OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 0
LIST OF CONTENTS
PAGE NUMBER
History
1 - 3
Examination
3 - 4
Description of a skin lesion
5 - 8
Lesion type (Primary & secondary skin lesions)
5
Changes encountered in skin
6
Lesion Configuration
6
Texture
7
Area involving the lesion & Lesion shape
7
Location and Distribution
7
Color
8
Special clinical & laboratory aids to
dermatologic diagnosis
9 - 13
Special techniques used in clinical examination
9
Clinical Signs
10
Clinical Tests
11
Laboratory tests
12
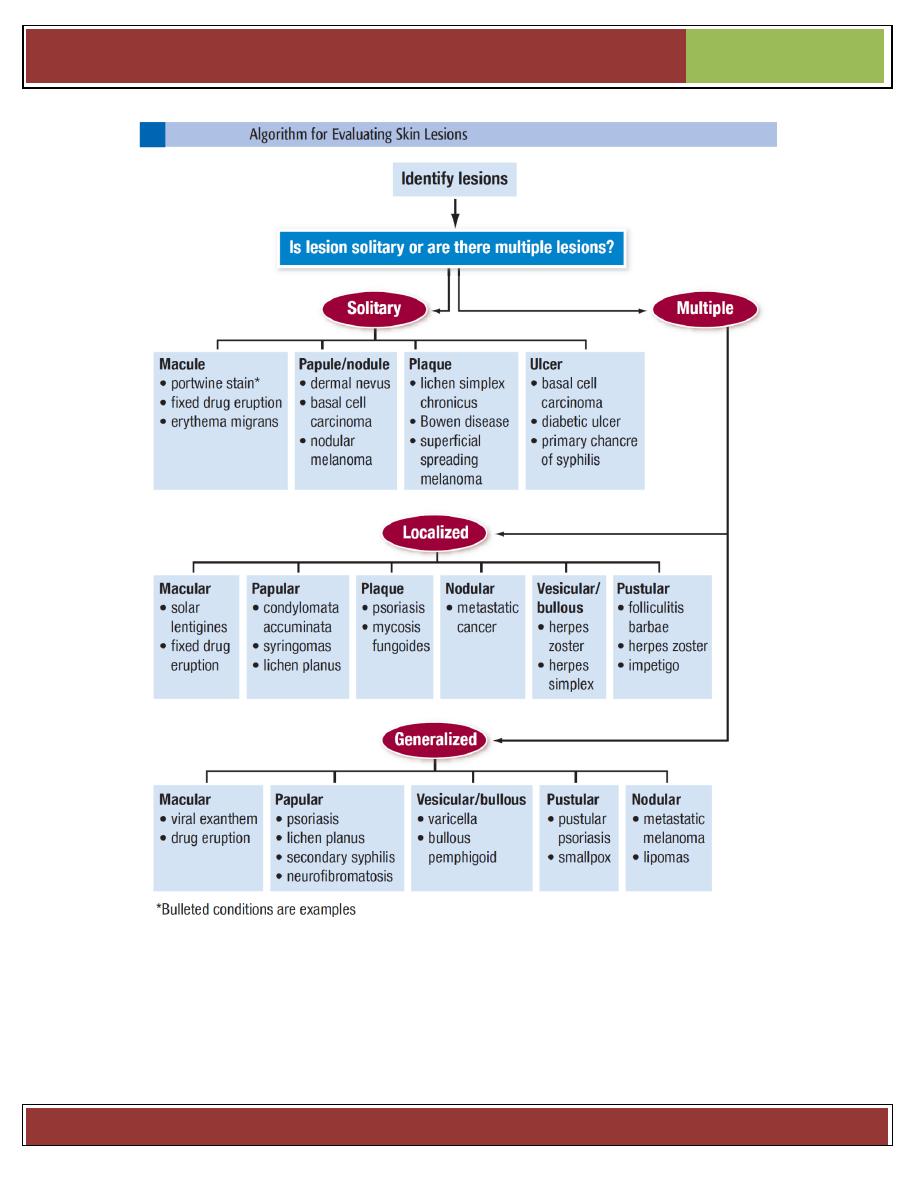
Algorithm of evaluating skin lesions
14
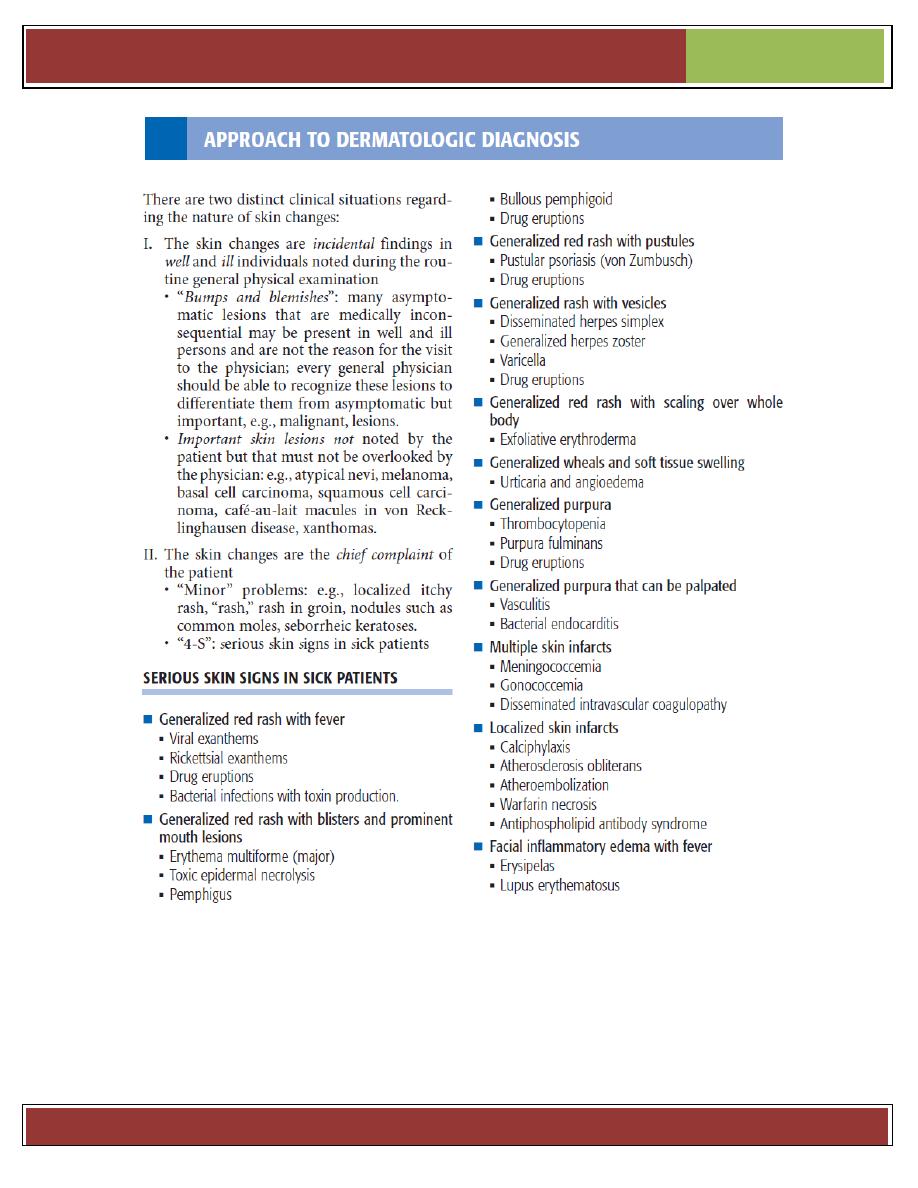
Approach to dermatological diagnosis
15
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 1
The starting point
Note basic demographics of the patient:
Age - infectious diseases are more common in children but malignancy gets more
common with advancing age.
Sex - some conditions are more common in men or more common in women.
Race and country of origin.
Current residence - important in an infectious outbreak.
Consider the lesion (History of present skin condition)
Duration:
Onset - sudden versus gradual. Establish whether this is an acute presentation or an
ongoing chronic problem.
Previous episodes - eg, photodermatoses tend to recur every spring with the onset of
good weather.
Change - fluctuation versus persistence. Consider variation in severity - eg,
occupational contact allergic dermatitis may improve when on holiday. Urticaria may be
quite dynamic in its presentation but others are much more static.
Location
As well as skin, remember mucous membranes.
Site at onset is important.
The site of lesions is important. Eczema tends to be on flexural surfaces (in adults and
