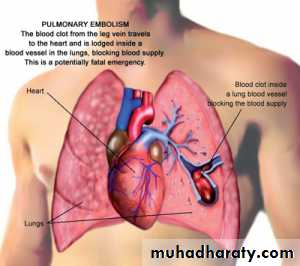
Pulmonary embolism
Dr. Rami M. Adil Al-HayaliAssistant Professor in Medicine
Venous thromboembolism:
pulmonary embolism (PE)deep vein thrombosis (DVT)
1% of all patients admitted to hospital
5% of in-hospital mortality
A common mode of death in patients with cancer, stroke and pregnancy.
Ventilation-perfusion mismatch and ischaemia to the peripheral pulmonary lung tissues.
Acute increase in pulmonary vascular resistance which increase right ventricular load and may reduce cardiac output.Pathophysiology of pulmonary embolism
Risk factors for pulmonary embolism
• Major abdominal and pelvic surgery• Hip and knee surgery
• Postoperative intensive care
• Surgery
• Pregnancy and puerperium
• Obstetric
• COPD
• Congestive heart failure
• Cardiopulmonary
• Fracture
• Stroke
• Spinal cord injury
• Varicose veins
• Lowerlimb problem
• Abdominal and pelvic malignancy
• Advanced/metastatic
• Malignancy
• Increasing age
• Immobility
• previous VTE
• Thrombotic disorders
• Miscellaneous
The clinical presentation varies depending on the number and size of the embolus and on the underlying cardiopulmonary reserve.
It is possible to recognize three major categories of cases:
Acute massive PE
Acute small and medium PE
Chronic thromboembolism
Clinical features
A big thrombus obstructing a major pulmonary artery causing low cardiac output and acute right heart failure.Sudden collapse (fainting), crushing central chest pain and severe dyspnoea.
Examination would reveal tachypnoea, tachycardia, hypotension (or cardiogenic shock), raised JVP and cyanosis.
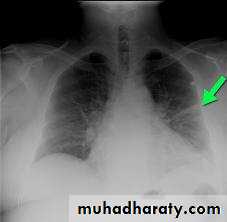
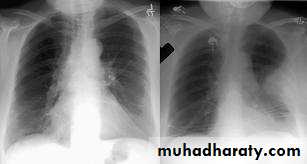
CXR is commonly normal (or show subtle oligaemia).
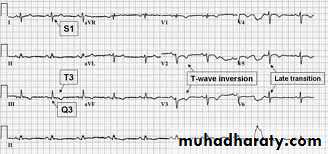
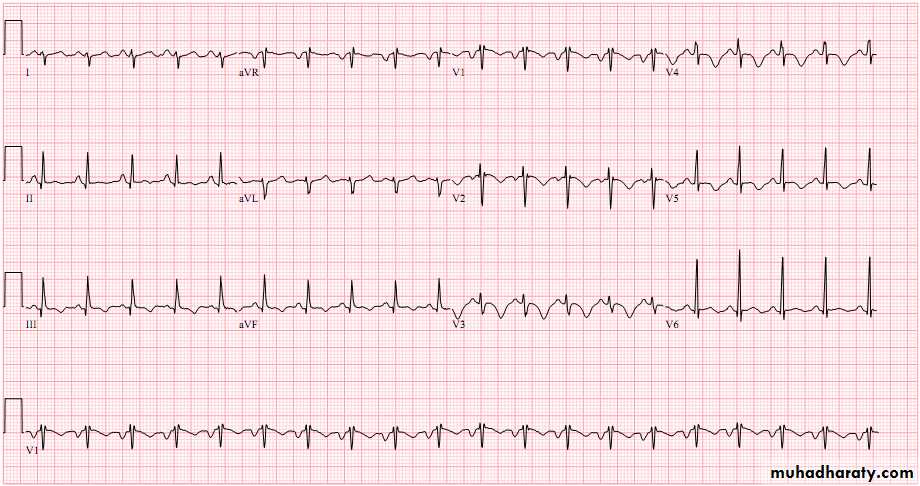
ECG: tachycardia and may show S1Q3T3, anterior T-wave inversion or RBBB
Arterial BGA: hypoxaemia and hypocapnea
Differential diagnosis: acute myocardial infarction (MI), pericardial tamponade and aortic dissection.
Clinical features Acute massive PE
Occlusion of segmental pulmonary artery leading to pulmonary infarction with or without pleural effusion.
Dyspnoea, pleuritic chest pain and haemoptysis.
Tachycardia, low grade fever, but normal BP. Pleural rub or crackles can be heard. Dullness and diminished breathing at the lung base may indicate pleural effusion or elevated dome of the diaphragm.
CXR may show opacities (of any size or shape); more specifically it may show horizontal linear opacities or wedge shaped pleural based opacities. Pleural effusion or raised hemidiaphragm may be noticed.
