
1
Forth stage
Obstetric
Lec-1
د. براء
1/1/6112
Antenatal care & Pre-conceptual counselling
Antenatal care
Definition: Careful, systeamatic assessment and follow up of a pregnant patient to assure
the best health of the mother and her fetus.
Aims of antenatal care
The main aim of antenatal care is to have a healthy mother and a healthy baby at the
end of the pregnancy:
To prevent, detect, and manage those factors that adversely affect the health of the
mother and baby.
To provide advice, reassurance, education, and support for the woman and her family.
To deal with the minor ailments of pregnancy.
To provide general health screening.
Advice, Reassurance & Education
Reassurance & explanation on pregnancy symptoms:
1. Nausea
2. Heartburn
3. Constipation
4. Shortness of Breath
5. Dizziness
6. Swelling
7. Back-ache
8. Abdominal Discomfort
9. Headaches
Mostly these represent the physiological adaptation of her body to the pregnancy and are
often called the ‘minor complaints’ of pregnancy.
Information regarding smoking, alcohol consumption and the use of drug during
pregnancy (both legal and illegal) is extremely important.
Woman also need advice on work, exercise, sexual intercourse and maternity benefit.

2
Parentcraft is the term used to describe formal group education of issue relating to
pregnancy, labour and delivery and care of the newborn. The aim of this is to lessen
anxiety and increase the sense of maternal control surrounding delivery.
Working during pregnancy
The majority of women can be reassured that it is safe to continue working during
pregnancy.
A woman’s occupation during pregnancy should be ascertained to identify those at
increased risk through occupational exposure.
Folic acid
Dietary supplementation with folic acid, before conception and up to 12 weeks’
gestation, reduces the risk of having a baby with neural tube defects (anencephaly &
spina bifida).
The recommended dose is 400 micrograms per day.
Prescribed medicines
Few medicines have been established as safe to use in pregnancy.
Prescription medicines should be used as little as possible during pregnancy and should
be limited to circumstances where the benefit outweighs the risk.
Smoking in pregnancy
There are specific risks of smoking during pregnancy (such as the risk of having a baby
with low birth weight and preterm).
The benefits of quitting at any stage should be emphasized.
Women who are unable to quit smoking during pregnancy should be encouraged to
reduce smoking.
The booking visit
The first risk assessment is usually made at the booking visit. Before risk assessment begins,
the pregnancy should be confirmed and the expected date of delivery (EDD) should be
calculated.
3
Confirmation of pregnancy
Symptoms of pregnancy combined with a positive urinary or serum pregnancy test is
sufficient confirmation of pregnancy.
In many regions, all pregnant women are referred for US ‘dating scan’ which both
confirm the pregnancy and accurately dates it.
It may be possible to hear the fetal heart with the Doppler US from approximately 12
weeks onwards.
Dating of pregnancy
Menstrual EDD
Naegele´s rule; EDD calculated by adding 7 days to the first day of the LMP and tacking away
3 months.