older children) whilst psoriasis tends to be on extensor parts. Lesions may have a specific
distribution - around the genitals, in sweaty regions or sun-exposed areas. Establish
whether the lesion has spread.
Provoking or relieving factors
eg, heat and cold may be either aggravating or relieving factors, especially with urticaria;
repeated drug exposures with fixed drug eruptions.
Exacerbating factors
Associated symptoms:
Itch - some lesions are renowned for being itchy & others for not being so but this can be
misleading. Psoriasis is said to be non-itchy but there may be pruritus in the genital area.
Burning & Tenderness - inflammation is often tender.
Bleeding or discharge - bleeding may indicate malignancy and discharge may occur
with an infected lesion. Is the lesion
Wet, dry, blister
?
Systemic symptoms - such as pyrexia, malaise, joint pain and swelling or weight loss.
Some skin lesions are markers for underlying malignancy.
History
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 2
Response to treatment
Both patient & doctor initiated (
Topical, systemic)
. A number of treatments may have been
tried prior to consultation eg antiseptic lotions, calamine, antihistamines, over-the-counter
(OTC) steroid or antifungal creams, herbal remedies or medication prescribed for another
family member or friend. Complementary medicines such as chinese herbs may have
unknown ingredients 7 potency. Partially treated lesions are the most difficult to diagnose.
Do not forget to cover
Past medical history:
Past history of skin disorders
Past history of other medical disorders: is often relevant - eg, diabetes may suggest
necrobiosis lipoidica.
Asthma & hay fever.
Operations
Family history:
Family history of skin disorders: If positive, inherited, infection, infestation.