ECG: sinus tachycardia
Arterial BGA: normal or show mild hypoxaemia and hypocapnea
Differential diagnosis: pneumonia
Clinical features Acute small or medium PE
Chronic occlusion of pulmonary microvasculature caused by multiple small emboli or a sequel to previous organized thrombus, resulting in chronic pulmonary hypertension.
The patient presents with exertional dyspnoea and features of right heart failure.
ECG: right ventricular hypertrophy and strain.
Arterial BGA: exertional hypoxaemia
Clinical features Chronic thromboembolism
Consider the diagnosis of VTE in any patient presenting with:
New or worsening dyspnoeaChest pain
Sustained hypotension
without alternative obvious cause
particularly in patients who have risk factors
Three questions should be in mind on facing a patient with suspected VTE:
Is the clinical presentation consistent with PTE?Does the patient have risk factors?
Any alternative diagnosis that can explain the presentation?
The ECG may show tachycardia only, the CXR is commonly normal. Both investigations are more useful in excluding other diagnosis like MI (ECG), pneumonia and pneumothorax (CXR)
Diagnosis
Well’s clinical probability score for pulmonary embolism
+ 3
Clinical signs of deep vein thrombosis
+ 3
Alternative diagnosis less likely than pulmonary embolism
+ 1.5
Previous pulmonary embolism or deep vein thrombosis
+ 1.5
Heart rate >100 beats per minute
+ 1.5
Recent surgery or immobilization (within the last 30 d)
+ 1
Haemoptysis
+ 1
Cancer (treated within the last 6 mo)
score
Clinical Probability of Pulmonary Embolism
0-1
Low
2-6
Intermediate
≥7
High
D-dimer is a specific degradation product of cross linked fibrin. Apart from PE, it also rises in MI, pneumonia and sepsis.
Low D-dimer has a high negative predicted value and other investigations are unnecessary if the clinical probability is low.
D-dimer is not useful in intermediate and high risk patients because a further investigation is mandatory even if it is normal
D-dimer
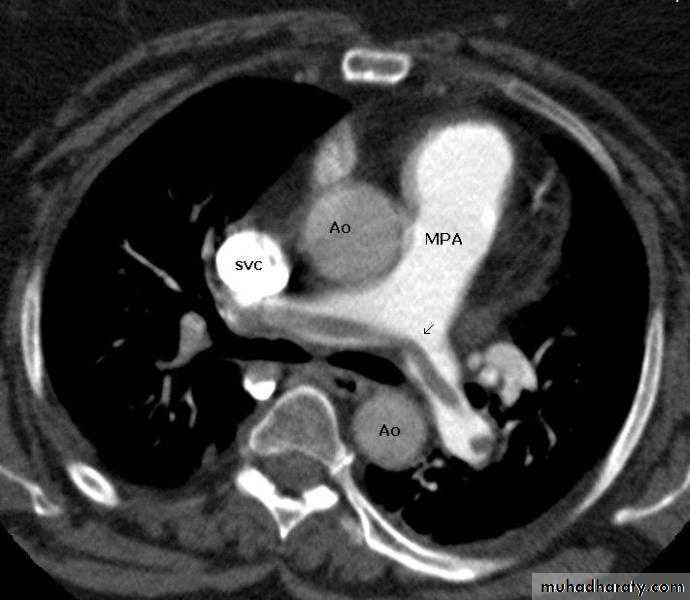
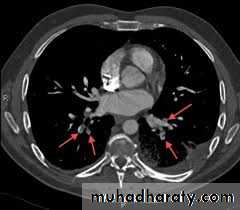
CT pulmonary angiography (CTPA)
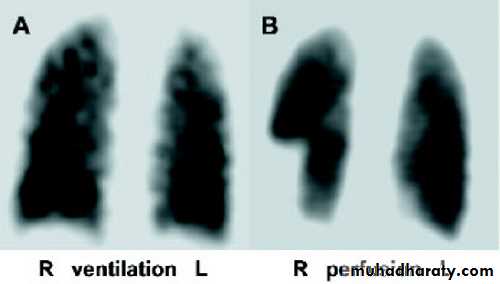
Ventilation-perfusion scan (V/Q scan)Colour Doppler ultrasound of the leg
Imaging
It visualizes the distribution and extent of emboli in positive cases.
It may also prove alternative diagnosisSimultaneous visualization of femoral and popliteal veins for DVT improves sensitivity.
Can be performed safely in pregnant women (with foetal shielding).
CT pulmonary angiography (CTPA)
Less commonly used.
It is more useful in patients without pre-existing cardiopulmonary disease and normal CXR; otherwise the interpretation of the results can be difficult.Ventilation-perfusion scan (V/Q scan)
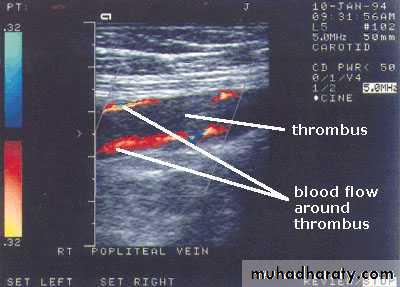
The investigation of choice in the assessment of suspected DVT.It can be performed in patients with suspected pulmonary embolism to prove the presence of thrombus in the leg veins.
