Postoperative Care &postoperative complications
The aim of postoperative care is:To provide the patient with as quick, painless and safe a recovery from surgery as possible.
Postoperative Care
Pain managementPostoperative fever
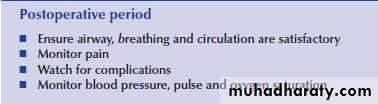
Recognize postoperative complicationsImmediate Postoperative Period:
Anesthesiologist in charge of cardiopulmonary functionsImmediate Postoperative Phase Recovery Room, ICU
ABCs of Immediate Recovery periodairway
breathing
Consciousness
Circulationsystem review
Discharge from the recovery room, ICUVital signs
Controlled pain
AwakeGag reflex returned
Respirations and circulatory function normalSurgeon responsible for all the rest
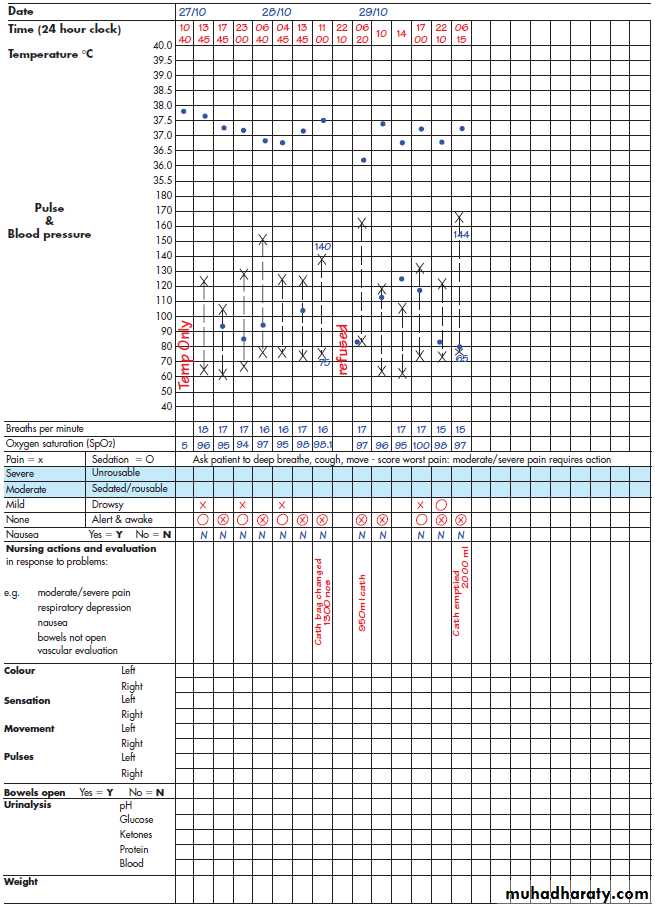
Surgeon’s ResponsibilitiesPost Operative ChecksNote time of return, note level of consciousness, monitor vital sign
• Check dressings, location
• Check incision, report drainage, redness, edema• Check IV site
• Report kinked tubing• Check pulses distal to op. site.
• Measure and record 1st. Void, report flatulence.• Learn type, purpose, location of all tubes, and how to empty.
• Report change in character of drainage, notify nurse of need for dressing change.• Report changes in skin color.
• Equipment- report if disconnected or malfunctioning.
Position in bedMobilization
MedicationsDiet
Fluid balance, electrolytesRespiratory care
Postoperative PhaseLevel of consciousness, movement, sensation
Skin color, temperature, nailbeds, oxygen saturation
Lungs sounds, pulses, heart rate.
Inspect abdomen for distention, monitor return of
bowel sounds, ask about flatusPain control.
Comfort measures: reposition, oral care, hygiene.Monitor dressing.
Empty drainage tubes.Turn, cough & deep breathing; incentive spirometry every hour.
early ambulation.Monitor output – minimum of 30cc/hr;
should void within 8 hours of surgeryNPO until ordered, start with clear liquids – full liquids – soft diet
Monitor closely for signs of infection
Administer medications as ordered-antibiotics.
