FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
ABCs of Head CT Interpretation in the Emergency Department:
CT Interpretation Workshop Guide
Heather M. Prendergast, MD, MPH, FACEP
Associate Professor
Department of Emergency Medicine
University of Illinois at Chicago
I. Course Description: This session will provide medical students with a skill
set to improve their ability to interpret Head CTs. To start the session, the
physics of CT scanning will be briefly reviewed. We will move quickly
into a review of normal neuroanatomy and CT appearance, followed by a
detailed review of the role of Head CT in the management of various
neurological emergencies. The diagnoses covered will include traumatic
injuries, such as epidural and subdural hematoma, skull fracture, and
contusion, and non-traumatic conditions such as stroke, subarachnoid
hemorrhage, and hydrocephalus. Tools to avoid errors of interpretation
will be discussed
.
II. Course Objectives: Upon completion of this course, participants will be
able to:
1. Discuss the physics that apply to CT scanning, including Hounsfield
numbers, windows, and frequent sources of scan artifact such as volume
averaging.
2. Describe the CT appearance of normal brain anatomy.
3. Be able to identify the pathologic conditions found on cranial CT
commonly encountered in the Emergency Department.

FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
III. Introduction: The cranial computed tomography (CT) has assumed a
critical role in the practice of emergency medicine for the evaluation of
neurological emergencies, both traumatic and atraumatic. Despite the
immediate importance for emergency physicians to recognize intracranial
emergencies on head CT, few receive formalized training in this area during
medical school or residency.
History of CT: In 1970, Sir Jeffrey Hounsfield combined a mathematical
reconstruction formula with a rotating apparatus that could both produce and
detect xrays, producing a prototype for the modern-day CT scanner. For this
work he received both a Nobel Prize and a knighthood.
IV.
X-Ray Physics: The most fundamental principle behind radiography of
any kind is the following statement: X-rays are absorbed to different
degrees by different tissues. Dense tissues, such as bone, absorb the
most x-rays, and hence allow the fewest through the body part being
studied to the film or detector opposite. Conversely, tissues with low
density (air/fat), absorb almost none of the x-rays, allowing most to pass
through to a film or detector opposite.
Conventional radiographs: Conventional radiographs are two-dimensional
images of three-dimensional structures, as they rely on a summation of
tissue densities penetrated by x-rays as they pass through the body. Denser
objects, because they tend to absorb more x-rays, can obscure or attenuate
less dense objects. Also subject to x-ray beam scatter which further blurs or
obscures low-density objects.
Computed tomography: As opposed to conventional x-rays, with CT
scanning an xray source and detector, situated 180o across from each other,
move 360o around the patient, continuously sending and detecting
information on the attenuation of x-rays as they pass through the body. Very
thin x-ray beams are utilized, which minimizes the degree of scatter or
blurring. Finally, a computer manipulates and integrates the
acquired data and assigns numerical values based on the subtle differences in
x-ray attenuation. Based on these values, a gray-scale axial image is
generated that can distinguish between objects with even small differences
in density.
Pixels: (Picture element) Each scan slice is composed of a large number of
pixels which represent the scanned volume of tissue. The pixel is the
scanned area on the x and y axis of a given thickness.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
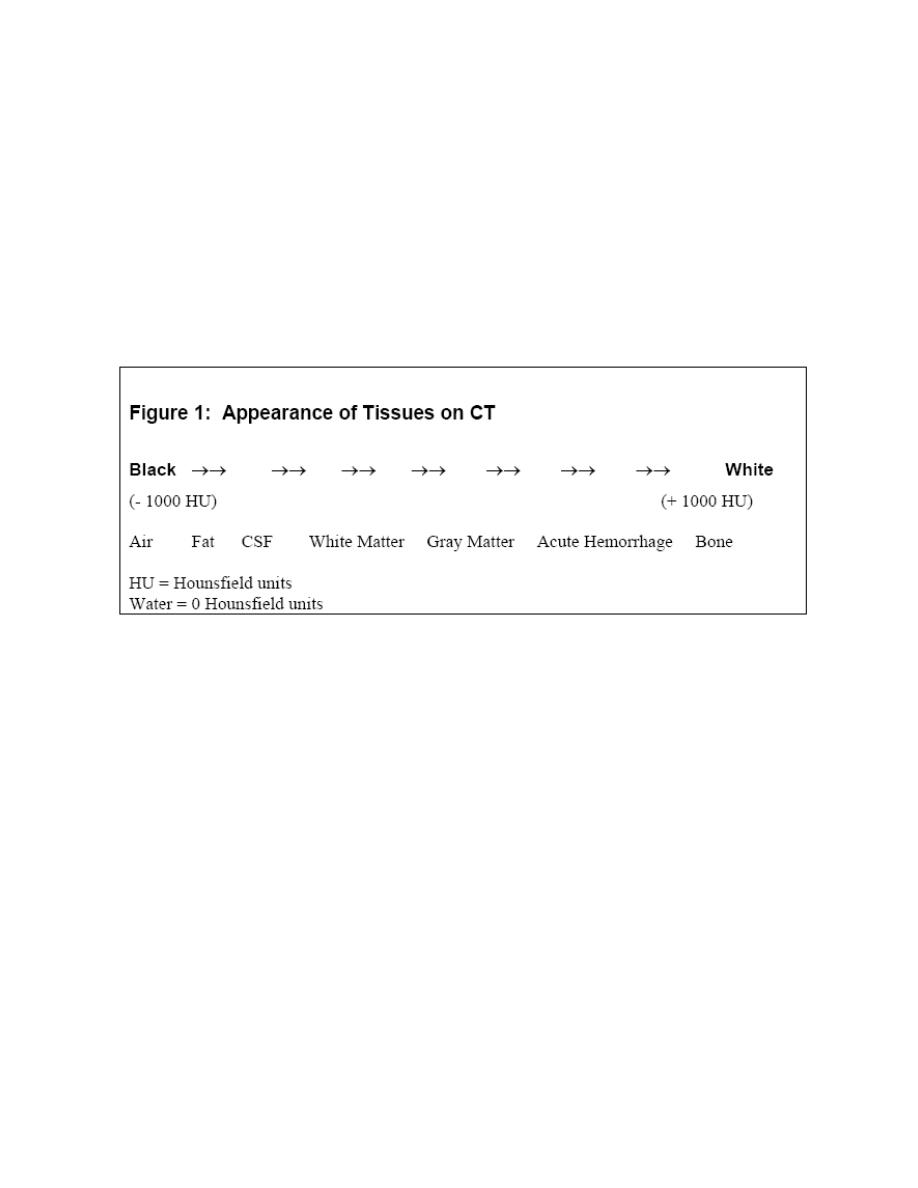
Attenuation coefficient: The tissue contained within each pixel absorbs a
certain proportion of the x-rays that pass through it (e.g. bone absorbs a lot,
air almost none).This ability to block x-rays as they pass through a substance
is known as “attenuation”. For a given body tissue, the amount of
attenuation is relatively constant, and is known as that tissue’s “attenuation
coefficient”. In CT scanning, these attenuation coefficients are mapped to an
arbitrary scale between –1000 (air) and +1000 (bone). (See Figure 1 below)
The Hounsfield numbers define the characteristics of the tissue contained within
each pixel, and are represented by an assigned portion of the gray-scale.
Windowing: Windowing allows the CT reader to focus on certain tissues on
a CT scan that fall within set parameters. Tissues of interest can be assigned
the full range of blacks and whites, rather than a narrow portion of the gray-
scale. With this technique, subtle differences in tissue densities can be
maximized.

FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
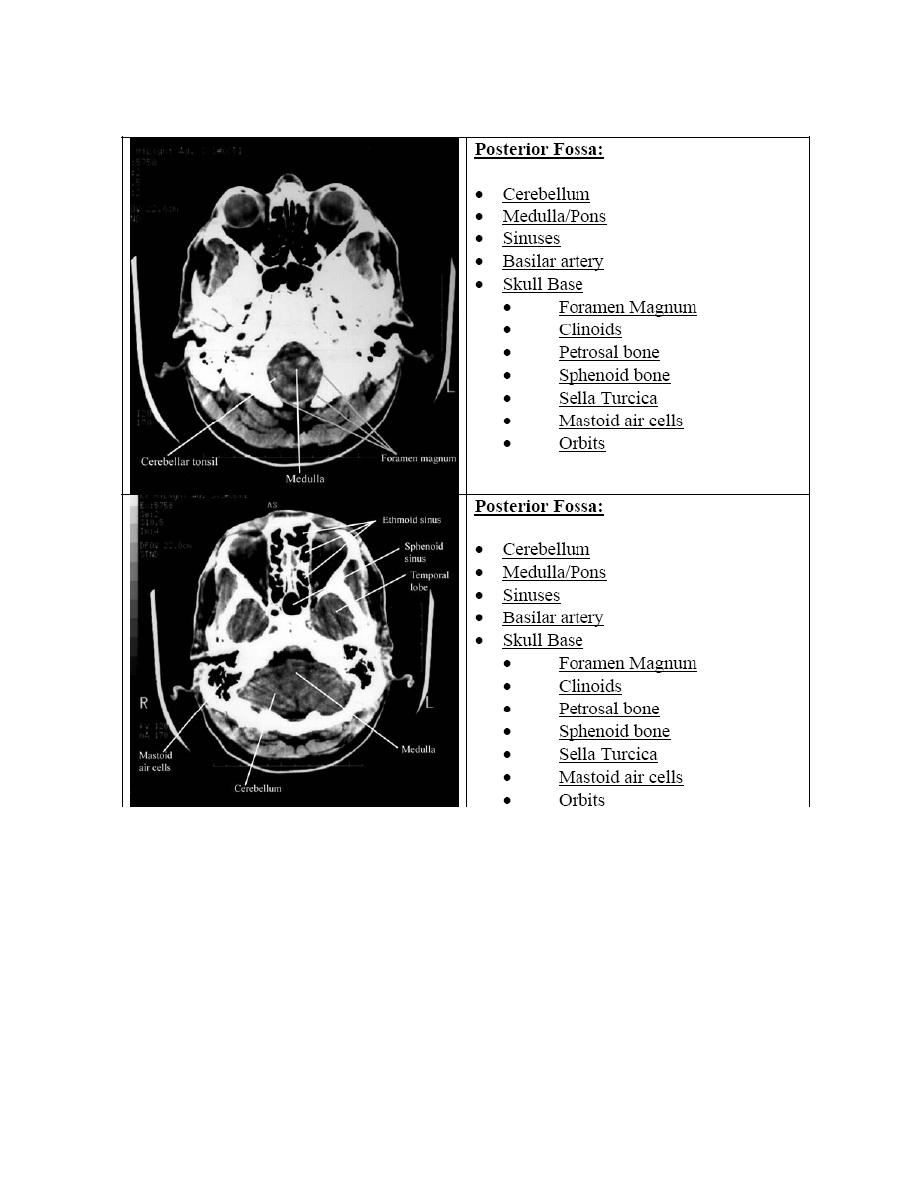
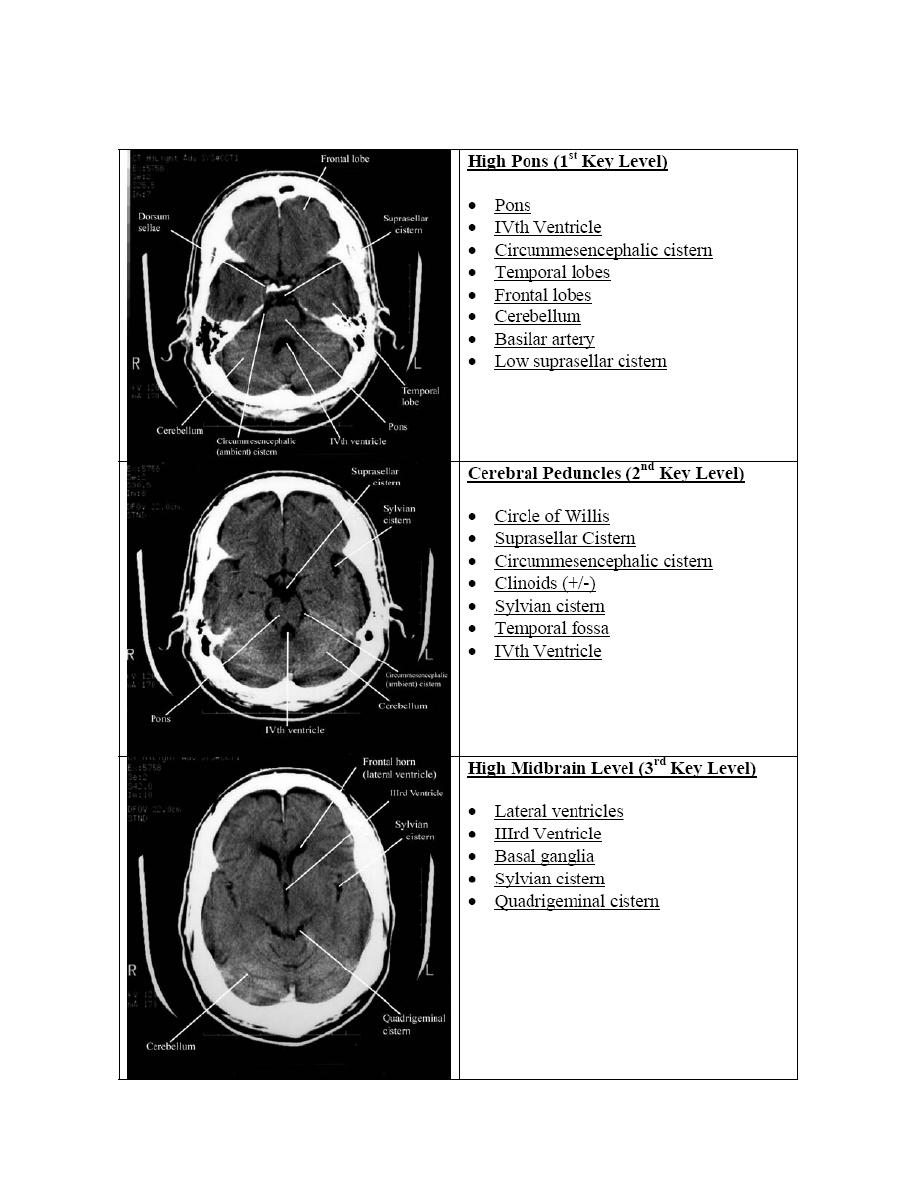
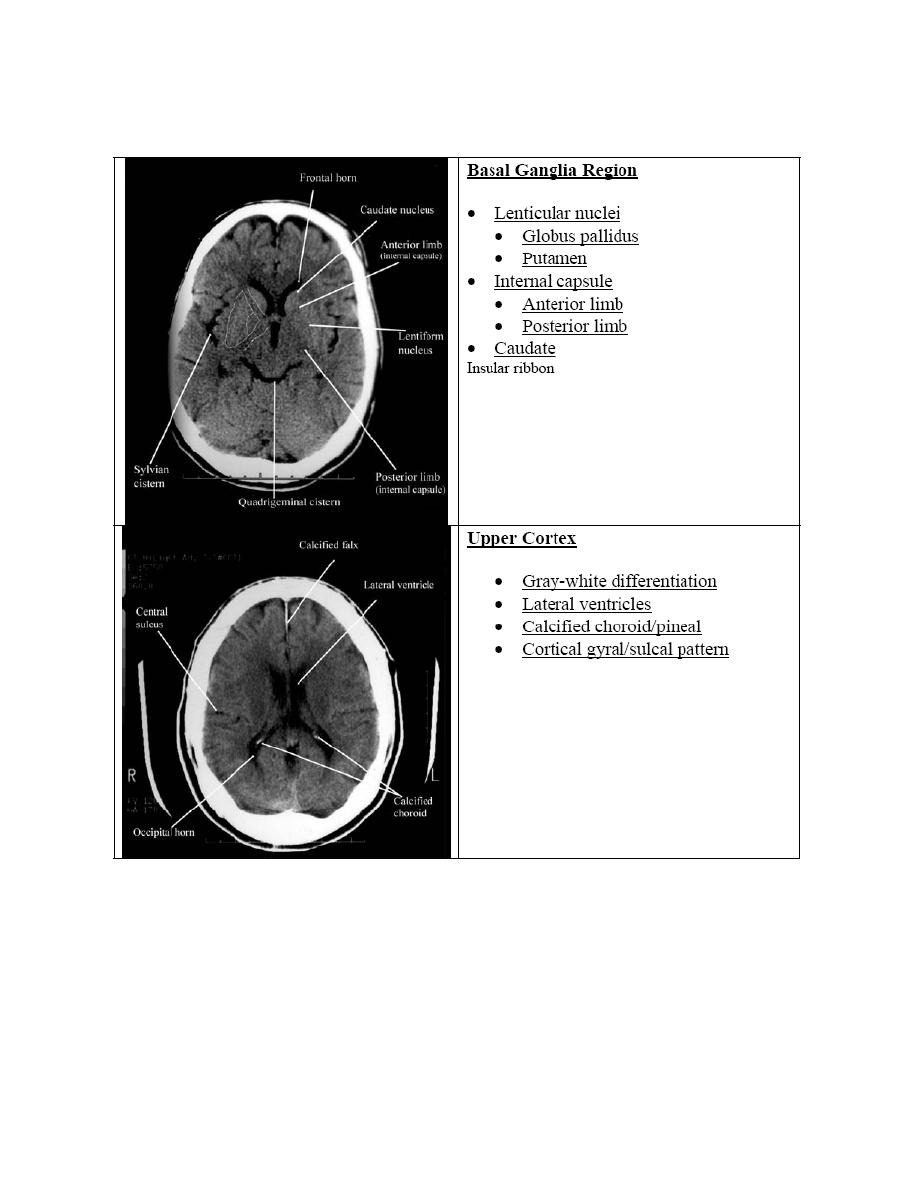
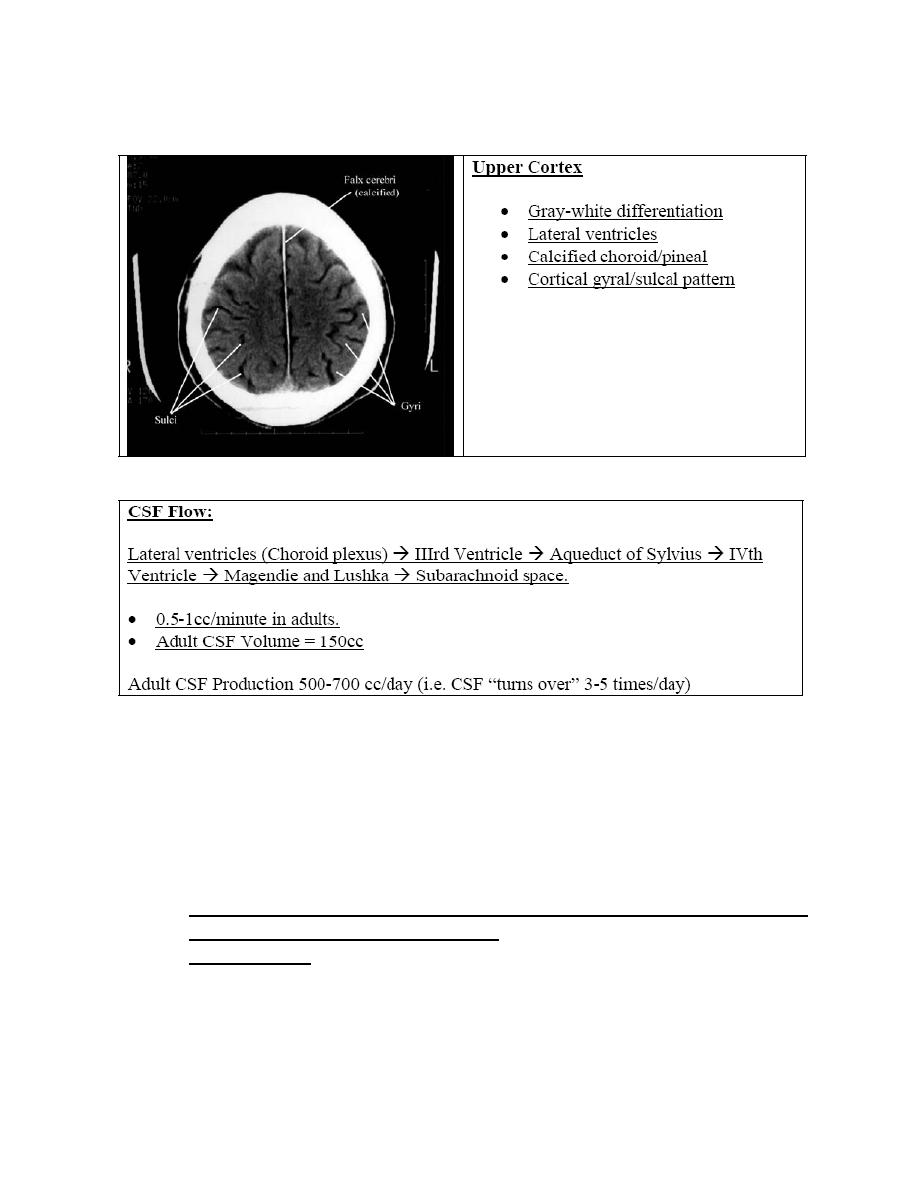
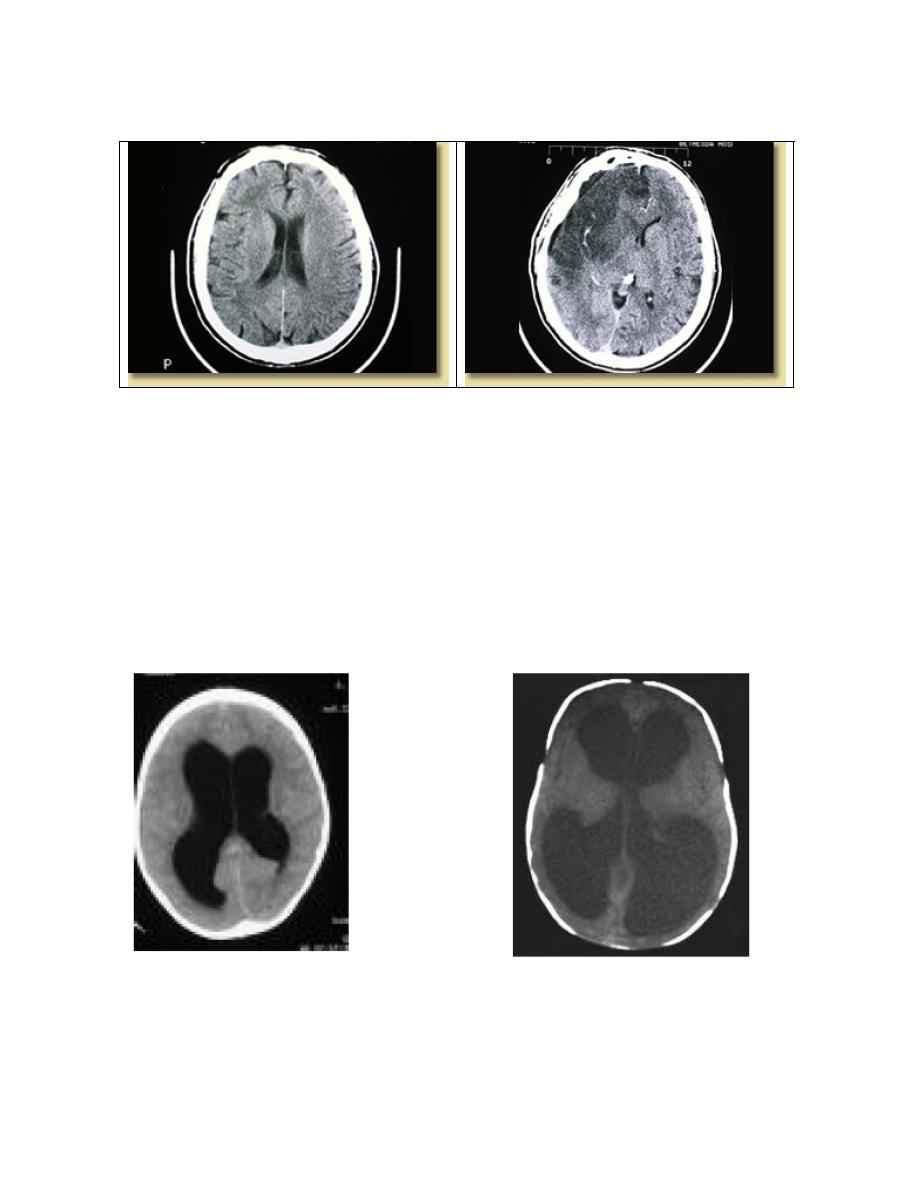
V. Normal Neuroanatomy as seen on Head CT:
As with x-ray interpretation of any body part, a working knowledge of
normal anatomic structures and location is fundamental to the clinician’s
ability to detect pathologic variants. Cranial CT interpretation is no
exception. Paramount in head CT interpretation is familiarity with the
various structures (from parenchymal areas such as basal ganglia) to
vasculature, cisterns and ventricles. Finally knowing neurologic functional
regions of the brain help when correlating CT with physical examination
