
1
Forth stage
Obstetric
Lec-1
د . سجى
1/1/2014
OBSTETRIC SHOCK
Shock is a condition resulting from inability of the circulatory system to provide the tissues
requirements from oxygen and nutrients and to remove metabolites.
TYPES
1-Haemorrhagic shock
excessive blood loss may be due to:
• bleeding early in pregnancy.
• antepartum haemorrhage.
• postpartum haemorrhage.
2-Neurogenic shock
painful conditions my be due to:
1. ectopic pregnancy.
2.Concealed accidental haemorrhage.
3.Forceps or breech extraction before full cervical dilatation.
4.Rough internal version.
5.Rupture uterus.
6.Acute inversion of the uterus.
7.Rapid evacuation of the uterine contents as in precipitate labour and rupture of
membranes in polyhydramnios. This is accompanied by rapid accumulation of blood in the
splanchnic area due to sudden relief of pressure (splanchnic shock).
3-Cardiogenic shock
ineffective contraction of the cardiac muscle due to
1.Myocardial infarction.
2.Heart failure.
4-endotoxic shock
generalised vascular disturbance due to release of toxins.
5-anaphylactic shock
caused by sensitivity to drugs.
2
6-others
• Embolism: amniotic fluid, air or thrombus.
• Anaesthetic complications: as Mendelson's syndrome.
• The shock may be caused by more than one factor as:
1. Incomplete abortion: leads to haemorrhagic and endotoxic shock.
2. Disturbed ectopic and rupture uterus: lead to haemorrhagic and neurogenic shock.
clinical presentation:
• Low blood pressure.
• Rapid weak (thready) pulse.
• Pallor.
• Cold clammy sweat.
• Cyanosis of the fingers.
• Air hunger.
• Dimness of vision.
• Restlessness.
• Oliguria or anuria

3
Tilt test :
• It is done in patient with considerable bleeding but the blood pressure and/ or pulse rate
are normal.
• When this patient is in a sitting position, she develops hypotension and / or tachycardia.
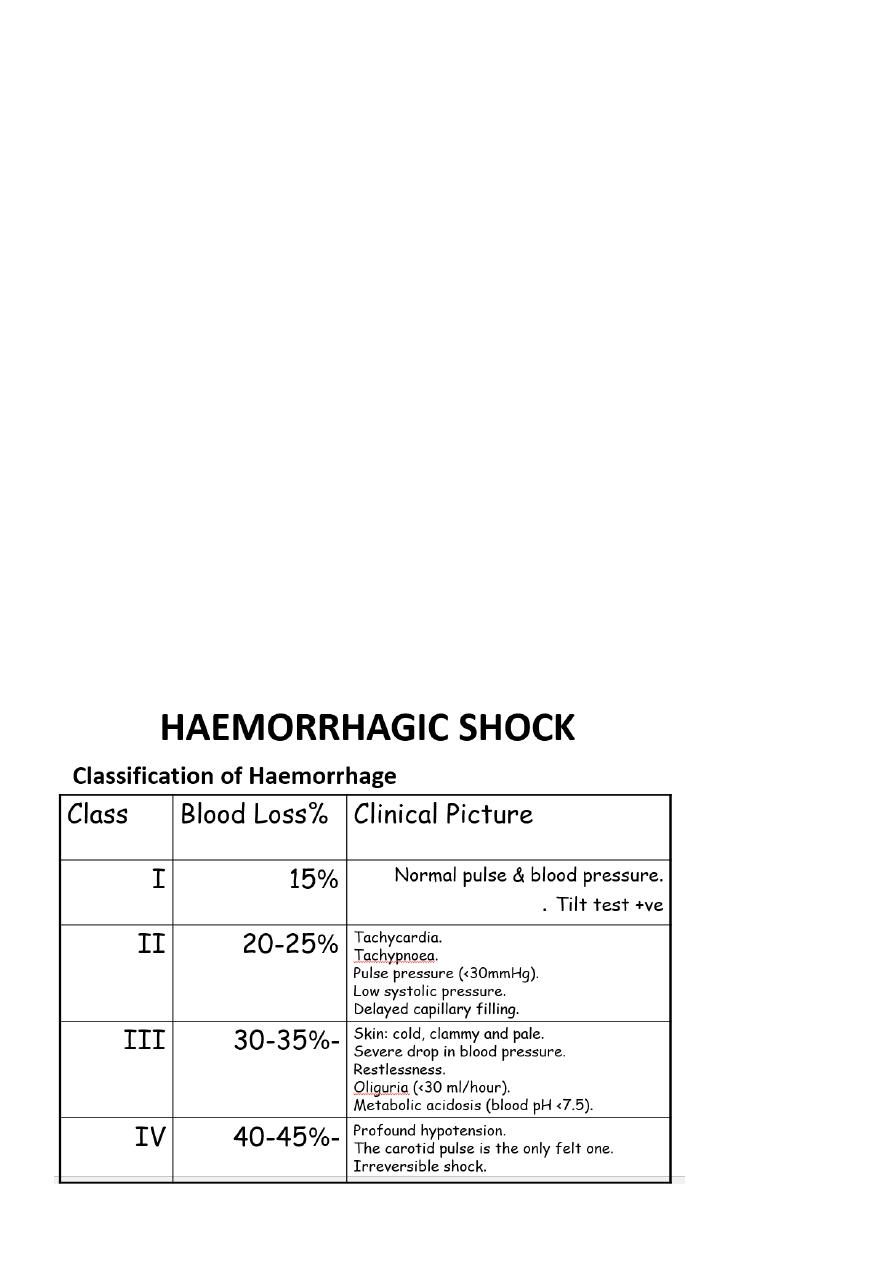
STAGES OF HAEMORRHAGIC SHOCK
The normal pregnant woman can withstand blood loss of 500 ml and even up to 1000 ml
during delivery without obvious danger due to physiological cardiovascular and
haematological adaptations during pregnancy.
Stage of compensation :
• Sympathetic stimulation: It is the initial response to blood loss leading to peripheral
vasoconstriction to maintain blood supply to the vital organs.
