1
4th stage
Medicine
Lec-4
Dr.Abdullah
19/4/2016
LIVER FUNCTION AND INVESTIGATION OF HEPATOBILIARY DISEASE
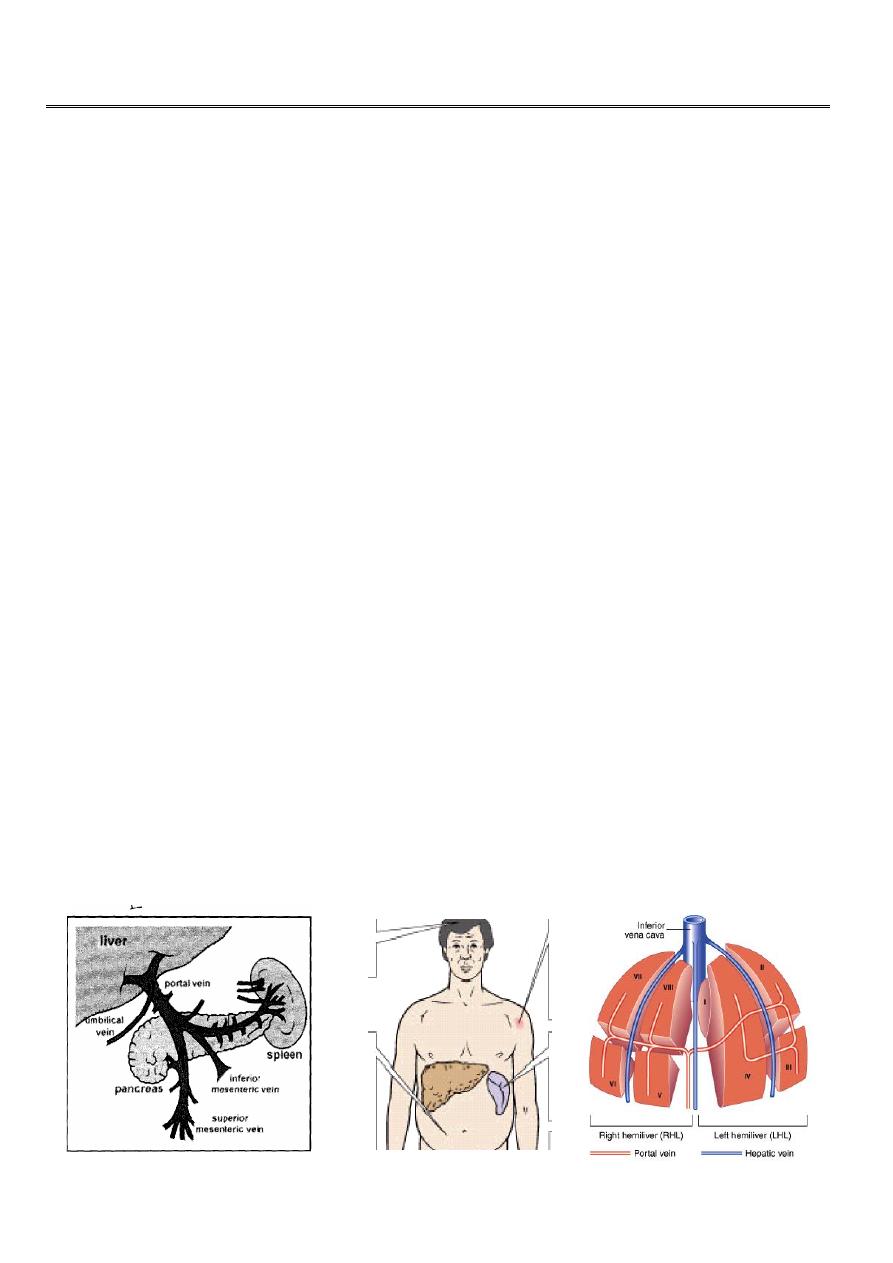
The liver is the largest organ in the body and weighing in average 1.2 – 1.5 Kg in adult. It has
dual and rich blood supply from 1. Hepatic arteries which are branches of celiac plexus and
supply oxygenated blood to the liver. 2. Blood from viscera and spleen through portal vein.
