
1
Forth stage
Obstetric
Lec-2
د. براء
1/1/6112
Management of Miscarriage
Management of early pregnancy loss
Assessment of the patient should include a full history and examination. Investigations may
include:
Pelvic ultrasound scan
Full blood count
Blood group and save serum
Incomplete, missed abortion:
If bleeding is heavy, there is considerable pain, then emergency medical attention is
recommended to be sought. Otherwise, there are three treatment options:
Expectant management
Medical management
Surgical management
Expectant management
With no treatment (watchful waiting), most of these cases (65–80%) will pass naturally within
two to six weeks. This path avoids the side effects and complications possible from
medications and surgery. This is mostly applied to missed abortion and blighted ovum.
Medical management
Misoprostol
Mifepristone plus Misoprostol
Methotrexate plus Misoprostol
There is no medical regimen for management of early pregnancy loss that is FDA
approved.
Misoprostol
Prostoglandin E1 analogue
FDA approved for prevention of gastric ulcers

2
Used off-label for many ob/gyn indications
o Labor induction
o Cervical ripening
o Medical abortion (with mifepristone)
o Prevention/treatment of post-partum hemorrhage
Can be administered by oral, buccal, sublingual, vaginal and rectal routes
Why misoprostol?
Do something while still avoiding surgery
Cost effective
Few side effects (especially with vaginal)
Stable at room temperature
Readily available
800 mcg. per vagina (or buccal)
Repeat x 1 at 12-24 hours if incomplete
Intervene with surgical management if:
o Continued gestational sac
o Clinical symptoms
o Patient preference
o Time (?)
Surgical management
Surgical treatment (most commonly vacuum aspiration, sometimes referred to as a D&C or
D&E) is the fastest way to complete the miscarriage. It also shortens the duration and
heaviness of bleeding, and is the best treatment for physical pain associated with the
miscarriage. In cases of repeated miscarriage, D&C is also the best way to obtain tissue
samples for pathology examination. D&C, however, has a higher risk of complications,
including
1. Risk of injury to the cervix and uterus
2. Perforation of the uterus
3. Potential scarring of the intrauterine lining.
Who should have surgical management?
o Unstable
o Infected
o Very heavy bleeding
o Anyone who wants immediate therapy

3
Postmiscarriage care
Anti D at time of diagnosis or surgery for non-sensitized Rh negative woman with Rh
positive husband
Pelvic rest for 2 weeks
No evidence for delaying conception
Expect light-moderate bleeding for 2 weeks
Menses return after 6 weeks
Negative BhCG values after 2-4 weeks
Appropriate grief counseling
Future miscarriage risk
Increased risk of miscarriage in future pregnancy
20% after 1 SAb
28% after 2 SAbs
43% after 3+ SAbs
Septic abortion
A septic abortion or septic miscarriage is a form of miscarriage that is associated with a
serious uterine infection. The infection carries risk of spreading infection to other parts of the
body and cause septicemia, a grave risk to the life of the woman. The infection can occur
during or just before or after an abortion.

4
Symptoms
In a woman with septic abortion, symptoms that are related to the infection are mainly:
High fever, usually above 101 °F , chills
Severe abdominal pain and/or cramping /or strong perineal pressure
Prolonged or heavy vaginal bleeding
Foul-smelling vaginal discharge
Backache or heavy back pressure
As the condition becomes more serious, signs of septic shock may appear, including:
hypotension
hypothermia
oliguria
Respiratory distress (dyspnea)
Septic shock may lead to kidney failure, bleeding diathesis, and disseminated
intravascular coagulation (DIC).
If the septic abortion is not treated quickly and effectively, the woman may die.
Risk factors
The risk of a septic abortion is increased by mainly the following factors:
The fetal membranes surrounding the unborn child have ruptured, sometimes without
being detected
The woman has a sexually transmitted infection such as chlamydia
An intrauterine device (IUD) was left in place during the pregnancy
Tissue from the unborn child or placenta is left inside the uterus after a miscarriage
Unsafe abortion was made to end the pregnancy
Mifepristone (RU-486) was used for a medical abortion
Treatment
The woman should have intravenous fluids to maintain blood pressure and urine
output. Broad-spectrum intravenous antibiotics should be given until the fever is gone.