Dating by ultrasound
Dating by an ultrasound scan in the first or early second trimester is more accurate,
especially if there is menstrual irregularity or uncertainity regarding the LMP
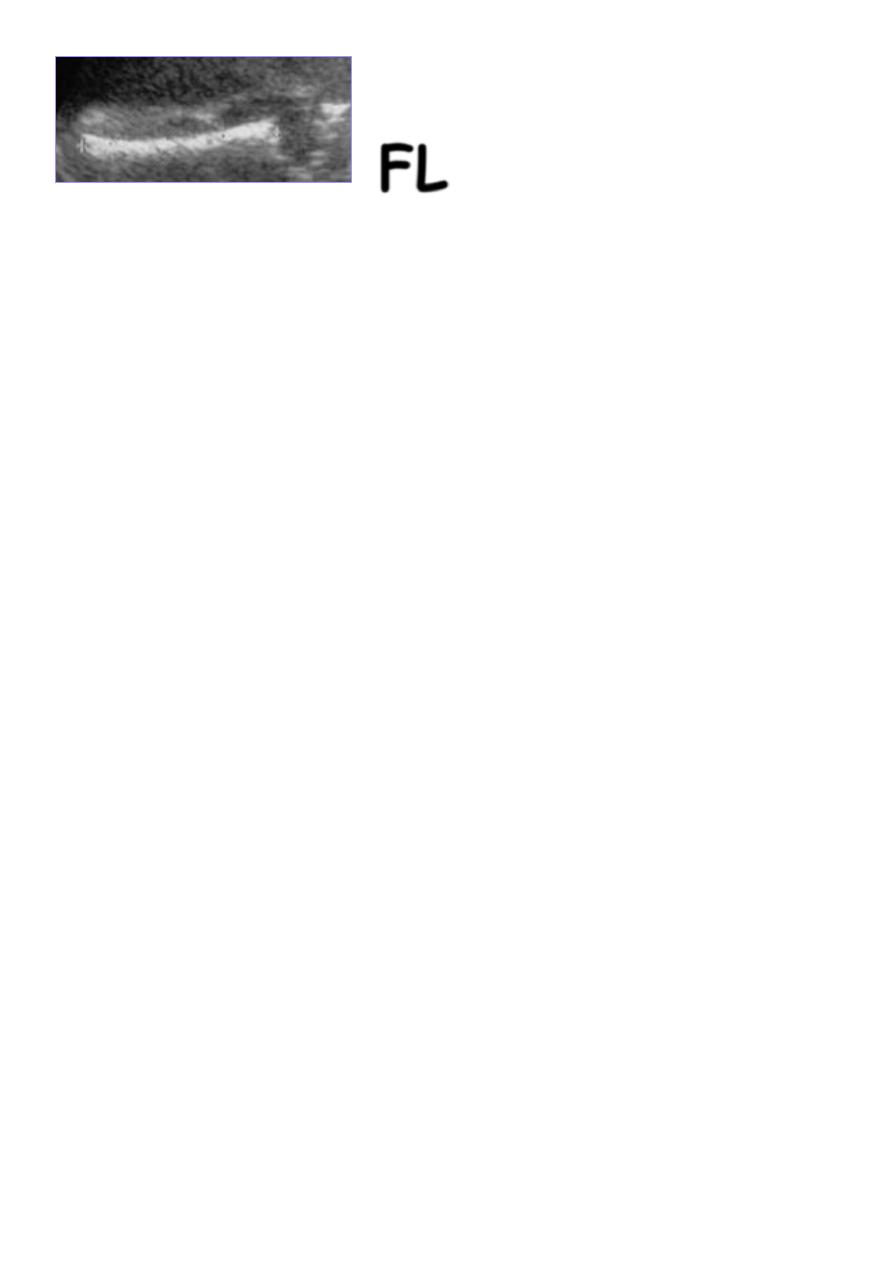
Before 15-16 weeks variation is little and the measurement of the crown-rump length
CRL, biparietal diameter (BPD) and femur length (FL) is used for estimation of the
gestational age.
If the EDD predicted by the dating scan differ by more than 7 days from the menstrual
EDD, the scan dating is usually chosen as the final EDD.