Pain Management
Essential part of postoperative managementPain can increase risk of complications
Pain relief- Multimodal
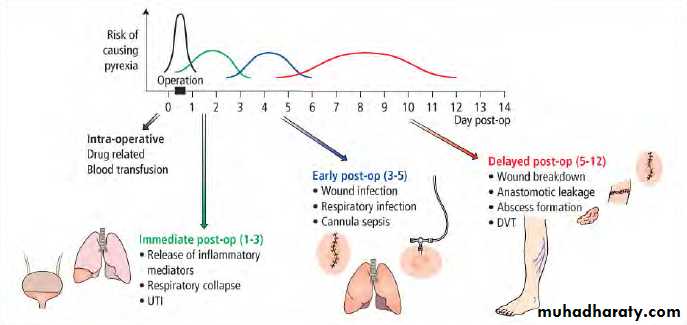
E.g. PCA, IM pethidine, oral analgesicsPostop Fevers
An important sign of postoperative complications.History
ExaminationInvestigations (to confirm the diagnosis)
Many possible DDX.
Time of onset may guide the management.
First 48hrs• Atelectasis
• Transfusion rx
• Pre-existing infection
3-7 days: infections like:
• UTI, wound infection, Catheter related phlebitis , pneumonia, anastomotic leakage
About 7 days onwards
• Abscess formation• Allergy to drug
• Transfusion related fever
• DVT/PE
Postop Complications
General
Specific
Complications do occur, but many are preventable!General
• Important examples:• MI
• pneumonia
• DVT/Pulmonary embolism
• CVA
• Specific
• Examples:• anastomotic leakage
• abscess formation
• wound infection
• ileus
• bleeding
Wound complications
Postoperative urinary retention
Respiratory complications
Postoperative parotitis
GIT complications
Wound complication
Wound infection
Wound hematoma
Wound seroma
Wound dehiscence
Wound infection
Operative wound classification :I clean 3.3-4 %
II clean-contaminated 8-10 %
III contaminated &
IV dirty (infected) 28 %
Wound infection
Clinical manifestation :pain
swollen & edematous
redness & cellulitis
warm to touch
Wound infection
Wound infections are classified as :
Minor
( purlent material around skin suture sites)
Major
( discrete collection of pus within the wound )
Wound infection
Wound infections are classified as :Superficial infection
( limited to skin & subcutanous tissue )
Deep infection
( involve area of the wound below the fascia )
Wound infection
• Skin preparation• Bowel preparation
• Prophylactic antibiotic
• Meticulous technique
• Appropriate drainage
Wound infection
Management :
Incision should be opened for drainage
Debridement if there is necrosis
Antibiotic if there is cellulitis
Wound Hematoma
Caused by inadequate hemostasis
Good media for bacteria
Manifested by pain & swelling
Drain should be used
Must be evacuated in certain location
The wound should be opened in OR
Wound Seromas
Are lymph collections
Operation in which large areas of lymph-bearing tissues are transected
Closed-suction drain with pressure dressing
Repeated aspiration is indicated
Fertile ground for bacteria
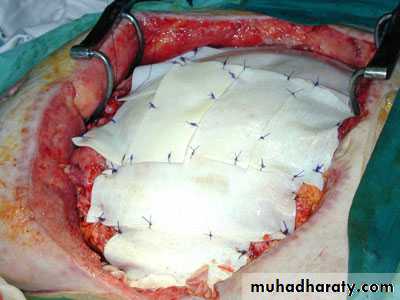
Wound Dehiscence
Dehiscence
( is separation within the fascial layer , usually of abdomen )
Evisceration
(extrusion of peritoneal contents through the fascial separation)
Incidence : 0.5 – 3.0 % in all abdominal procedures .
Wound Dehiscence
Related factors :
Imperfect technical closure
Increased intra-abdominal pressure from bowel distention, ascites, coughing, vomiting, or straining
Hematoma with or without infection
Infection
Metabolic diseases such as
diabetes mellitus,
uremia,
Malignant disease,
Radiation
Wound Dehiscence
Detected by the classical appearance of salmon colored fluid draining from wound occurs in about 85 % of cases about fourth or fifth postoperative days
Present late as an incisional hernia
Wound Dehiscence
Complete repair , the skin and subcutaneous tissue, facial layers closed.
