1
Forth stage
Obstetric
Lec-2
.د
امنة
1/1/2016
Post-partum haemorrhage (PPH)
Definitions
Primary post-partum haemorrhage; is defined as loss of blood estimated to be >500 ml in NVD &> 1000 ml
in CS within 24 hr.s of delivery.
Secondary post-partum haemorrhage; is defined as abnormal vaginal bleeding, from 24 hr.s after delivery
to 6 wks post partum.
Primary PPH
Aetiology .(4T.s)
1-Tone…uterine atony, the commonest cause.70%
2-Tissue…retained placenta or part of placenta.10%
3-Trauma…vulvar, cervical or vaginal lacerations or haematoma or uterine rupture.20%
4-Thrombosis…disorders of coagulation system & platelets (don't usually result in excessive bleeding).1%
Predisposing risk factors
A-Factors relating to pregnancy (Antenatal)
1-antepartum haemorrhage.
2-placenta previa.
3-multiple pregnancy, polyhydronnios.
4-hypertensive disorders.
5-grand mutipatity
6-previous PPH
7-obesity (risk of atonic uterine hemorrhage rapidly increased with increasing BMI).
8-fibroid
9-big baby >4kg.
B-Factors relating to delivery (Intrapartum)
1-CS
2
2-prolonged labour.
3-retained placenta, placenta accreta.
4-delay in progress of second stage.
5-instrumental delivery.
6-precipitate labour.
7-laceration
C-pre-existing maternal haemorrhagic conditions
1-carrier haemophilia A
2-carrier haemophilia B
3-Von Willbrands disease.
Assessment of patient with PPH (Diagnosis)
History & examination
...continuous bleeding which fail to stop after delivery of placenta (third stage).
...feeling unwell &/or fainting.
...pallor, cold extremities
...hypotension &/or tachycardia (if blood loss of > 1000ml).
...agitation &/or confusion.
...examination of lower genital tract
Management
1-recognition
Assessment of ongoing blood loss is an essential aspect of post-partum care. Clinical sign of shock or
tachycardia should prompt a full assessment of mother.
2-communication
The successful management of PPH require a good team approach. Senior obstetric & mid wifery staff will
be needed in first instances, but other clinicians such as anasthetists, haematologists or transfusion
specialists, intensivists & sub-specialty surgeons may be called in case of more serious haemorrhage. Also
communication with patient & their support person is important.

3
3-resuscitation
*immediate call for help.
*assessment of airway & breathing initially with administration of high flow O2.
*wide bore IV access should be established with blood sent for full blood count, cross match & coagulation
profile.
*rapid infusion of fluids once IV access is achieved.
*the use of group specific or group O Rh negative blood should be considered early to restore O2 carrying
capacity with infusion of colloid or crystalloid
*additional measures such as keeping the woman warm & positioned flat or head tilt down.
*IV antibiotics
4-monitoring & investigation
The haematological investigation, pulse rate, bl.p., O2 saturation, urinary output measurement should be
done if there is PPH., & invasive monitoring of arterial blood pressure or CVP may be necessary depending
on clinical situation.
5-treatment
To manage the case of PPH, you should identify the causes commonly known as (4 T.s).
¤¤¤Mechanical & medical
A.Tone...uterine atony is the most common cause of primary PPH., the following interventions have all
been used to stop bleeding
a-mechanical..uterine message or bimanual uterine compression+empty of bladder.
WHO has recommended non-pnematic anti-shock garment (NASG) to help until other measures carried
out.
Fig.1
(a) uterine massage
(b) bimanual compression

4
b-pharmacological..
.....Oxytocin (syntocinon ) 5 units by slow IV injection if already administered for the 3rd stage of labour, a
repeated dose may be given. Or 40 units in 500 ml Hartmann's solution at 125 ml/hr.
.....Ergometrine 250 mcg by slow iv.or im.injection, repeated if necessary up to a maximum of 1000 mcg if
there is no contraindication.
.....Misoprostol (1000mcg ) rectally once only.