May indicate a familial trend for the disease. Other family members will have been given
a diagnosis. A genetic predisposition is important in many diseases, including eczema &
psoriasis. Alternatively, concurrent and recent affliction of other members of the family
suggests a contagious or environmental aetiology. Familial atypical mole and melanoma
(FAMM) syndrome should be considered where several family members have multiple
melanocytic lesions, some atypical, with at least one case of melanoma in the family.
Family history of other medical disorders.
Occupation, hobbies and pastimes:
Where there may be exposure to chemicals or a very hot environment, for example.
Travel:
Particularly to exotic locations, may increase the risk of rarer tropical diseases. Consider
cumulative exposure to sunlight or sunbeds and history of sunburn, as these increase the
risk of skin malignancies.
Drugs (
prescribed for other disorders = those taken before onset of skin disorders)
:
prescribed, over-the-counter or other therapies. Drug eruptions can be highly variable. Illegal
drug use may have dermatological manifestations - eg, anabolic steroids and acne.
Smoking and alcohol:
Alcohol use has an association with psoriasis. Smoking increases the risk of some
malignancies and has a close association with palmoplantar pustular psoriasis.
Allergies.
Psychological and social sequelae:
People with severe, chronic, visible and disfiguring skin disease may suffer from anxiety,
depression and social isolation, these issues require exploration. Psychological problems
may also cause skin disease - eg, dermatitis artefacta. See the separate article on Living
with Skin Disease.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 3
Sexual history:
This can be a tricky topic to cover but some sexually transmitted diseases are associated
with skin conditions (herpes, syphilis). Try to get a rough idea about the patient's sexual
history in order to assess their risk of an infection.
History of risk factors of HIV: blood transfusions, IV drugs, sexually active, multiple
partners, sexually transmitted disease?
Exam the skin properly, under uniform & bright lighting, undress the patient fully, a
magnifying lens is very helpful, exam the mucous membrane, hair & nails.
In general, a thorough examination of the whole skin is considered best practice but may
not be warranted - eg, diagnosis of a verruca.
Description of skin lesion
Discussed below
If the skin lesion is nodule, examination (in addition to above) includes:
Inspection
Secretion: There may be evidence of a punctum (with sebum secretion). For example,
this can help differentiate a lipoma from a sebaceous cyst.
Palpation
Surroundings
Examination around the lump may reveal associated swellings. For example, lymph
nodes, breast nodules, neurofibromatosis and lipomatosis. Examine the regional lymph
nodes or, if this lump may be a lymph node, examine its drainage area.
Examine the corresponding area on the other side of the body, as appropriate.
Structure or consistency
The lump may be solid, fluid, or gaseous.
Lumps may be described as soft and fluctuant, firm or even 'stony hard'. Fluctuation
indicates a fluid swelling and this is elicited by compression of the swelling with
displacement in two planes.
Stability
It is important to define if the lump is mobile, attached or fixed to other structures.
Move
lump in two directions, right-angled to each other. Then repeat exam when muscle contracted:
Bone: immobile.
Examination
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 4
Muscle: contraction reduces lump mobility,
for example,
breast lumps.
Subcutaneous: skin can move over lump.
Skin: moves with skin,
for example, 'peau d'orange' dimpling of the skin.
Sensation
Temperature - the skin over inflammatory lesions may be raised, red and warm (increased
blood flow).
Tenderness - inflammatory lesions are often tender to touch. Tumours are often non-tender.
Pulsatile swellings - distinguish between transmitted and expansile pulsation.
o Assess with 2 fingers on mass:
o Transmitted pulsation: both fingers pushed same direction.
o Expansile: fingers diverge (esp for AAA).
Fluctuation [fluid-containing]
Assess by placing 2 fingers in "peace sign" on either edge of lump, then tapping lump
center with index finger of other hand: fluctuant lump will displace peace sign fingers.
Very large masses can be assessed by a fluid thrill.
Sign of emptying
When compressed, the swelling diminishes in size or disappears and slowly refills when
pressure is released. For example, cavernous haemangioma, lymphangiomata & meningoceles.
Sign of indentation
On compression the lump remains indented. For example, some sebaceous cysts.
Percussion
Usually of little value in defining a mass with the exception of some abdominal swellings.
Auscultation
Sound
This would usually be detected at auscultation. For example, venous hum over a vascular
swelling. Vascular sounds may be detected. For example, a systolic murmur or 'bruit'
may be heard over large tumours, vascular goitres and arterial aneurysms.
Transillumination
This will differentiate between a solid and a fluid-filled swelling.
Find a dark room and a bright, thin 'pencil' torch and place it on the lump, from behind,
so the light is shining through the lump towards your eye. If the lump glows red it is said
to transilluminate.
Fluid-filled lumps such as hydroceles are good examples of transilluminable swellings.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 5
Lesion Type
Skin eruption is divided into (2) groups: Primary & secondary.
