1
Forth stage
Medicine
Lec-7
د.فاخر
1/1/6102
Male hypogonadism
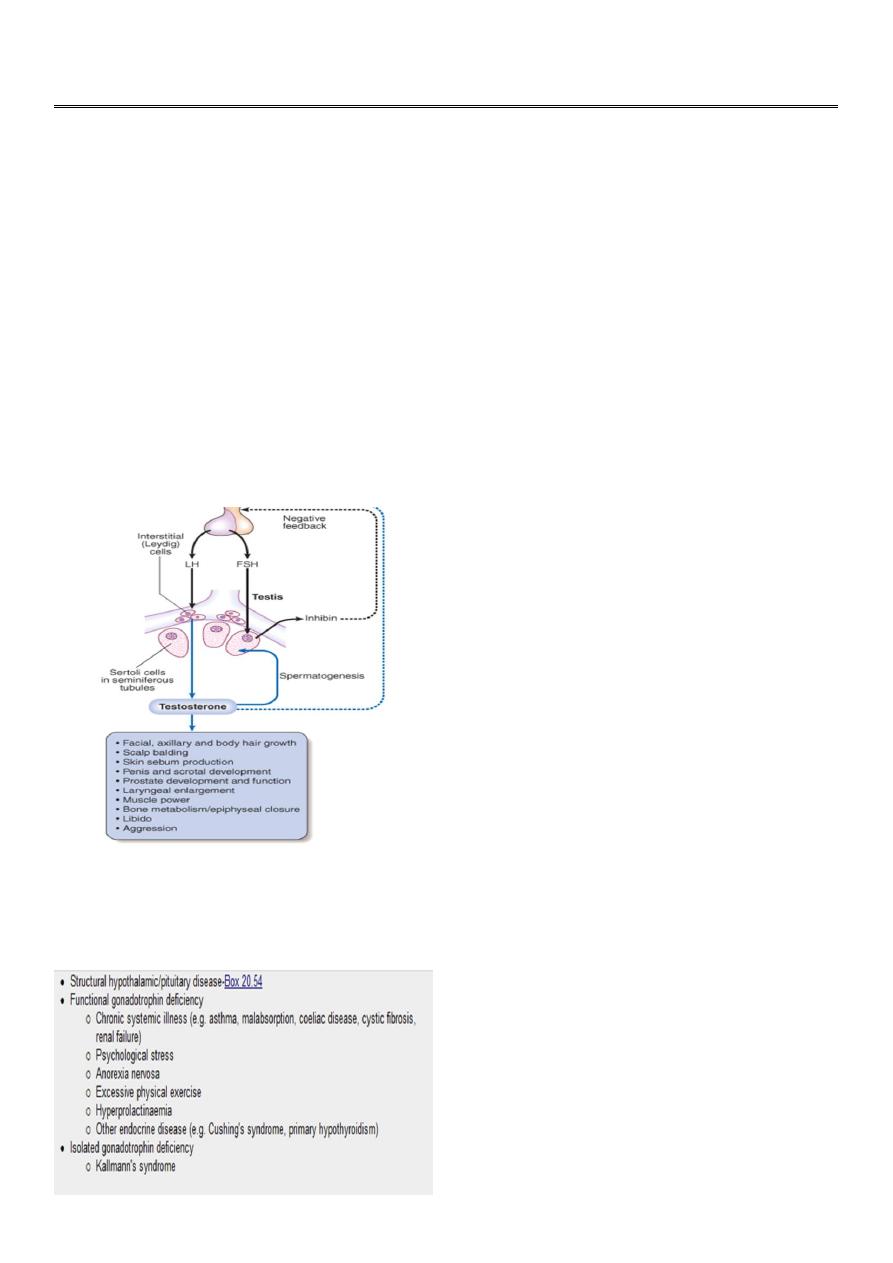
In the male, the testis subserves two principal functions: synthesis of testosterone by the
interstitial Leydig cells under the control of luteinising hormone (LH), and spermatogenesis
by Sertoli cells under the control of follicle-stimulating hormone (FSH) (but also requiring
adequate testosterone)..