After 20 weeks there is significant variation in fetal size, so dating pregnancy by
ultrasound scan becomes less accurate
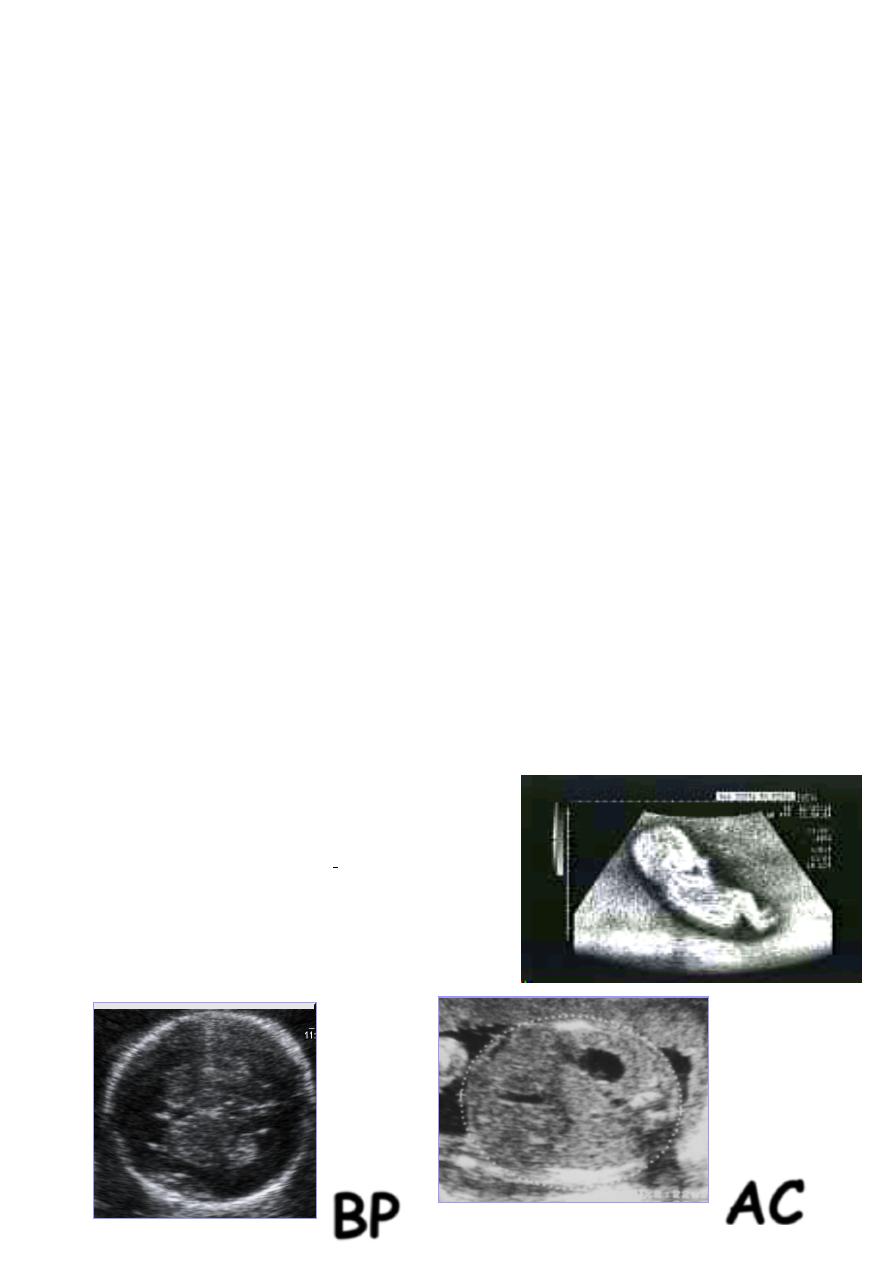
Ultrasonic estimation of EDC
1
st
trimester:
-The best & most accurate.
- Measure crown-rump (CRL ± 5 days).
2
nd
trimester:
- (BPD, HC, AC, FL ± 10 days).
BP
D
AC
4
3
rd
trimester:
- Much less accurate.
Gestational age assessment: LMP and ultrasound
Pregnant women should be offered an early ultrasound scan to determine gestational age
and to detect multiple pregnancies.
Ideally, scans should be performed between 10 and 13 weeks and crown–rump length
measurement used to determine gestational age.
