1
Forth stage
Obstetric
Lec-2
.د
ولدان
1/1/2016
Female reproductive physiology
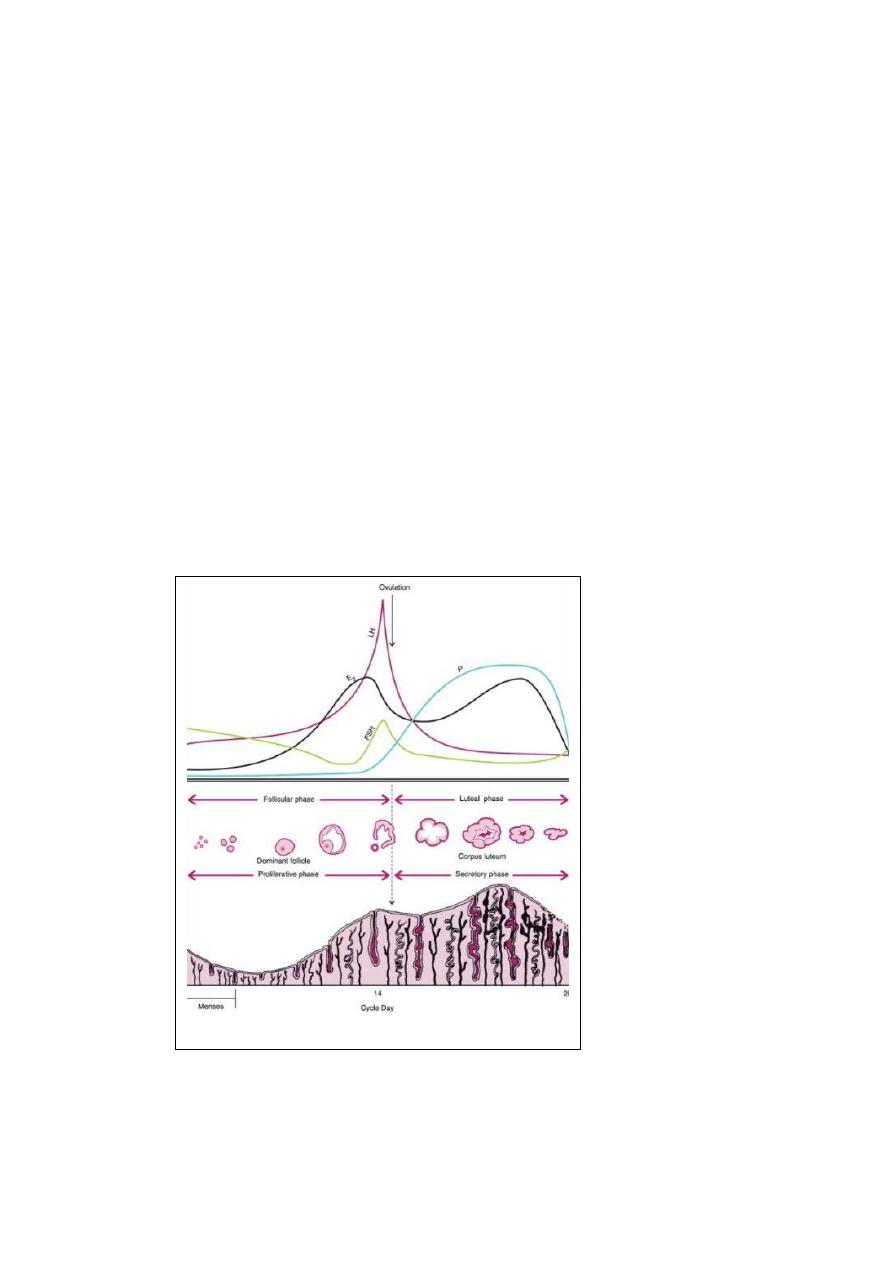
The most obvious manifestation of the normal menstrual cycle is the presence of regular
menstrual periods. These occur as the endometrium is shed following failure of implantation
or fertilization of the oocyte.
An intact hypothalamo-pituitary-ovarian axis is required for normal menstruation.
I-Ovary:
Within the ovary, the menstrual cycle can be divided into three phases:
1- follicular phase.
2- ovulation.
3- luteal phase.
1-The follicular phase:
The ovary contain thousands of primordial follicles. These initial stages of follicular
development are independent of hormonal stimulation. In the absence of the correct
hormonal stimulus, follicular development fails at the preantral stage, with ensuing follicular
atresia. Development beyond the preantral stage is stimulated by LH and FSH (key regulator
of oocyte development).
At the start of the menstrual cycle, FSH levels start to rise as the pituitary is released from
the negative feed back effects of progesterone, oestrogen and inhibin. Rising FSH rescue a
cohort of follicles from atresia.
The basis of hormonal activity in preantral to preovulatory follicles is described as the (two
cells, two gonadotrophin) hypothesis. The two cells are theca and granulosa cells. These two
cells are responsive to two gonadotrophin LH and FSH respectively.