Definition
A decrease in either of the two major functions of the testes:
sperm production
testosterone production
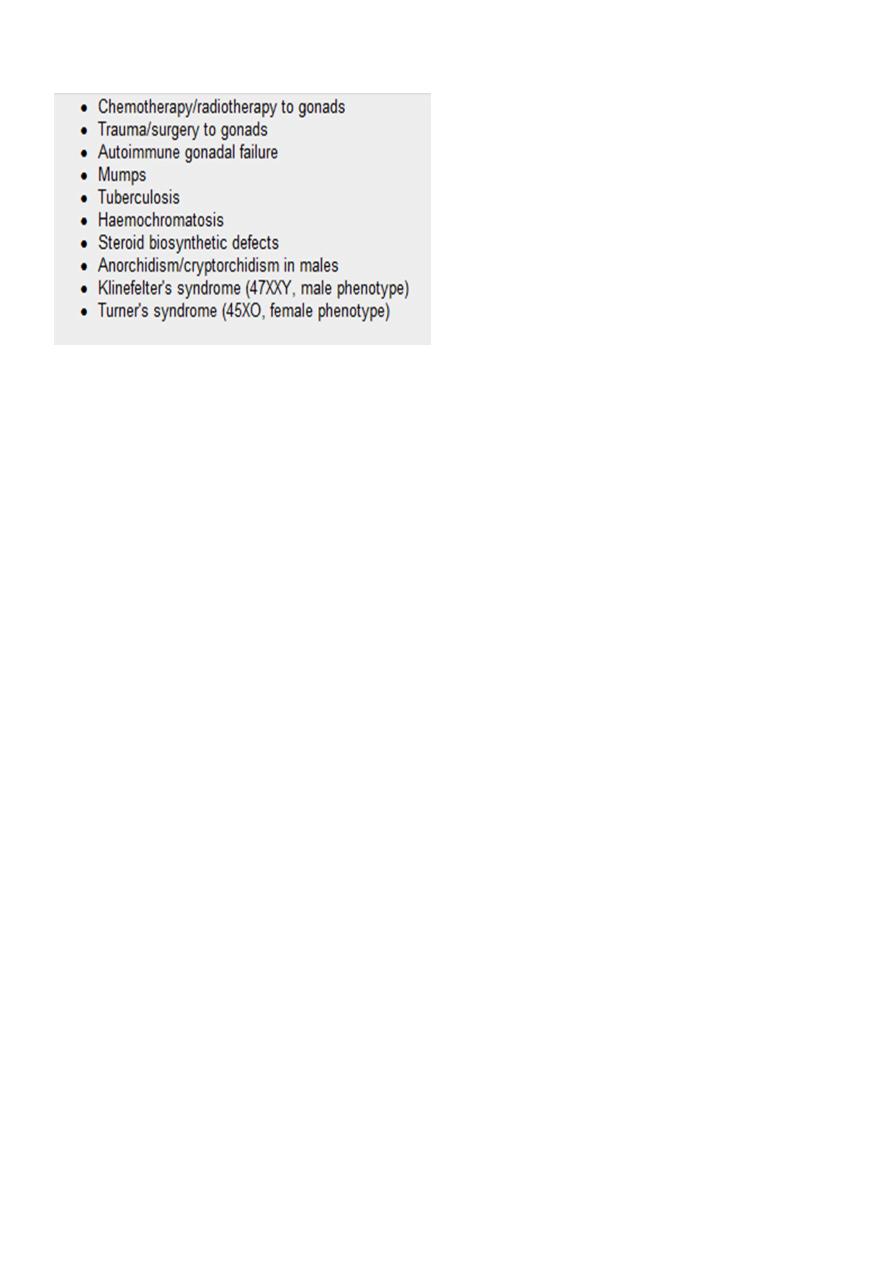
CAUSES OF DELAYED PUBERTY AND HYPOGONADISM
Hypogonadotrophic hypogonadism
2
Hypergonadotrophic hypogonadism
Negative feedback suppression of LH is mediated principally by testosterone, while secretion
of another hormone by the testis, inhibin, suppresses FSH
The axis can be assessed easily by a random blood sample for testosterone, LH and FSH.
Testosterone is largely bound in plasma to sex hormone-binding globulin,. Testicular function
can also be tested by semen analysis.
The clinical features
The clinical features of both hypo- and hypergonadotrophic hypogonadism include loss of
libido, lethargy with muscle weakness, and decreased frequency of shaving. Patients may
also present with gynaecomastia, infertility, delayed puberty and/or anaemia of chronic
disease.