A dilatation and curettage (D&C) may be needed to clean the uterus of any residual
tissue.
In cases so severe that abscesses have formed in the ovaries and tubes, it may be
necessary to remove the uterus by hysterectomy, and possibly other infected organs
as well.
Recurrent pregnancy loss
5
3 or more consecutive pregnancy losses prior to 20 weeks not including ectopic, molar,
biochemical
Causes
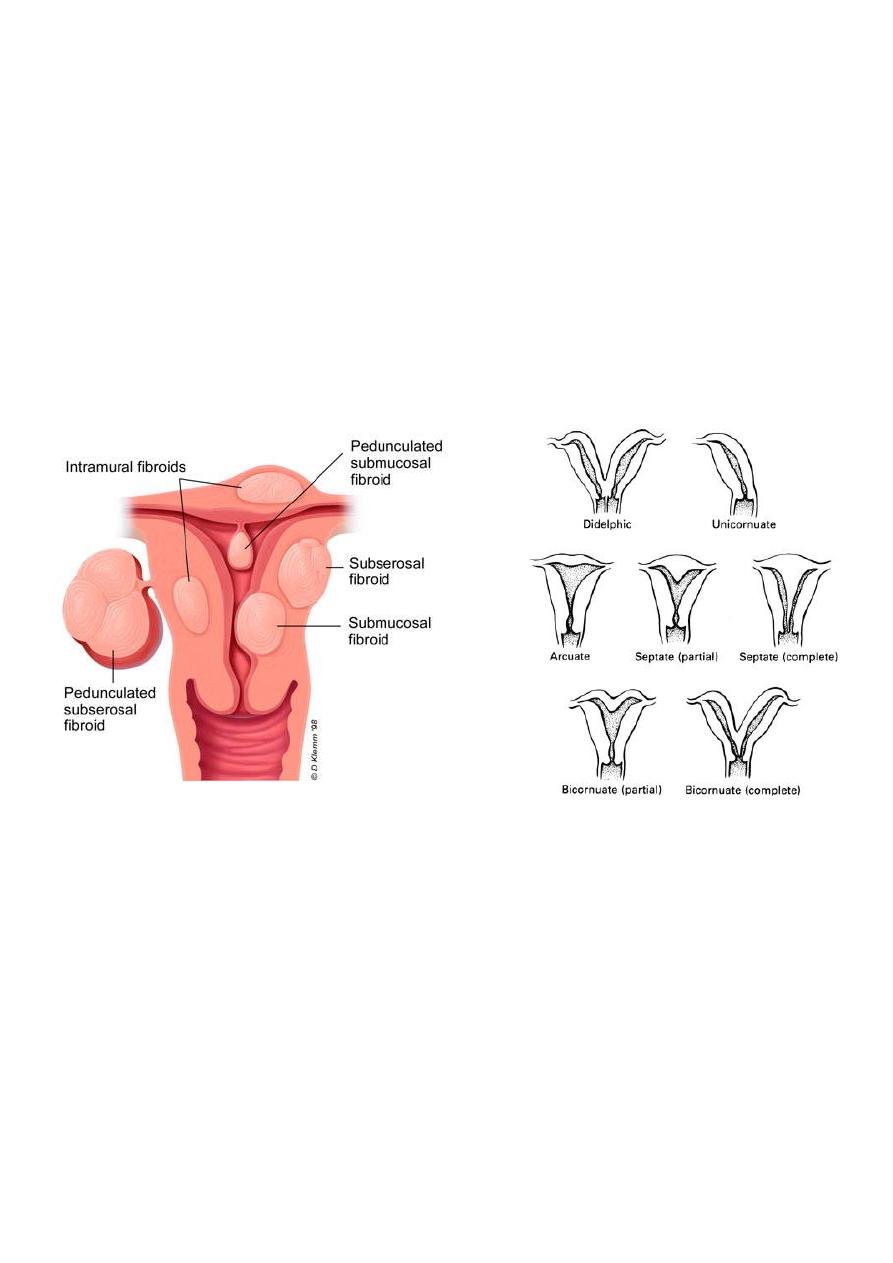
1. Uterine Pathology
10-50% of RPL via abnormal implantation and uterine distention
Mullerian anomalies of septate, bicornuate, didelphic uteri (not arcuate)
Submucous leimyoma >>intramural or subserous
Intrauterine synechiae (Asherman’s)
Cervical incompetence – midtrimester
Evaluation: Sonohysterography or Hysterosalpingogram; 2
nd
line tests include hysteroscopy,
laparoscopy, or MRI
2. Hypercoagulable States
Antiphospholipid syndrome
5-15 % of RPL, as well as late fetal death
History of thromboembolism or pregnancy complication with high titers of anti-
cardiolipin antibody and/or lupus anticoagulant
Treat with heparin (5,OOO-10,000 units BID) and aspirin .