findings. Our goal is not to be a neuroradiologist, but to be familiar with a
relatively few structures, regions, and expected findings will allow for
sufficient interpretation of most head CT scans by the emergency physician.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
VI.
Neurological Emergencies
Building on the first portion of the workshop, we will look at the most
common traumatic and atraumatic pathological processes that are found
on emergent cranial CT scans.
Utilizing a systematic approach is one way that the clinician can ensure
that significant neuropathology will
not be missed.
Just as physicians are taught a uniform, consistent approach to reading an
ECG(rate, rhythm, axis, etc.), the cranial CT can also be broken down
into discreet entities, attention to which will help avoid the pitfall of a

FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
missed diagnosis. One suggested mechanism to employ in avoiding a
missed diagnosis is using the mnemonic
“Blood Can Be Very Bad”. In this mnemonic, the first letter of each
word prompts the clinician to search a certain portion of the cranial CT
for pathology: Blood = blood, Can =cisterns, Be = brain, Very =
ventricles, Bad = bone.
Use the entire mnemonic when examining a cranial CT scan, as the presence
of one pathological state does not rule out the presence of another one.
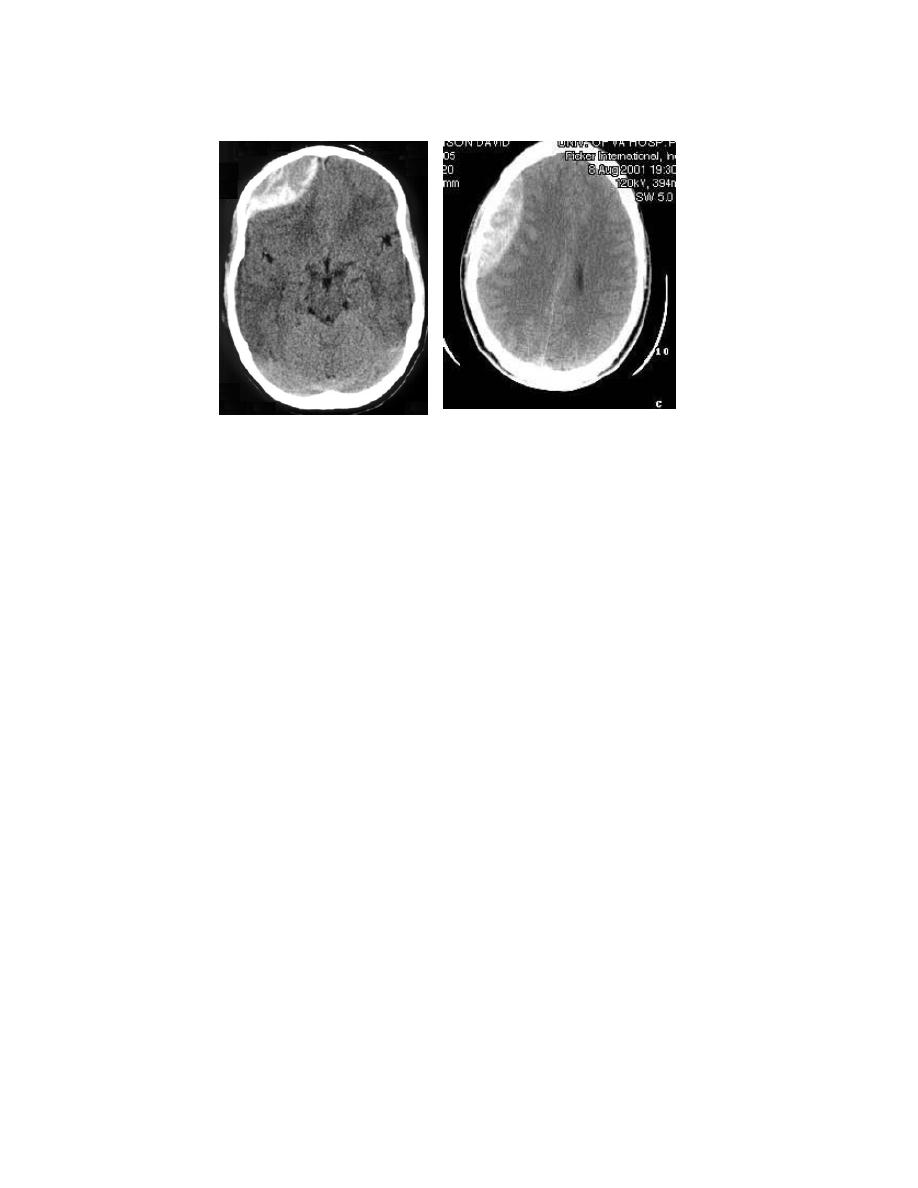
Blood- Acute hemorrhage will appear hyperdense (bright white) on
Head CT. This is attributed to the fact that the globin molecule is relatively
dense, and hence effectively absorbs x-ray beams. Acute blood is typically
in the range of 50-100 Hounsfield units.
