensitivity.
5- Visual field defect: depends on the
type of the pathology, e.g. central
scotomas, centrocaecal scotomas and
altitudinal.
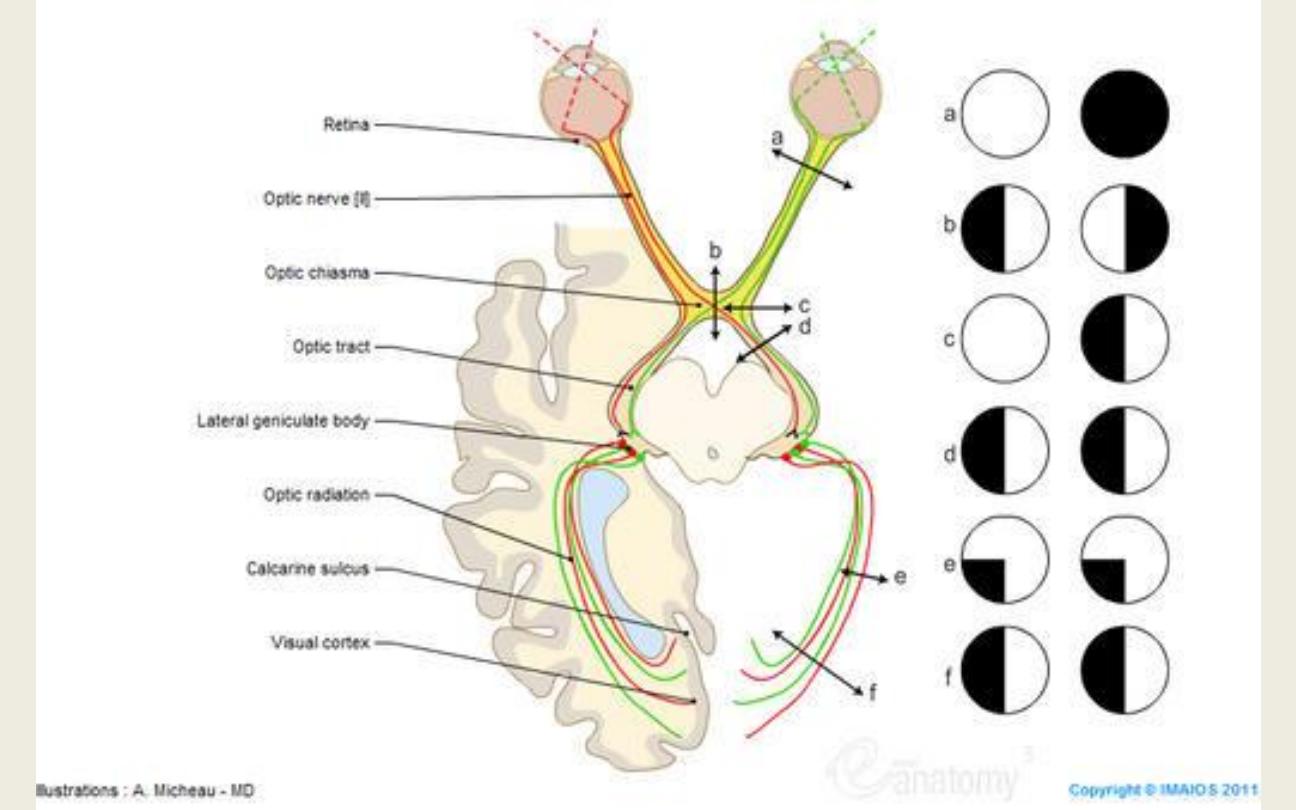
Optic neuritis
• Inflammatory or demyelinating process affecting the optic nerve.
• Ophthalmoscopic classification:
Retrobulbar neuritis: optic disc appearance is normal, at least initially (as in
longstanding cases may end with optic disc atrophy), because the optic nerve
head is not involved.
Papillitis: affects the optic nerve head. It is characterized by variable hyperaemia
and oedema of the optic disc, which may be associated with parapapillary flame-
shaped haemorrhages.
• Etiological classification:
Demyelinating.
Para-infectious: it is follow a viral infection or immunization.
Infectious.
Associated with Autoimmune disease.
• Treatment is according to the etiology.
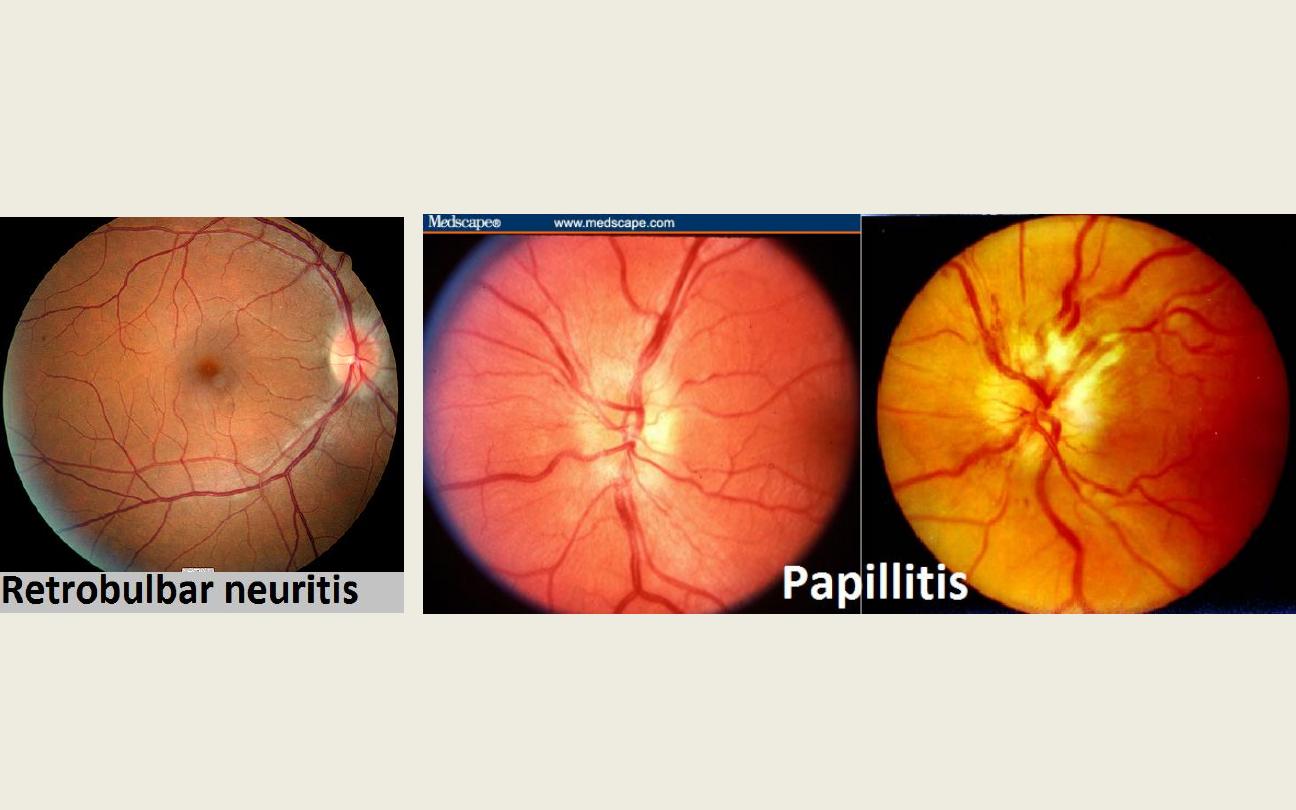
Optic atrophy
• It is an important sign of advanced optic nerve disease. It is of two types:
Primary optic atrophy:
• It is occurs without antecedent swelling of the optic nerve head. It may be caused
by lesions affecting the visual pathways. Lesions anterior to the optic chiasm result
in unilateral optic disc atrophy, whereas those involving the chiasm and optic tract
will cause bilateral optic disc atrophy.
• Causes:
- Retrobulbar neuritis. - Compressive lesions, such as tumors and aneurysms.
- Hereditary optic neuropathies. - Toxic and nutritional optic neuropathies.
• Signs: - Pale, flat disc with clearly delineated margin.
- Reduction in number of small blood vessels on the disc surface.
Secondary optic atrophy:
• It is preceded by swelling of the optic nerve head.
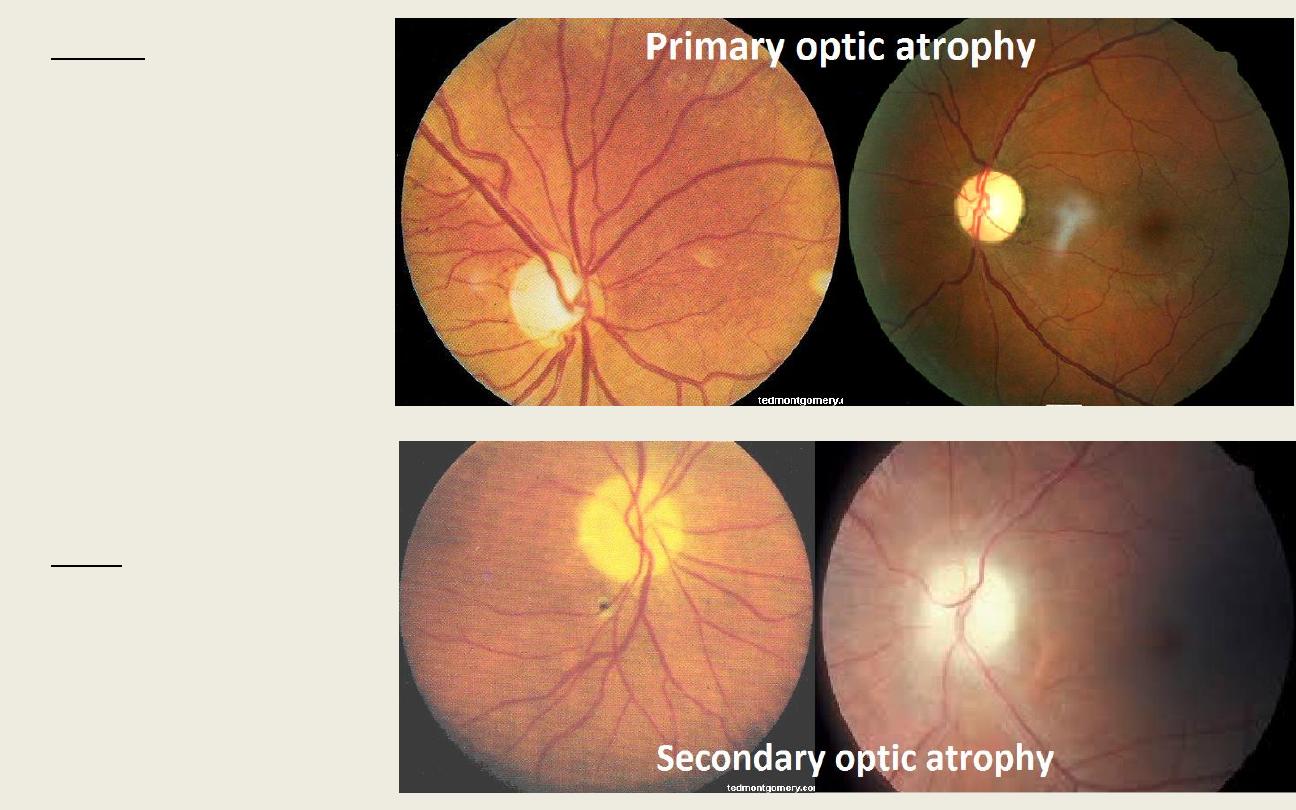
• Causes:
Papillitis.
Chronic papilloedema.
AION (Anterior
Ischaemic Optic
Neuropathy): usually
occurs in old age
patients, it is of two
types; non arteritic [in
diabetes, hypertension]
& arteritic .e.g. Giant
cell arteritis.
• Signs: - White or dirty
grey, slightly raised disc
with poorly delineated
margins due to gliosis.
- Reduction in number of
small blood vessels on
the disc surface.
Papilloedema
• It is swelling of the optic nerve head secondary to raised intracranial pressure.
• All other causes of disc oedema in the absence of raised ICP are referred to as
"disc swelling" & usually produce visual impairment.
• All patients with papilloedema should be suspected of having an IC mass until
proved otherwise.
• Early features of papilloedema:
- Visual symptoms are absent and visual acuity is normal.
- Optic disc shows hyperaemia and mild elevation.
• Established papilloedema: - Transient visual obscurations lasting a few seconds.
- Visual acuity is normal or reduced.
- Optic disc shows severe hyperaemia, moderate elevation and indistinct margin.
• Atrophic papilloedema:
- Visual acuity is severely impaired.
- Optic discs are dirty grey color, slightly elevated and indistinct margin.