3. Endocrine Disorders
15-60 % of RPL
Poorly controlled diabetes with HgA1c > 8
PCOS

6
Poorly controlled thyroid disease and potentially subclinical hypothyroidism
Hyperprolactinemia
Historically luteal phase defects
Diagnosis in question and suggested treatments not effective, but source of
progesterone trial
4. Immunologic Factors
Alloimmune reaction of mother to “foreign” tissue of embryo
HLA-mediated factors
5. Chromosomal Factors
2-4% of RPL with chromosomal rearrangement: ½ balanced translocation; ¼
Robertsonian translocation; other sporadic mutations, inversions
Evaluation: Parental karyotype and karyotype of abortus if possible
Treatment: Genetic counseling; IVF with preimplantation screening of embryos or
gamete donation
6. Environmental Factors
No good evidence for recurrent SAb
Sporadic pregnancy loss affected by smoking, alcohol, anesthetic gases, caffeine >
300mg/day, obesity.
Cervical incompetence
Cervical incompetence is a medical condition in which a pregnant woman's cervix begins to
dilate (widen) and efface (thin) before her pregnancy has reached term.
Cervical incompetence may cause miscarriage or preterm birth during the second and third
trimesters. In a woman with cervical incompetence, dilation and effacement of the cervix
may occur without pain or uterine contractions. If the responses are not halted, rupture of
the membranes and birth of a premature baby can result.
Risk factors
history of conization (cervical biopsy),
Diethylstilbestrol exposure, which can cause anatomical defects, and
uterine anomalies

7
Repeated procedures (such as mechanical dilation, especially during late pregnancy) appear
to create a risk. Additionally, any significant trauma to the cervix can weaken the tissues
involved
Symptoms of Cervical Incompetence
Women with incompetent cervix typically present with "silent" cervical dilation (i.e., with
minimal uterine contractions) between 16 and 28 weeks of gestation. When the cervix
reaches 4 cm or more, active uterine contractions or rupture of membranes may occur.
Diagnosis of Cervical Incompetence
Cervical incompetence is an important, but undoubtedly over-diagnosed, condition.
A diagnosis of cervical incompetence is usually made on the basis of a woman's past
pregnancy history. Classically this is following one or more late second trimester or early third
trimeser losses . Usually they begin with a gradual painless dilatation of the cervix, with
membranes bulging into the vagina.
Transvaginal ultrasound (TVS) during pregnancy has shown some promise. The usual length
of the cervix is about 4cm as measured on TVS. Women with a cervical length of less than
2.5cm have been found to have a 50% risk of preterm delivery in one study. Other studies
have looked at opening of the internal section of the cervix ('funnelling' or 'beaking') in
response to pressure on the top of the uterus.
