
1
Forth stage
Medicine
Lec-3
د.ضياء الليلة
1/1/2014
Acute pancreatitis
Definition:
An acute inflammatory process of the pancreas with variable involvement of regional
tissues and remote organ systems.
Pathogenesis:
Premature activation of zymogen granules, releasing proteases which digest the pancreas
and surrounding tissue.
The severity of pancreatitis depend on the balance between activity of released proteolytic
enzymes and antiproteolytic factors.
Causes:
Common (90%)
1.Gallstones
2.Alcohol
3.Idiopathic
4.Post-ERCP
Rare:
1.Drugs: thiazide, azathioprine, sodium valproate
2.Metabolic: hypercalcemia,hypertriglyceridemia - Infection: mumps
3.Congenital: pancreas divisum
4.Hereditary
5.Trauma
Clinical approach:
Aims:
1.To establish the diagnosis.
patients according to severity and treat accordingly.
2.To assess and
.To identify and treat complications.
3
4.To prevent recurrences.
Diagnosis:
Two of three of the followings:
.Characteristic clinical features
1
2.Elevated pancreatic enzymes
3.Imaging evidence of pancreatic swelling

2
Clinical features:
Symptoms:
Pain: Almost all patients with acute pancreatitis have acute upper abdominal pain at the
onset . The pain is steady and may be in the mid-epigastrium, right upper quadrant, diffuse,
or, infrequently, confined to the left side. One characteristic of the pain that is present in
about one-half of patients, is band-like radiation to the back.
The abdominal pain is typically accompanied by nausea and vomiting, which may persist
for many hours.
Restlessness, agitation, and relief on bending forward are other notable symptoms.
Patients with fulminant attacks may present in shock or coma.
Signs:
Marked epigastric tenderness
-
Guarding and rebound tenderness are absent in the early stages (because the
inflammation is retroperitoneal).
Diminished or absent bowel sounds (localized paralytic ileus)
Grey-Turner's sign (ecchymotic discoloration in the flank
)
or Cullen's sign (ecchymotic discoloration in the periumbilical region) occurs in 1 percent
of cases but is not diagnostic
.
These signs reflect intraabdominal hemorrhage and are associated with a poor prognosis.
-
Jaundice due to obstruction of the common bile duct or edema of the head of the
pancreas.
Pancreatic enzymes
Serum amylase
—
Serum amylase is the most frequently ordered test to diagnose
acute pancreatitis. It rises within 6 to 12 hours of onset, and is cleared fairly rapidly
from the blood (half-life approximately 10 hours). In uncomplicated attacks, serum
amylase is usually elevated for three to five days.
Amylase must be measured early (within 24-48 hrs)
It is usually more than three times the upper limit of normal. However, the serum
amylase may be normal or minimally elevated
It is nonspecific finding.
Question
What are the causes of high serum amylase?
Serum lipase:
-
The sensitivity of serum lipase for the diagnosis of acute pancreatitis ranges from 85 to 100
percent.
Lipase measurement is more specific than serum amylase.
lipase measurements have been difficult to perform.

3
Imaging studies:
1.Abdo.USG:
Values:
To exclude biliary pancreatitis (may show gallstones, biliary obstruction).
-
-Diagnosis:
not sensitive,a diffusely enlarged
hypoechoic pancreas is the
classic
ultrasonographic image of acute pancreatitis.
Complications: pseudocyst
-
2.CT:
Early:
To rule out other causes of acute abdomen
Late (3-8 days):
To define the viability of the pancreas (to detect pancreatic necrosis which manifest as
decreased enhancement after iv contrast).
3.Abdominal plain film
To exclude other causes of abdominal pain such as obstruction and bowel perforation.
The radiographic findings in acute pancreatitis range from unremarkable in mild disease to
localized ileus of a segment of small intestine ("sentinel loop).
4.Chest Films:
Approximately one-third of patients with acute pancreatitis have abnormalities visible on
the chest radiograph such as elevation of a hemidiaphragm, pleural effusions, basal
atelectasis, pulmonary infiltrates, or acute respiratory distress syndrome.
Left-sided or bilateral pleural effusions suggest increased risk of complications.