.....Prostaglandin F2 alfa & it's analogues but have serious side effect include sever hypertension &
bronchospasm as Dinoprost 500 mcg i.m. or intra-myometrially or Carboprost (prostin) 250 mcg i.m.
B.Trauma of genital tract...full assessment of entire genital tract is essential. The perineum, vagina & cevix
should be inspected for bleeding sources. Pressure should be applied to bleeding area & repaire
attempted. If the patient is shocked & the amount of vaginal bleeding is normal, conside intra-abdominal
sources as rupture uterus, broad ligament hematoma, subcapsular liver rupture, rupture spleen.
C.Tissue... (retained products of conception) usually due to retained placenta, cotyledon or membrane.
Examine mother vaginally to assess the adherence of placenta, if adherent, repeated oxytocin dose+ empty
the bladder+transfer the patient to theatre for manual removal of it.
D.Thrombin... (abnormalities of coagulation ) it's rarely the primary cause of PPH.
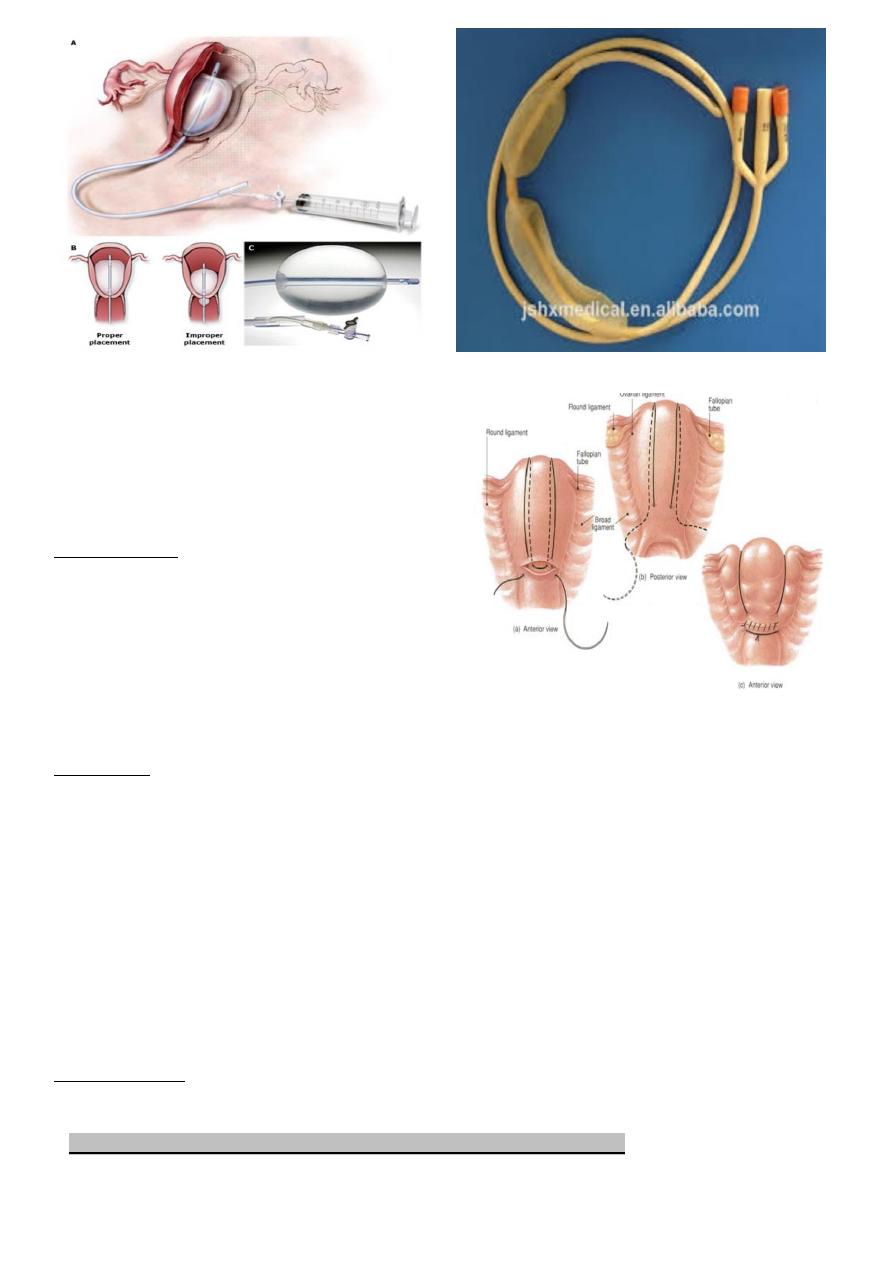
¤¤¤Surgical
Surgical interventions should be initiated sooner as hysterectomy in case of rupture uterus, placenta
accreta or uncontrolled massive bleeding. The following procedures avilable are;
a-balloon tamponade as (Foley catheter or Bakri balloon or Sengstaken Blakmore catheter)
b-haemostatic uterine brace suturing (B-Lynch suture ) to anterior & posterior uterine walls has been
shown to be effective with reports of successful pregnancy following it.