Anatomy
1. Basic anatomy:
The liver has traditionally divided into: A relatively large right lobe and smaller left lobe by
different ligaments and fissures (falciform ligament, fissure of the ligamentum teres and
fissure of the ligamentum venosum). Most of the liver is under lower rubs at right side of
the chest with liver span of about 12 cm in the adult. When the liver is enlarged
(hepatomegaly) the right lobe will be palpable at right hypochondrial region. Some time the
liver is just palpable normally in small children and in conditions that push the liver
downward as in advanced emphysema. The healthy liver is dark red and firm in consistency.
2. Functional or surgical anatomy:
This is the most important way of liver division, in which the liver is divided into right and
left hemilivers depending on the hepatic blood supply. The R and L hemilivers are further
divided into a total of 8 segments in accordance with subdivisions of the hepatic and portal
veins. Each segment is made up of multiple lobules.
The lobules consist of: a. central vein b. radiating sinusoids which are separated from each
other by single liver cell plate. c. peripheral portal tracts.
2
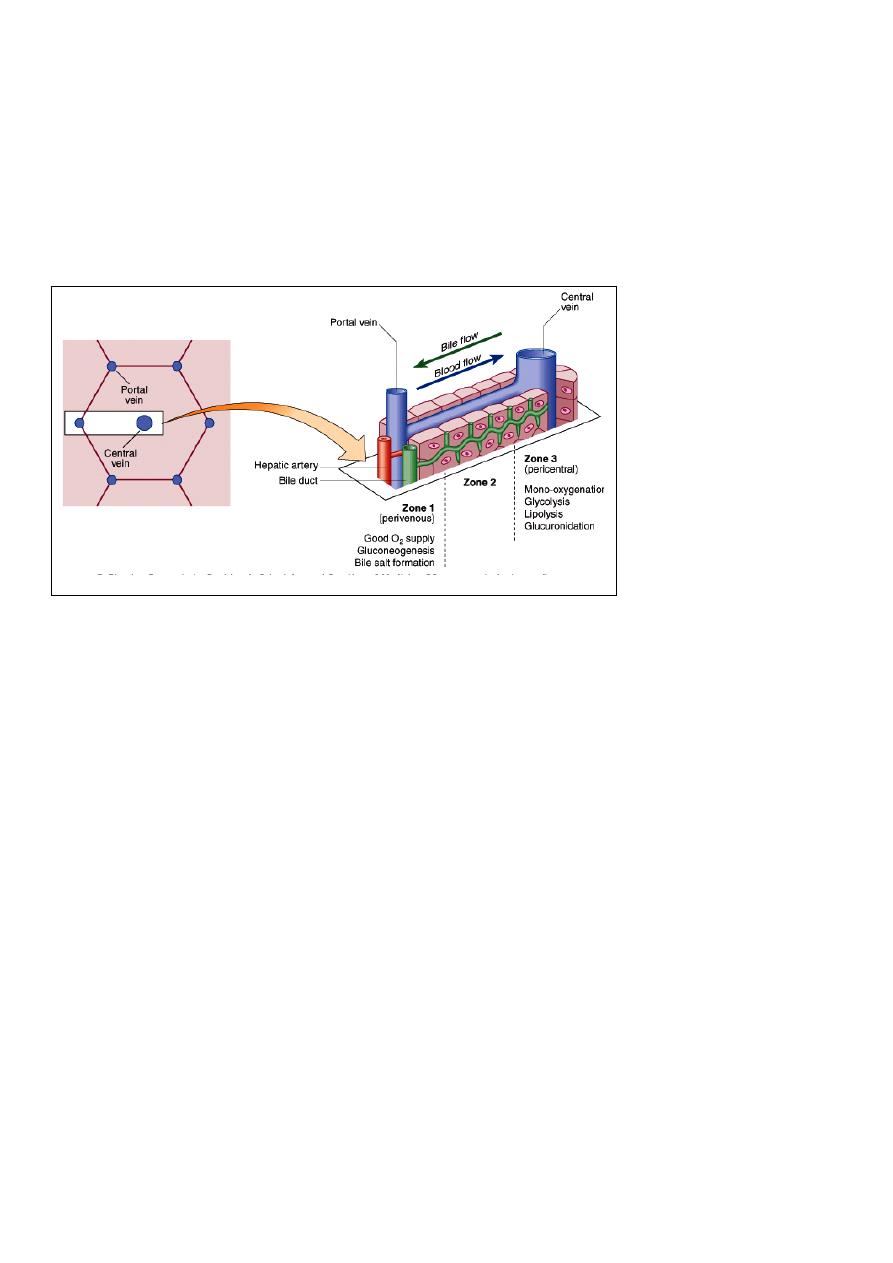
The functional unit of the liver is the hepatic acinus which is anatomically almost the
reverse of the hepatic lobule. The blood flow from peripheral (terminal branches of portal
vein and hepatic artery in the portal tract) through sinusoid toward central vein.
