
1
Forth stage
Obstetric
Lec-3
د . سجى
1/1/2014
The neonate
The baby in the first 4 weeks of life is called a neonate
Resuscitation :
Babies fall into one of three categories within a minutes of birth:
Well, healthy and vigorous. The child has a good respiratory effort, is pink centrally, and
the heart rate is >100 bpm. This infant can be wrapped up in a warm towel and given back
to his mother. Do not suck him out; this risk producing a vagal bradycardia and cools him.
Cyanosed, poor respiratory effort, with or without a heart rate <100 bpm. Dry the baby
and place him under a radiant heat source wrapped in a warm, dry towel. Drying often
provide enough stimulation to induce breathing, but gentle rubbing can also be used. If
there is no response, begin active resuscitation using inflation breath via a bag and mask
Pale, apnoeic or terminal gasp, with absent heart beat or profound bradycardia (<60
bpm). These babies are usually completely floppy. This baby is in need of prompt
resuscitation and will not recover without it.
Dry him quickly, place him on the resuscitation surface in a warm, dry towel and call for
help.
Initiate basic resuscitation with mask ventilation.
If the heart rate remains < 60 bpm, commence chest compressions.
If there is not a rapid response, proceed to intubation as soon as a person with a necessary
skill arrives
The Apgar score
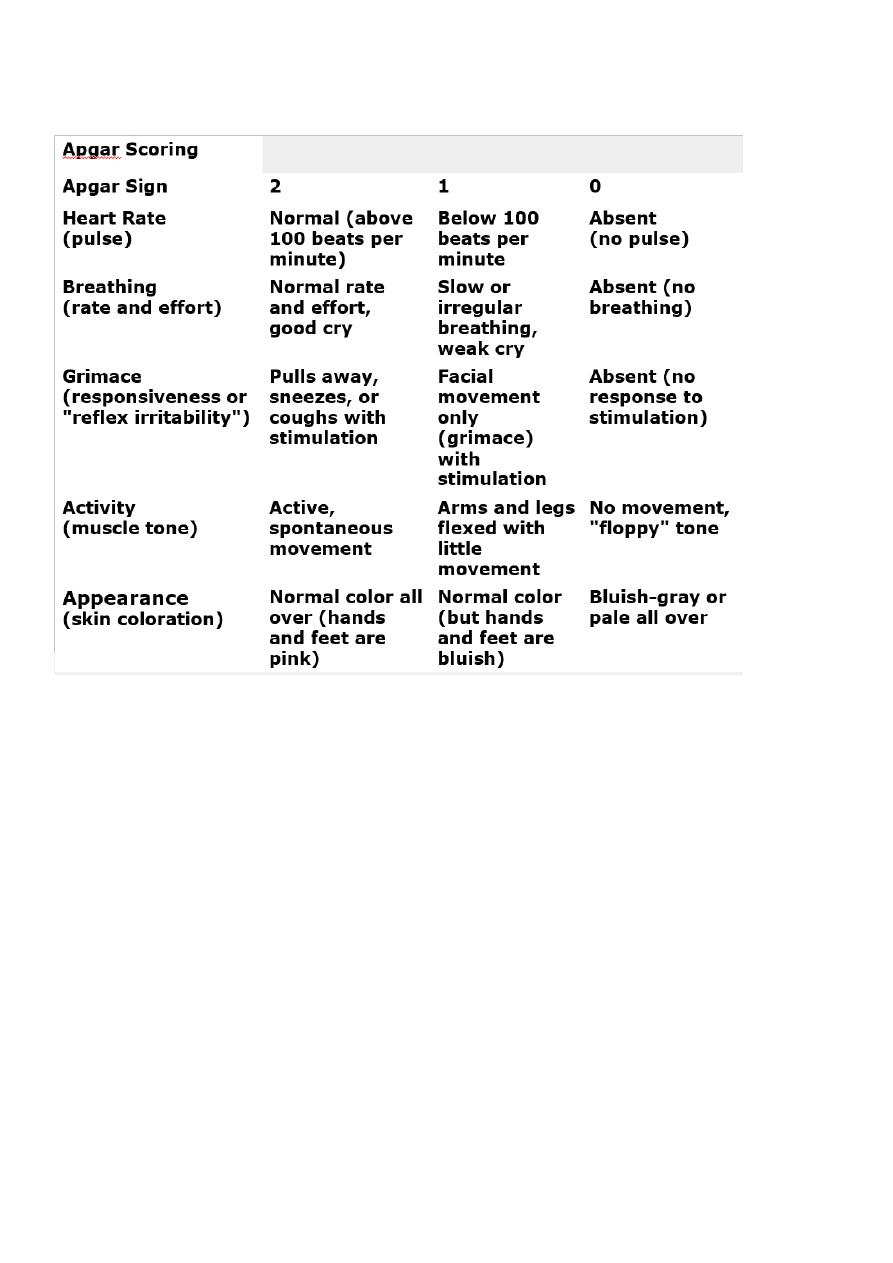
Assessment (and reassessment) is vital to a successful outcome. Many workers use the
Apgar score to aid them.
Apgar score are carried out at 1 minute and 5 minutes of life. Further score may be carried
at 5 minute intervals depending on subsequent progress
Five factors are used to evaluate the baby's condition and each factor is scored on a scale of
0 to 2, with 2 being the best score:
activity and muscle tone
pulse (heart rate)
grimace response (medically known as "reflex irritability")
2
appearance (skin coloration)
respiration (breathing rate and effort)
Normally the Apgar score is of 7 to 10. Infants with a score between 4 and 6 have moderate
depression of their vital signs while infants with a score of 0 to 3 have severely depressed
vital signs and are at great risk of dying unless actively resuscitated.
WHAT CAUSES A LOW APGAR SCORE?
Fetal distress due to hypoxia
Maternal anaesthesia or recent analgesia.
Preterm infant.
Difficult or traumatic delivery.
Excessive suctioning of the pharynx after delivery.
Severe respiratory distress.
Deliveries at which a trained neonatal resuscitator should be present
Preterm deliveries
Vaginal breech deliveries
Thick meconium staining of the amniotic fluid