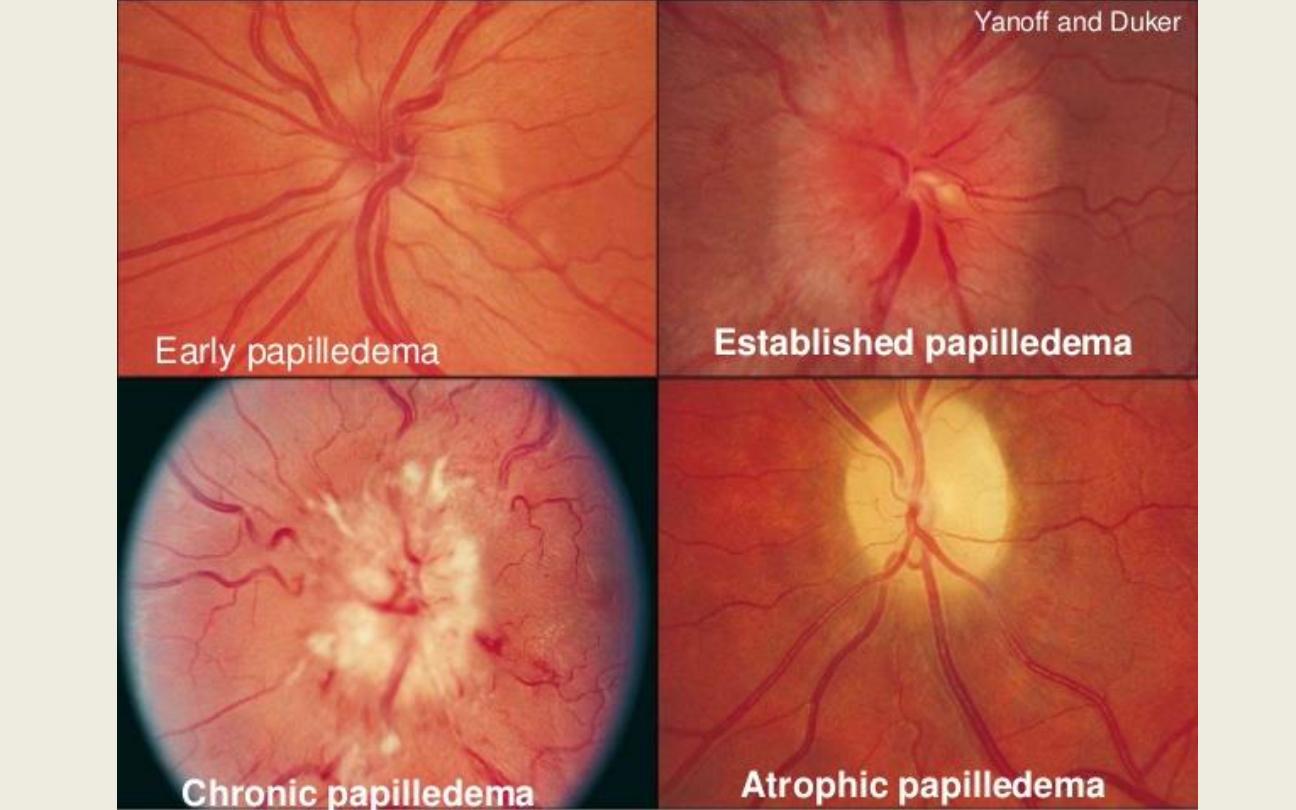
Abnormal pupillary reaction
Afferent pupillary conduction defects
• A total afferent defect (TAPD, amaurotic pupil)
is caused by a complete optic nerve lesion and is characterized by the following:
The involved eye is completely blind (i.e. no light perception).
Both pupils are equal. When the affected eye is stimulated neither pupil reacts but
when the normal eve is stimulated both pupils react normally.
The near reflex is normal in both eyes.
• A relative afferent defect (RAPD, Marcus Gunn pupil)
is caused by an incomplete optic nerve lesion or severe retinal disease, but not by
a dense cataract. The clinical features are those of an amaurotic pupil but more
subtle.
The difference between the pupillary reactions is enhanced by the 'swinging-
flashlight test' in which each pupil is stimulated in rapid succession. When the
abnormal pupil is stimulated it dilates instead of constricting.
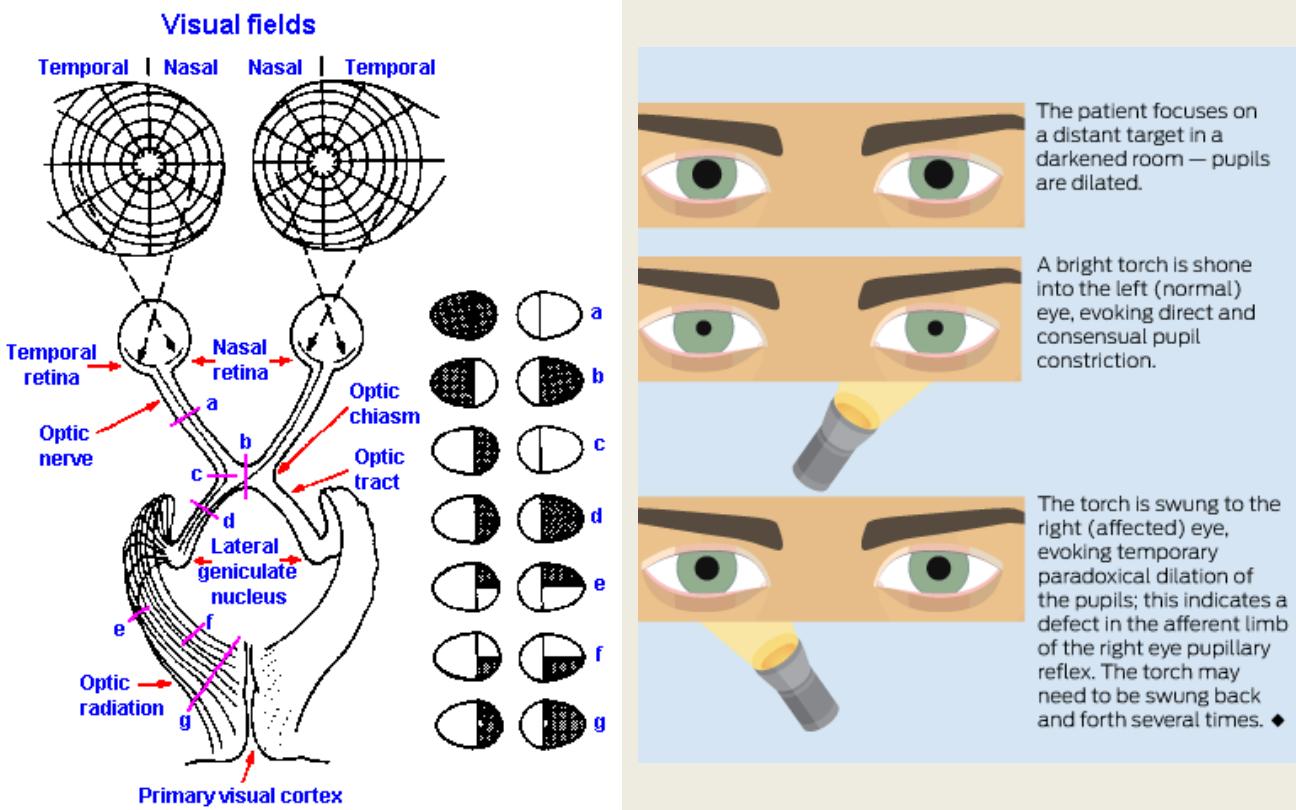
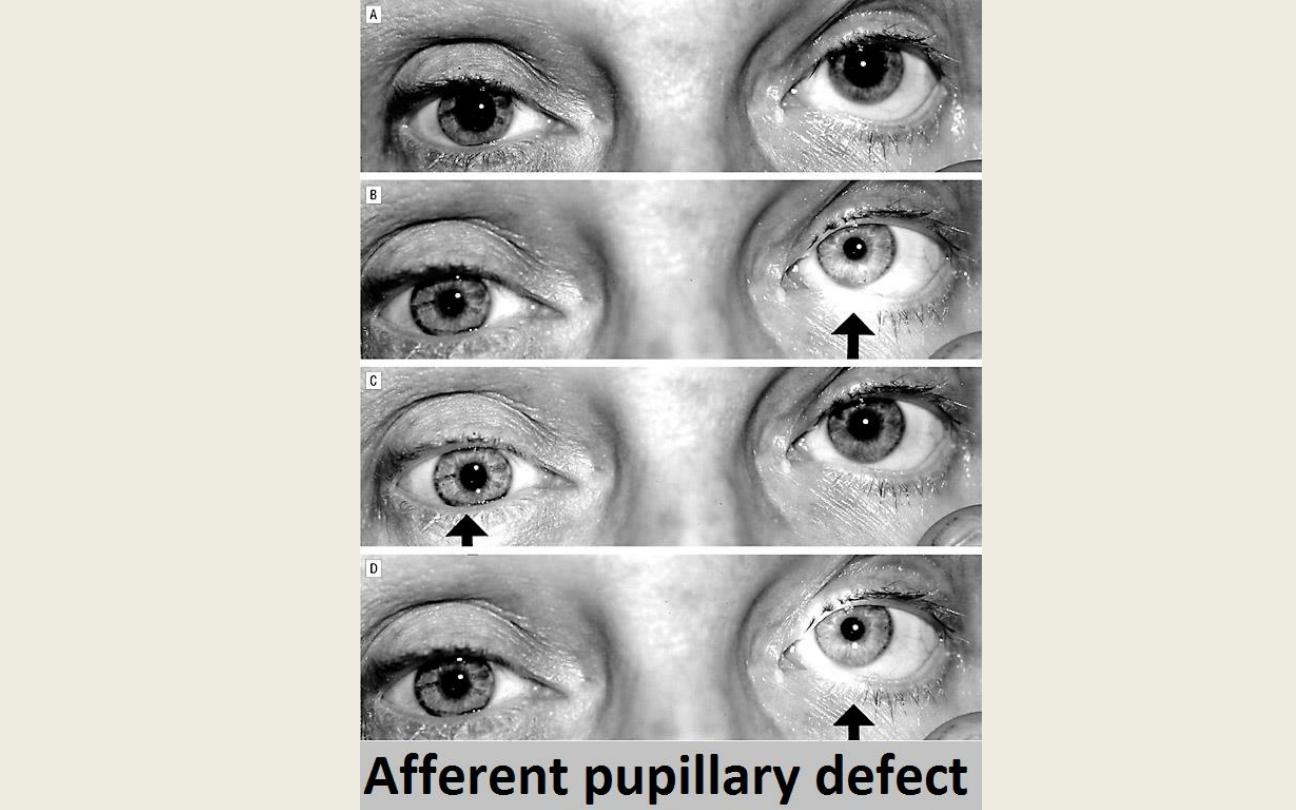
“Squint”
Anatomy of extraocular muscles
• They are four recti, two oblique's and levator palpebrae superioris.
• Listing plane: Imaginary plane dividing the eyeball into anterior and posterior
halves, passing through the center of rotation.
• Axes of Fick:
Axes around which the movements of eyeball are occur.
They are three; X (horizontal axis parallel to the iris plain), Y (horizontal axis
perpendicular to the iris plain and X-axis) & Z (vertical axis).
Movements around X-axis are elevation and depression.
Movements around Y-axis are Intorsion and extorsion.
Movements around Z-axis are adduction and abduction.
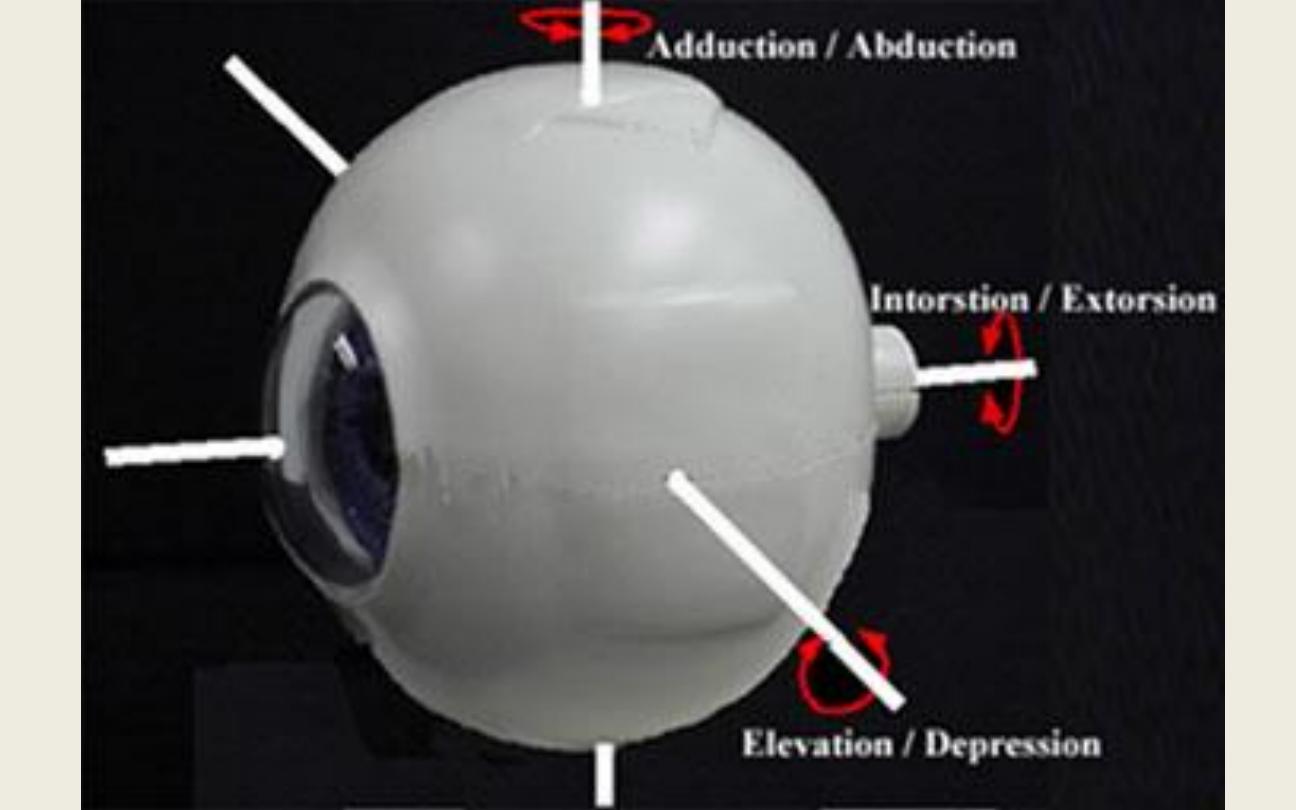
Recti muscles
• Innervations of the recti:
Medial, inferior and superior recti are innervated by oculomotor nerve,
the lateral rectus in innervated by abducent nerve.