Colour Doppler ultrasound of the leg
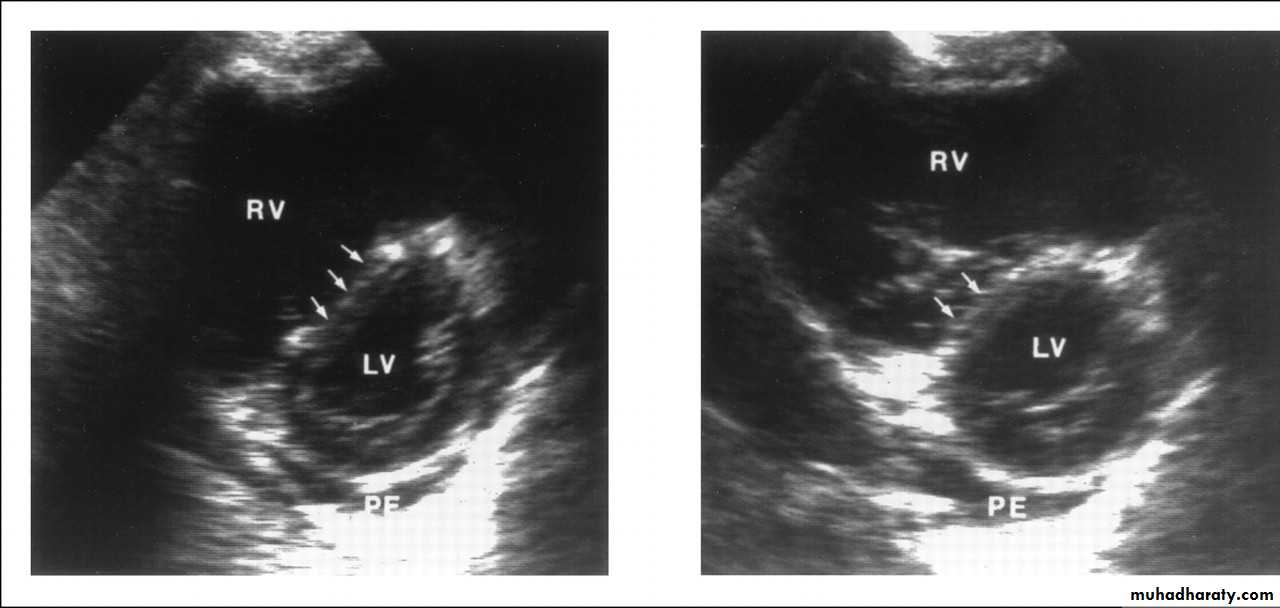
It is helpful in the evaluation of patients with acute circulatory collapse.
Acute right ventricular dilatation is usually present in massive PEA thrombus may be visible.
Alternative diagnosis, like heart failure and pericardial tamponade can be excluded
Echocardiography
Oxygen therapy for hypoxaemic patientsCirculatory shock should be treated with intravenous fluids. Enotropic agents are of limited value
Opiates may be necessary to relieve pain and distress
Resuscitation by external cardiac massage in moribund patient may be successful
Diuretics and vasodilators should be avoided
ManagementGeneral measures
Subcutaneous low molecular weight heparin (LMWH) is preferredFondaparinux is a pentasaccharide that is also approved for treatment of VTE.
Unfractionated heparin can also be used, but it should be administered as continuous intravenous infusion (through infusion pump) and requires adjustment of APTT
The duration of heparin (or fondaparinux) treatment should be at least 5 days, during which oral warfarin is commenced
Anticoagulation
Patients with a persistent risk factor or a history of previous thrombosis should receive warfarin for life.
Those with identifiable and reversible risk factor require 3 months therapy.
If the condition is idiopathic or the risk factor is weak, anticoagulation for 6 months is recommended.
Warfarin is teratogenic, so VTE should be treated with LMWH during pregnancy (giving prophylactic dose after the initial therapeutic dosing).
Anticoagulation
Thrombolysis is indicated in any patient presenting with acute massive PE accompanied by cardiogenic shock.Less certain indications include right ventricular dilatation and hypokinesia on echocardiography , severe hypoxaemia or high troponin level
Patients with haemorrhagic risks should be excluded, as there is a risk of intracranial haemorrhge.
Thrombolytic therapy
Inferior vena caval filter is indicted in the following situations:When anticoagulation is contraindicated
Massive haemorrhage on anticoagulation
Recurrent PE despite anticoagulation
Caval filters
The case mortality rate of acute pulmonary embolism ranges from 1% - 60%
The immediate mortality is greatest in those with cardiogenic shock or right ventricular dysfunction.Recurrence is possible especially in the first 6-12 months after the initial event.
The majority regain normal right ventricular function within 3 weeks, however by 2 years, 4% of patients have persistent pulmonary hypertension