3
Significant fetal distress
Significant antepartum haemorrhage
Serious fetal abnormality (e.g. hydrops, diaphragmatic hernia)
Rotational forceps or vacuum deliveries
Caesarean section – unless elective and under regional anasthesia
Multiple delivery
Care of the normal term newborn baby:
A suggested order of examination is as follows
Ask the mother about any antenatally diagnosed problems that may need follow up, and
any family problems (deafness, dislocation of hips). Check for risk factors that
predispose to neonatal sepsis, such as pyrexia in labour.
Remove the baby clothes except the nappy; look at the skin.
Feel the anterior fontanel for tension; palpate the sutures (craniosynostosis is a disorder
with premature fusion of the sutures); check the scalp for swellings (a
cephalhaematoma is the most common).
Measure the head circumference
Look at the face for colour (cyanosis/ pallor / jaundice).
Listen to the heart and estimate the heart rate – normally 110 – 150 bpm, but can drop
to 80 bpm in sleep.
Count the respiratory rate – normally <60 breaths per minute.
Palpate the abdomen, feeling for masses, including large bladder or kidneys.
Examine the eyes, checking that it is possible to obtain a red reflex using an
ophthalmoscope to exclude cataract.
Examine the ear, nose and mouth (cleft palate)
Examine the neck including the clavicle
Examine the arms, hand, legs and feet.
Remove the nappy.
Feel for femoral pulses.
Examine the genitalia and anus
Turn the baby to the prone position and examine his back and spine; assess tone.
Return the infant to the supine position and evaluate the central nervous system.
Examine the hips

4
The aims of the neonatal examination
Diagnosis of congenital malformations (present in about 10 – 15 per 1000 babies).
Diagnosis of common minor problem with advice about management or appropriate
reassurance if no intervention is indicated (e.g. Mongolian blue spot, jaundice, naevi)
Continuing screening, begin antenatally, to identify those babies who should be offered
specific intervention, e.g. hepatitis vaccination.
Health education advice, e.g. regarding breast feeding, cot death prevention, immunization
General parental reassurance
Common neonatal complications presenting in the first 24 hours :
Transient tachypnoea of the newborn:
Is the commonest respiratory disease of term infant.
The disease is due to delayed clearance of lung liquid and is much more common after
caesarean section delivery, particularly without labour.
At term, the incidence falls between 37 and 40 weeks.
The baby will have grunting (noise made by forced expiration against closed epiglottis) and
tachypnoea
These signs usually appear within the first few hours after birth and settle within 24 – 48
hours.
It must be remembered that this is a diagnosis of exclusion. More serious condition such as
sepsis or pneumothorax should be excluded.
Fortunately, the disease is usually mild, but sometimes requires intubation and ventilation,
with the associated risk of complications.
Hypoglycemia:
The importance of hypoglycemia is to identify and treat the ‘at –risk’ infant. Examples
include:
Infants with intrauterine growth restriction
Infants of diabetic mothers
Preterm infants
Infants who have suffered fetal distress in labour (infants with perinatal asphyxia)
Infants who are ‘large for dates’ - possibility of undiagnosed maternal gestational
diabetes

5
In these groups, a blood glucose <2.6 mmol/L is generally accepted to indicate
hypoglycemia.
Signs of hypoglycemia in the newborn are vague and include apathy/ floppiness,
apnoea, excessive jitteriness. These non specific signs can also be due to sepsis.
Hypothermia
:
This can be defined as a rectal temperature <36°C.
It is most commonly seen in:
Growth restricted babies
Preterm small infants
As part of the clinical features in the sick infants
The septic infant may also present with hypothermia rather than pyrexia
Hypothermia can cause significant morbidity:
Infants are lethargic and feed poorly
More seriously, hypothermia is associated with hypoglycemia, metabolic acidosis and
respiratory distress
Perinatal asphyxia
Neonatal asphyxia is defined as failure of the infant to cry or breath well after delivery.
Perinatal asphyxia occurs when a lack of oxygen and acidosis cause organ impairment.
Deprivation of the oxygen to the brain can occur in two ways:
hypoxaemia – a reduction in the amount of oxygen in the blood.
Ischaemia – a reduction in the amount of blood perfusing the brain.
The majority of cases occur in the intrapartum period.
Features include
:
Fetal distress
Birth depression (low Apgar score require ressuscetation
Metabolic acidosis on cord blood or early neonatal sample
Seizures (the hallmark of this condition)
Renal impairment (blood in the urine and a low urine output)
Alteration of central nervous system state – the baby is not normally conscious between
seizures, but is irritable or lethargic with abnormal primitive reflex