As the blood becomes older and the globin molecule breaks down, it will
lose this hyperdense appearance, beginning at the periphery and working
centrally. On CT blood will 1st become isodense with the brain (4 days to 2
weeks, depending on clot size), and finally darker than brain (>2-3 weeks).
The precise localization of the blood is as important as identifying its
presence.
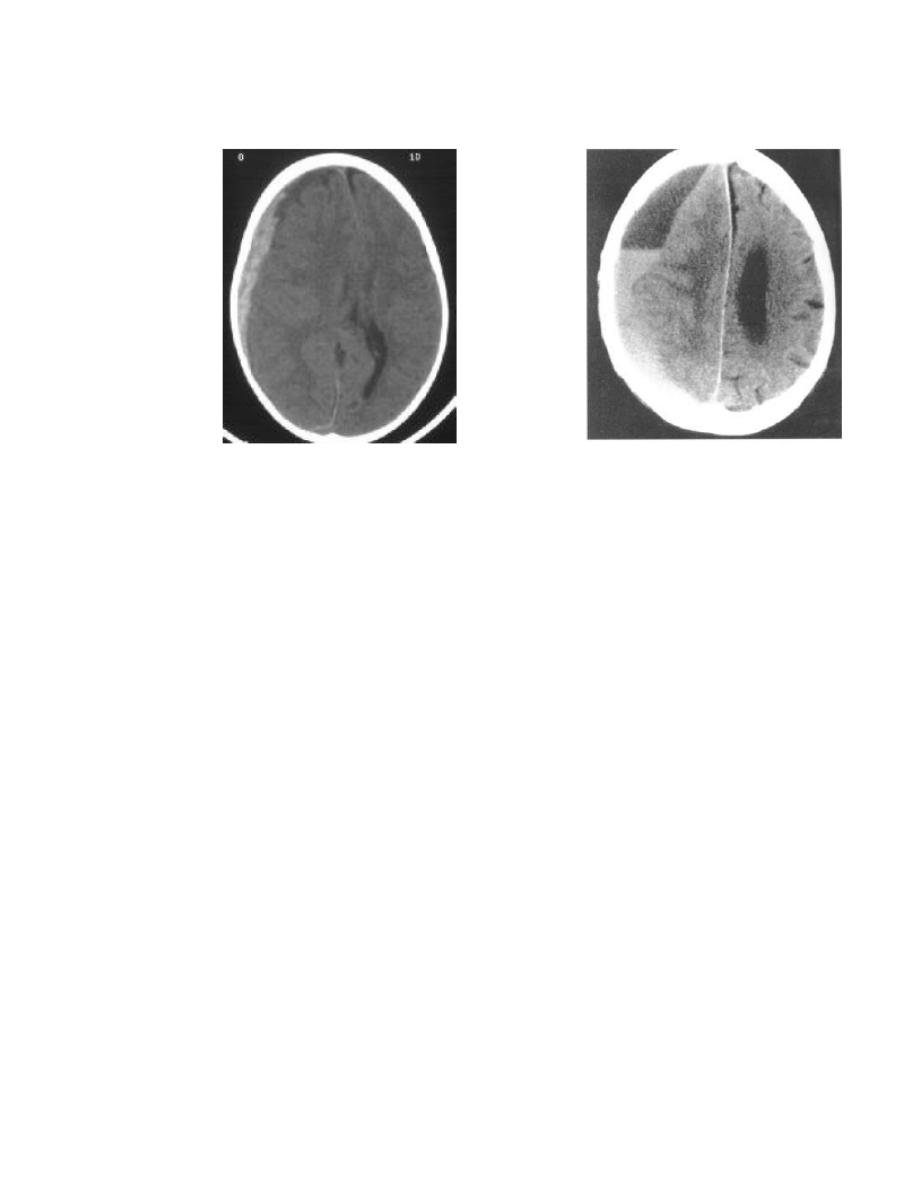
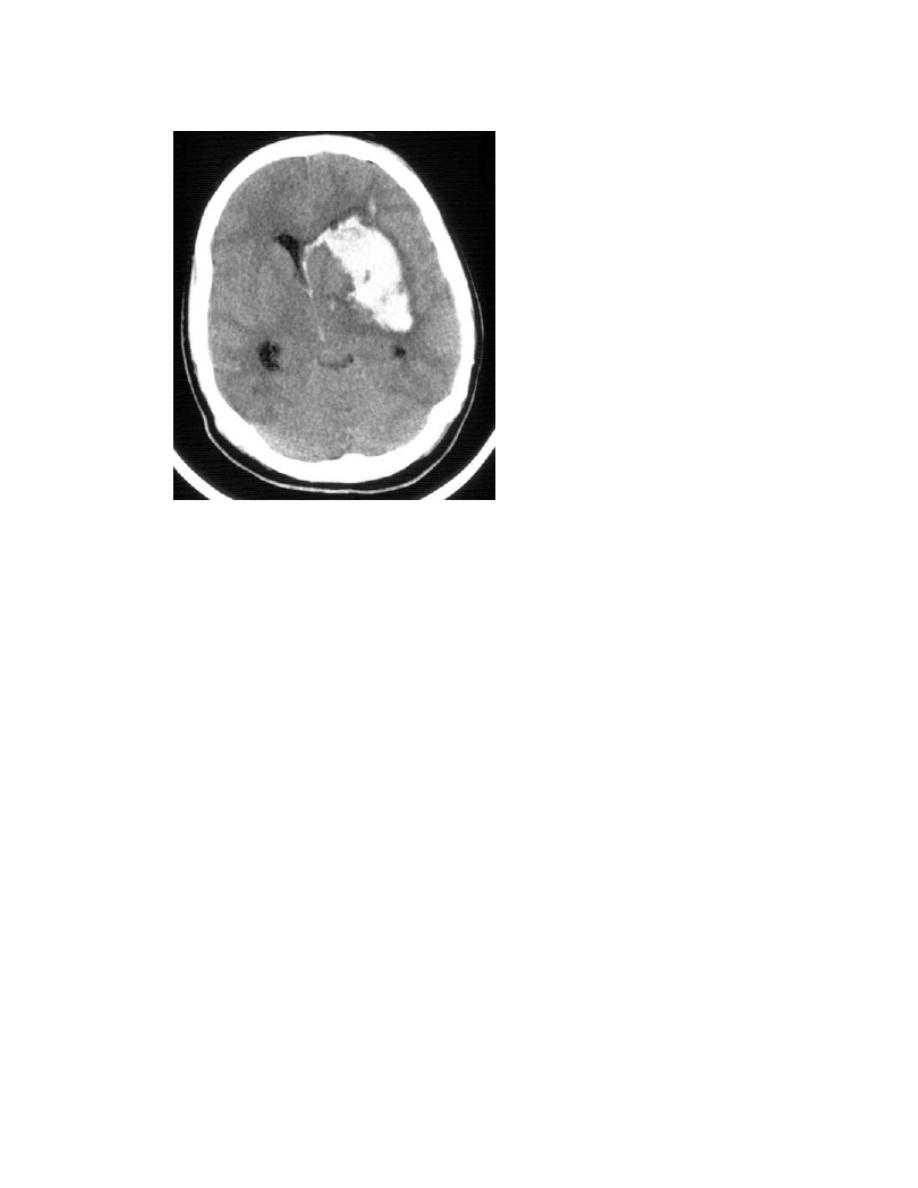
1. Epidural hematoma (EDH)-
Most frequently, a lens shaped (biconvex) collection of blood, usually
over the brain convexity. EDH never crosses a suture line. Primarily
(85%) from arterial laceration due to a direct blow, with middle
meningeal artery the most common source. A small proportion can be
venous in origin. With early surgical therapy, mortality of <20% can
be expected.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
2. Subdural hematoma (SDH)-
Sickle or crescent shaped collection of blood, usually over the
convexity. Can also be interhemispheric or along the tentorium.