• Clinical picture: Pallor, tachycardia, tachypnoea.
Stage of decompensation :
1. Blood loss exceeds 1000 ml in normal patient or less if other adverse factors are
operating.
2. Clinical picture: is the classic clinical picture of shock (see before).
3. Adequate treatment at this phase improves the condition rapidly without residual
adverse effects.
stage of cellular damage&danger of death :
Inadequately treated haemorrhagic shock results in prolonged tissue hypoxia and damage
with the following effects:
1. Metabolic acidosis
2. Arteriolar dilatation
3. Disseminated intravascular coagulation
4. Cardiac failure
5. In this phase death is imminent, transfusion alone is inadequate and if recovery
from acute phase occurs residual tissue damage as renal and/ or pituitary necrosis
will occur.
4
Management :
1. Establish an airway and give oxygen by mask or endotracheal tube.
2. Elevate the legs to encourage return of blood from the limbs to the central circulation.
3. Two or more intravenous ways are established for coagulation screen,blood
group&cross match.thereafter blood, fluids and drugs infusion which should be given by
IV route in shocked patient. If the veins are difficult to find a venous cut down or
intrafemoral canulation is done.
4. Detect the cause&arrest bleeding
• Restoration of blood volume by:
1. Crystalloid solutions: as ringer lactate, normal saline or glucose 5%. They have a short
half life in the circulation and excess amount may cause pulmonary oedema.
2. Colloid solutions: as dextran 40 or 70, plasma protein fraction or fresh frozen plasma
3. Whole blood: cross-matched from the same group if not available group O-ve may be
given as a life -saving.
• drugs
1. Analgesics: 10-15 mg morphine IV if there is pain, tissue damage or irritability .
2. Corticosteroids: Hydrocortisone 1gm or dexamethasone 20 mg slowly IV. Its mode of
action is controversial; it may decrease peripheral resistance and potentiate cardiac
response so it improves tissue perfusion .
3. Sodium bicarbonate: 100 mEq IV if metabolic acidosis is demonstrated .
4. Vasopressors: to increase the blood pressure so maintain renal perfusion .
1. Dopamine: 2.5m g/ kg/ minute IV is the drug of choice .
2.
ß -adrenergic stimulant: isoprenaline 1mg in 500 ml 5% glucose slowly
IV
infusion .