• Action:
Medial rectus: Adduction.
Lateral rectus: Abduction.
Superior rectus: elevation (primary action in primary position of eye) & intortion
(2
nd
action) . It is pure elevator in abduction and pure intorter in adduction.
Inferior rectus: depression (primary action) and extortion (2
nd
action) . It is pure
depression in abduction and pure extortion in adduction. So the best position to
examine superior & inferior recti muscles is abduction to assess elevation &
depression respectively.
The Oblique muscles
• Innervation: Inferior oblique: Oculomotor nerve
Superior oblique: Trochlear nerve.
• Action:
Inferior oblique: extortion (primary action) and elevation (2
nd
action) in primary
position of the eye. It is pure elevator in adduction and pure extorter in abduction.
Superior oblique: intortion (primary action) and depression (2
nd
action) in primary
position of the eye. It is pure depressor in adduction and pure intorter in
abduction. So the best position to examine inferior and superior obliques muscles
is adduction to assess elevation and depression respectively.
• For movement of one eye, we use terms "Adduction" (for inward movement) and
"Abduction" (For outward movement).
• For simultaneous movement of both eyes, we use terms "Dextroversion" (for
movement to right) and "Levoversion" (for movement to left).
• We have combined movement like: dextro-elevation, dextro-depression, levo-
elevation and levo-depression.
• Definition of Squint: is a misalignment of the visual axes.
Visual axis: is a line between the point of fixation and the fovea passing through
nodal point. The normal visual axes intersect at the point of fixation.
Optical axis: line perpendicular to iris that falls on the retina between the mucula
& the optic nerve.
The angle between visual axis and optical axis is called alpha (α) or kappa (κ).
• The squint is either: Manifest (-tropia) or Latent (-phoria)
Latent (-phoria): is tendency of the eye to deviate when fusion blocked ((;when
one eye covered)
Manifest (-tropia): is a squint present when both eyes are open. It is of two types:
1- Comitant (or Concomitant): when the angle of squint is the same in all
directions of gaze.
2- Incomitant (paralytic): when angle of squint varies in various direction of gaze
and it become larger in the direction of paralytic muscle.
• Eso-= inward, Exo-= outward, Hyper-= Elevation, Hypo-= depression.
Squint
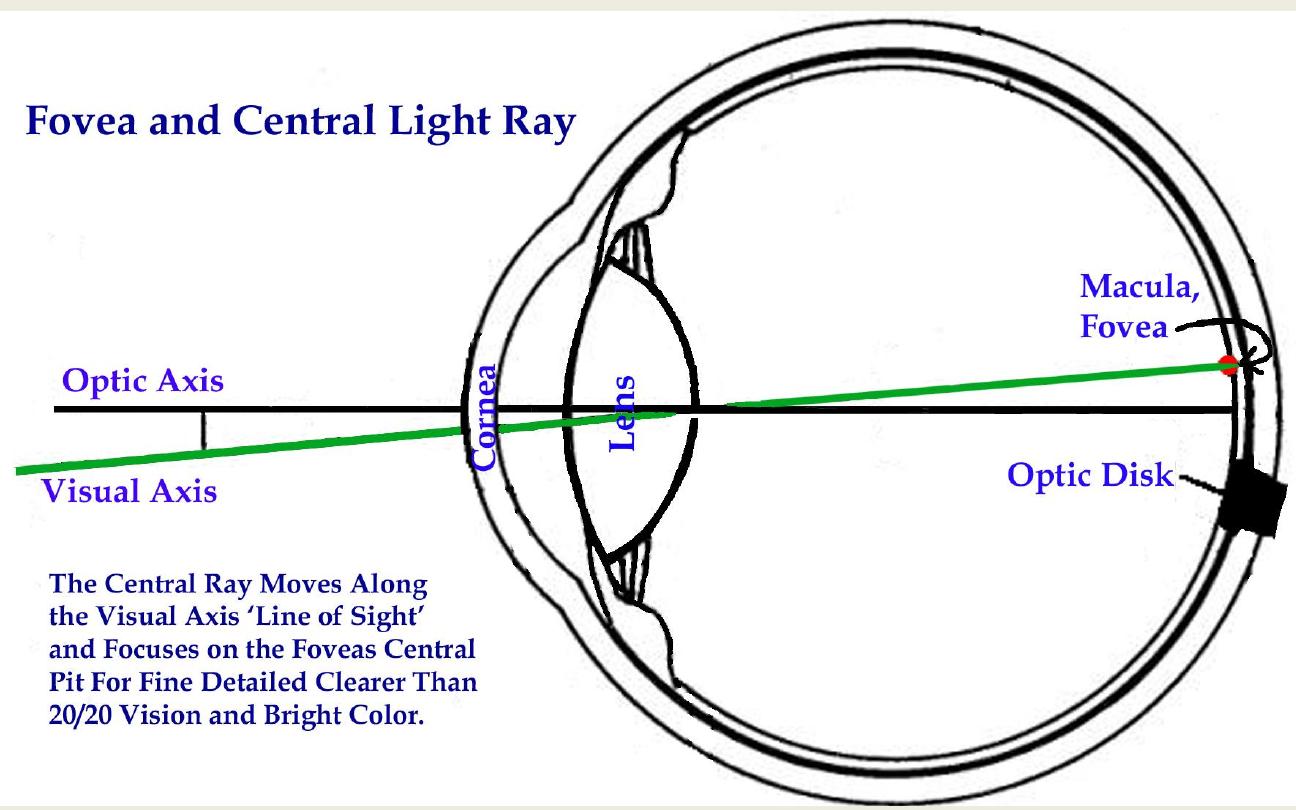
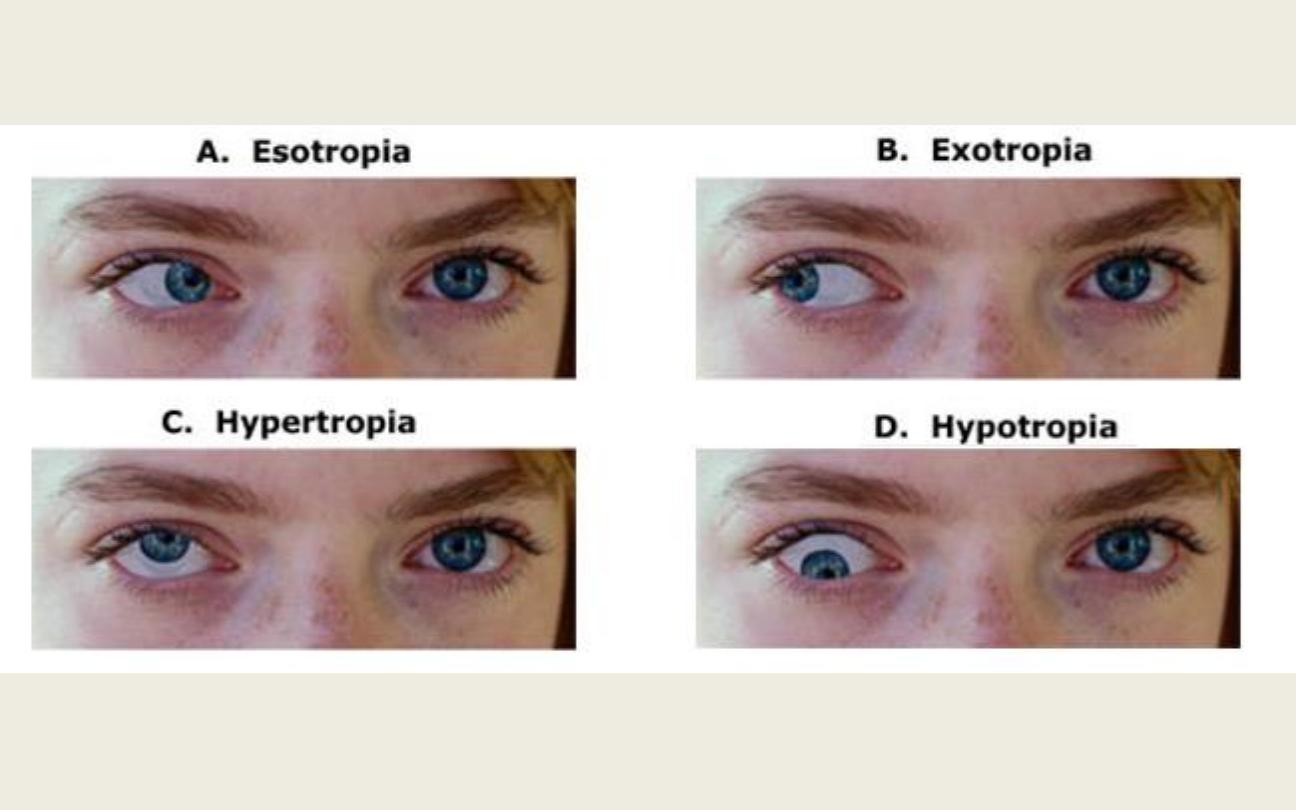
Pseudosquint
Convergent Pseudosquint
Divergent Pseudosquint
Small inter-pupillary distance
Wide inter-pupillary distance
Negative angle kappa e.g. myopia Large positive angle kappa e.g. hypermetropia.
Wide epicanthic folds
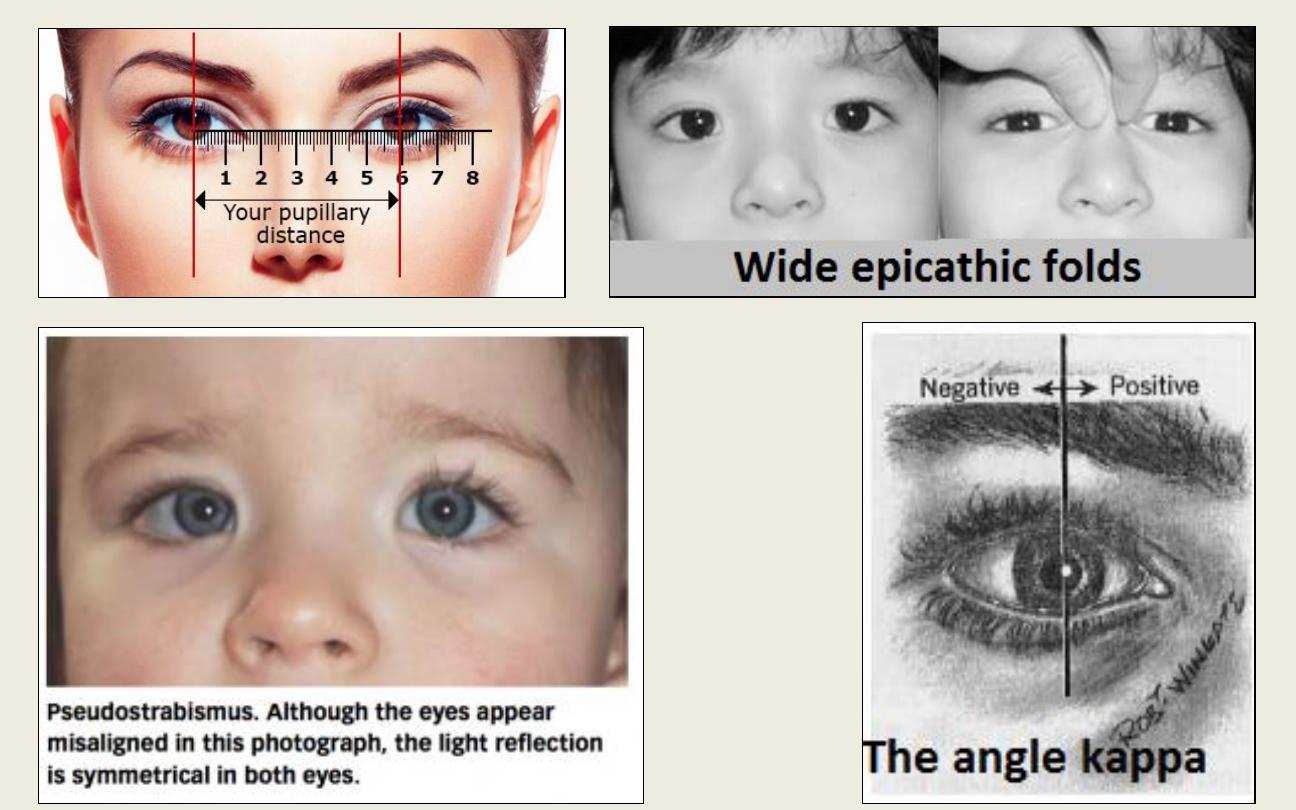
“Eye trauma”
Eyelid trauma
Haematoma (Black eyes) (Panda eyes):
• It is the most common result of blunt injury to the eyelid or forehead (due to
continuous space below the tense aponeurosis of scalp that extends to the loose
space around the eye). It is important to exclude the following serious associated
conditions: a- Trauma to the globe. b- Orbital walls fracture c- Basal skull fracture.