Urinary retention
Incidence :
major abd. Surgery : 4 – 5 %
Anorectal surgery : > 50 %
Urinary retention
Stress ,pain ,spinal anesthesia & anorectal reflexes lead to increased Alpha-adrenergic stimulation , which prevent release of musculature around the bladder neck
Urgency ,discomfort , fullness ,enlarged bladder
Catheterization to relive retention
Respiratory complication
5 – 35 % of postop. DeathsPredisposing factors :
smoking , age ,
obesity , COPD ,
cardiac disease
Respiratory complication
• Atelectasis
• Aspiration
• Pulmonary edema
• Pulmonary embolism
• Collapse of alveoli
Anesthesia , postop. Incisional pain
Lung inflation in postop. period
2) Aspiration :
During induction of anesthesia
CXR show progression of local damage & infiltration
Prevention is only effective treatment
3) Pulmonary edema :
Most common causes are fluid over load or myocardial insufficiency
Occur during :
* resuscitation
* postop. Period
3) Pulmonary edema :
Simple therapy including O2 , digitalization & upright position
4) Pulmonary embolism :
100’000 patients died in US per year
90 % originate from DVT of iliofemoral ves.
4) Pulmonary embolism :
Mild tachypnea to sudden cardiopulmonary arrest
Diagnosis require combination of :
- ABG
- CXR
- ECG
- Doppler studies for lower extremities
- Radionucleotide ventilation – perfusion scan
4) Pulmonary embolism :
Management options :
* intensive supportive measures & resuscitation.
* direct or systematic thrombolysis.
* surgical pulmonary ebolectomy.
* IVC filter.
Prevention of PE by using mechanical devices or pharmacologic inhibition of coagulation
Postoperative Parotitis
Serious complication
High mortality rate
Rt. & Lt. equally involved
Bilaterally 10 – 15 % of cases
75 % of patients are 70 year or older
Poor oral hygiene , dehydration , use of anticholinergic drugs
Postoperative Parotitis
Majority of infections are from staphylococi
Lack of oral intake to stimulate parotid secretions predisposes to bacterial invasion of Stensen’s duct
Interval between operation & the onset varies from hours to many weeks
Postoperative Parotitis
Present with :
pain in the parotid region
swelling & tenderness
cellulitis on face & neck
temperature & leukocyte high
Prophylaxis includes adequate hydration & good oral hygiene
Postoperative Parotitis
Antibiotic should be started against staphylococi
Surgical drainage
( by incision made ant. to ear extending to mandible angle )
In 80 % of patient treated with incision & drainage the parotitis was palliated or cured
GIT complications
• Ileus• Anastomotic leaks
• Fistulas
• Stomal complication
1) Ileus :
Non-mechanical obstruction that prevents normal postop. Bowel function
Arise from neural inhibition of bowel motor activity & effective peristalsis
Increased with manipulation ,inflammation , peritonitis & blood left in peritoneal cavity
1) Ileus :
Blood in retroperitoneum often produces ileus
Hypokalemia , hypocalcemia , hyponatremia & hypomagnesemia prolong postop. Ileus
Treatment is purely supportive
2) Anastomotic leaks :
The etiology factors :
1) poor surgical tech.
2) distal obstruction
Risk increase with S.Albumin < 3.0 mg/dl
2) Anastomotic leaks :
Three technical factors play roles in a proper anastomosis :
1- both end of bowel should have adequate blood supply
2- anastomosis should lie in tension-free manner
3- adequate hemostasis
3) Fistulas :
Abnormal communication between two epithelial surfaces
Common problem of GIT surgery
Can occur between :
( enterocutanous fistula ) , ( enteroenteric fistula )
( enterovesical fistula ) , ( enterovaginal fistula )
3) Fistulas :
Most common cause is anastomotic leakage
Persistence secondary to ( FRIEND )
( F.B. , Radiation , Infection , Epithiallization , Neoplasm , Distal obstruction )
Spontaneous closure usually occurs within 5 weeks with adequate nutrition
If persist >5 weeks operation is indicated
4) Stomal complications :
Stomal necrosis & retraction
( inadequate blood supply lead to ischemia )
Stomal stricture
( late complication , caused by development of serositis )
Peristomal hernia & prolapse
( resecting the stomal prolapse & fixing it again in place )
Skin complication