SDH will cross suture lines. Subdural hematoma can be either an
acute lesion, or a chronic one. While both are primarily from venous
disruption of surface and/or bridging vessels, the magnitude of impact
damage is usually much higher in acute SDH. Acute SDH is
frequently accompanied by severe brain injury, contributing
to its poor prognosis. With acute SDH, overall significant morbidity
and mortality can approach 60-80% primarily due to the tremendous
impact forces involved (with the above mentioned damage to
underlying parenchyma). Chronic SDH, in distinction to acute SDH,
usually follows a more benign course. Attributed to slow venous
oozing after even a minor CHI, the clot can gradually accumulate,
allowing the patient to compensate. As the clot is frequently encased
in a fragile vascular membrane, these patients are at risk of re-
bleeding with additional minor trauma. The CT appearance of a
chronic SDH depends on the length of time since the bleed .
Subdurals that are isodense with brain can be very difficult to detect
on CT, and in these cases contrast may highlight the
surrounding vascular membrane.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
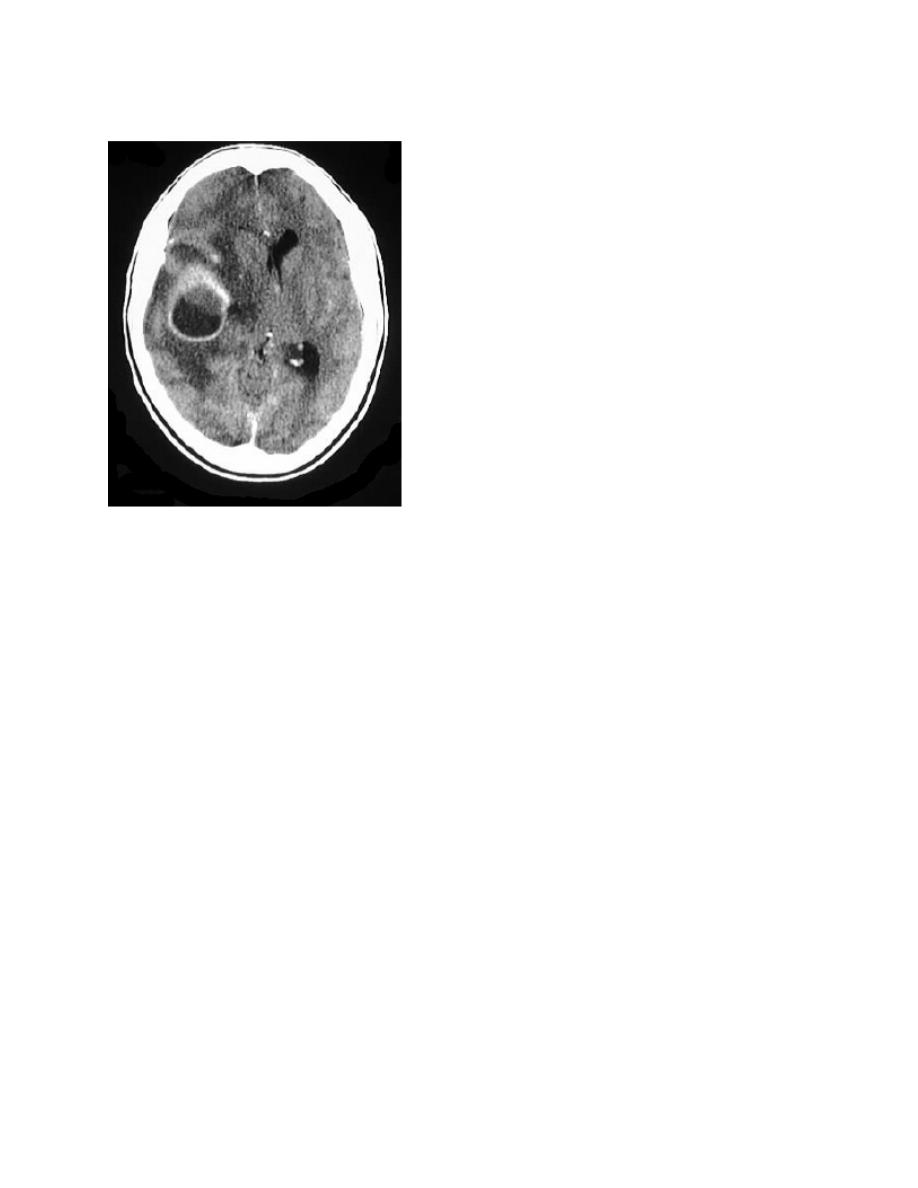
3. Intraparenchymal hemorrhage (aka Intracerebral hemorrhage ICH)–
Cranial CT will reliably identify intracerebral hematomas as small as 5 mm.
These appear as high-density areas on CT, usually with much less mass
effect than their apparent size would dictate.
Nontraumatic lesions due to hypertensive disease are typically seen in
elderly patients and occur most frequently in the basal ganglia region.
Hemorrhage from such lesions may rupture into the ventricular space, with
the additional finding of intraventricular hemorrhage on CT. Hemorrhage
from amyloid angiopathy is frequently seen as a cortical based wedge-
shaped bleed with the apex pointed medially. Posterior fossa bleeds (e.g.
cerebellar ) may dissect into the brainstem (pons, cerebellar peduncles) or
rupture into the fourth ventricle.Traumatic intracerebral hemorrhages may be
seen immediately following an injury. Contusions may enlarge and coalesce
over first 2-4 days. Most commonly occur in areas where sudden
deceleration of the head causes the brain to impact on bony prominences
(temporal, frontal, occipital poles).