Primary skin lesions
Erythema: Redness caused by vascular dilatation
Macule: Small flat area of altered color or texture
Patch: Large macule > 0.5 cm in diameter
Papule: Elevated solid lesion up to 0.5 cm
Plaque: Elevated area of skin > 0.5 cm, often formed by confluence of papules
Nodule: Circumscribed, elevated, solid lesion, usually > 0.5 cm in diameter in both width
& depth. Seen top-elevated (exophytic) or palpated (endophytic). Large nodule = tumor.
Vesicle: Circumscribed, elevation of skin, < 0.5 cm in diameter & containing fluid.
Pustule: A visible accumulation of pus in the skin.
Abscess: Localized collection pf pus in cavity > 1cm in diameter
Wheal: Elevated, white, compressible evanscent area produced by dermal odema
Angioedema: Diffuse swelling caused by odema extending to the subcutaneous tissue.
Cyst: Closed cavity or sac with an epithelial lining & containing fluid or semisolid material.
Petechia: Pin-head sized macules of blood in the skin
Ecchymosis: Macular area of haemorrhage > 2 cm.
Purpura: Extravasation of blood into the skin up to 2 mm in diameter.
Haematoma: Swelling from gross bleeding
Burrow: Small tunnel in the skin that houses a parasite.
Comedon: Plug of keratin & sebum in a dilated piloseba-ceous orifice with dilated
follicular orifice. Open comedon (Black heads): follicular orifice dilated.
Closed comedon (White heads): follicular orifice narrow.
Telangiectasia: Visible dilatation of small cut blood vessel.
Secondary skin lesions
Scale: Flat plate or flake of stratum corneum
Crust: Dried serum & other exudates.
Erosion: Focal loss of epidermis, not penetrate below DEJ, heal without scarring.
Ulcer: Focal loss of epidermis, dermis, subcutaneous tissue, heal with scaring.
Fissure: Linear gap or a slit in the skin surface.
Atrophy: Depression of skin result from thinning of epidermis, dermis or subcutaneous tissue.
Scar: Is a result of healing where normal structure is permanently replaced by fibrous tissue.
Sinus: Channel that permits the escape of fluid or pus.
Description of a skin lesion
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 6
Stria (Stretch mark): Is a streak-like linear atrophic pink, purple or white lesion of the
skin caused by changes in connective tissue.
Excoriation: Loss of skin substance caused by scratching.
Lichenification: Thickened skin with exaggeration of normal skin line
Changes encountered in skin
Alopecia:
hair loss from any part of the body.
Pigmentation:
De-pigmentation: Complete loss of pigment of the skin.
Hyper-pigmentation (melanosis): Darkening of the skin due to increased melanin
activity.
Hypo-pigmentation: Lightening of the skin due to decreased melanin activity.
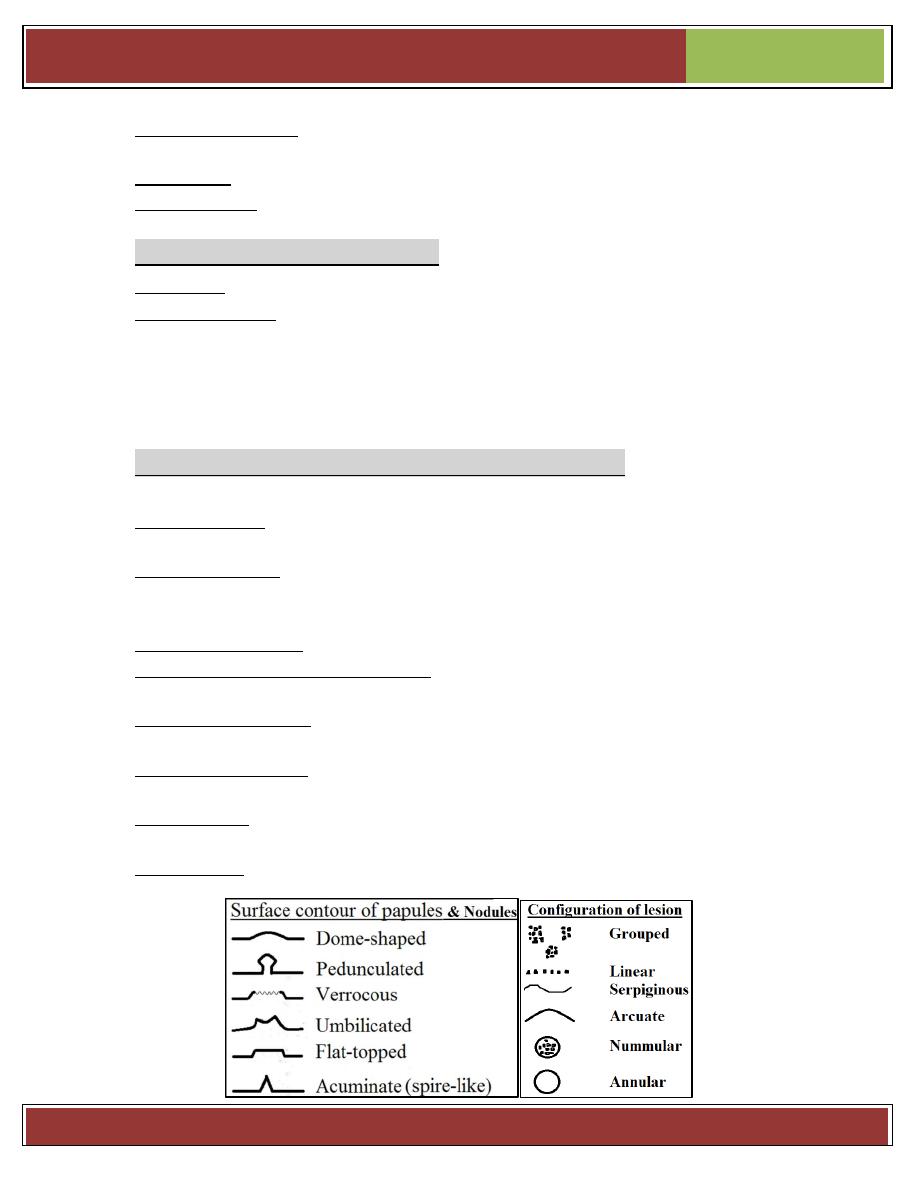
Lesion Configuration (Secondary Morphology)
Configuration is the shape of single lesions and the arrangement of clusters of lesions.
