1
Forth stage
Medicine
Lec-2
.د
رامي
1/1/2014
Chronic Obstructive Pulmonary Disease (COPD)
Definition
COPD is defined as a disease state characterized by airway limitation "obstruction" that is
not fully reversible.
COPD includes:
•
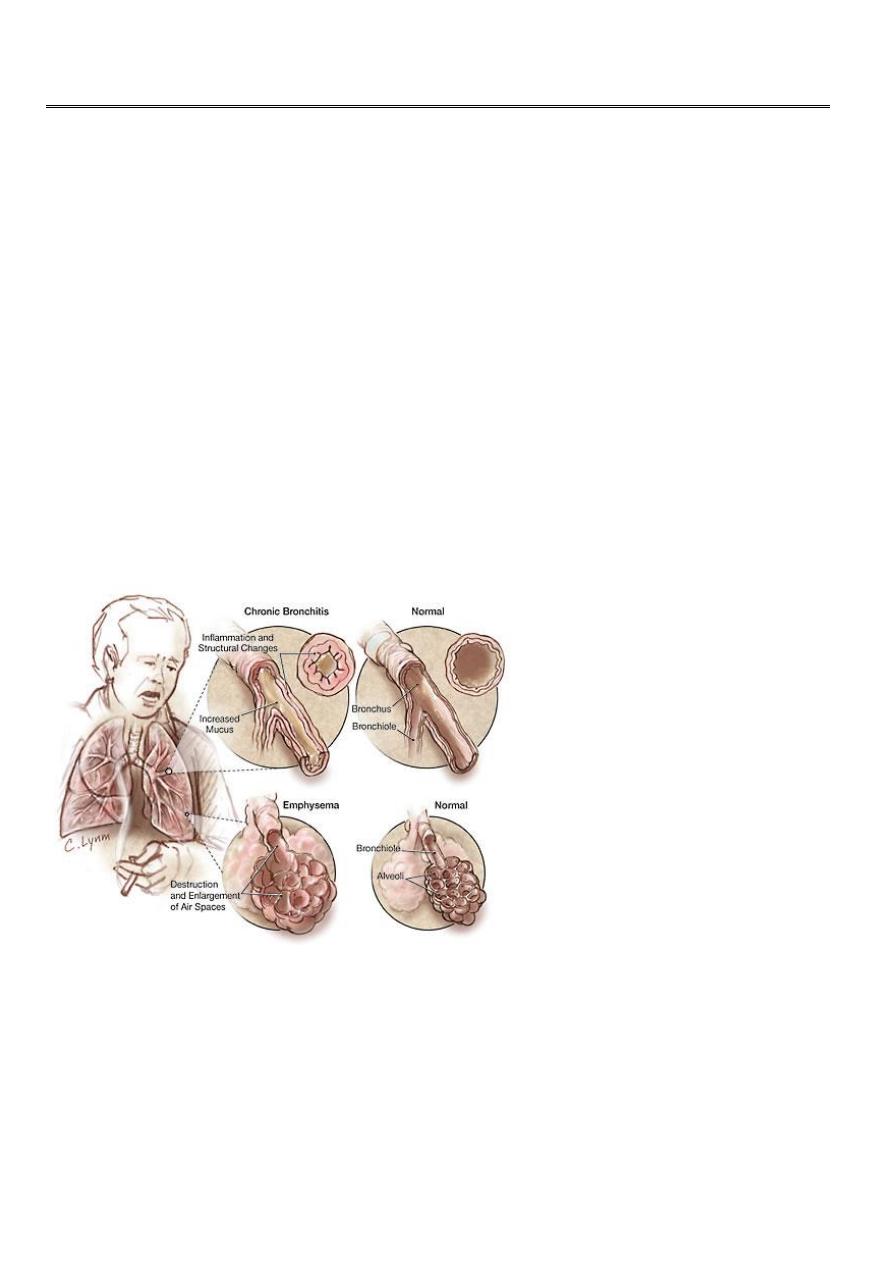
Emphysema, anatomically defined condition characterized by abnormal permanent
enlargement of the airspaces distal to the terminal bronchioles accompanied by
destruction of their walls.
•
Chronic bronchitis, a clinically defined condition as cough and sputum on most days
for at least 3 consecutive months for at least 2 successive years.
Epidemiology
• Around 80 million people worldwide suffer moderate to severe disease.