Laceration:
Two types of eyelid laceration:
• Superficial lacerations:
They are parallel to the lid margin without gaping.
Treatment: suturing.
• Lid margin lacerations:
Which are invariably gape and must therefore be carefully sutured with perfect
alignment to prevent notching.
Improper suturing may end with notching or fibrosis (scars) that causes foreign
body sensation and then corneal abrasion.


Orbital Fractures
Blow-out floor fracture:
• Caused by sudden increase in the orbital pressure by a striking object such as a fist
or tennis ball. most frequently involves the floor.
• Signs:
Periocular signs: ecchymosis, oedema and subcutaneous emphysema.
Infraorbtal nerve anaesthesia: involving the lower lid, cheek, side of the nose,
upper lip, upper teeth and gums. Vertical diplopia. & Enophthalmos.
Ocular damage, e.g. hyphaema, angle recession and retinal dialysis.
Angle recession: recession of the angle between the periphery of the iris and
anterior face of ciliary body, which seen by gonioscope.
Retinal dialysis: break at ora serrata (disinsertion of retina).
• Treatment of Blow out floor fracture:
Initially, it is conservative with systemic antibiotics; the patient should be
instructed not to blow the nose to avoid transmission of bacteria from maxillary
sinus to the orbit. Then surgical repair

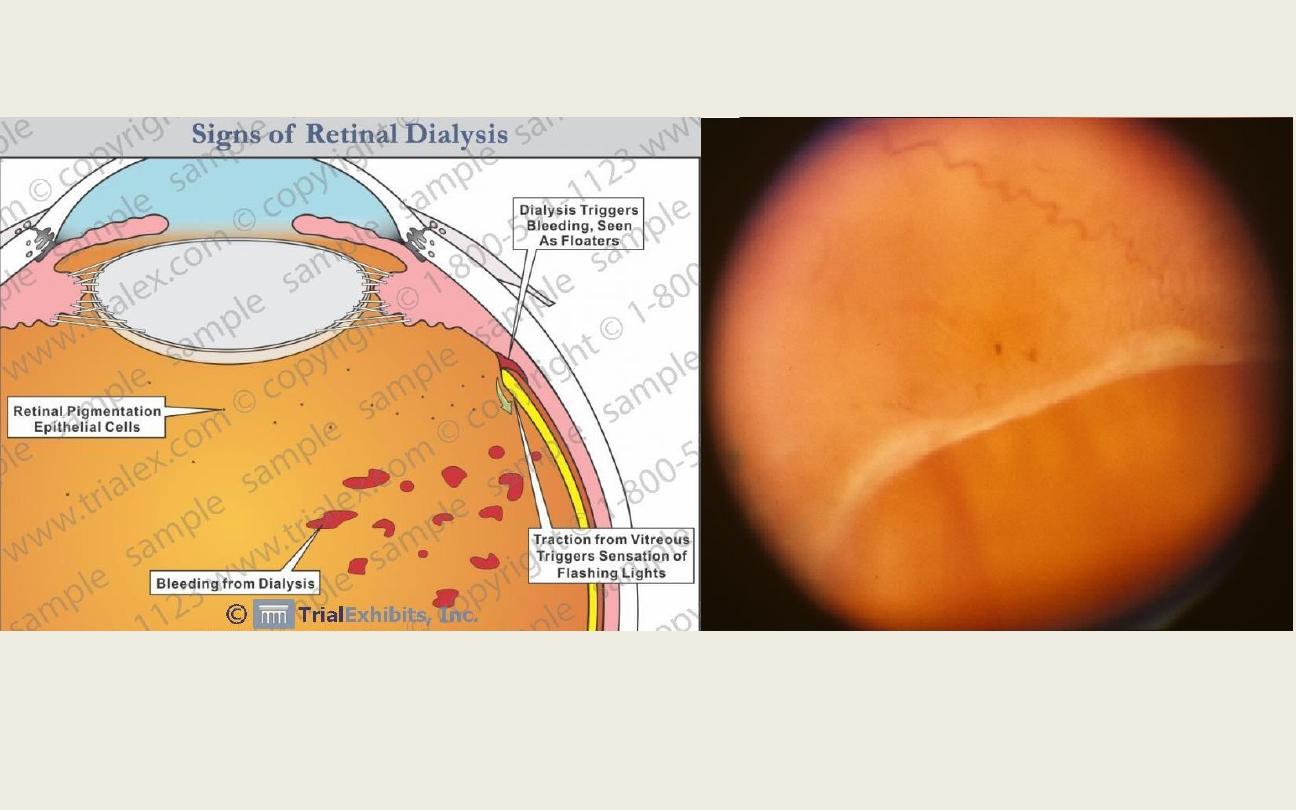
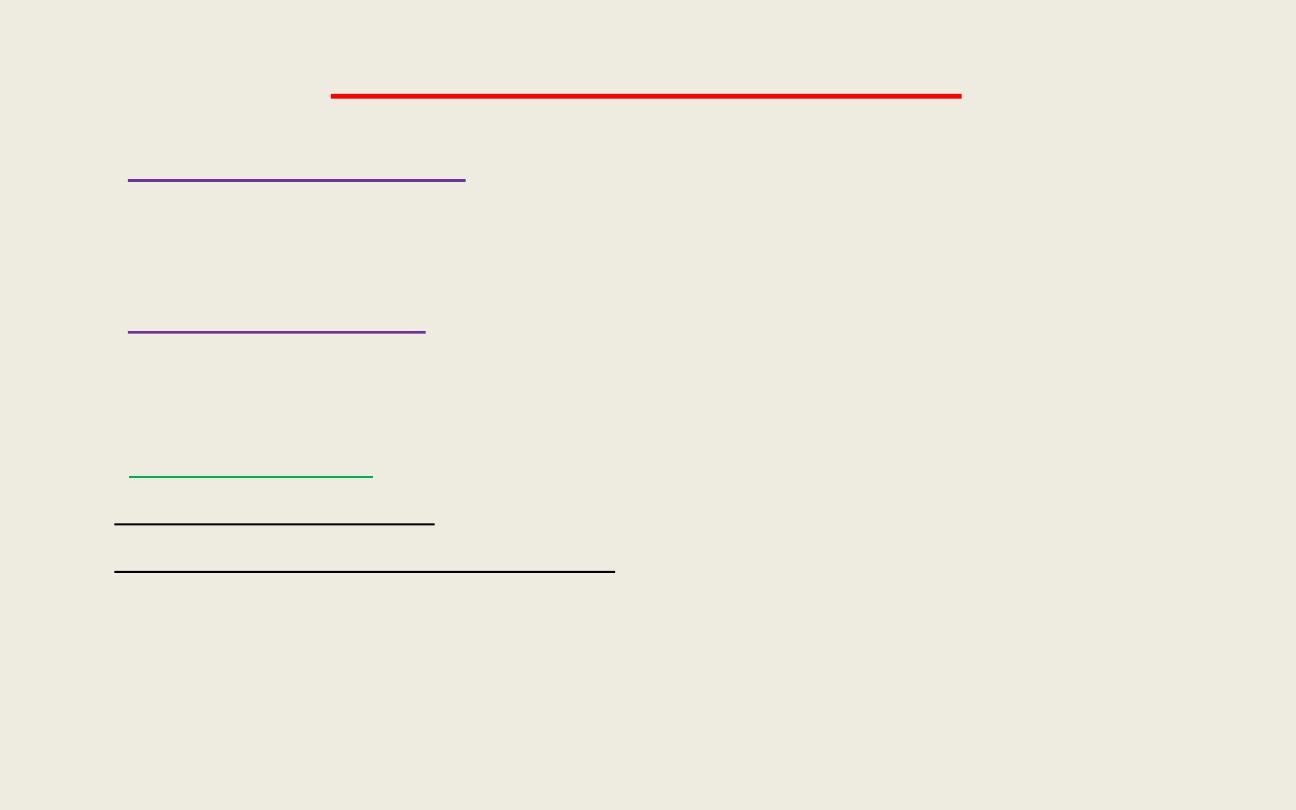
Trauma to the globe
Closed injury:
it is commonly seen due to blunt trauma. The corneoscleral wall of the globe is
intact; however, intraocular damage may be present.
Open injury:
it involves a full-thickness wound of the corneoscleral wall. Open injury can occur
by the following mechanisms:
Blunt trauma
• Trauma by sharp object: e.g. knife.
• Trauma by high velocity sharp object: e.g., shell injury, small foreign bodies
scattering from hammer or other material, which can cause single full-thickness
wound without an exit wound (there is intraocular retention of the foreign body),
this type of wound is called "Penetration wound". If it cause two full-thickness
wounds, one entry and one exit, which is usually caused by a missile (no retention
of the foreign body), this type of wound called "Perforation wound".
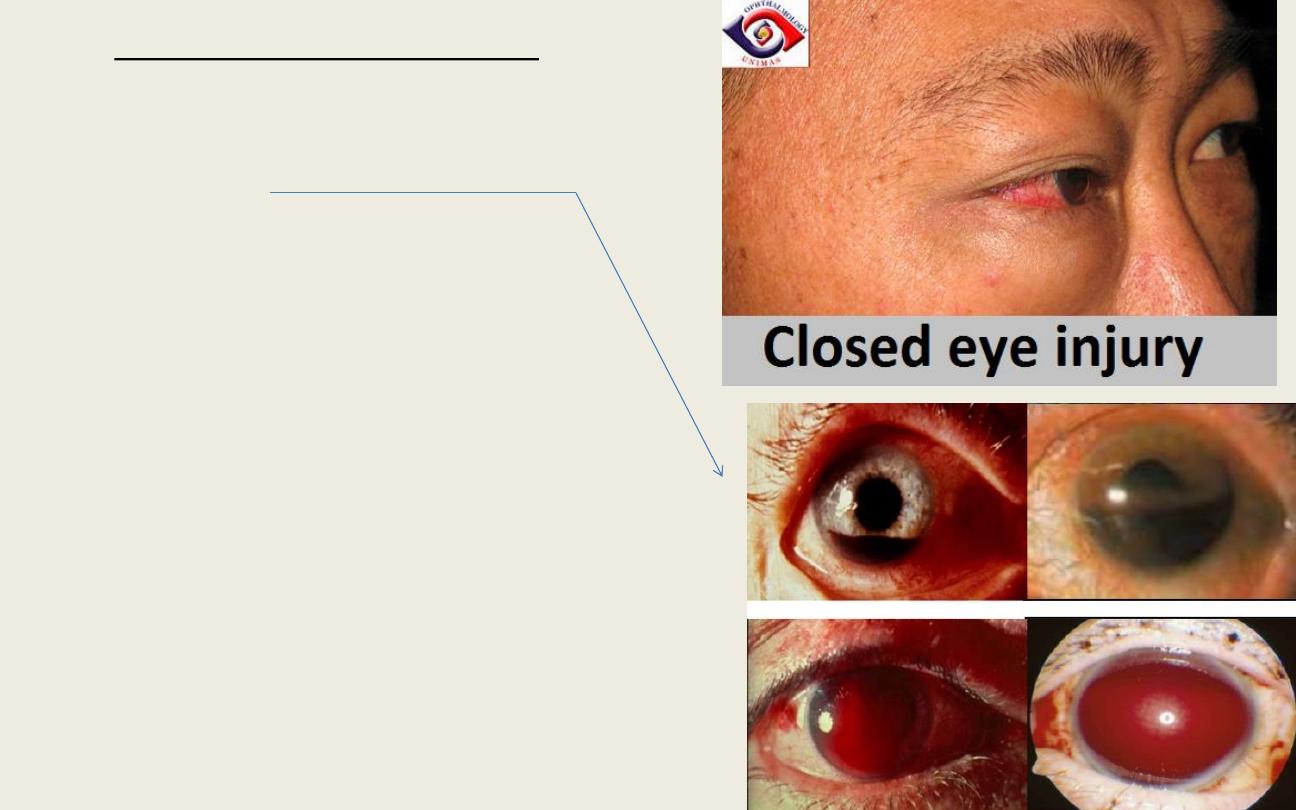
• Complications of blunt trauma:
Anterior segment complications:
o Corneal abrasion
o Hyphaema
o Traumatic mydriasis
o Iridodialysis
o Ciliary body shock & angle recession
o Lens (cataract)
o Rupture of the globe
Posterior segment complications:
o PVD (posterior vitreous detachment)
o Commotio retinae
o Choroidal rupture.