Monitoring :
1. Central venous pressure (CVP): normal 10-12 cm water.
2. Pulse rate.
3. Blood pressure.
4. Urine output: normal 60 ml/hour.
5. Clinical improvement in the: pallor, cyanosis, air hunger, sweating and consciousness

5
Complications :
• Acute renal failure .
• Pituitary necrosis (Sheehan’s syndrome).
• Disseminated intravascular coagulation .
ENDOTOXIC SHOCK (septic or bacteraemic shock)
Obstetric Causes
1. Septic abortion .
2. Prolonged rupture of membranes .
3. Manipulations and instrumentations .
4. Trauma .
5. Retained placental tissues .
6. Puerperal sepsis .
7. Severe acute pyelonephritis .
Causative Organisms
1. Gram-negative bacilli: E.coli, proteus, pseudomonas and bacteroids. The endotoxin is a
phospholipopolysaccharide released by lysis of its cell envelope .
2. A similar picture is produced from exotoxin of ß-haemolytic streptococci, anaerobic
streptococci and clostridia .
clinical presentation :
A-Reversible stage It has 2 phases:
1-Early (warm) phase:
hypotension,
tachycardia,
pyrexia,
rigors,
flushed skin,
patient is alert,
leucocytosis develops within hours.

6
2-Late (cold) phase:
cold and clammy skin,
mottled cyanosis,
purpura,
jaundice,
progressive mental confusion,
coma.
B-Irreversible stage
Prolonged cellular hypoxia leads to:
1. metabolic acidosis,
2. acute renal failure,
3. cardiac failure,
4. pulmonary oedema,
5. adrenal failure and ultimately death.
Management :
1-Restoration of circulatory function and oxygenation
• Replacement of blood loss: by whole blood, if not available start with colloids or
crystalloids. The CVP measurement is essential to guard against circulatory overload.
• Corticosteroids: as;
– Hydrocortisone 1gm IV / 6 hours or,
– Dexamethasone 20 mg initially followed by 200 mg/day by IV infusion.
• β-adrenergic stimulants: as isoprenaline cause arteriolar dilatation, increase heart
rate and stroke volume improving tissue perfusion. Blood volume must be normal
prior to its administration.
• Oxygen: if respiratory function is impaired.
• Aminophylline: improves respiratory function by alleviating bronchospasm.
2-Eradication of infection
• Antibiotic therapy:
• Swabs for culture and sensitivity are taken first.