There are 3 zones of hepatocytes according to their location from terminal portal tract of
the acinus: a. zone 1 near the terminal branches of portal vein and hepatic artery. This
zone is rich in oxygen. b. zone 2 (middle zone) c. zone 3: near the central veins (branches of
hepatic veins), least oxygenated.
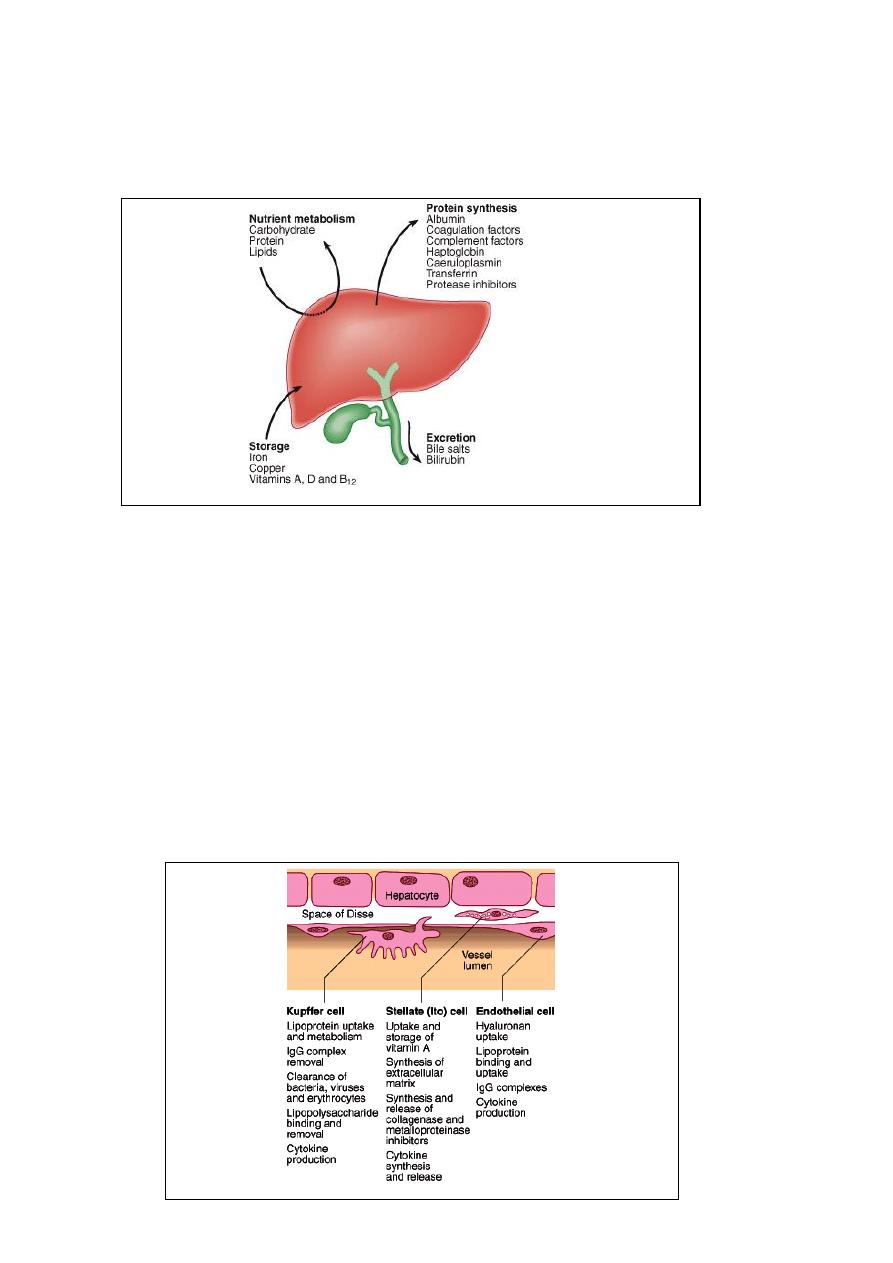
Summary of the main functions of the liver:
Carbohydrate metabolism:
