1
Forth stage
Obstetric
Lec-4
د. أحمد جاسم
17/11/2015
Marginal Haemorrhage
:
ž
Bleeding from the edge of a normally situated placenta after 24th weeks’
gestation.
:
1. Similar to that of placenta praevia.
2. Symptoms
3. Vaginal bleeding.
Signs :
• General examination:
– The general condition proportionates to the amount of bleeding as
all the blood loss is revealed
• Abdominal examination:
– No characteristic signs.
• Vaginal examination:
– Done under the same precautions in placenta praevia.
– There is vaginal bleeding and if the cervix is dilated the placenta is
not felt.
:
ž
Ultrasound reveals a normally situated placenta in the upper uterine segment
with no retroplacental haematoma.
:
• At home :
As in placenta praevia.
• At hospital
1. Assessment, resuscitation and ultrasound.
2. If the patient is not in labour:
– If the bleeding is severe ⟶ caesarean section.
– If the bleeding is slight ⟶ Gestational age is completed 37 weeks or
more termination of pregnancy by induction of labour or C.S.
If not completed 37 weeks conservative treatment is carried out as
placenta praevia till completed 37 weeks.
3. If the patient is in labour:
2
– Delivery is carried out by amniotomy + oxytocin or C.S if indicated.
:
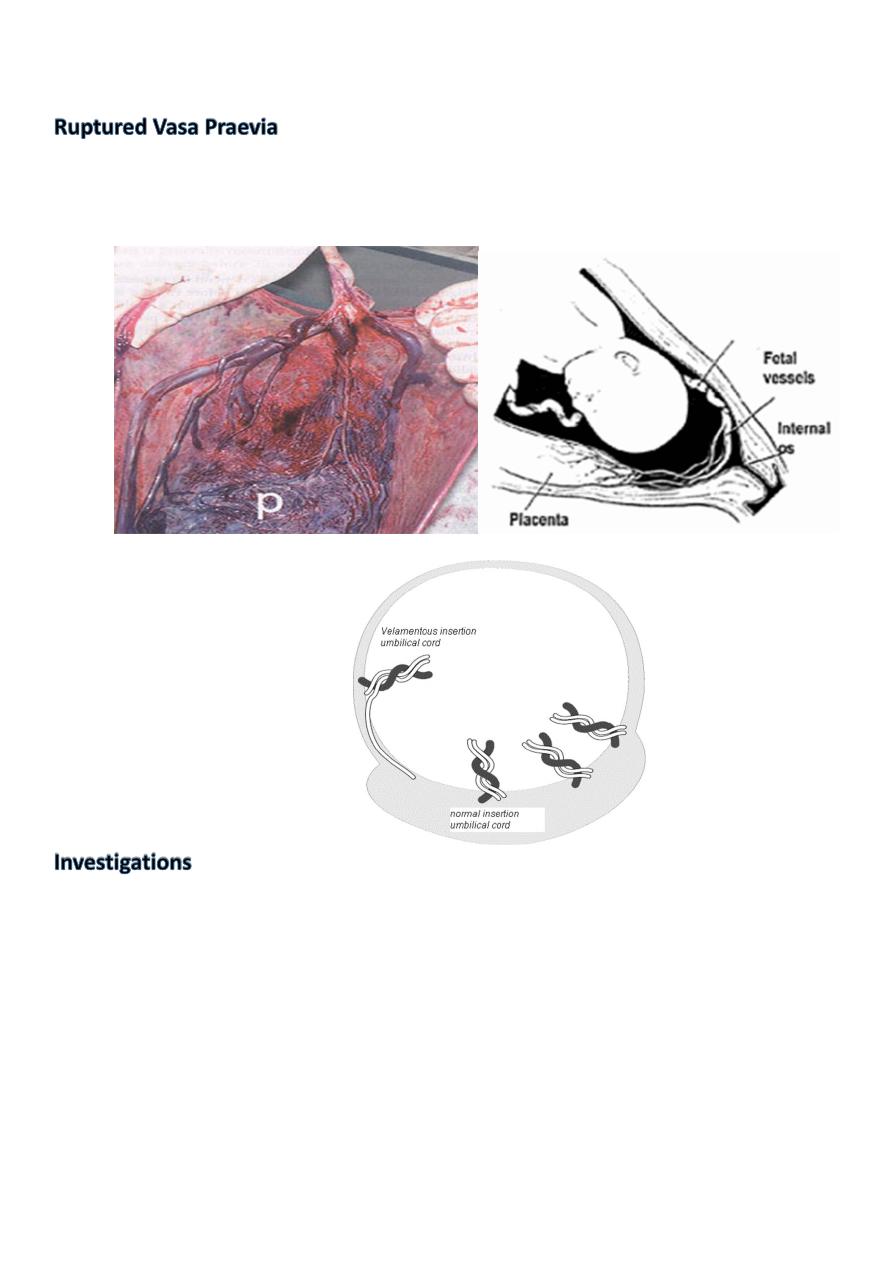
In velamentous insertion of the cord, some of the foetal vessels in the membranes cross the
region of the internal os. When the membranes ruptures, the foetal vessels are torn and
bleeding occurs which is usually slight. Foetal heart rate abnormalities are detected .
