Diabetic ketoacidosis
Essential early investigationsBlood glucose(11.1mmol/L) or (>300mg/dl)
Urea and electrolytes, creatinine (dehydration)
Blood gas analysis (severe metabolic acidosis)
Urinary glucose and ketones (both are present (
Evidence of a precipitating cause, e.g. infection (blood and urine cultures performed(
Cardiac monitor for T-wave changes of hypokalaemia
Treatment
Treatment is divided into 3 phasestreatment of ketoacidosis
transition period
continuing phase and guidance
Goals of treatment of DKA
intravascular volume expansioncorrection of deficits in fluids, electrolytes, and acid-base status
initiation of insulin therapy to correct catabolism, acidosis
Intravascular volume expansion
dehydration is most commonly in the order of 10%
initial hydrating fluid should be isotonic saline
this alone will often slightly lower the blood glucose
rarely is more than 20 cc/kg fluid required to restore hemodynamics
Treatment of electrolyte abnormalities
serum K+ is often elevated, though total body K+ is depleted
K+ is started early as resolution of acidosis and the administration of insulin will cause a decrease in serum K+
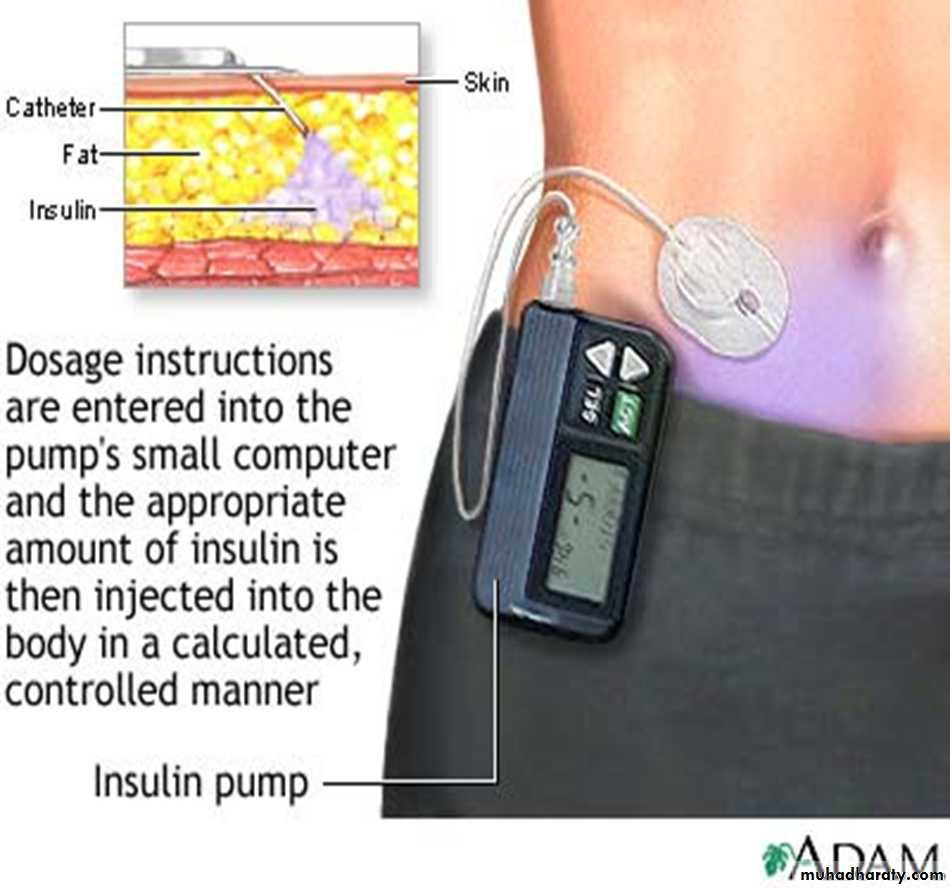
Insulin Therapy
continuous infusion of low-dose insulin IV (~ 0.1 U/kg/hr) is effective, simple, and physiologically sound or 0.5-1u/kg then o.2-o.4 every 6hrgoal is to slowly decrease serum glucose, frequent laboratory and blood gas analyses are obtained to ensure ongoing resolution of metabolic acidosis
AM 2/3
PM 1/32/3 NPH
1/3 Regular
NPH (2/3)
Regular (1/3)
NPH and Regular