1. Storage of absorbed glucose in the form of glycogen.
2. Release of glucose during fasting
3. Gluconeogenesis: glucose formation from amino acids.
4. Lactate formation
Protein metabolism:
1. Serum protein synthesis (albumin and globulin).
2. Synthesis of endogenous and liver proteins.
3. Gluconeogenesis.
4. Urea synthesis
Urea and endogenous protein synthesis are suppressed during fasting.
Formation of coagulation factors:
Especially F II, VII, IX and X
Vitamines metabolism:
3
1. Some vitamins are stored in liver in large amount and for long time, so deficiency
of such vitamins occurs after years e. g. vit. B12, A and D.
2. Some vits. Are stored in small amounts and disappeared rapidly if dietry intake is
insufficient like folic acid and vit K.
3. Metabolism of some vitamins like vit D and tryptophan to more active form.
Storage of minerals:
Like iron in form of ferritin and haemocidern and also storage of copper and this is used
some time for diagnosis of some diseases like Wilson disease by measuring the quantity of
copper in biopsy speciment.
Metabolism of drugs, alcohol and different toxins in diet.
Metabolism and synthesis of bile salt and bilirubin.
Immunological function:
Approximately 15% of liver cells are Kupffer cells (modified monocytes), with phagocytic
activities.

4
INVESTIGATIONS OF HEPATIC AND BILIARY DISEASES
TESTS TO DETECT HEPATIC ABNORMALITIES
Liver function tests
A. Liver enzymes:
Transaminase enzymes: Normal (average for each less than 20 U / L )
The two most important enzymes are: a. Alanine aminotransferase (ALT) also called SGPT
and b. (AST) also called SGOT, they are present in cytoplasm of hepatocytes. ALT activity
occurs mainly in liver, but AST activity occurs in other tissues like heart and muscles. They
are increased (released into circulation) mainly in diseases that cause liver cell damage e. g.
viral hepatitis and drug induced hepatic damage.
Alkaline phosphatase: Normal range (30 – 85 U /L).
These are groups of enzymes that hydrolysis phosphate esters at alkaline PH. This enzyme is
widely distributed in the body in particular in liver, GIT, bone and placenta. The enzyme
concentrated in membranes associated with absorptive or secretary function such as in
sinusoidal and biliary canaliculi membrane. This enzyme increased mainly in obstructive
jaundice.
Gamma-glutamyl transferase (GGT)
It is microsomal enzyme that occurs in many cells and tissues of the body. Isolated increase
of this enzyme occurs in microsomal enzyme induced drugs like alcohol and alcoholic liver
disease, also in barbiturate, carbamazepine, INH and Rifampicin ingestion.
Large increase in aminotransferase activities with small increase in alkaline phosphatase
activities is in favour of hepatocellular damage, while the reverse indicates biliary
obstruction. Unfortunately these tests are not sufficient to separate between the two
groups of diseases, so further investigations are needed.
B. S. Bilirubine (see below).
C. Hyponatremia: Multi-causes. Indicate severe liver diseases.
D. Serum urea: normal range (3.3 – 7.3 mmol/L).
Usually low, as its synthesis is decreased in both acute and chronic liver diseases.
(Urea increase to some degree if upper GIT bleeding from varices or DU, known
consequences of chronic liver diseases and hepatorenal syndrome have occurred).

5
Haematological finding:
NC/NC anaemia as a result of acute upper GIT bleeding.
MC/HC anaemia (iron deficiency) as a result of chronic blood loss from
e. g. in DU.
Increase in size of RBCs (Macrocytosis): in alcoholic liver diseases.
Erythrocytosis: Rarely occur in hepatocellular carcinoma (ectopic
erythropoietin excretion)
Leucopenia, thrombocytopenia and anaemia in portal hypertension with
hypersplenism.