Linear lesions take on the shape of a straight line and are suggestive of some forms of
contact dermatitis, linear epidermal nevi, and lichen striatus.
Annular lesions are rings with central clearing. Examples include granuloma
annulare, some drug eruptions, some dermatophyte infections (eg, ringworm),&
secondary syphilis.
Nummular lesions are circular or coin-shaped; an example is nummular eczema.
Target (bull’s-eye or iris) lesions appear as rings with central duskiness and are
classic for erythema multiforme.
Serpiginous lesions have linear, branched, and curving elements. Examples include
some fungal and parasitic infections (eg, cutaneous larva migrans).
Reticulated lesions have a lacy or networked pattern. Examples include cutis
marmorata and livedo reticularis.
Herpetiform describes grouped papules or vesicles arranged like those of a herpes
simplex infection.
Zosteriform describes lesions clustered in a dermatomal distribution similar to herpes zoster.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 7
Texture
Some skin lesions have visible or palpable texture that suggests a diagnosis.
Verrucous lesions have an irregular, pebbly, or rough surface. Examples include
warts and seborrheic keratoses.
Lichenification is thickening of the skin with accentuation of normal skin markings; it
results from repeated scratching or rubbing.
Induration, or deep thickening of the skin, can result from edema, inflammation, or
infiltration, including by cancer. Indurated skin has a hard, resistant feeling. Induration is
characteristic of panniculitis, some skin infections, and cutaneous metastatic cancers.
Umbilicated lesions have a central indentation and are usually viral. Examples
include molluscum contagiosum and herpes simplex.
Xanthomas, which are yellowish, waxy lesions, may be idiopathic or may occur in
patients who have lipid disorders.
Define the area involving the lesion and describe the shape
of the lesion
Is the border well or poorly defined?
Look at the centre of the lesion- is it continuous with the rest of the lesion or is it
raised/depressed?
The shape of the area on the skin surface- is it round, oval or irregular?
Overall shape of the lesion- spherical, domed, pedunculated (lesion attached to
skin by a narrow stalk), flat-topped.
Location and Distribution
It is important to note whether
o Lesions are single or multiple
o Particular body parts are affected (eg, palms or soles, scalp, mucosal membranes)
o Distribution is random or patterned, symmetric or asymmetric
o Lesions are on sun-exposed or protected skin
Although few patterns are pathognomonic, some are consistent with
certain diseases.
o Psoriasis frequently affects the scalp, extensor surfaces of the elbows and knees,
umbilicus, and the gluteal cleft.
o Lichen planus frequently arises on the wrists, forearms, genitals, and lower legs.
o Vitiligo may be patchy and isolated or may group around the distal extremities and
face, particularly around the eyes and mouth.
o Chronic cutaneous lupus erythematosus has characteristic lesions on sun-exposed
skin of the face, especially the forehead, nose, and the conchal bowl of the ear.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 8
o Hidradenitis suppurativa involves skin containing a high density of apocrine glands,
including the axillae, groin, and under the breasts.
Color
Red skin (erythema) can result from many different inflammatory or infectious
diseases. Cutaneous tumors are often pink or red. Superficial vascular lesions such as
port-wine stains may appear red.
Orange skin is most often seen in hypercarotenemia, a usually benign condition of
carotene deposition after excess dietary ingestion of β-carotene.
Yellow skin is typical of jaundice, xanthelasmas & xanthomas, & pseudoxanthoma
elasticum.
Green fingernails suggest Pseudomonas aeruginosa infection.
Violet skin may result from cutaneous hemorrhage or vasculitis. Vascular lesions or
tumors, such as Kaposi sarcoma and hemangiomas, can appear purple. A lilac color of
the eyelids or heliotrope eruption is characteristic of dermatomyositis.
Shades of blue, silver, and gray can result from deposition of drugs or metals in
the skin, includingminocycline, amiodarone, and silver (argyria). Ischemic skin appears
purple to gray in color. Deep dermal nevi appear blue.