Treatment
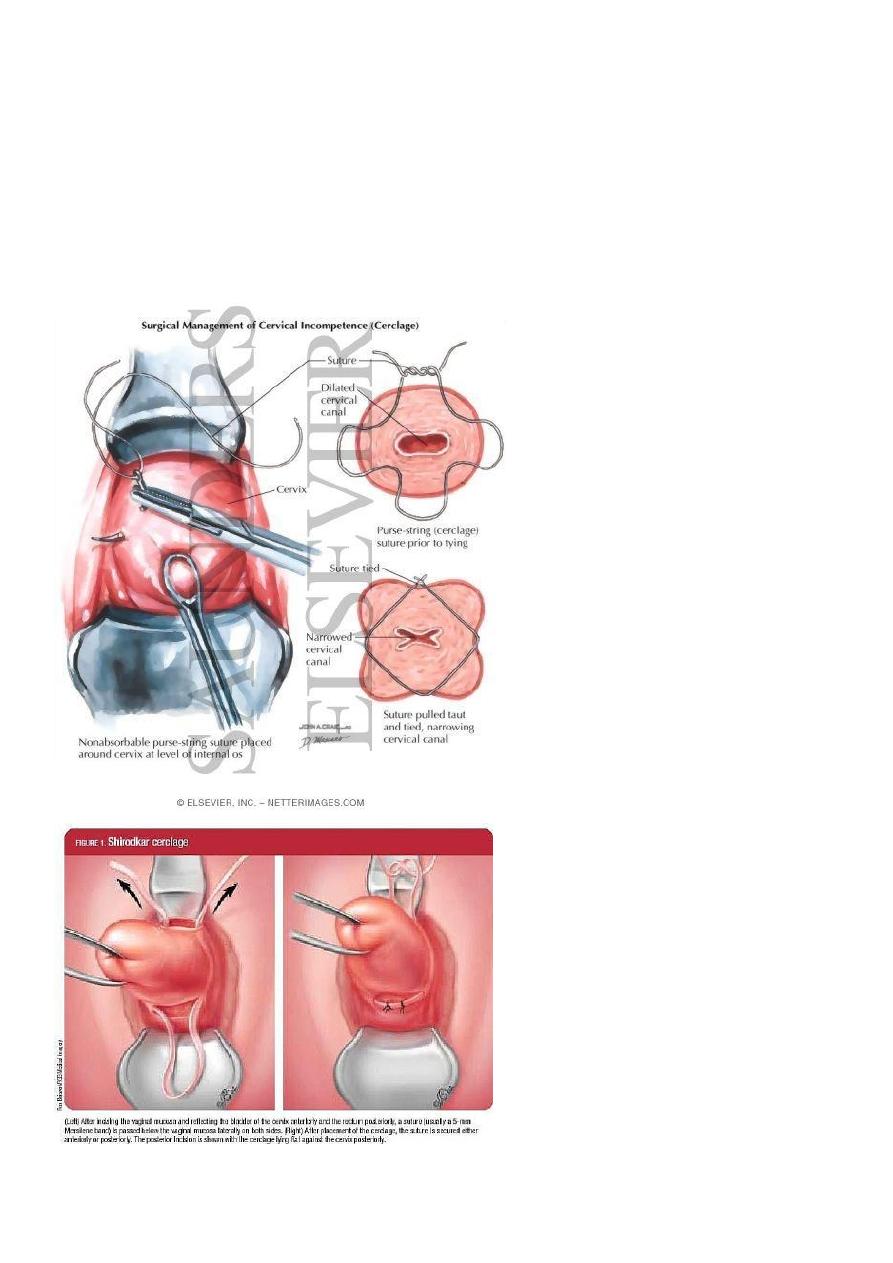
Cervical cerclage is the treatment that is offered. This involves placing a stitch high up
around the cervix to try & keep it closed. The stitch can be placed either vaginally or
via an abdominal incision. The latter is usually used when vaginally placed stitches fail.
They are called McDonald or Shirodkar stitches. The Shirodkar variant involves a bit
more extensive surgery to ensure the stitch is high up on the cervix.
8
This is usually performed after the twelfth week of pregnancy, the time after which a
woman is least likely to miscarry for other reasons - but it is not done if there is rupture
of the membranes or infection.
The stitch is usually removed around 37 weeks and labour ensues fairly rapidly if the
diagnosis was correct. Abdominal cerclage requires an elective caesarean section and
the stitch is usually left in-situ for future pregnancies. Complications of the stitch
include rupture of the membranes at the time of placement, and increased risk of
infection