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
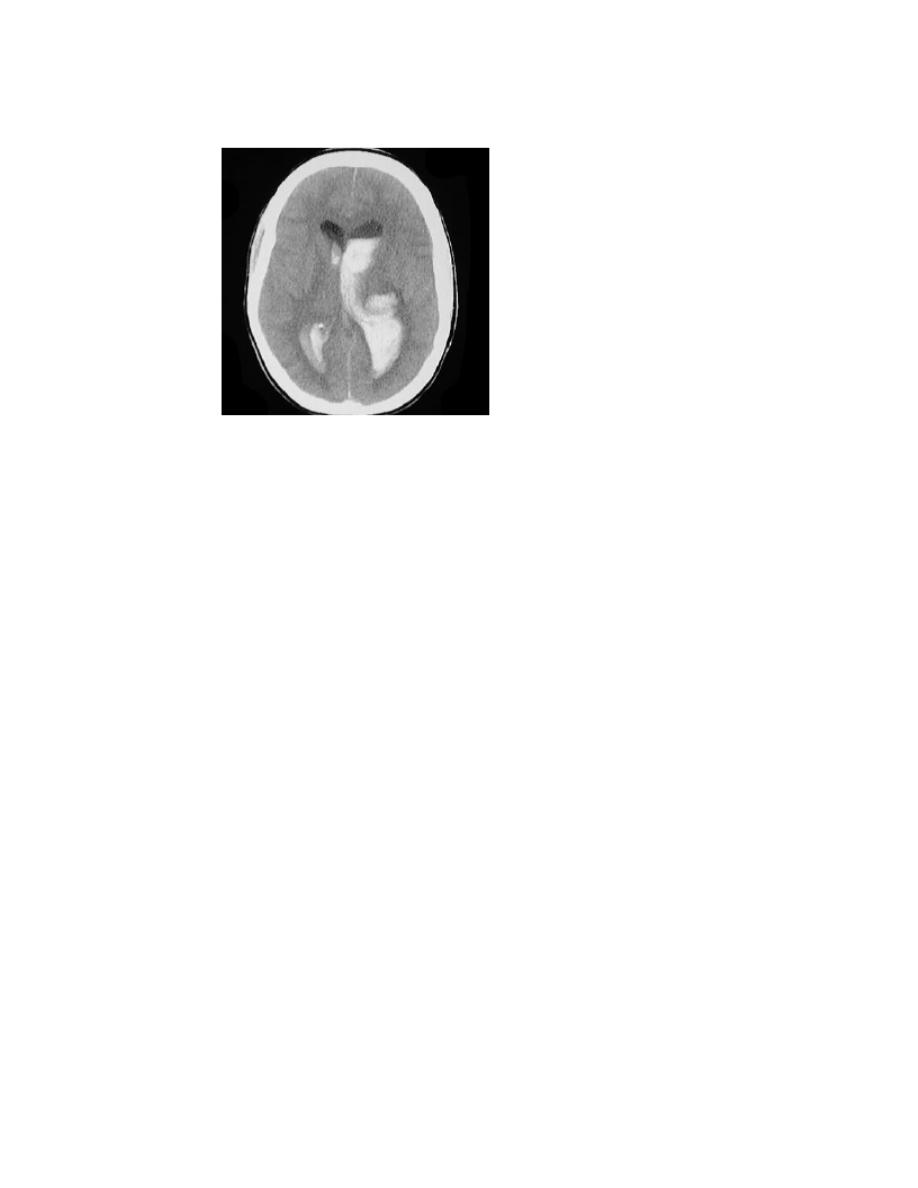
4. Intraventricular hemorrhage (IVH)-
can be traumatic, secondary to IPH with ventricular rupture, or from
subarachnoid hemorrhage with ventricular rupture
(especially PICA aneurysms). IVH is present in 10% of severe head
trauma. Associated with poor outcome in trauma (may be marker as
opposed to causative). Hydrocephalus may result regardless of
etiology.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
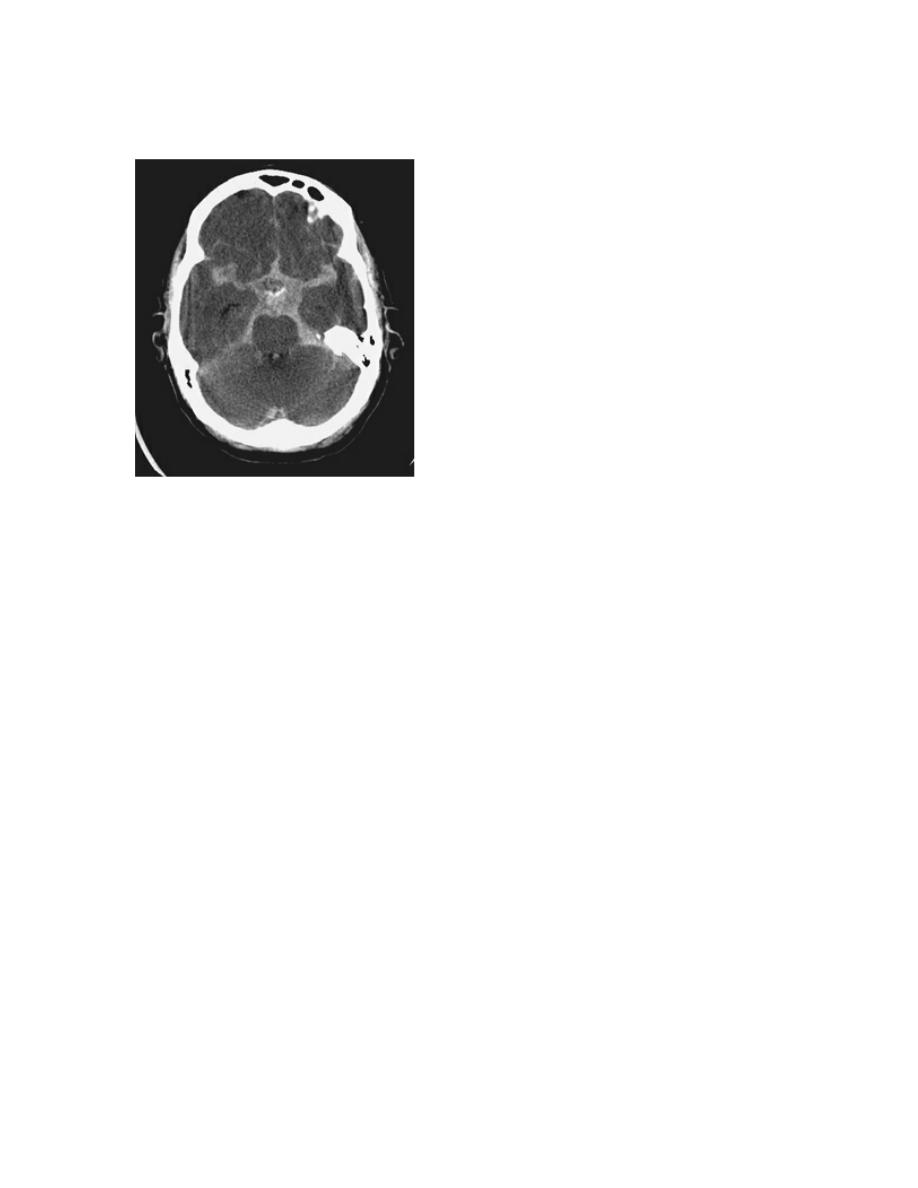
5. Subarachnoid hemorrhage (SAH)-
Hemorrhage into CSF space (cisterns,convexity). Hyperdensity is frequently
visible within minutes of onset of hemorrhage. Most commonly aneurysmal
(75-80%), but can occur with trauma, tumor, AVM (5%), and dural
malformation. The etiology is unknown in approximately 15% of cases.
Hydrocephalus complicates 20% of patients with SAH. The ability of a CT
scanner to demonstrate SAH depends on a number of factors, including
generation of scanner, time since bleed, and skill of reader. Depending on
which studies you read, the CT scan in 95-98% sensitive for SAH in the 1st
12 hours after the ictus. This sensitivity drops off as follows:
95-98% through 12 hours
90-95% at 24 hours
80% at 3 days
50% at 1 week
30% at 2 weeks
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
The location of the SAH on a CT scan has been used by some to prognosticate
the location of the presumed aneurysm, although this has been challenged:
Anterior communicating artery aneurysm (30%): Blood in and around the
interhemispheric fissure, suprasellar cistern, and brainstem.
Posterior communicating artery aneurysm (25%): Blood in suprasellar
Cistern
.
Middle cerebral artery aneurysm (20%): Blood in the adjacent sylvian cistern
and suprasellar cistern.
Aneurysmal SAH can also rupture into the intraventricular, intraparenchymal,
and subdural spaces.
Extracranial – often overlooked. Use extraaxial blood and soft-tissue swelling to
lead you to subtle fractures in areas of maximal impact.
Cisterns- CSF collections jacketing the brain. 4 key cisterns must be examined for
blood, asymmetry, and effacement (as with increased ICP).
Circummesencephalic – ring around the midbrain
Suprasellar- (Star-shaped) Location of the Circle of Willis
Quadrigeminal- W-shaped at top of midbrain

FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
Sylvian- Between temporal and frontal lobes
Brain- Inhomegenious appearance of normal gray and white matter. Examine for:
*Symmetry- Easier if patient’s head is straight in the scanner. Sulcal pattern (gyri)
should be well differentiated in adults, and symmetric side-to-side.
*Grey-white differentiation- Earliest sign of CVA will be loss of gray-white
differentiation (the “insular ribbon” sign). Metastatic lesions often found at gray-
white border.