o Retinal break
o Optic neuropathy
o Optic nerve avulsion
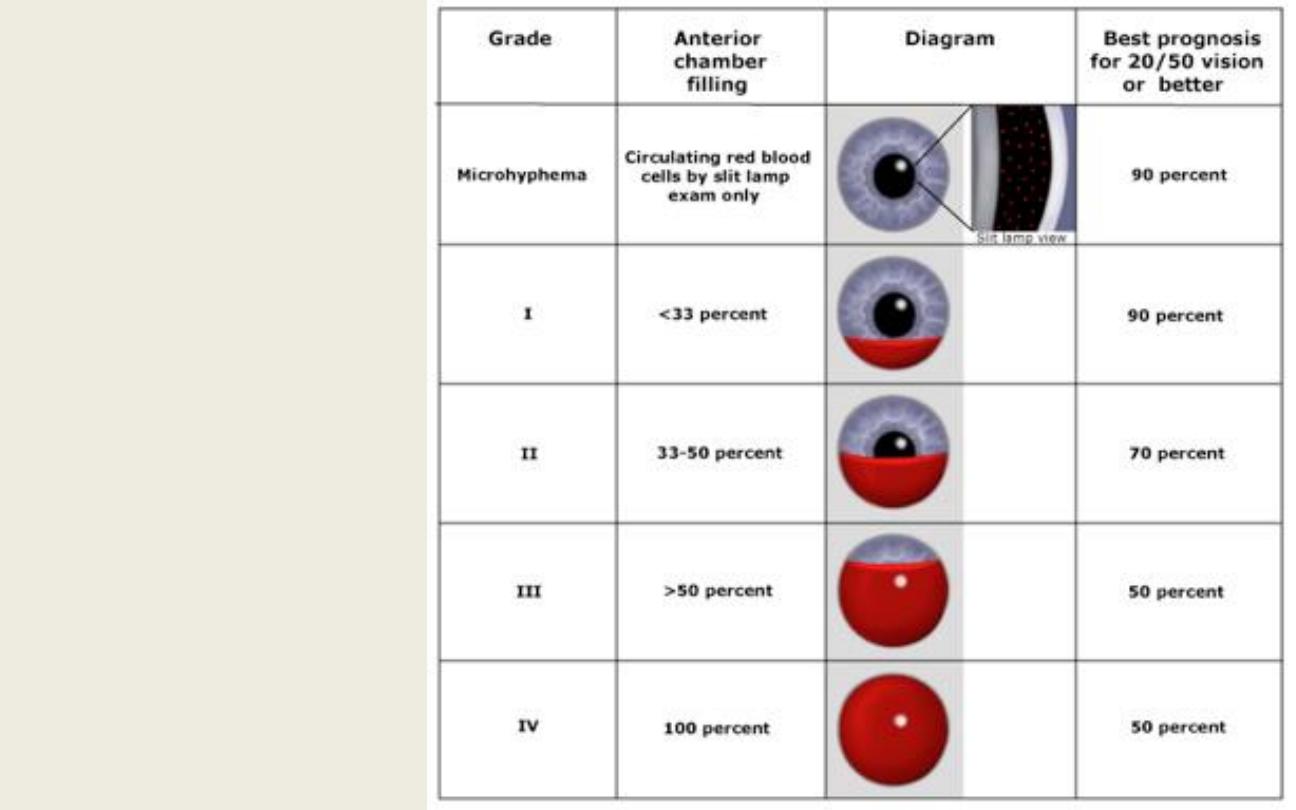
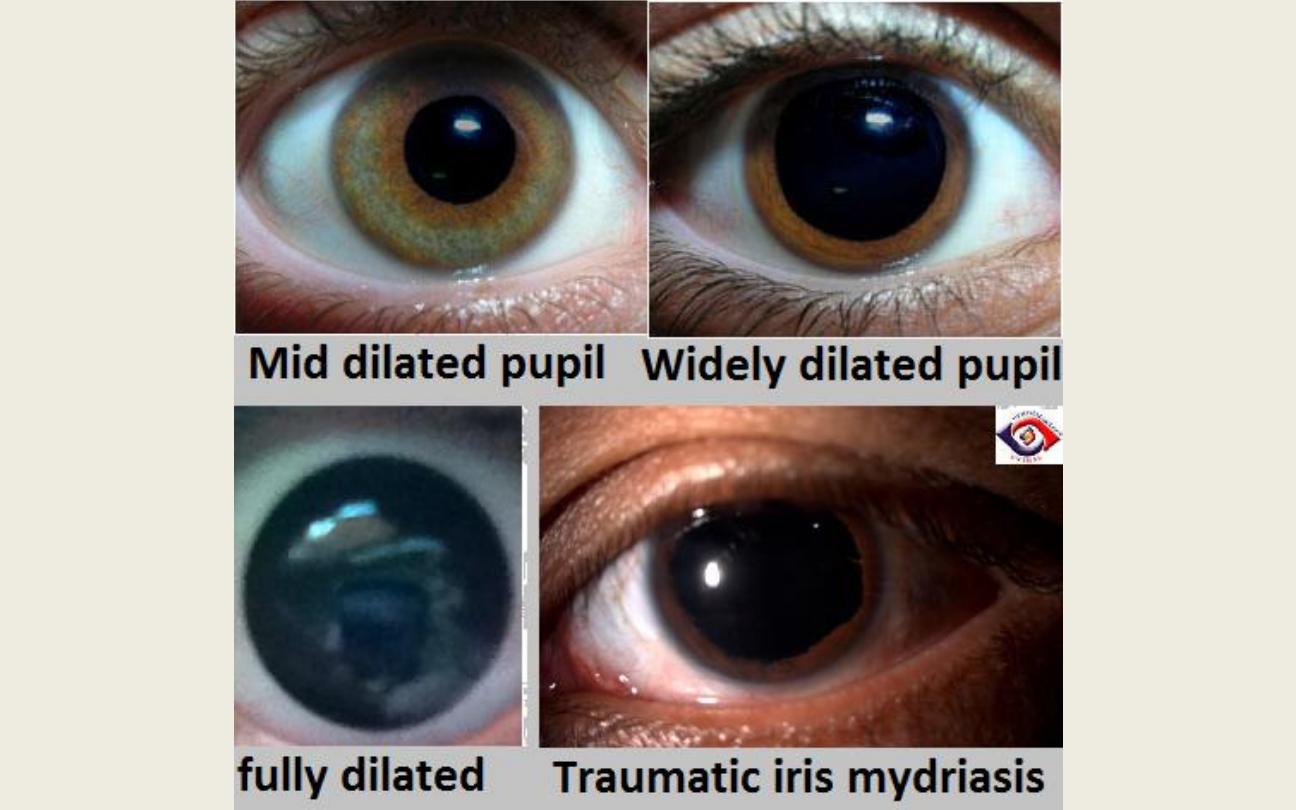
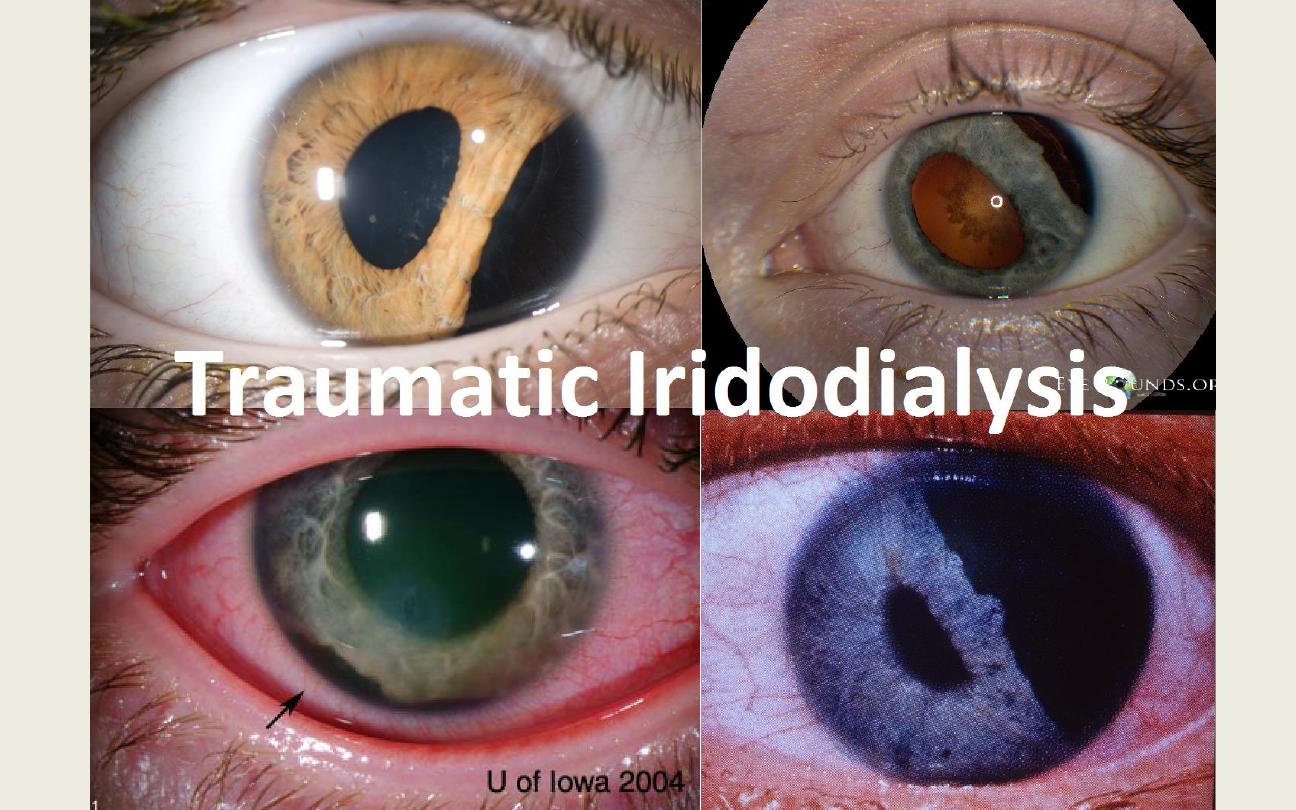
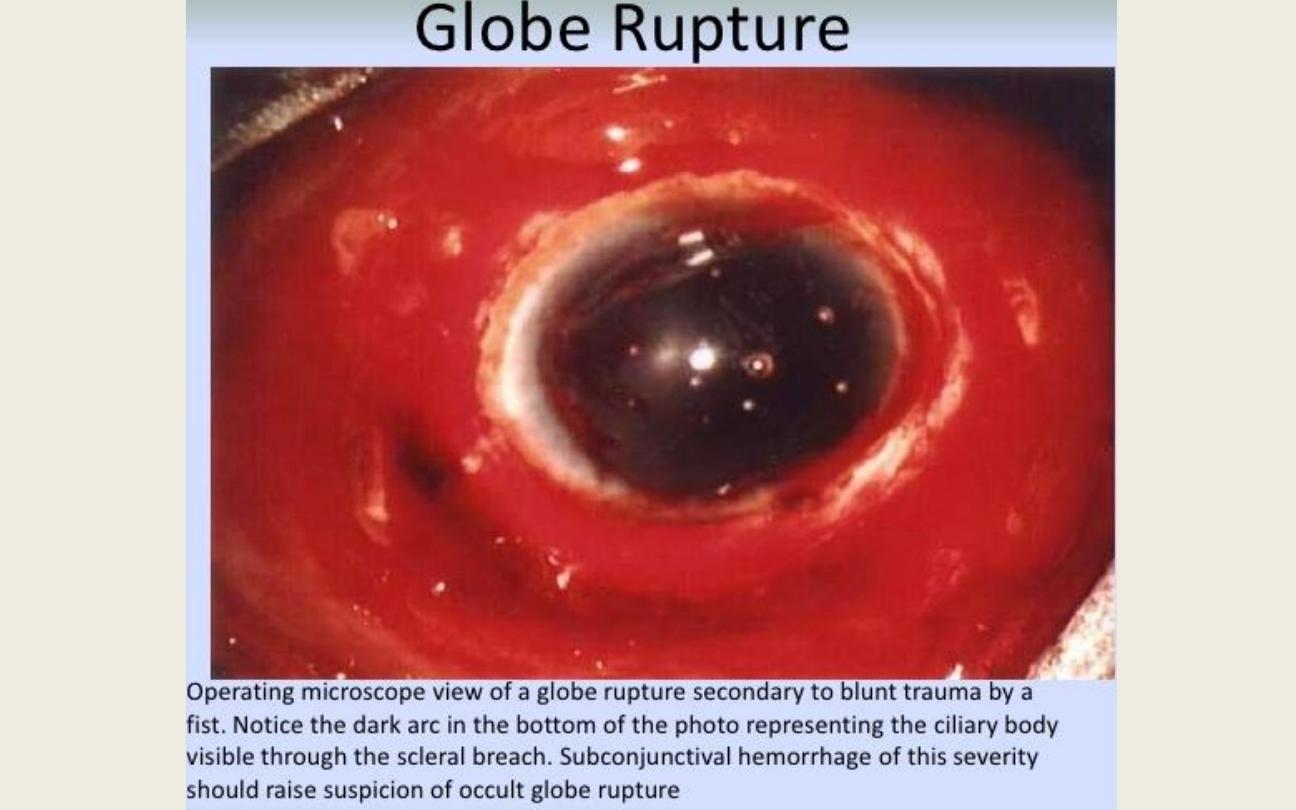
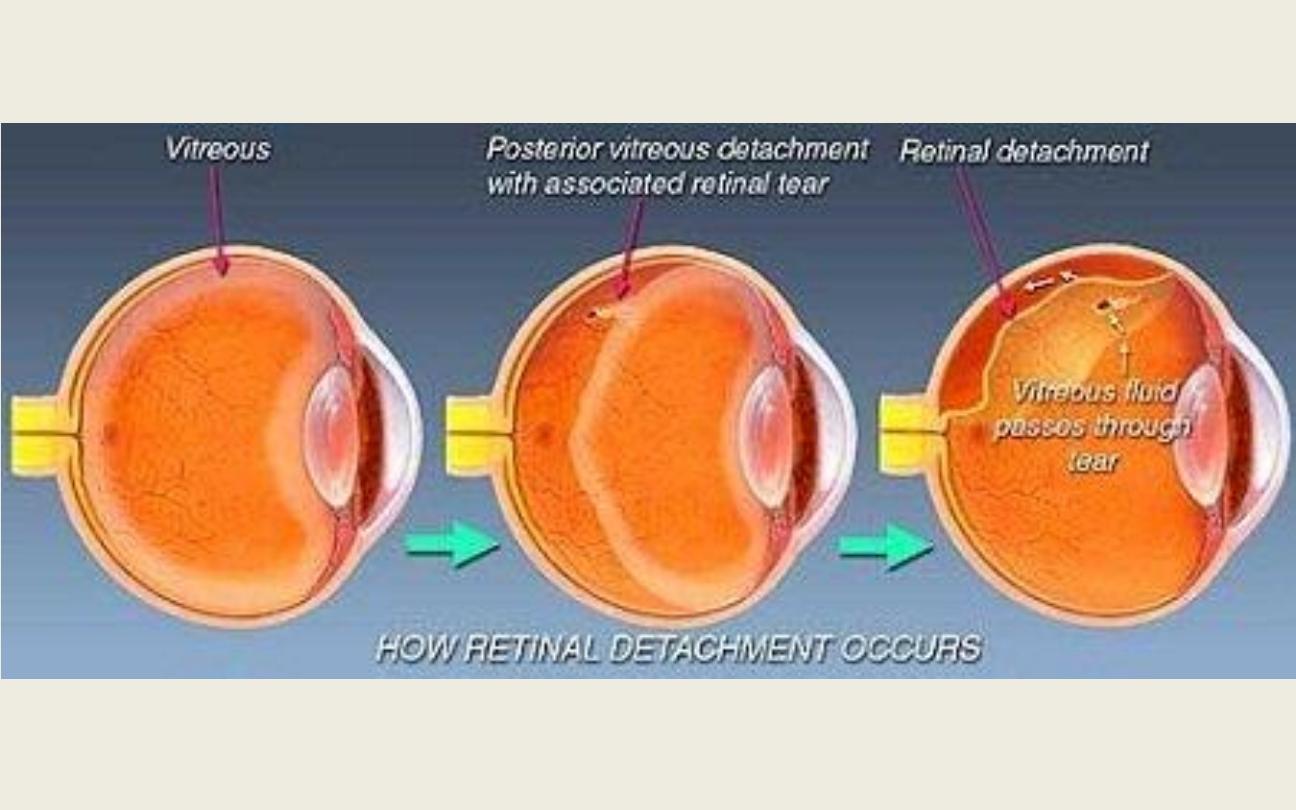
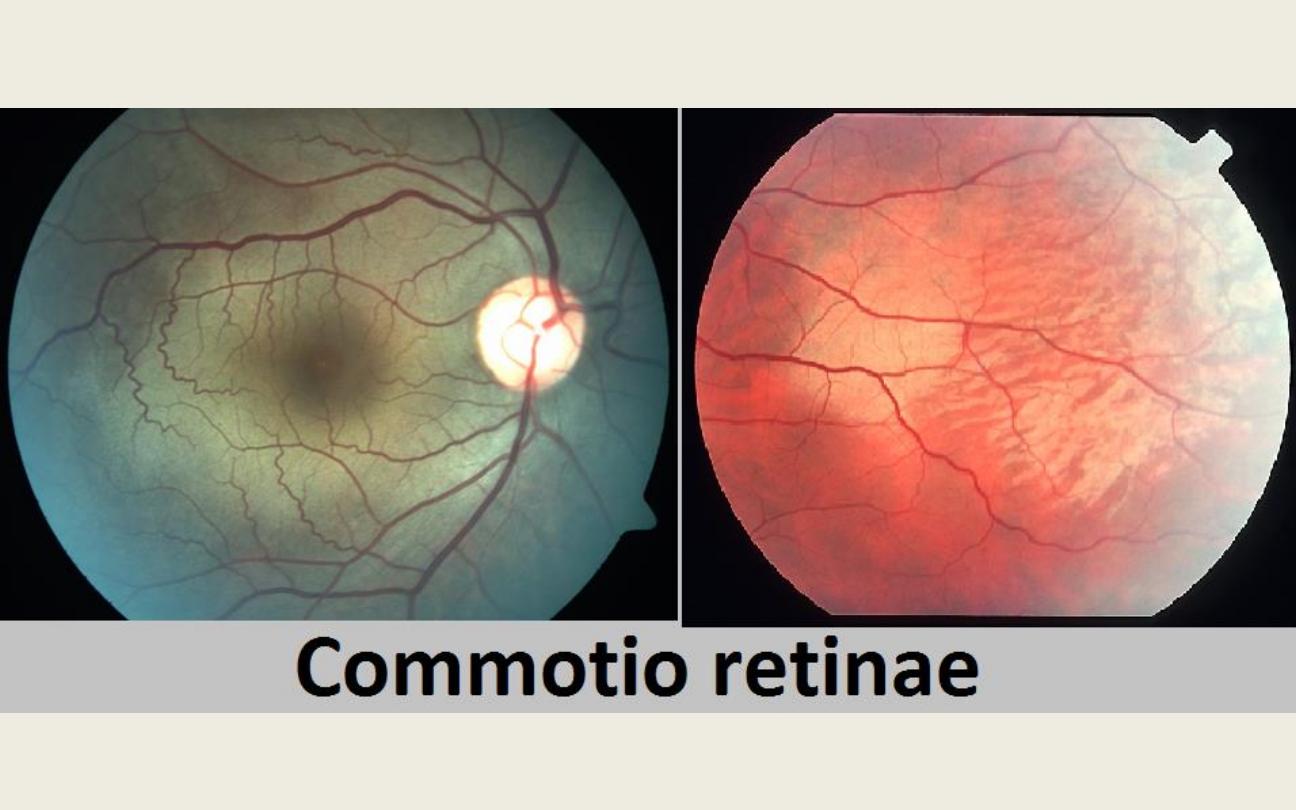
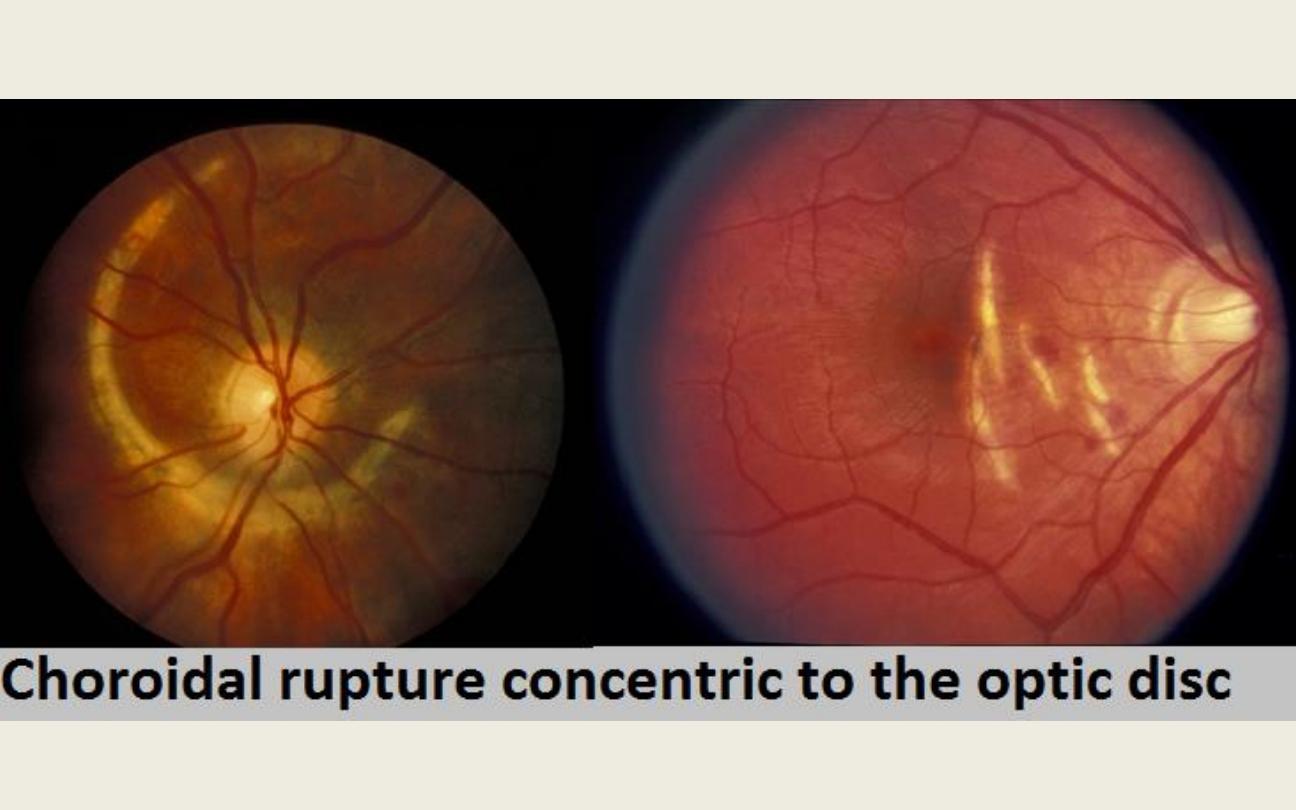
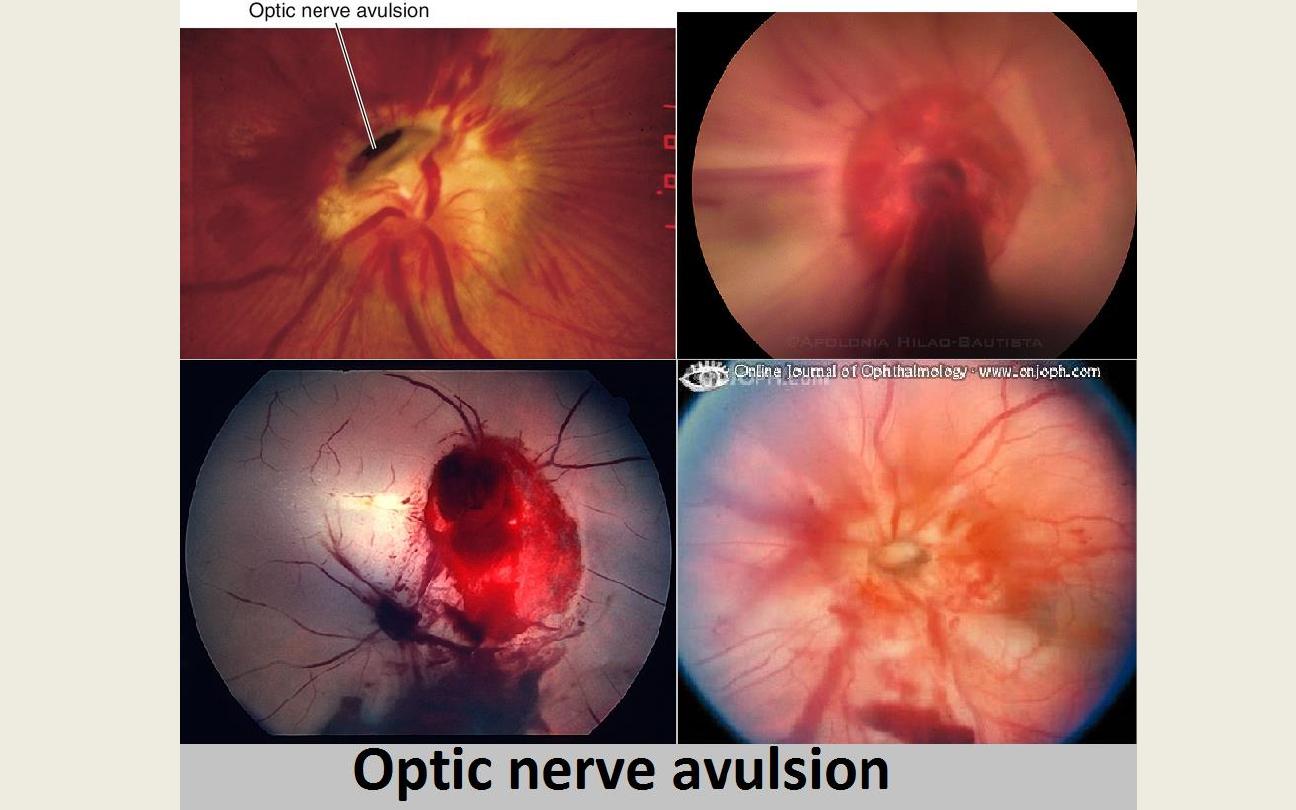
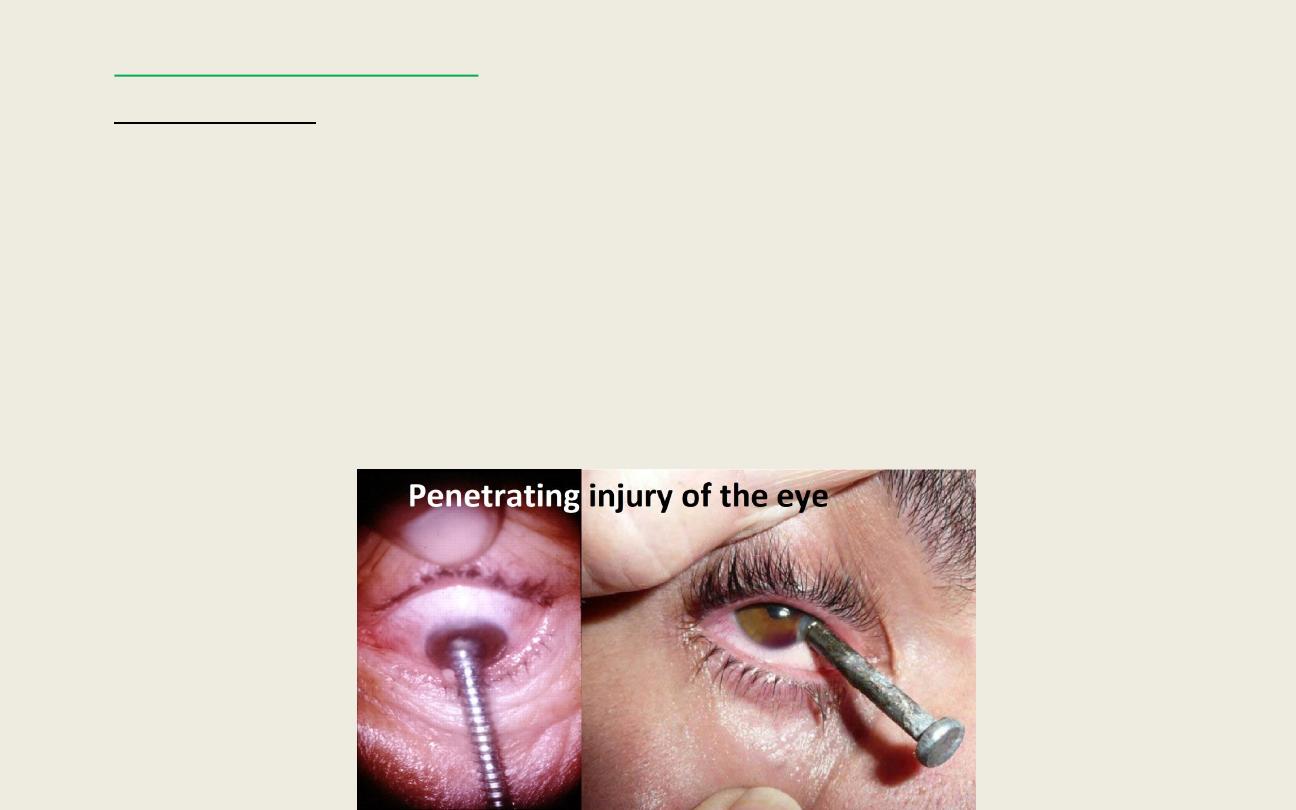
Penetrating trauma
• Complications:
Anterior segment complications:
o Small corneal lacerations
o Medium-sized corneal lacerations
o Corneal lacerations with iris prolapse
o Corneal lacerations with lenticular (lens) damage
o Anterior scleral laceration ± Iridociliary prolapse and vitreous incarceration
Posterior segment complications: Posterior scleral lacerations
• General principles of management:
Initial assessment:
a- Determination of any associated life-threatening problems, and general
condition should be stabilized.