Assessment of severity
1
.Mild: with minimal organ dysfunction and uneventful recovery.
Most attacks of AP are mild with recovery occurring within five to seven days.
Death is unusual (less than 3 percent)
2. Severe (necrotising pancreatitis): 15 to 25 percent
It is associated with a high rate of complications (local and systemic) and mortality
(approximately 17 percent)
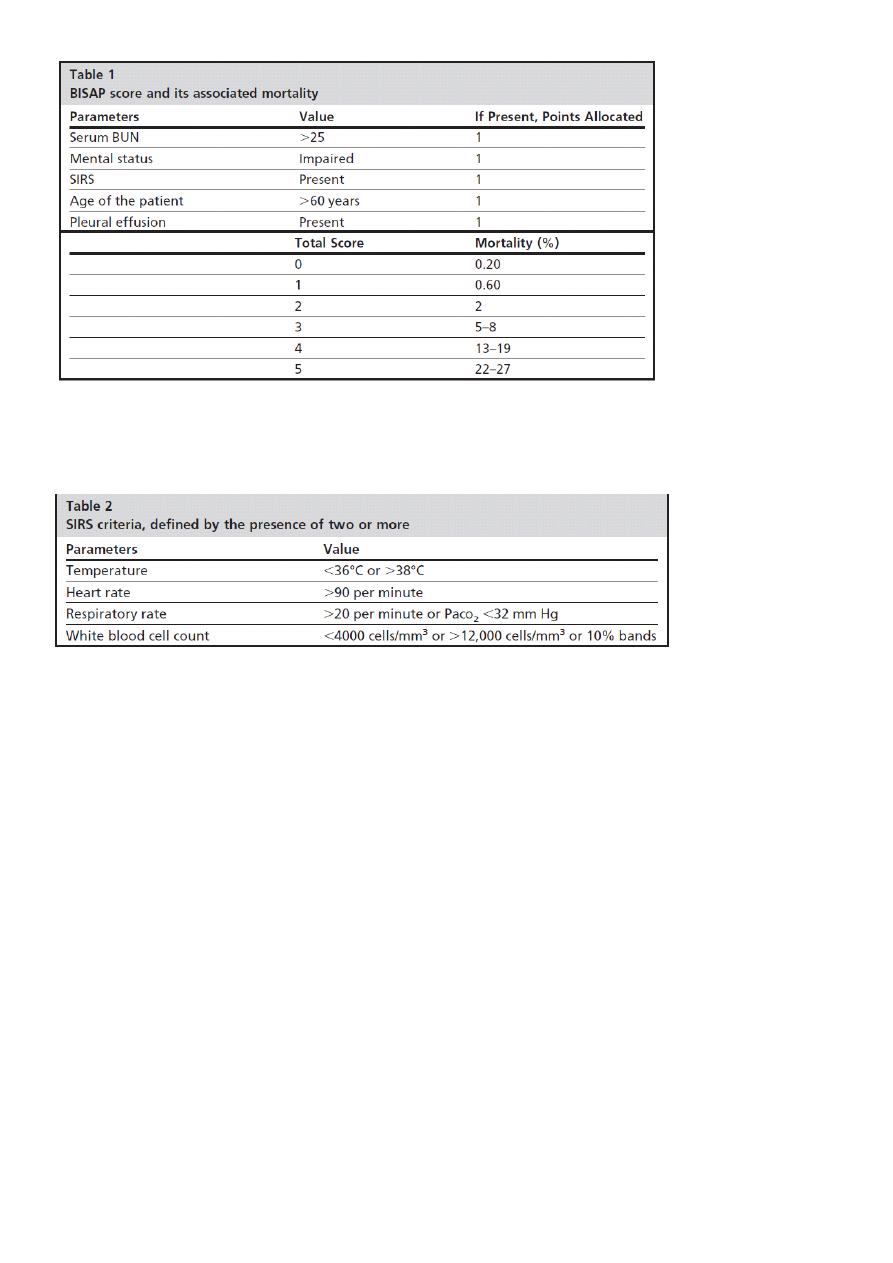
Bedside Index of Severity in Acute Pancreatitis(BISAP score)
Patients are assigned 1 point for each of the following during the first 24 hours:
4
Question
What are SIRS criteria?