*Shift- Falx should be midline, with ventricles evenly spaced to the sides. Can also
have rostro-caudal shift, evidenced by loss of cisternal space. Unilateral
effacement of sulci signals increased pressure in one compartment. Bilateral
effacement signals global increased pressure.*Hyper/Hypodensity- Increased
density with blood, calcification, IV contrast. Decreased density with
Air/gas (pneumocephalus), fat, ischemia (CVA), tumor.
Mass lesions:
Tumor: Brain tumors usually appear as hypodense, poorly-defined lesions on non-
contrasted CT scans. From the radiology literature, it is estimated that 70-80% of
brain tumors will be apparent without the use of contrast. Calcification and
hemorrhage associated with a tumor can cause it to have a hyperdense appearance.
Tumors should be suspected on a non-contrasted CT scan when significant edema
is associated with an ill-defined mass. This vasogenic edema occurs because of a
loss of integrity of the blood-brain barrier, allowing fluid to pass into the
extracellular space. Edema, because of the increased water content, appears
hypodense on the CT scan. Intravenous contrast material can be used to help define
brain tumors. Contrast media will leak through the incompetent blood-brain barrier
into the extracellular space surrounding the mass lesion, resulting in a contrast-
enhancing ring. Once a tumor is identified, the clinician should make some
determination of the following information: Location and size (intraaxial-within
the brain parenchyma, or extraaxial), and the degree of edema and mass effect (e.g.
is herniation impending due to swelling).
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
Abscess: Brain abscess will appear as an ill-defined hypodensity on non-contrast
CT scan. A variable amount of edema is usually associated with such lesions and,
like tumors, they frequently ring-enhance with the addition of intravenous contrast.
Ischemic infarction:
Strokes are either hemorrhagic or non-hemorrhagic. Non-hemorrhagic infarctions
can be seen as early as 2-3 hours following ictus (if you count ultra-early changes
such as the “insular ribbon sign”), but most will not begin to be clearly evident on
CT for 12-24 hours. The earliest change seen in areas of ischemia is loss of gray-
white differentiation. This can initially be a subtle finding. Edema and mass effect
are seen in association with approximately 70% of infarctions,
and is usually maximal between days 3 and 5.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
Lacunar infarctions are small, discreet non-hemorrhagic lesions, usually secondary
to hypertension and found in the basal ganglia region.
Ventricles - Pathologic processes cause dilation (hydrocephalus) or
compression/shift. Communicating vs. Non-communicating. Communicating
hydrocephalus is first evident in dilation of the temporal horns (normally small,
slit-like). The lateral, IIIrd, and IVth ventricles need to be examined for
effacement, shift, and blood.
FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
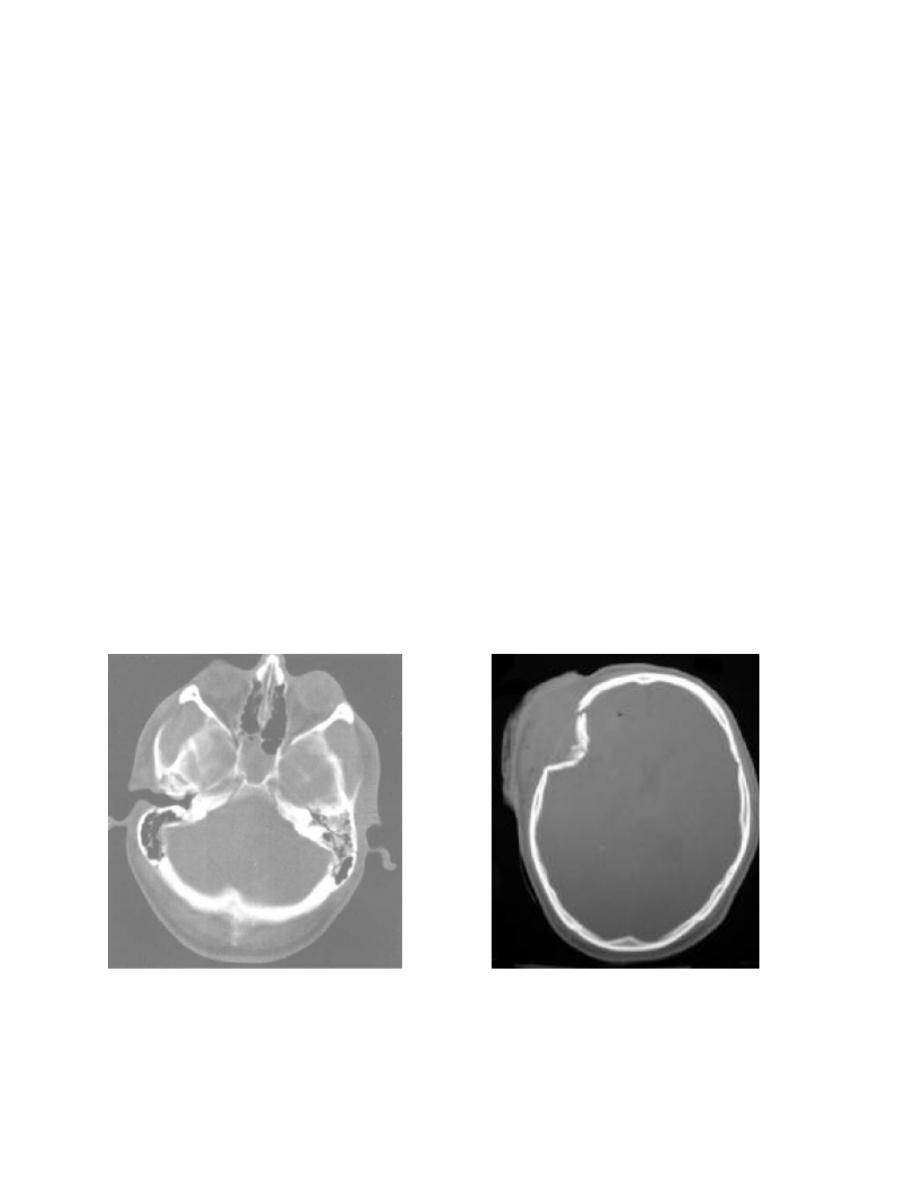
Bone - Has the highest density on CT scan (+1000 Hounsfield units). Note soft
tissue swelling to indicate areas at risk for fracture.
Skull fracture:
Making the diagnosis of skull fracture can be confusing due to the presence of
sutures in the skull. Fractures may occur at any portion of the bony skull. Divided
into nondepressed (linear) or depressed fractures, the presence of any skull fracture
should increase the index of suspicion for intracranial injury. The presence of
intracranial air on a CT scan means that the skull and dura have been violated at
some point. Basilar skull fractures are most commonly found in the petrous ridge
(look for blood in the mastoid air cells). Maxillary/ethmoid/sphenoid sinuses all
should be visible and aerated: the presence of fluid in any of these sinuses in the
setting of trauma should raise suspicion of a skull fracture.

FERNE / EMRA 2009 Mid-Atlantic Emergency Medicine Medical Student Symposium:
ABCs of Head CT Interpretation; Heather M. Prendergast MD, MPH.
Summary:
Cranial computed tomography is integral to the practice of emergency medicine,
and is used on a daily basis to make important, time-critical decisions that directly
impact the care of ED patients. An important tenet in the use of cranial CT is that
accurate interpretation is required to make good clinical decisions. Cranial CT
interpretation is a skill, like ECG interpretation, that can be
learned through education, practice, and repetition.
Acknowledgement: Special thanks to Andrew D. Perron, MD, FACEP and Brian
A. Stettler, MD, FACEP .