Black skin lesions may be melanocytic, including nevi and melanoma. Black eschars
are collections of dead skin that can arise from infarction, which may be caused by
infection (eg, anthrax, angioinvasive fungi including Rhizopus, meningococcemia),
calciphylaxis, arterial insufficiency, or vasculitis.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 9
Special techniques used in clinical examination
Magnification with hand lens.
To examine lesions for fine morphologic detail, it is necessary to use a magnifying glass
(hand lens) (7×) or a binocular microscope (5× to 40×). Magnification is especially
helpful in the diagnosis of lupus erythematosus (follicular plugging), lichen planus
(Wickham striae), basal cell carcinomas (translucence and telangiectasia), and melanoma
(subtle changes in color, especially gray or blue); this is best visualized after application
of a drop of mineral oil.
Oblique lighting of the skin lesion,
Done in a darkened room, is often required to detect slight degrees of elevation or
depression, and it is useful in the visualization of the surface configuration of lesions and
in estimating the extent of the eruption.
Subdued lighting
In the examining room enhances the contrast between circumscribed hypopigmented or
hyperpigmented lesions and normal skin.
Wood’s lamp (ultraviolet long-wave light, “black” light):
Emitting long wave length intra violet radiation through wood’s (nickel oxide) filter is an
important investigation tool in diagnosis & treatment.
Useful in the following conditions
1) Fungal infection [tinea capitis & tinea versicolor (yellow fluorescence)]
2) Bacterial infection (pseudomonas & erythrasma)
3) Genodermatosis (porpheria & tuberous sclerosis)
4) Malignancy (squamous cell carcinoma)
5) Pigmentary disorder (vitiligo & melasma)
6) Drugs [tetracycline (teeth), mepacrine (nail)]
With the Wood lamp (365 nm), fluorescent pigments and subtle color differences of
melanin pigmentation can be visualized; the Wood lamp also helps to estimate
variation in the lightness of lesions in relation to the normal skin color in both dark-
skinned and fair-skinned persons; e.g., the lesions seen in tuberous sclerosis and tinea
versicolor are hypomelanotic and are not as white as the lesions seen in vitiligo, which
are amelanotic. Circumscribed hypermelanosis, such as a freckle and melasma, is much
more evident (darker) under the Wood lamp. By contrast, dermal melanin, as in a
Mongolian sacral spot, does not become accentuated under the Wood lamp. Therefore, it
Special clinical & laboratory aids to
dermatologic diagnosis
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 10
is possible to localize the site of melanin by use of the Wood lamp; however, this is
more difficult or not possible in patients with brown or black skin.
Wood lamp is particularly useful in the detection of the fluorescence of dermatophytosis
in the hair shaft (green to yellow) and of erythrasma (coral red). A presumptive diagnosis
of porphyria can be made if a pinkish-red fluorescence is demonstrated in urine examined
with the Wood lamp; addition of dilute hydrochloric acid intensifies the fluorescence.
Diascopy
Consists of firmly pressing a microscopic slide or a glass spatula over a skin lesion.
It is used to blanch vascular lesion to unmask their underlying color. The examiner will
find this procedure of special value in determining whether the red color of a macule or
papule is due to capillary dilatation (erythema) or to extravasation of blood (purpura) that
does not blanch.
Diascopy is also useful for the detection of the glassy yellowbrown appearance of
papules in sarcoidosis, tuberculosis of the skin, lymphoma, and granuloma annulare.
Also used to detect granulomatous nodule in lupus vulgaris.
Dermoscopy (also called epiluminescence microscopy).
A hand lens with built-in lighting and a magnification of 10× to 30× is called a
dermatoscope and permits the noninvasive inspection of deeper layers of the epidermis
and beyond. This is particularly useful in the distinction of benign and malignant growth
patterns in pigmented lesions in vivo especially malignant melanoma.
Digital dermoscopy is particularly useful in the monitoring of pigmented skin lesions
because images are stored electronically and can be retrieved and examined at a later date
to permit comparison quantitatively and qualitatively and to detect changes over time.
Digital dermoscopy uses computer image analysis programs that provide
(1) Objective measurements of changes;
(2) Rapid storage, retrieval, and transmission of images to experts for further discussion
(teledermatology); and
(3) Extraction of morphologic features for numerical analysis. Dermoscopy and digital
dermoscopy require special training.
Clinical Signs
Dermatographism
is the appearance of an urticarial wheal after focal pressure (eg,
stroking or scratching the skin) in the distribution of the pressure. Up to 5% of normal
patients may exhibit this sign, which is a form of physical urticaria.
Darier sign
refers to rapid swelling of a lesion when stroked. It occurs in patients
with urticaria pigmentosa or mastocytosis. In other term, Darier sign is “positive” when a
brown macular or a slightly papular lesion of urticaria pigmentosa (mastocytosis)
becomes a palpable wheal after being vigorously rubbed with an instrument such as the
blunt end of a pen. The wheal may not appear for 5–10 min.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 11
Nikolsky sign
is epidermal shearing that occurs with gentle lateral pressure on
seemingly uninvolved skin in patients with toxic epidermal necrolysis and some
autoimmune bullous diseases. In other term, The Nikolsky phenomenon is positive when
the epidermis is dislodged from the dermis by lateral, shearing pressure with a finger,
resulting
in an erosion. It is an important diagnostic sign in acantholytic disorders such as
pemphigus or the staphylococcal scalded skin (SSS) syndrome or other blistering or
epidermonecrotic disorders, such as toxic epidermal necrolysis.
