
1
Forth stage
Medicine
Lec-9
.د
رامي
1/1/2014
Empyema
This is a collection of pus in the pleural space, which may be as thin as serous fluid or
so thick that it is impossible to aspirate, even through a wide-bore needle.
Microscopically, neutrophil leucocytes are present in large numbers. An empyema
may involve the whole pleural space or only part of it (‘loculated’ or ‘encysted’ empyema)
and is usually unilateral. It is always secondary to infection in a neighbouring structure,
usually the lung, most commonly due to the bacterial pneumonias and tuberculosis. Over
40% of patients with community acquired pneumonia develop an associated pleural
effusion (‘para-pneumonic’ effusion) and about 15% of these become secondarily
infected.
Other causes are infection of a haemothorax following trauma or surgery, oesophageal
rupture, and rupture of a subphrenic abscess through the diaphragm.
The pus in the pleural space is often under considerable pressure, and if the
condition is not adequately treated, pus may rupture into a bronchus, causing a
bronchopleural fistula and pyopneumothorax, or track through the chest wall with the
formation of a subcutaneous abscess or sinus, so-called empyema necessitans.
Clinical assessment:
An empyema should be suspected in patients with pulmonary infection if there is severe
pleuritic chest pain or persisting or recurrent pyrexia, despite appropriate antibiotic
treatment. In other cases, the primary infection may be so mild that it passes
unrecognised and the first definite clinical features are due to the empyema itself. Once an
empyema has developed, systemic features are Prominent.
2
Investigations:
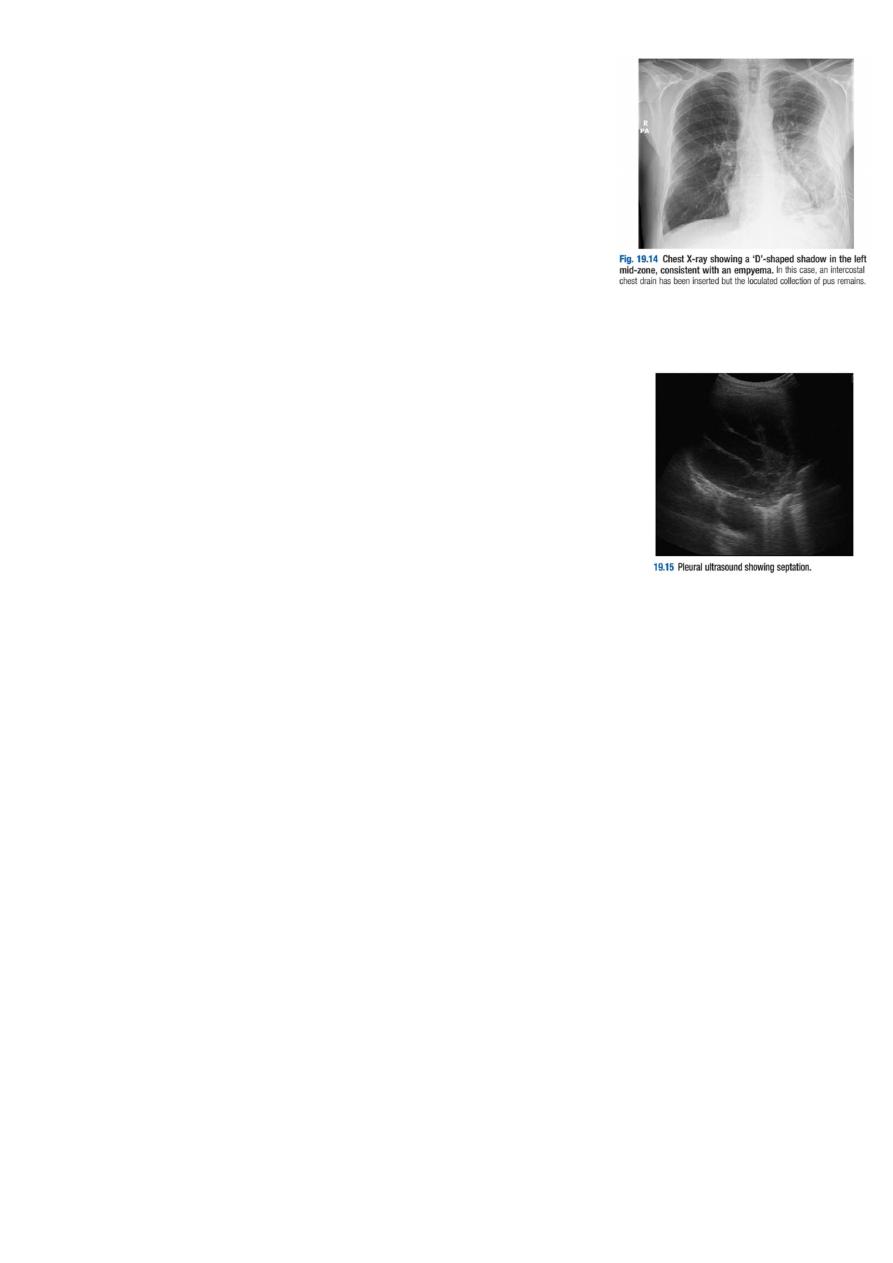
Chest X-ray appearances may be indistinguishable from those
of pleural effusion, although pleural adhesions may confine
the empyema to form a ‘D’-shaped shadow against the inside of
the chest wall .When air is present as well as pus
(pyopneumothorax), a horizontal ‘fluid level’ marks the
air/liquid interface.
Ultrasound shows the position of the fluid, the extent of pleural thickening and
whether fluid is in a single collection or multiloculated, containing
fibrin and debris .
CT provides information on the pleura, underlying lung parenchyma
and patency of the major bronchi.
Ultrasound or CT is used to identify the optimal site for aspiration, which is best
performed using a widebore needle. If the fluid is thick and turbid pus, empyema is
confirmed. Other features suggesting empyema are a fluid glucose of less than 3.3
mmol/L (60 mg/dL), lactate dehydrogenase (LDH) of more than 1000 U/L, or a fluid pH
of less than 7.0 .
However, pH measurement should be avoided if pus is thick, as it damages blood gas
machines. The pus is frequently sterile on culture if antibiotics have already been given.
The distinction between tuberculous and non-tuberculous disease can be difficult and
often requires pleural biopsy, histology and culture.
Management:
An empyema will only heal if infection is eradicated and the empyema space is
obliterated, allowing apposition of the visceral and parietal pleural layers. This can only
occur if re-expansion of the compressed lung is secured at an early stage by removal of
all the pus from the pleural space. When the pus is sufficiently thin, this is most
easily achieved by the insertion of a wide-bore intercostal tube into the most dependent
part of the empyema space. If the initial aspirate reveals fluid or frank pus, or if

3
loculations are seen on ultrasound, the tube should be put on suction (−5 to -10 cm
H2O) and flushed regularly with 20 mL normal . If the organism causing the empyema
can be identified, the appropriate antibiotic should be given 2–4 weeks. Empirical
antibiotic treatment (e.g. intravenous co-amoxiclav or cefuroxime with metronidazole)
should be used if the organism is unknown.
Intrapleural fibrinolytic therapy is of no benefit.
An empyema can often be aborted if these measures are started early, but if the intercostal
tube is not providing adequate drainage – for example, when the pus is thick or
loculated, surgical intervention is required to clear the empyema cavity of pus and break
down any adhesions. Surgical ‘decortication’ of the lung may also be required if gross
thickening of the visceral pleura is preventing re-expansion of the lung. Surgery is also
necessary if a bronchopleural fistula develops.