b- History: circumstances, timing and likely object.
c- Thorough examination of both eyes and orbits.
Special investigations: to localize the foreign body & associating ocular injury.
a- Plain radiographs:
b- CT. MRI should never be performed if a metallic foreign body is suspected
c- Ultrasound.
d- Electrophysiological tests (VEP, EOG, ERG)
If the foreign body is in the vitreous, we do vitrectomy & if it is the lens, we do
intracapsular cataract extraction (ICCE) to remove the cataractous lens with the
F.B.
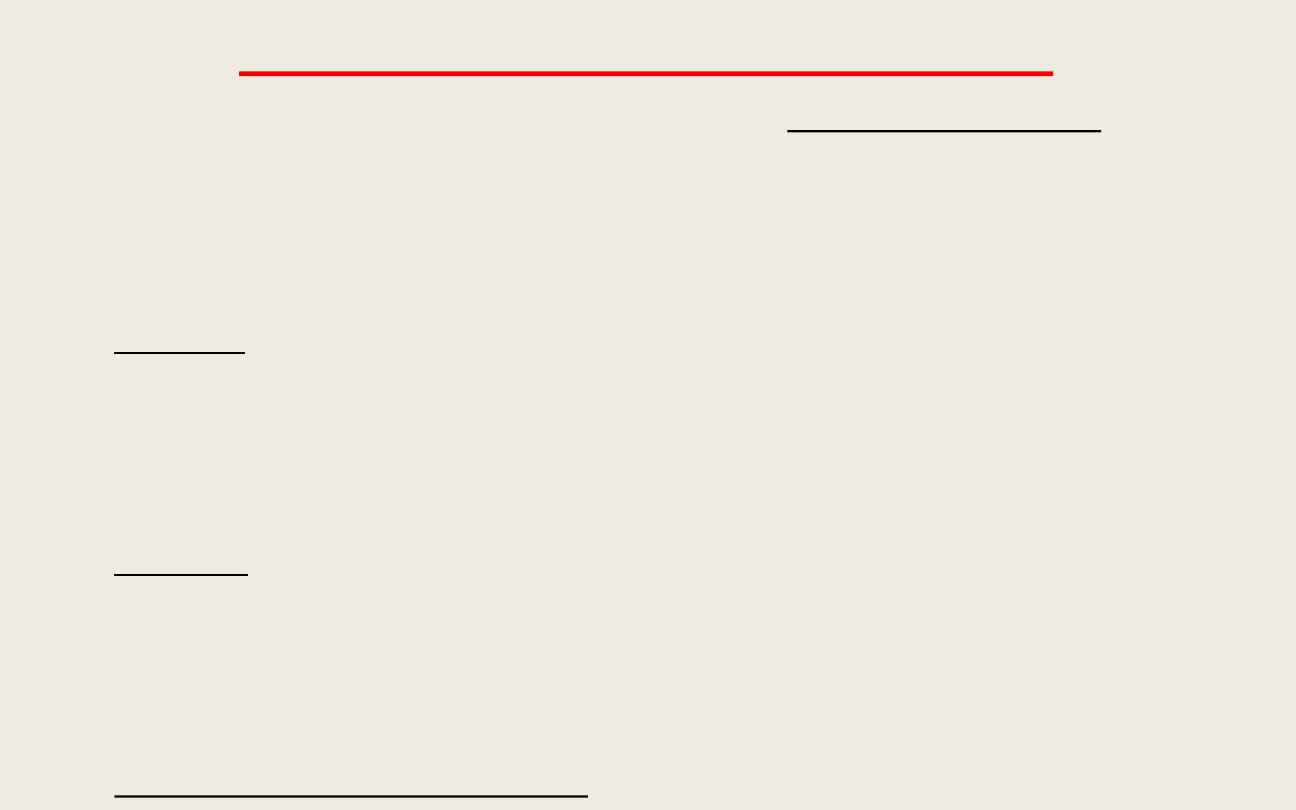
Intraocular foreign bodies
• An IO foreign body may traumatize the eye by the following mechanisms:
1- Mechanically (laceration). 2- Introduce infection.
3- Toxic effects on the IO structures.
• Stones and organic foreign bodies are prone to result in infections.
• Glass, plastics, gold & silver are inert, so we can leave the object if it has no effect.
• Siderosis:
IO ferrous foreign body result in the deposition of Iron in the IO epithelial cells
(especially in lens and retina) that leads to toxic effect that leads to cell death.
Features: cataract, reddish-brown staining of the iris, secondary glaucoma (due to
trabecular meshwork deposition) & pigmentary retinopathy (blindness).
• Chalcosis:
The ocular reaction to an IO foreign body with a high copper content involves a
violent endophthalmitis-like picture which often progress to phthisis bulbi.
Endophthalmitis means that there is inflammation of all IO structures except the
sclera, but if inflammation involves the sclera it is called "Panophthalmitis".
• Treatment of siderosis & chalcosis: Iron & Copper foreign body should be removed
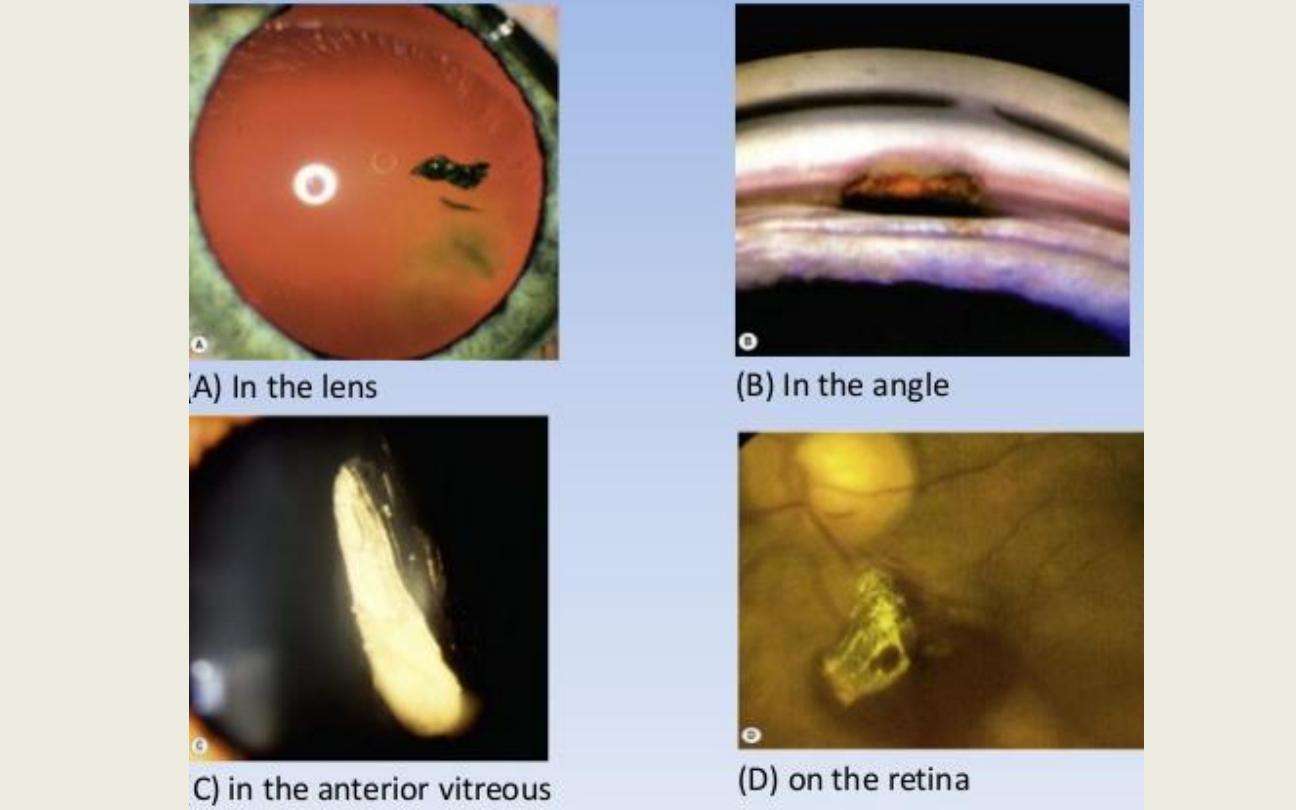
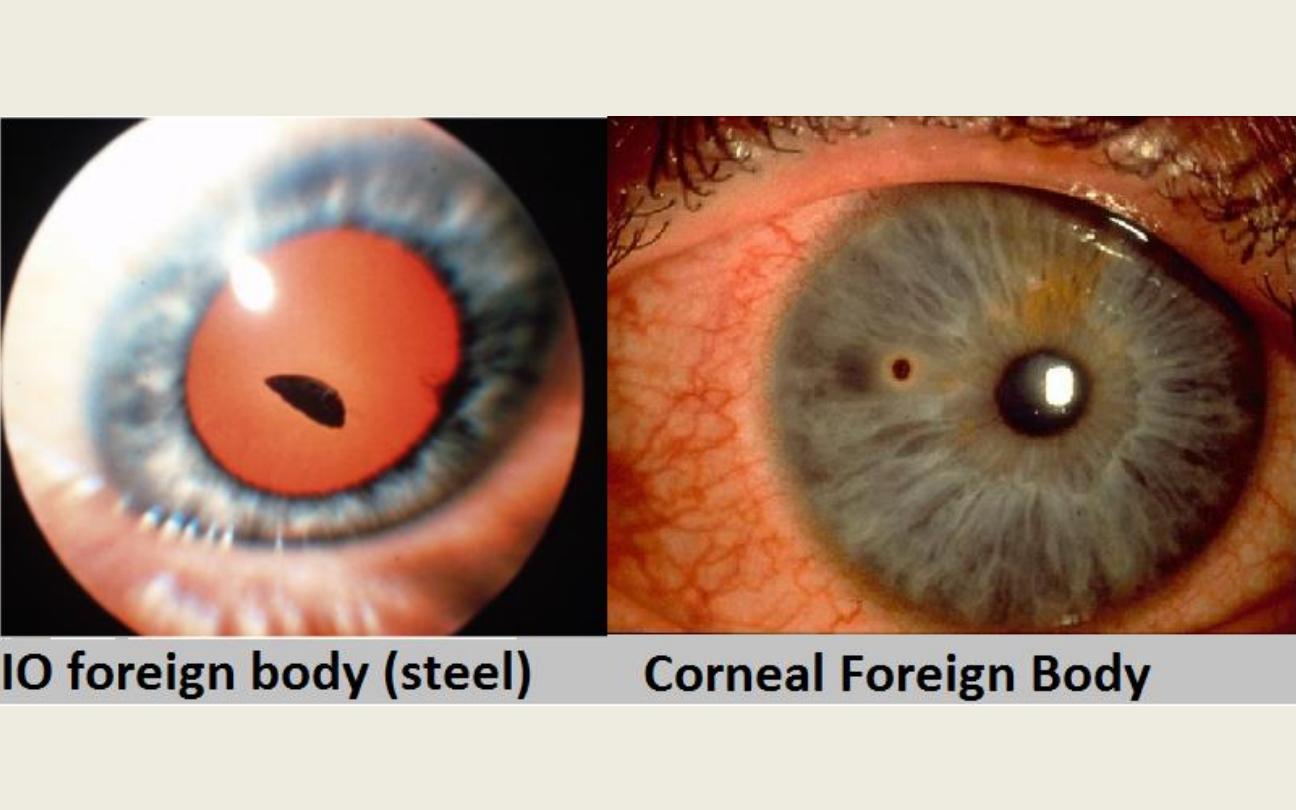
Chemical trauma
• The alkaline is twice as common as acidic because it is more widely used than
acid. Alkaline burn more dangerous than acid, because alkaline one penetrate
deeply causing liquefactive necrosis of corneal collagen while acid causing
coagulative necrosis forming barrier against further penetration of acidic material.