Benefits of a dating scan:
1. Accurate dating in women with irregular menstrual cycles or poor recollection of LMP
2. Reduced incidence of induction of labour for prolonged pregnancy
3. Maximizing the potential for serum screening to detect fetal abnormalities
4. Early detection of multiple pregnancy
5. Detection of asymptomatic failed intrauterine pregnancy
Booking History
1. Past Medial History
2. Past Obstetric History
3. Previous Gynaecological History
4. Family History
5. Social History
Past medical history
Taking a detailed history about any previous medical illness is important as:
The disease and its treatment may adversely affect the growth of the fetus
There may be an associated increased risk of placental dysfunction
Pregnancy may cause improvement or deterioration in the medical illness
FL

5
Major pre-existing diseases that impact on pregnancy:
Diabetes mellitus
Hypertension
Renal disease
Epilepsy
Venous thromboembolic disease
Human immunodeficiency virus (HIV) infection
Connective tissue disease
Past obstetrical history
1- Details of previous pregnancy complications. The features that are likely to have
impact on future pregnancies include:
recurrent miscarriage (increased risk of miscarriage, intrauterine growth restriction
(IUGR)),
preterm delivery (increased risk of preterm delivery),
early onset pre-eclampsia (increased risk of pre-eclampsia/ IUGR),
abruption (increased risk of recurrence),
congenital abnormality (recurrence risk depends on type of abnormality),
macrosomic baby (may be related to gestational diabetes),
IUGR (increased recurrence),
Unexplained stillbirth (increased risk of gestational diabetes)
2- Details of previous labours and deliveries
Previous gynecological history:
Previous history of infertility or recurrent abortion
Previous history of cone biopsy as it may cause cervical incompetence or stenosis
Previous history of myomectomy as it increase risk of uterine rupture during labour
Family history:
Important areas are a maternal history of a first degree relative (sibling or parent) with:
diabetes (increased risk of gestational diabetes),
thromboembolic disease (increased risk of thrombophilia, thrombosis),
preeclampsia (increased risk of preeclampsia),
psychotic psychiatric disorder ( increased risk of puerperal psychosis).

6
For both parents, it is important to know about any family history of baby with congenital
abnormality and any potential genetic problems, such as haemoglobinopathies.
Social history:
Smoking and drug abuse
Social deprivation
Domestic violence
The booking examination
Historically, a full physical examination (CVS, RS, abdominal, pelvic and breast
examination) was carried out at the booking visit. The value of this has been
questioned, as the detection of significant pathology in the absence of focal symptoms
is uncommon.
For most healthy women without complicating medical problems, the booking
examination will include the following:
Accurate measurement of blood pressure.
Abdominal examination for the size of the uterus.
Recognition of previous abdominal scars.
Measurement of height, weight and estimation of BMI.
Urine examination to look for asymptomatic bacteriuria
Booking investigation
Full blood count; this Screens for anaemia and thrombocytopenia. Anaemia in
pregnancy is most frequently caused by iron deficiency, however, other causes must
be considered, especially if the Hb level is <9.0g/dl.
Blood group and red cell antibodies,
Hepatitis B; vertical transmission to the fetus may occur, mainly during labour.
human immunodeficiency virus
syphilis
haemoglobin studies; test for haemoglobinopathies for women with family history of
it
gestational diabetes; screening for gestational diabetes in those with risk factors at 28
weeks gestation
7
Screening for fetal abnormalities
It is a routine aspect of antenatal care, offered to all pregnant women at 11 and 22 weeks
gestation and includes:
nuchal translucency scanning (11-13 weeks), or serum screening (15-19 weeks) for
down's syndrome
maternal serum alpha-fetoprotein (15-19 weeks) for neural tube defects
detailed or anomaly ultrasound scan (19-22 weeks), for structural congenital
abnormalities
Follow-up visits
For those with normal pregnancy and normal past obstetrical history should have:
4 weekly appointment from 20 - 32 weeks
Fortnight visits from 32 - 36 weeks
Weekly visit from 36 weeks and on
The minimum number of visits recommended by the royal college of obstetricians and
gynecologist is 5, occurring at 12, 20, 28-32, 36, 40-41 weeks
For high risk pregnancy more frequent visits
Contents of follow up visit
In every visit the following should be carried out:
Asking about maternal well being
Fetal movements
Measurement of blood pressure
Urinanalysis for infection, protein, blood, and glucose
Examination of oedema especially the face and hands
Abdominal palpation for fundal height (symphysis fundal height assessment)
Fetal heart auscultation
The following are carried out in addition to the above:
Full blood count and red cell antibody screen → 28 and 36 weeks
Gestational diabetes screening → 28 weeks
The lie and presentation of the fetus → 36 weeks
Iron supplementation to prevent iron deficiency anaemia
Prophylactic anti-D for Rh negative women at 28 and 34 weeks

8
Pre-conceptual counselling
Pre-conceptual counselling is helpful in a wide variety of circumstances. There is potential for
general advice, an opportunity to plan care in those with background medical disease, a
chance to review those with previous obstetric complications and a discussion with those at
increased risk of fetal anomaly.