Male hypogonadism is confirmed by demonstrating a low serum testosterone level. The
distinction between hypo- and hypergonadotrophic hypogonadism is by measurement of
random LH and FSH. Patients with hypogonadotrophic hypogonadism should be investigated
as described for pituitary disease on
Patients with hypergonadotrophic hypogonadism should have the testes examined for
cryptorchidism or atrophy and a karyotype performed (to identify Klinefelter's syndrome
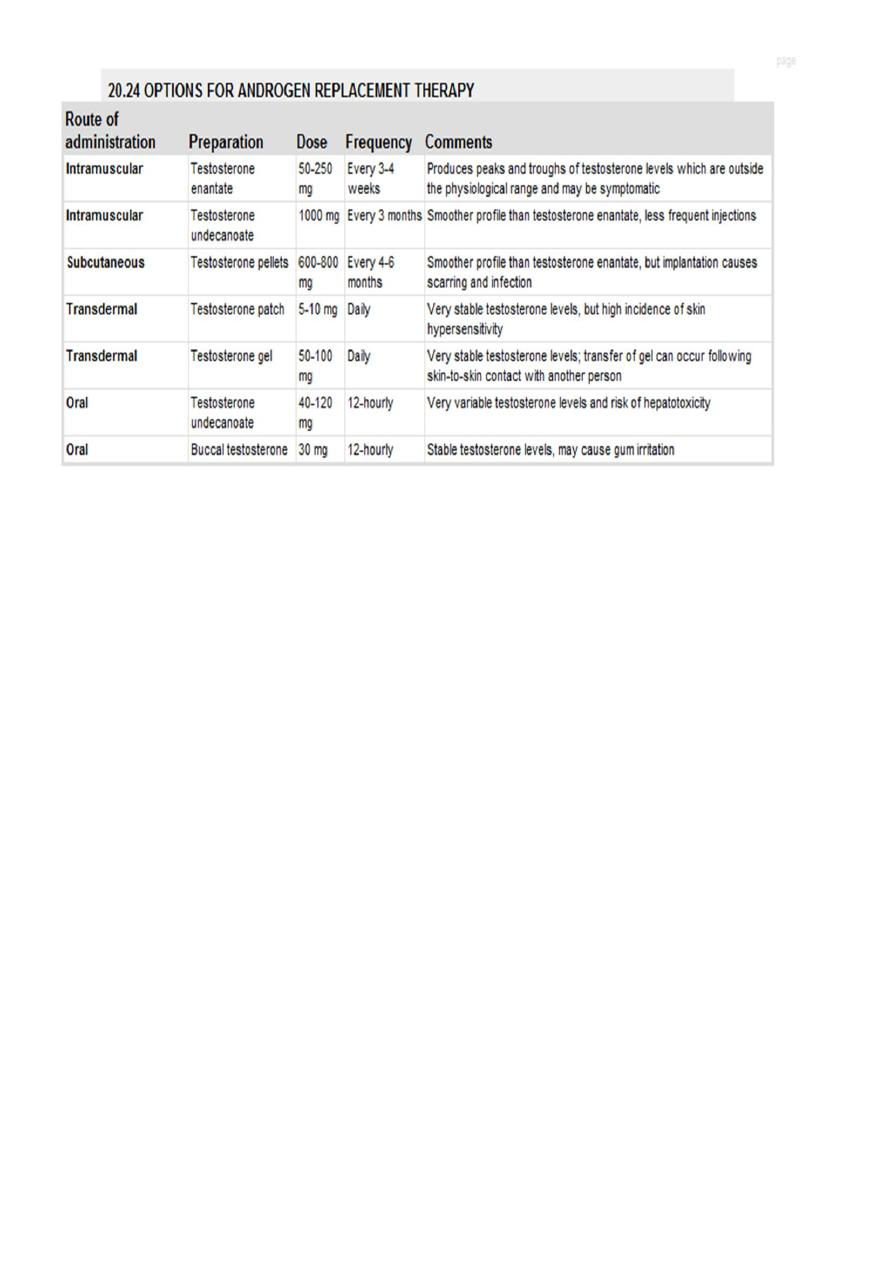
Management Testosterone replacement is indicated in hypogonadal men to prevent
osteoporosis, and restore muscle power and libido.. First-pass hepatic metabolism of
testosterone is highly efficient so bioavailability of ingested preparations is poor. Doses of
systemic testosterone can be titrated against symptoms
3
Testosterone replacement inhibits spermatogenesis. Men with hypogonadotrophic
hypogonadism who wish fertility are usually given injections of hCG several times a week
(recombinant FSH may also be required in men with hypogonadism of pre-pubertal origin).
The duration of gonadotrophin therapy depends on the duration and cause of
hypogonadism.
If there is a hypothalamic cause, then pulsatile GnRH therapy is an alternative. Extraction of
sperm from the epididymis, in vitro fertilisation and intracytoplasmic sperm injection (ICSI)
are being used increasingly to try to achieve fertility in men with primary testicular disease.
GYNAECOMASTIA
Gynaecomastia is the presence of glandular breast tissue in males. Normal breast
development in women is oestrogen-dependent, while androgens oppose this effect.
Gynaecomastia results from an imbalance between androgen and oestrogen activity, which
may reflect androgen deficiency or oestrogen excess
Idiopathic
Physiological
Drug-induced
Cimetidine
Digoxin
Anti-androgens, e.g. cyproterone acetate, spironolactone
Some exogenous anabolic steroids, e.g. diethylstilbestrol

4
Investigations If a clinical distinction between gynaecomastia and adipose tissue cannot be
made, then ultrasonography or mammography is required. A random blood sample should
be taken for testosterone, LH, FSH, oestradiol, prolactin and hCG. Elevated oestrogen
concentrations are found in testicular tumor
Management
An adolescent with gynaecomastia who is progressing normally through puberty may be
reassured that the gynaecomastia will usually resolve once development is complete. If
puberty does not proceed in a harmonious manner, then there may be an underlying
abnormality that requires investigation
Androgen replacement will usually improve gynaecomastia in hypogonadal males and any
other identifiable underlying cause should be addressed if possible.