c-bilateral ligation of uterine arteries.
d-bilateral ligation of internal iliac arteries.
e-selective arterial embolization.
f-hysterectomy.
5
Fig2
(a) Bakri balloon
(b) Sengstaken Blakmore catheter
(c) B-Lynch suture
Complications
-Shock
-Collapse
-DIC
-Sheehan syndrome.
-Maternal mortality.
Prevention
*be aware of risk factors
*treat anaemia antenatally
*Active management of the third stage of labour.
*Prophylactic oxytocin should be routinely used in the third stage to decrease the risk of PPH. & it's
preferred in patient with hypertension. Syntometrine (ergometrine 0.5 mg+5 IU oxytocin) is the drug of
choice.
*nipple stimulation & breast feeding triggers the release of natural oxytocin in the body.
Secondary PPH
Aetiology
1-subinvolution of uterus due to retained placental tissue &/or endometritis (1-3% after spontaneous
vaginal delivery).

6
2-Lower genital tract laceration/ hematoma.
3-Surgical injury.
4-Dehiscence of CS scar.
5-Coagulopathy/ bleeding disorder.
Infection is the most common cause of post natal morbidity between day 2 & day 10.
Endometritis risk factors
-CS
-Prolonged rupture of membranes
-Sever meconium stained liquor
-Long labour with multiple pelvic examinations
-Manual removal of placenta
-At extremes of maternal age
-Low socio-economic status
-Maternal anaemia
-Prolonged surgery
-Internal fetal monitoring
Assessment
History... History of offensive lochia, abdominal cramping& maternal pyrexia is often present.
Examination...fever, rigor, tachycardia, uterine tenderness, enlarged uterus & open cervical os.
Investigations
*FBC
*blood culture is positive in 10-30%
C-reactive protein
*high vaginal swab
*USG in case of retained product of conception.
*duplex color Doppler.
Management
1-If bleeding mild, observation for the patient. If she continuous to bleed or has signs of infection, give her
antibiotics as combination of amoxicillin, gentamycin & metronidazole.
7
2-If bleeding is severe, she need uterotonic agents, antibiotics, resuscitation & exploration of her uterus
for retained pieces of placenta. Speculum examination will allow visualization of cervix & lower genital
tract to exclude laceration.
Oxytocin can be given as IV or IM bolus (10 units) or in combination with ergometrine IM then followed by
oxytocin infusion (40 U in 500 ml normal saline). Misoprostol can be given (400-800 mcg orally or rectally).
If clot is visible within the cervical os, it may be removed with tissue forceps.
If retained products of conception are suspected, elective curettage with antibiotic cover may be
required. If patient conditions is stable, start antibiotics for 24hrs.s before doing curretage .
Patient may require iron supplementation if Hb has fallen.
If the uterus is empty & she is still bleeding severely, pack it & her vagina.
If packing of uterus fails to control bleeding, processed to laparotomy & tie her uterus or internal iliac
arteries, if this also fails (rare) do a hysterectomy.
Prognosis
For cases treated with antibiotics improve 90% within 48-72hr. If this is not the case, the patient should be
reevaluated.