• Anticipated that it would be the 4th leading cause of death in 2020.
• More common in men

2
Aetiology
• Cigarette smoking (the major risk factor for COPD )
• Other exposures:
Biomass solid fuel fires
Occupational
Passive smoking
• Airway hyperreactivity
• Genetic factors:
α1 anti-proteinase (α1AP) deficiency
Pathology
Chronic bronchitis
• The bronchial mucosa has enlarged mucus secreting glands with inflammatory cell
infiltration (mainly neutrophils), resulting in increased sputum production.
• Narrowing of small airways (< 2mm) occur by fibrosis, excessive mucus production,
oedema and cellular infiltration.
Emphysema
• Chronic exposure to cigarette smoke cause inflammatory cell recruitment in the
terminal airways.
• These cells release elastolytic proteinases that damage the extracellular matrix of the
lungs, while oxidative stress cause alveolar cell death.
• Progressive destruction of the alveolar cells and matrix leads to progressive
enlargement of the distal airspaces characteristic of emphysema.
• Bullae (large air-filled spaces) form in some patients.
Pathophysiology
• Airway limitation (obstruction) results from both small airway obstruction and
emphysema.

3
• Airway obstruction and the tendency of the airways to collapse during expiration
lead to progressive air trapping and dynamic hyperinflation.
• The hyperinflation causes flattening of the diaphragm, misalignment of the
intercostals muscles, markedly increasing the work of breathing.
• The patient ultimately develops respiratory failure, pulmonary vascular remodeling,
pulmonary hypertension and cor-pulmonle.
Extra-pulmonary features
• impaired nutrition
• weight loss
• muscle wasting
• osteoporosis,
(at least partially caused by increased circulating inflammatory markers)
Clinical features
(History)
• COPD should be suspected in any patient over the age of 40 years "especially
smokers" who present with chronic cough or breathlessness.
• Cough and sputum are usually the first symptoms "commonly referred to as smokers
cough".
• Haemoptysis may occur during exacerbation but should not be attributed to COPD
without thorough investigations to exclude other condition
• The development of exertional dyspnoea is gradual.
• As the disease advances, the patient is breathless on doing simple activities of daily
living and even at rest.
• The disease course is complicated by acute exacerbations that become more
frequent with disease progression.
Physical examination
• In the early stages of the disease, the physical examination may be normal.

4
• Current smokers may have the odour of smoke and nicotine staining of their hands.
• In more severe disease: the patient is breathless, sometimes with pursed lip
breathing, use of accessory muscles of inspiration and intercostal muscle indrawing
during inspiration. The patient may be cyanosed.
• The chest may be hyperinflated "barrel chest", with reduced crico-sternal distance
and inward movement of the lower ribs in inspiration (because of low flat
diaphragm).
• The cardiac apex is commonly impalpable, and the heart sounds may be louder in the
epigastrium (sometimes with epigastric pulsation).
• There is hyper-resonance and loss of cardiac dullness.
• Breath sounds are typically diminished with wheezing. Crackles may accompany
infections, but when persistent should suggest associated bronchiectasis.
• Finger clubbing is not a feature of COPD and should trigger further investigations to
exclude lung cancer, bronchiectasis or fibrosis.
• Oedema usually reflects poor salt and water excretion by the hypoxic kidneys. Less
commonly it reflects right heart failure (complicating cor-pulmonale).
• Advanced disease is associated with significant wasting and is a poor prognostic
feature in COPD.
Pink Puffer Vs Blue Bloater

5
Investigations
Pulmonary function tests
Spirometry:
• The diagnosis requires objective demonstration of airflow obstruction by spirometry.
• This is established when FEV1/FVC ratio <70%.
• Post-bronchodilator FEV1 is used to define disease severity (and the prognosis of the
patient)
mild: >80 of predicted
moderate: 50 % – 80%
severe: 30% - 50%
very severe <30% of predicted value.
• PEF is less reliable in COPD than in asthma.
Lung volumes:
• Measurement of lung volumes provides an assessment of hyperinflation, where TLC,
FRC and RV are increased.
Diffusion capacity:
• The presence of emphysema is suggested by low gas transfer (reduced diffusion
capacity)
Arterial blood gases and oximetry
• May demonstrate resting or exertional hypoxaemia
• Arterial blood gas analysis provides additional information about PaCO2 and pH,
where hypercapnoea is a feature of advanced disease.