Medical
Chronic maternal disease may have a deleterious effect on fertility that may lessen as the
disease process itself improves. Maternal disease can affect the fetus, and the pregnancy
itself may affect the disease. E.g. SLE, Diabetes, HIV, Renal disorders, Thromboembolic
disease and Thyroid disorders.
It is rare to advise against pregnancy in those with cardiac disease, although those with fixed
pulmonary output may be advised that the risks to their own health are too great (e.g. in
those with pulmonary hypertension).
Those on warfarin for valvular problems or venous thromboembolic disease are at increased
risk of teratogenic problems (particularly midfacial hypoplasia). Consideration should be
given to timing of pregnancy and whether a change to heparin, at least in very early
pregnancy, is appropriate.
As anticonvulsants for epilepsy may also be teratogenic, seizure control with a single drug
regime is ideal or, if seizure-free for 2-3 years, drug withdrawal may be considered (this may
have implications for the patient's work and/or driving licence). Pre-conceptual folate
supplements should be given because anticonvulsants lead to a reduction in serum folate.
Obstetrics
It is also an opportunity to identify those with abnormal grief reactions who might benefit
from further counselling before considering another pregnancy.
Pre-eclampsia tends to improve with subsequent pregnancies, with the possible exception of
severe pre-term disease. The incidence of proteinuric pre-eclampsia in a second pregnancy
is 10-15 times greater if there was preeclampsia in the first pregnancy compared to those
with a normal first pregnancy. It has been suggested that low-dose aspirin taken from early
pregnancy (< 17 weeks and probably from the first trimester) may reduce the incidence of
IUGR or perinatal mortality in those with previous severe disease. Studies in this area have
provided conflicting evidence.
Those who have had a previous difficult instrumental delivery usually have a much more
straightforward delivery next time around, but may occasionally request an elective
caesarean section. This is controversial, and careful consideration of the advantages and
disadvantages is required. In general, those with a previous caesarean section for a non-
recurrent indication, e.g. breech, fetal distress or relative cephalopelvic disproportion

9
secondary to fetal malposition, should be offered a trial of labour, but repeat elective
caesarean section may be considered in certain circumstances.
In situations where there has been previous IUGR or an intrauterine death, subsequent
management depends on the cause and the estimated likelihood of recurrence. More
intensive antenatal monitoring is usually offered and the outcome is usually good,
particularly when the loss was 'unexplained'.
Risk of fetal anomaly
Those who have had a previous baby with a fetal anomaly are often anxious to know the risk
of this happening again and whether any prenatal testing can be carried out. This discussion
has usually taken place after the problem pregnancy, but further discussion is sometimes
welcomed.
A couple who have had a previous Down's syndrome baby, or fetal loss from Down's
syndrome, carry a risk of 0.75% above their baseline age-related risk. Down's, however, may
rarely also be inherited from a parental translocation (e.g. 14:21) or mosaicism, which
increases this recurrence risk significantly. The complexities of these issues often require
specialist advice from a clinical geneticist.
This also applies to many other abnormalities, for example congenital heart disease: while in
general the recurrence risk of this is ~ 5%, it is dependent on the family history, drug history
and whether the anomaly was isolated or part of some other syndrome.
Other structural abnormalities, for example Potter's syndrome or diaphragmatic herniae,
usually carry a low recurrence risk.
There may be a family history of certain conditions, and others have a racial predisposition,
e.g. Tay-Sachs disease in Ashkenazi Jews or haemoglobinopathies in those of Mediterranean
origin. Invasive fetal testing may be appropriate after parental gene testing if both partners
are homozygous for a recessive condition.
Lifestyle education
Smoking
Alcohol and drug misuse
Those whose work environment exposes them to radiation, hazardous gases or
specific chemicals should be appropriately counselled.
Moderate exercise is likely to be of benefit and should be encouraged, but should
probably be avoided if there are complications, e.g. hypertension, multiple
pregnancy, cardiorespiratory compromise, antepartum haemorrhage or preterm
labour.