• Treatment
Emergency treatment: ○ Copious irrigation: by sterile balanced puffered
solution eg ringer lactate, normal saline. Tap water can be used if solutions not
available. Irrigation for 15-30 m or till PH normalized.
o Double lid elevation: retained particle if trapped in the fornix should be removed.
o Admission: for sever chemical injuries.
Medical treatment:
o Topical steroid: anti-inflammatory & for associated ant. Uveitis.it has action
against fibroblast migration & reduce collagen synthesis so it used for 1
st
week
only &stopped in the 2
nd
week. ○ Topical prophylactic antibiotic.
o Ascorbic acid (topical & systemic): enhance collagen synthesis & wound healing.
o Tetracycline systemic & topical: had anti collagenase action, reduce ulceration.
o Topical cycloplegic agent: for comfort.
Surgical treatment: For eyelid & corneal complications
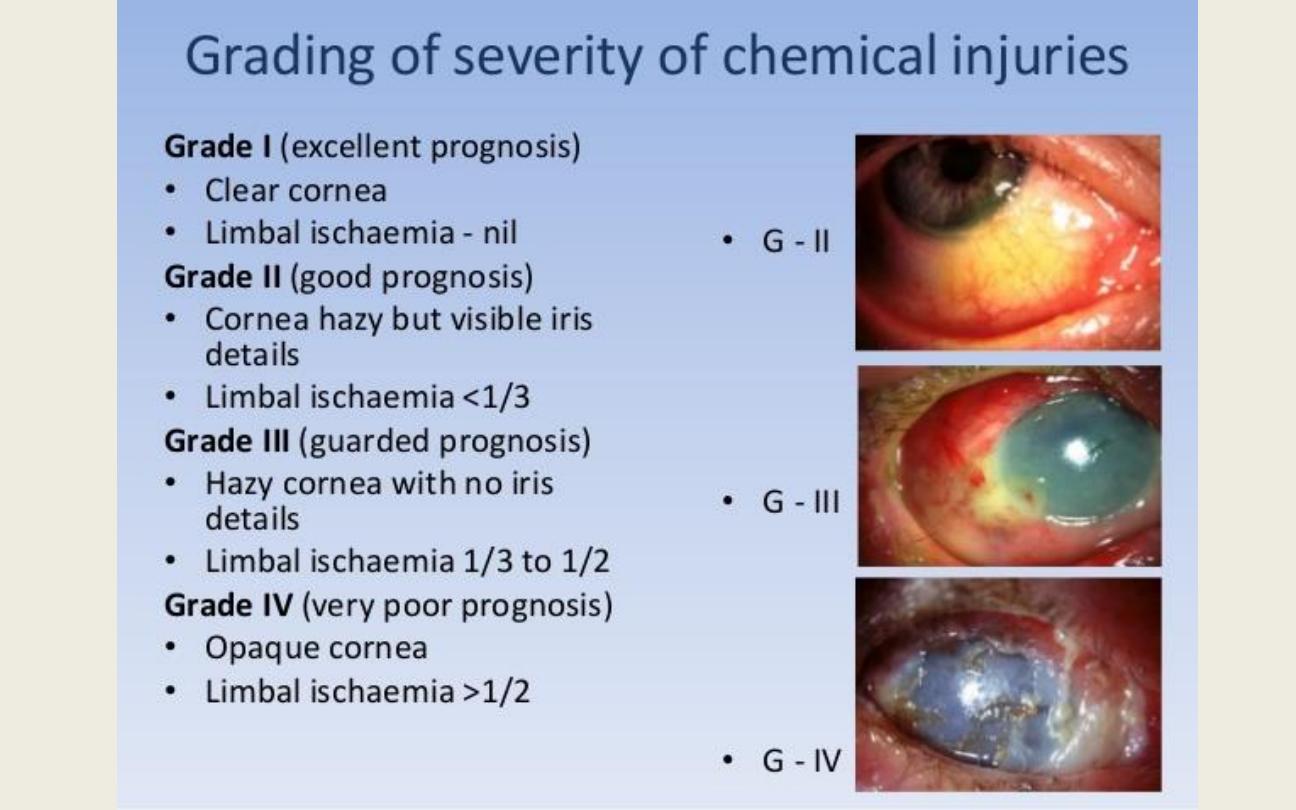

“Differential
diagnosis”
• Conjunctivitis
• Subconjunctival hemorrhage
• Episcleritis
• Chronic red eye
• Dry Eye Syndrome
• Scleritis
• Corneal Abrasion
• Corneal Ulcer
• Anterior uveitis (iritis)
• Acute Angle-closure Glaucoma
• NVG (neovascular glaucoma) angle closure type
DDx of red eye
• Usually nonurgent
Blepharitis
Subconjunctival hemorrhage
Inflamed pterygium
Inflamed pinguecula
Dry eye syndrome
Airborne contaminants or irritants
Tiredness
Drug use including cannabis
• Usually urgent
Acute glaucoma
Injury
keratitis
Iritis
Scleritis
Episcleritis
Tick borne illnesses like Rocky Mountain
spotted fever
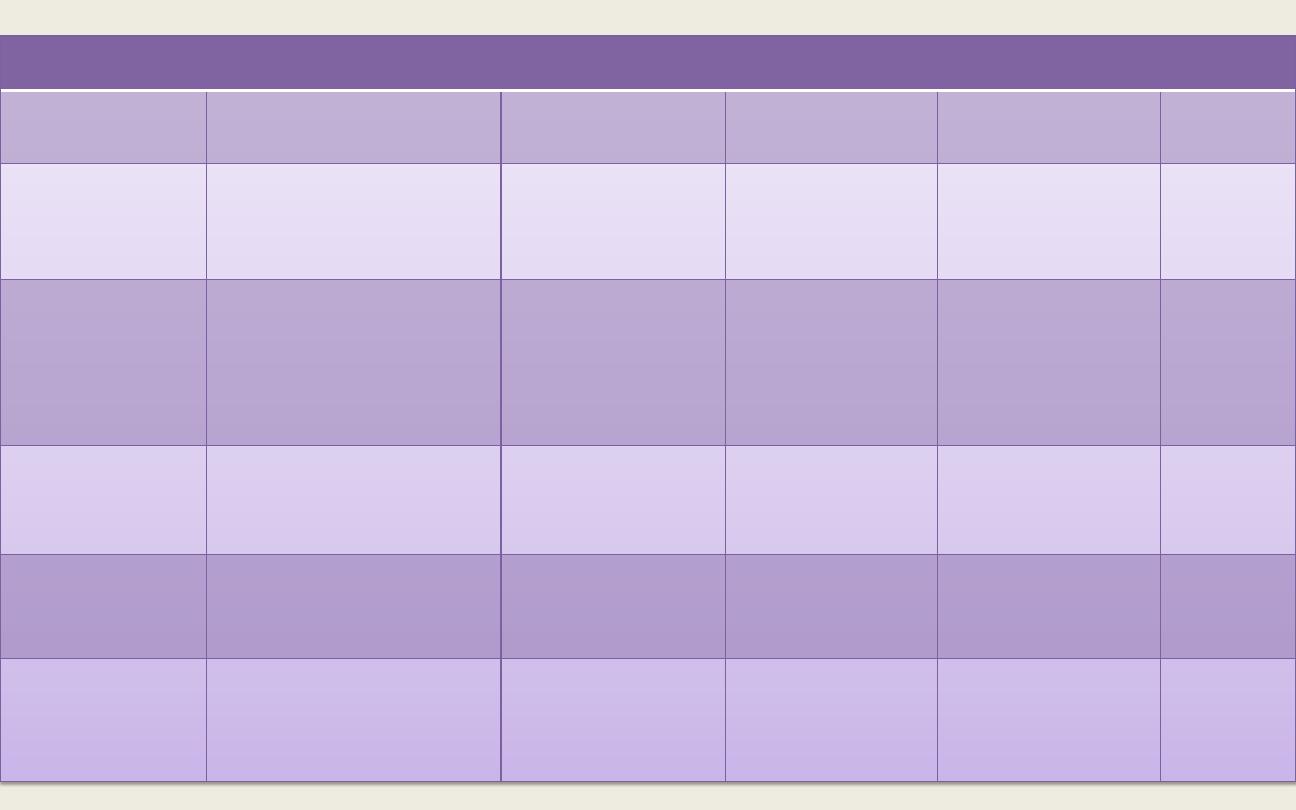
IOP
Discharge
Pupil
VA
Site of redness
Normal
No
Normal
Normal
Bright blood j.
Subconj hage.
Normal
Yes
Normal
Normal
Injection mainly at
the fornix
Conjunctivitis
May
affected
Yes
May affected if
iritis present
Affected
Juxtalimbal in jection,
corneal infiltrate.
Keratitis
Affected
+_ Lacrimation
Miosed
Affected
Juxta limbal (ciliary
flush)
Iritis
50 &
above
No
Fixed mid
dilated
Affected
Diffuse redness
Acute angle
closurea
Normal
No
Normal
Normal unless
necrotizing with
complication
Deep episcleral
plexus injection
Scleritis
DDx of eye pain
• Allergies
• Blepharitis (eyelid inflammation)
• Blocked tear duct
• Chalazion (a type of cyst on your eyelid)
• Cluster headache
• Contact lens problem
• Corneal abrasion (scratch): First aid
• Dry eyes (decreased production of tears)
• Ectropion (outwardly turned eyelid)
• Entropion (inwardly turned eyelid)
• Foreign object in the eye: First aid
• Glaucoma (group of conditions that damage the optic nerve)
• Injury, such as from a blunt trauma or burn
• Iritis (inflammation of the colored part of the eye)
• Keratitis (inflammation of the cornea)
• Optic neuritis (inflammation of the optic
nerve)
• Pink eye (conjunctivitis)
• Scleritis (inflammation of the white part of
the eye)
• Sty
• Uveitis (inflammation of the middle layer of
the eye)
DDx of gradual vision loss
Painless loss
• Refractive error
• Cataracts
• Age-related macular degeneration (AMD)
• Chronic (primary) open-angle glaucoma
• Diabetic retinopathy
• Compression of optic nerve or optic pathway
• Drugs, toxins or nutritional deficiency
Amiodarone - various effects on the eye
Antituberculous drugs - ethambutol and isoniazid (optic neuritis).
Hydroxychloroquine (maculopathy).
Systemic steroids (cataracts and glaucoma)
Phosphodiesterase inhibitors (eg, sildenafil).
Others drugs - tetracyclines (benign intracranial hypertension), isotretinoin,
tamoxifen (various possible effects on vision).
Alcohol, smoking and nutritional deficiency: Tobacco-alcohol amblyopia,
Methanol poisoning & Vitamin A deficiency (classically causes night blindness).
• Hereditary retinal dystrophies
Painful loss
This is much rarer and tends to suggest a more sinister pathology such as:
• A progressive neoplastic (eg, choroidal melanoma) or inflammatory process (eg,
chorioretinitis).
• A systemic problem (eg, sarcoidosis or collagen vascular disease).
• Lesions on the optic nerve (eg, optic neuritis, granuloma or neuroma).
• Intracranial pathology or masses (may present with headache, or with endocrine
symptoms if a pituitary tumour).
• Intracranial hypertension (may have headache).
DDx of sudden vision loss
Trauma
blunt trauma, lacerations or penetrating injuries, as well as either open or closed
head trauma.
Drugs
Non-traumatic
• Media Opacities
Corneal edema
Angle-closure glaucoma
Hyphema
Vitreous hemorrhage
• Retinal Abnormalities
Retinal detachment
Acute maculopathy
Transient monocular blindness
Retinal artery occlusion
Retinal vein occlusion
• Neurologic Disease
Papilledema
Optic neuritis
Ischemic optic neuropathy
Compressive optic neuropathy
Chiasm or retrochiasmal disorder
Migraine/idiopathic
• Functional Vision Loss
Benign causes, such as dry eye disease or migraine.
More serious causes are common, including GCA, carotid artery disease or retinal
detachment.