DD:
-
Acute MI
-
Acute cholecystitis
-
Perforated DU
Treatment
1.Early treatment according whether the disease is mild or severe
2.Detection and treatment of complications.
gallstones
-
3.Treating the underlying cause – specifically
Initial management
1.Analgesia
2.Correction of hypovolemia using aggressive
fluid resuscitation
(
targeting hematocrit
33
%
)
Type of iv fluid:
Use of the more pH-balanced lactated Ringer’s solution led to greater
reduction in SIRS.
compared to the use of normal saline
Vigorous fluid replacement is important because patients with necrotizing pancreatitis
develop vascular leak syndrome.

3
Approximately 250 to 300 cc of intravenous fluids per hour are typically required for 48
hours if the cardiac status permits
Inadequate hydration can lead to hypotension and acute tubular necrosis.
In addition, fluid depletion damages pancreatic microcirculation and results in further
pancreatic necrosis.
Correction of hypoxia
if present, ventilatory
3.support in patients who develop ARDS
4.NG tube: if paralytic ileus is present
5.Entral feeding should be started as soon as tolerated in patients with severe pancreatitis
because they are in severe catabolic state and need nutritional support.
Enteral feeding also decrease endotoxaemia
4.Prophylactic heparin
5.Prophylactic antibiotics
Indications:
`
It is only indicated in patients with infected pancreatic necrosis. Its use to prevent
infection of necrosis is controversial.
6.Cholecystectomy should be performed within 2 weeks following resolution of
pancreatitis in patients with biliary
pancreatitis to prevent
further attacks of
pancreatitis.
7.Urgent endoscopic or surgical necosectomy in patients with necrotising, ,pancreatitis or
pancreatic abcsess to debride all cavities of necrotic material.
8.Pancreatic pseudocysts
are treated by
drainge into the stomach
,
duodenum or
jejunum.
Complications:
A): Local
1.Acute fluid collections: occur early in the course of acute pancreatitis, are located in or
near the pancreas and always lack a wall of granulation of fibrous tissue.
In about half of patients, spontaneous regression occurs.
In the other half, an acute fluid collection develops into a pancreatic abscess or pseudocyst.
2.Pancreatic necrosis: diffuse or focal area(s) of non-viable pancreatic parenchyma
,
3.Acute pseudocyst: collection of pancreatic juice enclosed by a wall of fibrous or
granulation tissue, occurring at least 4 weeks after onset of symptoms, is round or ovoid
and most often sterile; when pus is present, lesion is termed a ‘pancreatic abscess.
’
4)Pancreatic abscess: circumscribed, intra-abdominal collection of pus, often 4 weeks or
more after onset.
B.Systemic complications:
1.Shock : systolic blood pressure<90 mmHg
PaO2 ≤ 60 mmHg
:
2.Pulmonary insufficiency
3.
3.Renal failure: creatinine ≥177 μmol/l
.
4.Gastrointestinal bleeding
.
Disseminated intravascular coagulation
3
.
platelets ≤100,000,fibrinogen<1.0 g/l

6
and fibrin-split products80
≥
μg/l
.
.Severe metabolic disturbances:
6
(.
Calcium ≤1・87 mmol/l ( ≤7・5 mg/dl
Identification
&
treatment of underlying cause
1.History
.
2.Physical examination
3.Blood tests
4.Imaging studies (USG
CT, MRI, MRCP
,Endo.uss)
5.Genetic studies
Prevention of recurrence
Can be achieved only
after establishing the
cause.
.
-
Total abstinence from alcohol is mandatory
.
-
Cholecystectomy: it is imperative in patients with acute biliary pancreatitis
.
Patients with acute biliary pancreatitis
discharged from the
hospital without
cholecystectomy 30to50 percent develop
recurrence of
pancreatitis.
a
,
Role of ERCP:
1.Urgent ERCP—within 24 hours—is indicated
In patients who have severe acute biliary pancreatitis with organ failure or cholangitis or
both.
2.Elective ERCP with sphincterotomy can be considered in patient with
a. Persistent or incipient biliary obstruction
b. Those deemed to be poor candidates for
cholecystectomy.
c Those in whom there is strong
suspicion of bile duct stones.