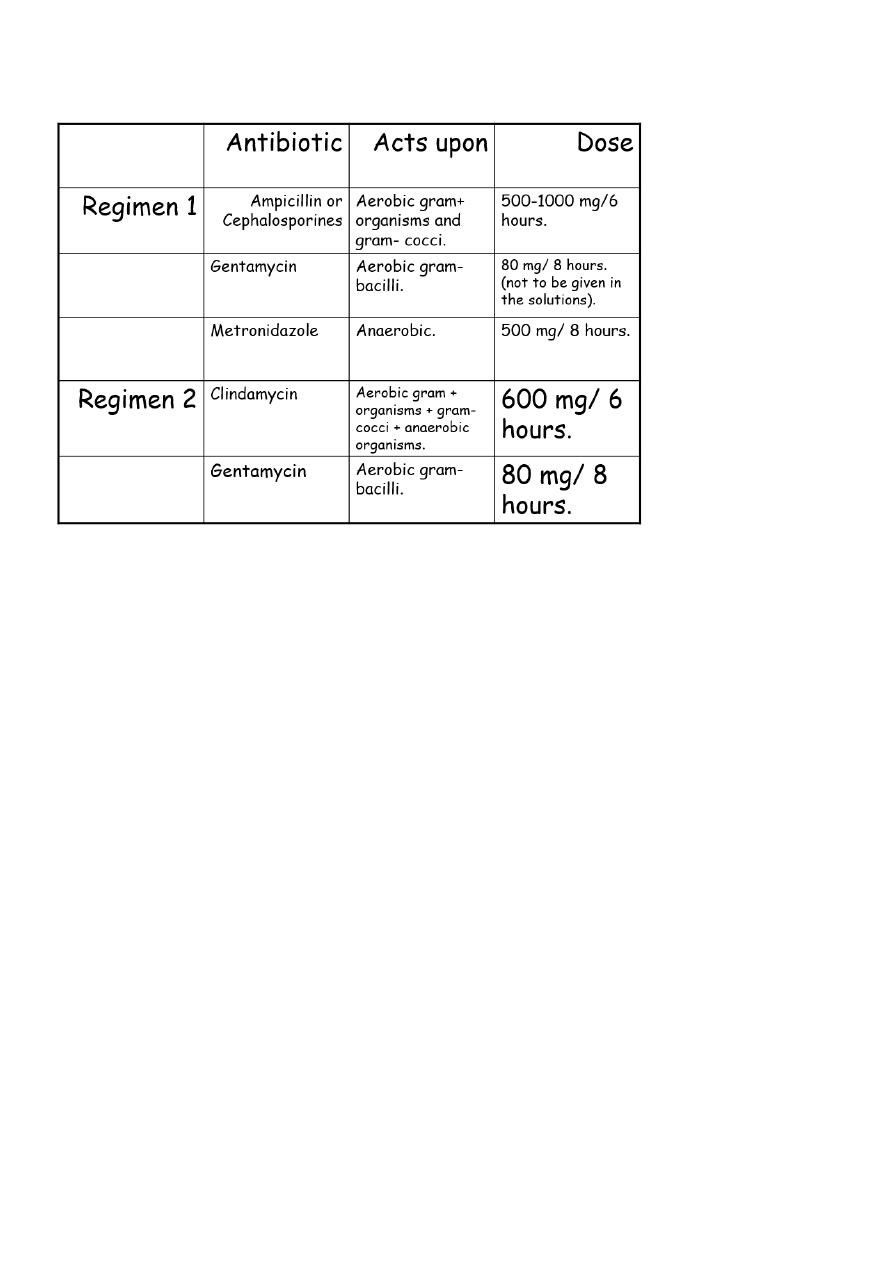
7
• Antibiotic therapy is starting immediately till the result of culture and given by IV
route. The therapy should cover the wide range of organisms:
3-Surgical treatment
is indicated when there is retained infected tissues as in septic abortion. It should be
removed as soon as antibiotic therapy and resuscitative measures have been started by:
• suction evacuation,
• digital evacuation, or
• hysterectomy in advanced infection with a gangrenous (clostridium welchii) or
traumatised uterus.
AMNIOTIC FLUID EMBOLISM :
Definition : Passage of amniotic fluid into the maternal circulation leads to sudden collapse
during labour but can only be confirmed at necropsy.
Pathology :
The condition is more common with strong uterine contraction, whether spontaneous or
induced, occurs after rupture of membranes particularly when there are open maternal
blood vessels in the placental site or in cervical lacerations.
The embolism passes to the pulmonary vessels leads to:
• sudden death,
• shock, or
• Later death due to DIC and postpartum haemorrhage

8
Clinical presentation :
The onset is acute with sudden collapse, cyanosis and severe dyspnoea .
This is soon followed by twitching, convulsions and right side heart failure, with tachycardia,
pulmonary oedema and blood stained frothy sputum .
If death does not occur in this stage, DIC develops within 1 hour leading to generalised
bleeding .
Investigations
ECG: evidence of right side heart failure.
X-ray: non-specific mottled chest appearance.
Lung scan: with technetium-99m albumin shows perfusion defect.
Laboratory tests: evidence of DIC.
Differential Diagnosis
1. Acute pulmonary oedema .
2. Pulmonary aspiration (Mendelson’s) syndrome .
3. Other coagulation defects .
Urgent treatment :
• Oxygen: endotracheal intubation and positive pressure respiration is usually indicated as
the patient is often unconscious.
• Aminophylline
• Isoprenaline
• Digoxin and atropine
• Hydrocortisone
• Bicarbonate solution
• Low molecular weight dextran: reduces platelets aggregation in vital organs.
• Heparin: for treatment of DIC if there is no active bleeding.
• Vaginal delivery: is safer than C.S. if the baby is not yet delivered.