• PaO2 usually remain normal until FEV1 is < 50% of predicted. hypercapnoea is not
expected until FEV1 is <25% of predicted.
Imaging
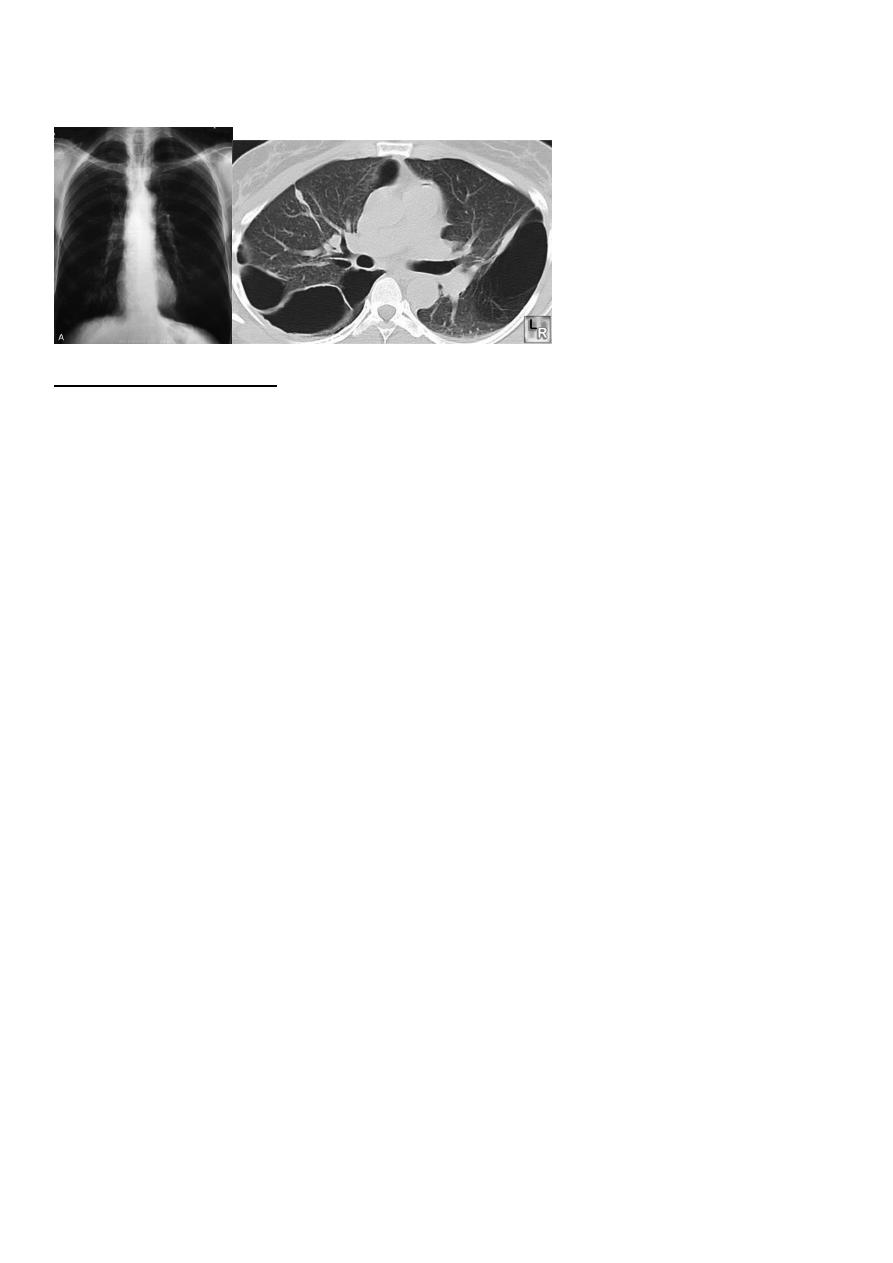
• Chest X-ray: typical changes of emphysema include paucity of parenchymal markings,
hyper-translucency and bulae. Increasing lung volume and flattening of diaphragm
suggest hyperinflation.
6
• High resolution CT scan (HRCT) is the definitive test to exclude the diagnosis of
emphysema. However, this is only required when planning for surgery
Additional investigations:
• Full blood count to exclude anaemia or polycythaemia
• α1 anti-proteinase assay in young patients with predominant emphysema