Leucocytosis with neutrophilia in cholangitis, cholecystitis, hepatic abscess, Weil’s
disease .
Lymphocytosis: in viral hepatitis.
Atypical lymphocytosis: in infectious mono nucleolosis.
Thrombocytosis: in acute upper GIT bleeding and rarely hepatocellular carcinoma.
TEST TO DETERMINE THE SEVERITY OF LIVER DISEASE
These include:
S. bilirubin (total 5 – 17 mmol/L).
Increase in the level of bilirubin more than 50 mmol/L cause clinical jaundice. The severity
of jaundice in hepatocellur type is related to the severity of the disease. Prolonged
obstructive jaundice causes vitamin K deficiency.
S. Albumin: The liver produces 8 – 14 gm of albumin daily. The albumin decrease in
severe and chronic liver diseases. Changes in globuline level occurs in different liver
diseases especially autoimmune diseases.
Prothrombin time (PT): Most factors are synthesized in the liver and require vit K for
activation of factors II, VII, IX and X. Severe liver disease and obstructive jaundice
(vit. K deficiency) lead to prolonged prothrombin time. PT depends on factors I, II, V,
VII and X. Half-life of vit K is short (5 – 72 hours) so changes of prothrombin time
occur quickly and can be corrected by giving 10mg of vitamin K iv.
Hypercoagulation state can occur due to different diseases and lead to obstruction of
hepatic vessels and Budd Chiari syndrome.
Severe hyponatraemia: S. Na < (less than) 120mmol/l.
S. Creatinine: > 1.5 mg/dl in the absence of other causes of reneal impairment may
indicate hepato-renal syndrome.

6
SPECIFIC TESTS
Serology for viral hepatitis
Hepatitis B: HB sAg, HB e Ag, Hepatitis viral DNA (PCR), Anti - Hepatitis B core (Anti-HBc IgM
and IgG), Anti – Hepatitis B surface (Anti-HBs).
Hepatitis C: Anti-hepatitis C, PCR
Hepatitis D: Anti- Hepatitis D (IgM and IgG)
Hepatitis E: Anti - Hepatitis E
In autoimmune chronic active hepatitis:
S. immunoglobulins, Anti-smooth
muscle antibodies (ASA), liver, kidney, microsomal antibodies (LKM), Anti-nuclear
antibodies (ANA) are present. In primary liver cirrhosis: Anti-mitochondrial antibody (AMA)
is useful in diagnosis.
Liver Biopsy
This is helpful in diagnosis of different types of chronic hepatitis and cirrhosis. It is also
important to know the severity of liver disease and some time to know the specific cause of
liver disease as in Wilson disease by measuring the quantity of cupper in biopsy material.
The procedure done percutanously by using Trucut needle or Mngihinni needle but
measurement of platelet count and prothrombin time is very important before procedure,
also co-operation of the patient is necessary. Another methods of taking liver biopsies are
through transjugular route or laparoscopy.
INVESTIGATIONS OF THE COMPLICATIONS OF LIVER DISEASES
1. Portal hypertension: by using US, OGD, CT scan, wedged hepatic venous pressure and
venography of hepatic veins.
2. Ascites:
A. US of abdomen then:
B. fluid aspiration for biochemical, bacteriological
and cytological examination.
C. percutanous needle biopsy if the ascetic fluid is
Exudate (usually the ascetic fluid is transudate in
chronic liver disease).
D. Laparoscopy.

7
3. Renal failure:
A. General urine examination.
B. US of kidney
C. Renal biopsy
D. S. Urea and Creatinine
E. Central venous pressure recording
4. Hepatocellur carcinoma:
A. alpha fetoprotein
B. US liver
C. CT abdomen
D. Laparoscopy
E. Hepatic angiogram
5. Hepatic encephalopathy:
A. tests for precipitating
B. Psychometric tests
C. EEG (Electroencephalography)
D. sensory evoked potentials
IMAGING TECHNIQUES
1. US abdomen and liver
2. CT scan
3. Cholangiography through:
A. PTC (percutanous transhepatic cholangipography
B. Through
ERCP
(Endoscopic
retrograde
cholangio-
pancreatography).
C. MRI (ERCP)
4. Hepatic arteriography
5. Endoscopic ultrasonography.
6. Isotope imaging study of liver
7. Plain X-ray