9
Coagulation disorders :
Normal hemostasis: requires 3 main factors:
• Vascular constriction
• Platelet aggregation and formation of platelet plug
• Fibrin formation through the coagulation system
When these factors stop bleeding, the fibrinolytic system start to remove the thrombus and
restore the vascular patency
Coagulation system during pregnancy:
Pregnancy represent a hypercoagulable state. This include the following:
1. Plasma fibrinogen concentration rises during pregnancy by about 50%.
2. Increase in factors V, VII, VIII, IX, X, XII.
Venous thromboembolism(TE)
is the most common cause of maternal death during pregnancy.It also causes significant
morbidity by the postphlebitic syndrome
The incidence of thromboembolic complications, pulmonary thromboembolism and deep
vein thrombosis presented during pregnancy is around 1 in 1000 with a further 2 per 1000
women presenting in the puerperium.
Risk factors:
A-factors related to pregnancy
1. Hypercoagulable state of pregnancy.
2. Decrease activity of naturally occurring anticoagulant.
3. Decrease fibrinolytic activity.
4. Increase tendency to venous stasis during pregnancy.
5. Operative delivery ,increasing Age and parity, ,Obesity ,restricted activity: HT, DM,
PP, multiple pregnancy, heart disease (bed rest).
11
B:factors not related to pregnancy
a. Previous TE.
b. Lupus anticoagulants, anticardiolipin antibodies, and antiphospholipid syndrome.
c. Inherited thrombophilia like antithrombin III deficiency, protein C deficiency, protein
S deficiency.
d. smoking
Clinical Features of Venous TE:
1. Superficial thrombophlebitis:
This means inflammation of a superficial vein which if extended to a deep vein it carries a
risk of PE. Active mobilization of the affected limb is encouraged to prevent DVT.
2. Deep Vein Thrombosis (DVT) :
The classical signs of DVT are leg edema, calf tenderness, and positive Homans sign, which
is calf pain on dorsiflexion of the foot, it could be asymptomatic.
3. pulmonary embolism(PE):
a. Massive PE: cyanosis, shortness of breath, chest pain, hemoptysis.
b. Small PE: transient dyspnea, tinge of cyanosis, some pleuritic chest pain, unproductive
cough, unexplained pyrexia, tachycardia, leukocytosis.
DIGNOSIS
1. Clinical features usually affects left femoral vein.
2. Investigations
a. Impedance plethysmography (IPG)
c. Dopplar US
d. Contrast venography, gold standard.
e. Iodine 125 fibrinogen
Radiological studies are contraindicated in pregnancy

11
Management of venouthromboembolism
1.
Acute phase treatment.
2. Chronic phase treatment.
Acute phase treatment:
1 Thrombolytic therapy: by streptokinase, and tissue plasminogen activaters.
2. Anticoagulants: unfractionated heparin 40,000 IU daily continuous intravenous infusion
Heparin is given for 3-7 days.
Low molecular weight heparin has replaced unfractionated heparin.
3. Surgery
Chronic phase treatment:
Warfarin which crosses the placenta.
Side effects : during pregnancy is teratogenicity and bleeding tendency in the fetus,
bleeding in the mother.
Reversal of the effect is by stopping the drug, it will take three days to reserve the action,
so we can give FFP and vitamin K.
Disseminated intravascular coagulationDIC
trigger mechanism of DIC during pregnancy:
1. Endothelial injury:
a. preeclampsia.
b. Hypovolemia.
c. septicemia
2. Release of thromboplastin as in:
a. Abruptio placentae.
b. Amniotic fluid embolism.
c. Retained dead fetus.
d. Intrauterine sepsis
e. Hydatidiform mole
f. Placenta accreta

12
3. Release of phospholipid as in:
a. Intravascular hemolysis
b. Incompatible blood transfusion
c. Large fetomaternal bleed
d. septicemia
Clinical manifestation of DIC:
1. Asymptomatic: compensated state. There is lab evidence of increased production and
breakdown of coagulation factors, as in PET and in retained dead fetus.
2. Variable degrees of thrombocytopenia as in small abruptio placentae and in severe PET.
3. Massive uncontrollable hemorrhage as abruptio placentae, amniotic fluid embolism and
eclampsia.
Management:
1. Fluid replacement to avoid renal shut down usually by simple crystalloid eg
Hartmanns solution 2-3 times the estimated volume blood loss.
2. FFP which contains all coagulation factors
3. Fresh blood transfusion