Within the theca cells, LH stimulates the production of androgen from cholestrol. Within the
granulosa cells, FSH stimulates the conversion of thecally derived androgens to estrogens
(aromatization). Normally only one of these follicles is destined to grow to a pre-ovulatory
follicle and be released at ovulation ( the dominant follicle). The dominant follicle is the
largest and most developed follicle in the ovary at the mid-follicular phase. So the largest
follicle therefore requires the lowest levels of FSH and LH for continued development. At
the time of follicular selection, FSH are declining in response to the negative feed back effects
of oestrogen. Therefore the dominant follicle is the only follicle that is capable of continued
development in the phase of falling FSH levels.
2
2- the ovulation:
Late in the follicular phase, FSH induces LH receptors on granulosa cells. As the dominant
follicle develops further, follicular estrogen production increases. This lead to a +ve feed back
effect on the pituitary LH secretion. LH levels increase at first slowly (day 8-12) and then
more rapidly (day 12 on wards). During this time, LH induces luteinization of granulosa cells
in the dominant follicle, so that progesterone is produced and this will further amplifies the
+ve feed back effect of estrogen on pituitary LH secretion, leading to a surge of the LH.
Ovulation occurs 36 hours after the onset of the LH surge. At the time of ovulation, the LH
surge stimulates the resumption of meioses, a process which is completed after the sperm
enters the egg. The increase in FSH, LH and progesterone stimulate the proteolytic enzymes
within the follicle cause follicular wall break down and release of the oocyte.
3-Luteal phase:
This phase characterized by the production of progesterone from the corpus luteum within
the ovary. The corpus luteum is derived both from the granulosa cells and from some of theca
cells. The duration of the luteal phase is fairly constant, being around 14 days in the most
women. In absence of pregnancy and the production of HCG from the embryo, the corpus
luteum regress at the end of the luteal phase, a process known as leuteolysis this lead to
decrease in oestrogen, progesterone and inhibin levels and the pituitary is released from the
negative feed back effects of these hormonens, and gonadotrophins, particularly FSH start
to rise and a further menstrual cycle is initiated.
II- Pituitary gland:
The pituitary gland hormones LH and FSH are key regulators of folliculo- geneses. The output
of these hormones is stimulated by pulses of gonadotrophin releasing hormone (GnRH)
produced by the hypothalamus. The response of the pituitary is not constant, but is
modulated by ovarian hormones, particularly oestrogen and progesterone.
III- Hypothalamus:
The pulsatile secretion of GnRH, stimulates pituitary LH and FSH secretion. There is an
alteration in the amplitude and frequency of GnRH through out the cycle.
IV- Endometrium:
The endometrium undergo cyclic changes during the menstrual cycle. These changes can be
divided into the following:
3
1. Menstruation.
2. The proliferative (follicular) phase.
3. The secretary (luteal) phase.
1- Menstruation:
Is the shedding of the dead endometrium and ceases as the endomertrium regenerates. In
an ovulatory cycle, the endometrium becomes decidualized ( oestrogen and then
progesterone in an orderly manner ) during the 2
nd
half of the cycle to allow implantation of
the embryo. If implantation does not occur, apoptosis occurs. Menstruation is initiated by
the withdrawal of oestrogen and progesterone. This lead to intense spiral artery
vasoconstriction ( indirect effect) and then lead to ischemia and tissue damage, shedding of
functional endometrium ( stratum compactum and stratum spongiosum ) and bleeding from
fragments of arterioles remaining in the basal endometrium.
Haemostasis is secured by spiral artery vasoconstriction and scaring is reduced by enhanced
fibrinolysis, which breaks down blood clots. Later, repair of the endometrium and new vessel
formation ( angiogenesis) lead to complete cessation of bleeding within 5-7 days from the
start of the menstrual cycle.
2- The proliferative phase:
Under the effect of oestrogen the follicular phase characterized by glandular and stromal
growth. The epithelium lining of the endometrial glands changes from a single layer of low
columnar cell to pseudostratifid epithelium with frequent mitosis.
The endometrium thickness increased from 0.5mm at menstruation to 3.5mm at the end of
the proliferative phase.
3- The secretary phase:
Under the action of progesterone (from the corpus luteum) this phase is characterized by
glandular secretary activity with inhibition of proliferation. Subnuclear intracytoplasmic
granules appear in the cells and their content are released into the endometrial cavity. The
gland become tortuous and the stroma becomes edematous and the spiral arties continue
to extend into the superfacial layer of endometrium and become convoluted (these changes
occur only after ovulation). The peak secretory activity occurs at time of implantation (7 days
after the gonadotrophin surge)
In the late secretory phase, progesterone induces irreversible decidualization of the stroma.
Immediately prior to menstruation the endometrium shows three distinct zones:
4
1. Stratum basalis (25%) which is retained during menstruation and shows few changes
during the cycle.
2. Stratum spongiosum (in the mid 50%) edematous stroma and exhausted glands
3. Stratum compactum ( upper layer 25%) with prominent decidualized stromal cells.
The withdrawal of estrogen and progesterone leads to collapse of the deciualized
endometrium, repeated vasoconstriction and relaxation of the spiral arterioles, and
consequent shedding of the endometrium. The onset of menstruation heralds the end of one
menstrual cycle and the beginning of the next.
Normal menstrual cycle (clinical features):
Cycle duration 28 days (21-35).
Duration of blood flow 3-7 days (2-8).
Peak flow on the 1
st
or 2
nd
day.
Normal menstrual loss 35ml/month (max. 80ml).