:
• The foetal blood can be detected by:
1. Apt’s test: 4-6 drops of the antepartum haemorrhage blood is added to 10 ml of
water then 2 ml of sodium hydroxide is added. The foetal blood remains red/ pink
for at least 2 minutes and turns green/brown after 10-20 minutes due to
resistance to alkali in formation of alkaline haematin. If the blood is maternal in
origin it turns green/ brown within 10 seconds.
2. Spectrophotometer: Foetal haemoglobin shows different ultraviolet absorption
than adult haemoglobin.
3. Blood film: Foetal RBCs can be detected by a special cytochemical stain and it may
be nucleated.
3
:
Immediate caesarean section.
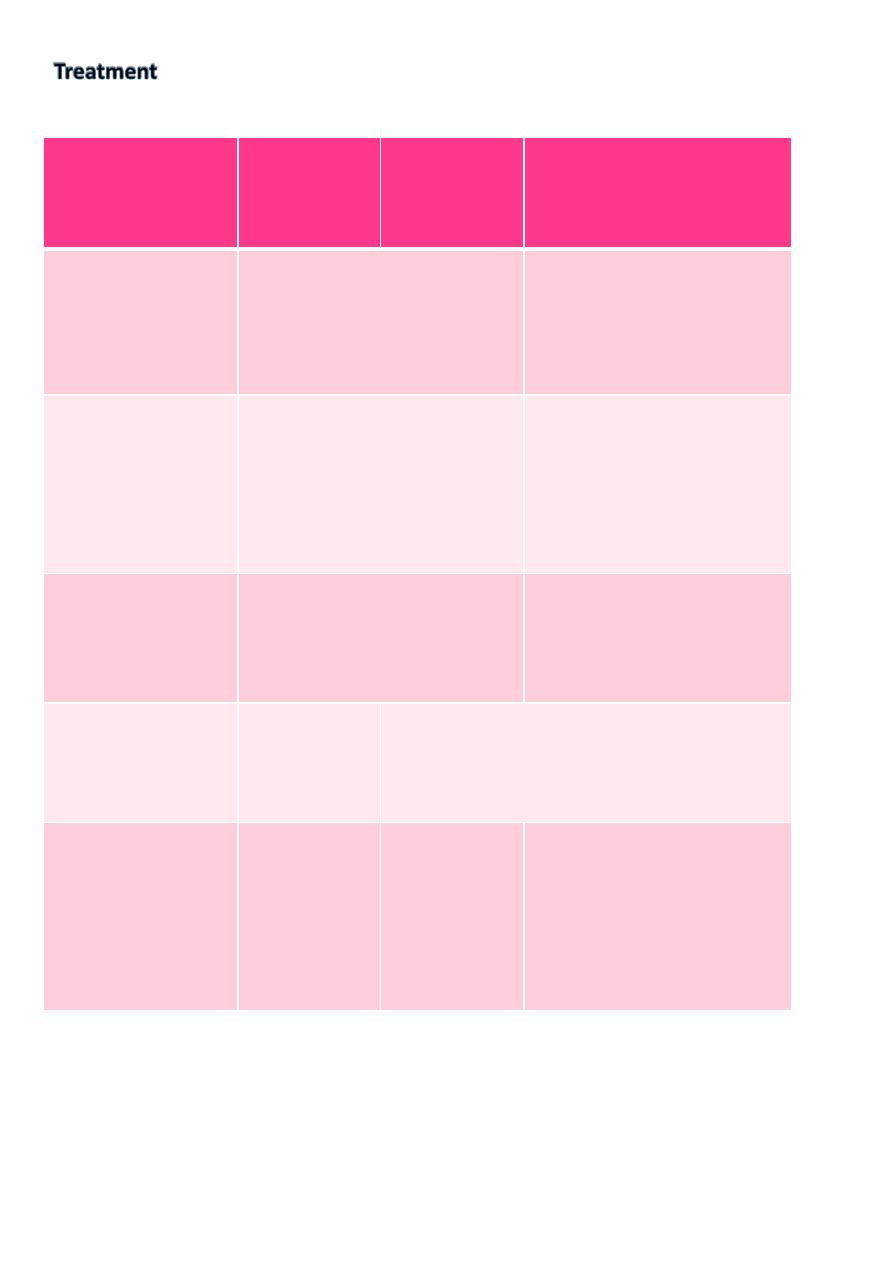
Placenta
Praevia
Marginal
Haemorrhage
Abruptio
Placentae
(I) History:
Bleeding
- Painless, causeless,
recurrent.
- Usually starts slight
in amount.
- Associated with
abdominal pain.
- A cause may be
detected.
- Usually starts severe in
amount.
(II)
Examination:
1) General
- The degree of shock is
proportionate to the amount
of blood loss.
- Hypertension usually not
present.
- The degree of shock may
be out of proportion to
amount of blood loss.
- Hypertension usually
present.
(2) Abdominal
- Uterus
- Foetus
- FHS
- No tenderness or hardness.
- Easily felt.
- Usually normal.
- Tender, hard.
- Not easily felt.
- Absent or distressed.
(3) Vaginal (with
the precautions)
- Bleeding
- Placenta
- Bright red.
- Can be felt
- Dark red.
- Not felt.
(III) Investigations
- Urine
- Blood
- Ultrasound for
placenta
- Normal.
- Normal.
- In lower
segment.
- Normal.
- Normal.
- In upper
segment.
- Proteinuria.
- DIC may present.
- In upper segment +
retroplacental haematoma
may present.