Auspitz sign
is “positive” when slight scratching or curetting of a scaly lesion reveals
punctate bleeding points within the lesion. This suggests psoriasis, but it is not specific.
Koebner (Isomorphic) phenomenon
describes the development of lesions
within areas of trauma (eg, caused by scratching, rubbing, or injury). It is seen in:
Psoriasis, warts, lichen planus, vitiligo, acute eczema, molloscum contagiosum.
Clinical Tests
Patch test:
Used to detect allergens responsible for allergic contact dermatitis. (A.C.D.)
Patch testing is used to document and validate a diagnosis of allergic contact
sensitization and identify the causative agent. Substances to be tested are applied to the
skin in shallow cups (Finn chambers), affixed with a tape and left in place for 24–48 h.
Contact hypersensitivity will show as a papular vesicular reaction that develops within
48–72 h when the test is read. It is a unique means of in vivo reproduction of disease in
diminutive proportions, for sensitization affects all the skin and may therefore be elicited
at any cutaneous site. The patch test is easier and safer than a “use test” with a
questionable allergen, for test items can be applied in low concentrations in small areas of
skin for short periods of time (see Section 2).
Photopatch testing
is a combination of patch testing and UV irradiation of the test site and is used to
document photoallergy.
Prick testing
is used to determine type I allergies (immediate hypersensitivity reaction type I). A drop
of a solution containing a minute concentration of the allergen is placed on the skin and
the skin is pierced through this drop with a needle. Piercing should not go beyond the
papillary body. A positive reaction will appear as a wheal within 20 min. The patient has
to be under observation for possible anaphylaxis.
Acetowhitening
facilitates detection of subclinical penile or vulvar warts. Gauze saturated with 5% acetic
acid (white vinegar) is wrapped around the glans penis or used on the cervix and anus.
After 5–10 min, the penis or vulva is inspected with a 10× hand lens. Warts appear as
small white papules.
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 12
Laboratory tests
Microscopic Examination of Scales, Crusts, Serum, and Hair
1) Gram stains of smears and cultures of exudates and of tissue minces
Should be made in lesions suspected of being bacterial or yeast (Candida albicans)
infections. Ulcers and nodules require a scalpel biopsy in which a wedge of tissue
consisting of all three layers of skin is obtained; the biopsy specimen is divided into one-
half for histopathology and one-half for culture. This is minced in a sterile mortar and
then cultured for bacteria (including typical and atypical mycobacteria) and fungi.
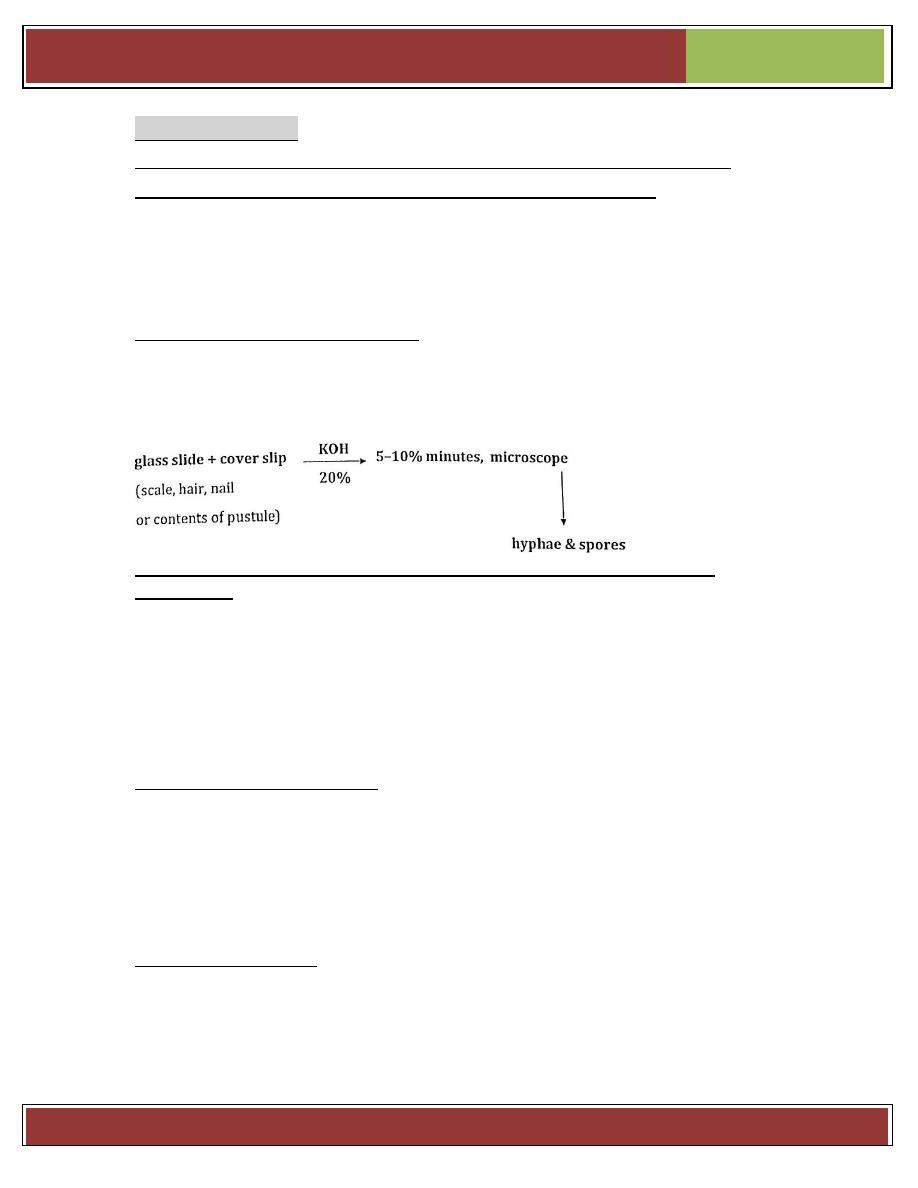
2) Microscopic examination for mycelia should be made of the roofs of vesicles or of
scales (the advancing borders are preferable) or of the hair in dermatophytoses. The tissue
is cleared with 10–30% KOH and warmed gently. Hyphae and spores will light up by
their birefringence (Fig. 25-1). Fungal cultures with Sabouraud medium should be made.
Potassium hydroxide preparation for diagnosis of fungal infection:
3) Microscopic examination of cells obtained from the base of vesicles (Tzanck
preparation) may reveal the presence of acantholytic cells in the acantholytic diseases
(e.g., pemphigus or SSS syndrome) or of giant epithelial cells and multinucleated giant
cells (containing 10–12 nuclei) in herpes simplex, herpes zoster, and varicella.
Material from the base of a vesicle obtained by gentle curettage with a scalpel is smeared
on a glass slide, stained with either Giemsa or Wright stain or methylene blue, and
examined to determine whether there are acantholytic or giant epithelial cells, which are
diagnostic (Fig. 27-27). In addition, culture, immunofluorescence tests, or polymerase
chain reaction for herpes have to be ordered.
4) Laboratory diagnosis of scabies. The diagnosis is established by identification of the
mite, or ova or feces, in skin scrapings removed from the papules or burrows. Using a
sterile scalpel blade on which a drop of sterile mineral oil has been placed, apply oil to
the surface of the burrow or papule. Scrape the papule or burrow vigorously to remove
the entire top of the papule; tiny flecks of blood will appear in the oil. Transfer the oil to a
microscopic slide and examine for mites, ova, and feces. The mites are 0.2–0.4 mm in
size and have four pairs of legs.
Biopsy of the Skin
Biopsy of the skin is one of the simplest, most rewarding diagnostic techniques because
of the easy accessibility of the skin and the variety of techniques for study of the excised
specimen (e.g., histopathology, immunopathology, polymerase chain reaction, electron
microscopy).
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 13
Selection of the site of the biopsy is based primarily on the stage of the eruption, and
early lesions are usually more typical; this is especially important in vesiculobullous
eruptions (e.g., pemphigus, herpes simplex), in which the lesion should be no more than
24 h old. However
,
older lesions (2–6 weeks) are often more characteristic
in discoid
lupus erythematosus.
Types of biopsy
a. Incisional: part of the lesion is removed.
b. Excisional: whole lesion is removed → diagnostic & therapeutic.
c. Punch biopsy.
A common technique for diagnostic biopsy is
the use of a 3- to 4-mm punch, a small
tubular
knife much like a corkscrew, which by rotating
movements between the thumb
and index
finger cuts through the epidermis, dermis, and
subcutaneous tissue; the base is
cut off with
scissors. If immunofluorescence is indicated
(e.g., as in bullous diseases or
lupus erythematosus),
a special medium for transport to the
laboratory is required.
For nodules, however, a large wedge should
be removed by excision including
subcutaneous
tissue. Furthermore, when indicated, lesions
should be bisected, one-half
for histology &
the other half sent in a sterile container for
bacterial & fungal cultures or
in special fixatives
or cell culture media, or frozen for immunopathologic
examination.
Specimens for light microscopy should be fixed immediately in buffered neutral
formalin. A brief but detailed summary of the clinical history and description of the
lesions should accompany the specimen.
Biopsy is indicated in all skin lesions that are suspected of being neoplasms, in all
bullous disorders with immunofluorescence used simultaneously, and in all dermatologic
disorders in which a specific diagnosis is not possible by clinical examination alone.
Other laboratory tests
1) Assays of blood, serum & urine (serological & non-serological test for syphilis).
2) Immunofluorescence & immune-histological examinations.
3) Radiography, ultrasonography
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 14
OUTLINE OF DERMATOLOGIC DIAGNOSIS
2015-2016
Page 15
