1
Forth stage
Medicine
Lec-1
.د
حسين محمد
1/1/2014
Acute diarrhea
Diarrhoea
Passage of abnormally liquid stools at an increased frequency.
For adults stool weight 200 g/d.
Infective diarrhoea Is usually short-lived lasting <10 days.
Causes of infectious gastroenteritis
Toxin in food: < 6 hours incubation
Bacillus cereus
Staph. Aureus
Clostridium spp. enterotoxin
Bacterial: 12-72 hours incubation
Vibrio cholerae
Enterotoxigenic E. coli
Shiga toxin-producing E. coli
Enteroinvasive E. coli
Viral: short incubation
Rotavirus
Norovirus "winter vomiting disease"
Protozoal: long incubation
Giardiasis
Cryptosporidium
Microsporidiosis
Amoebic dysentery
Isosporiasis
The majority of episodes are due to infections spread by the faecal-oral route .
Salmonella
Shigella
Campylobacter
Clostridium difficile

2
The clinical features
depend on the Organisms , Bacillus cereus, S.aureus and Vibrio cholerae, elute exotoxins,
which exert their major effects on the stomach and small bowel, and produce vomiting
and/or so-called secretory diarrhoea, watery without blood or faecal leucocytes.
The incubation period is short and little systemic upset occurs.
Shigella, Campylobacter and enterohaemorrhagic E. coli (EHEC) ,may directly invade the
mucosa of the small bowel or produce cytotoxins that cause mucosal ulceration, typically
affecting the terminal small bowel and colon.
The incubation period is longer and more systemic upset occurs, with prolonged bloody
diarrhoea.
Salmonella spp. are capable of invading enterocytes, and of causing both a secretory
response and invasive disease with systemic features. This is seen with Salmonella typhi
and S. paratyphi (enteric fever), and, in the immunocompromised host, with non-typhoidal
Salmonella spp.
Clinical assessment
The history ,include foods ingested, duration and frequency of diarrhoea, the presence of
blood, abdominal pain and tenesmus, and whether other members have been affected.
Fever and bloody diarrhoea suggest an invasive disease.
Examination
Assessment of the degree of dehydration by skin turgor, pulse and blood pressure, urine
output.
Investigations
Stool inspection for blood and microscopy for leucocytes, and also an examination for ova,
cysts and parasites .
Stool culture should be performed.
FBC and serum electrolytes indicate the degree of inflammation and dehydration.
Management
Patients with acute, potentially infective diarrhoea should be appropriately isolated to
minimise spread.
If the history suggests a food-borne source, public health measures must be implemented
to identify the source .
3
Fluid replacement
The fluid lost in diarrhoea is isotonic. Absorption of electrolytes from the gut is an active
process requiring energy.
Infected mucosa is capable of very rapid fluid and electrolyte transport if carbohydrate is
available as an energy source.Oral rehydration solutions (ORS) therefore contain sugars, as
well as water and electrolytes .
Intravenous fluid if there is vomiting.
Those with cardiac or renal disease, monitoring of urine output and central venous pressure
may be necessary.
The volume of fluid replacement
1. Replacement of established deficit. After 48 hours of moderate diarrhoea (6-10
stools per 24 hours) the average adult will lose 1-2 L, vomiting will compound this,
rapid replacement of 1-1.5 L, either orally (ORS) or by IV normal saline, within the
first 2-4 hours
2. Replacement of ongoing losses. The average adult's diarrhoeal stool accounts for a
loss of 200 mL of isotonic fluid. Rehydration sachets provide 200 mL of ORS; one
sachet per diarrhoea stool is an appropriate replacement.
3. Replacement of normal daily requirement
Adult daily requirement of 1-1.5 L of fluid,increased substantially in fever or a hot
environment.
Antimicrobial agents
In non-specific gastroenteritis, antibiotics have been shown to shorten symptoms by only 1
day. This benefit, when related to the potential for the development of antimicrobial
resistance or side-effects, does not justify treatment.
Evidence suggests that, in EHEC infections, the use of antibiotics may make the
complication of haemolytic uraemic syndrome more likely due to increased toxin release.
Antibiotics should therefore not be used routinely in bloody diarrhoea.
Conversely, antibiotics are indicated in
1. Sh. dysenteriae infection and
2. invasive salmonellosis, in particular typhoid fever.

4
3. Antibiotics may also be advantageous in cholera epidemics, reducing infectivity and
controlling the spread of infection.
4. If there is systemic involvement and a host with immunocompromise or significant
comorbidity.
Antidiarrhoeal, antimotility and antisecretory agents are not recommended in acute
infective diarrhoea and their use may even be contraindicated.
Bacillary dysentery (shigellosis)
Gram-negative rods.
Four main groups:
Sh. dysenteriae, flexneri, boydii and sonnei.
In the tropics bacillary dysentery is usually caused by Sh. flexneri.
The organism only infects humans and its spread is facilitated by its low infecting dose of
around 10 organisms.
Spread may occur via contaminated food or flies, but transmission by unwashed hands
after defecation is by far the most important factor. Outbreaks occur in mental hospitals,
and other closed institutions.
Clinical features
Disease severity varies from mild Sh. sonnei infections that may escape detection to more
severe Sh. flexneri infections, while those due to Sh. dysenteriae may be fulminating and
cause death within 48 hours.
In a moderately severe illness, the patient complains of diarrhoea, colicky abdominal pain
and tenesmus. Stools are small, and after a few evacuations contain blood and purulent
exudate with little faecal material. Fever, dehydration and weakness occur, with tenderness
over the colon.
Arthritis or iritis may occasionally complicate bacillary dysentery (Reiter's syndrome),
associated with HLA-B27.
Management
Oral rehydration therapy or, if diarrhoea is severe, intravenous replacement of water and
electrolyte loss is necessary.
Antibiotic therapy with ciprofloxacin (500 mg 12-hourly for 3 days).
Antidiarrhoeal medication should be avoided.
5
Prevention
The prevention of faecal contamination of food and milk. The isolation of cases may be
difficult, except in limited outbreaks. Hand-washing is very important.
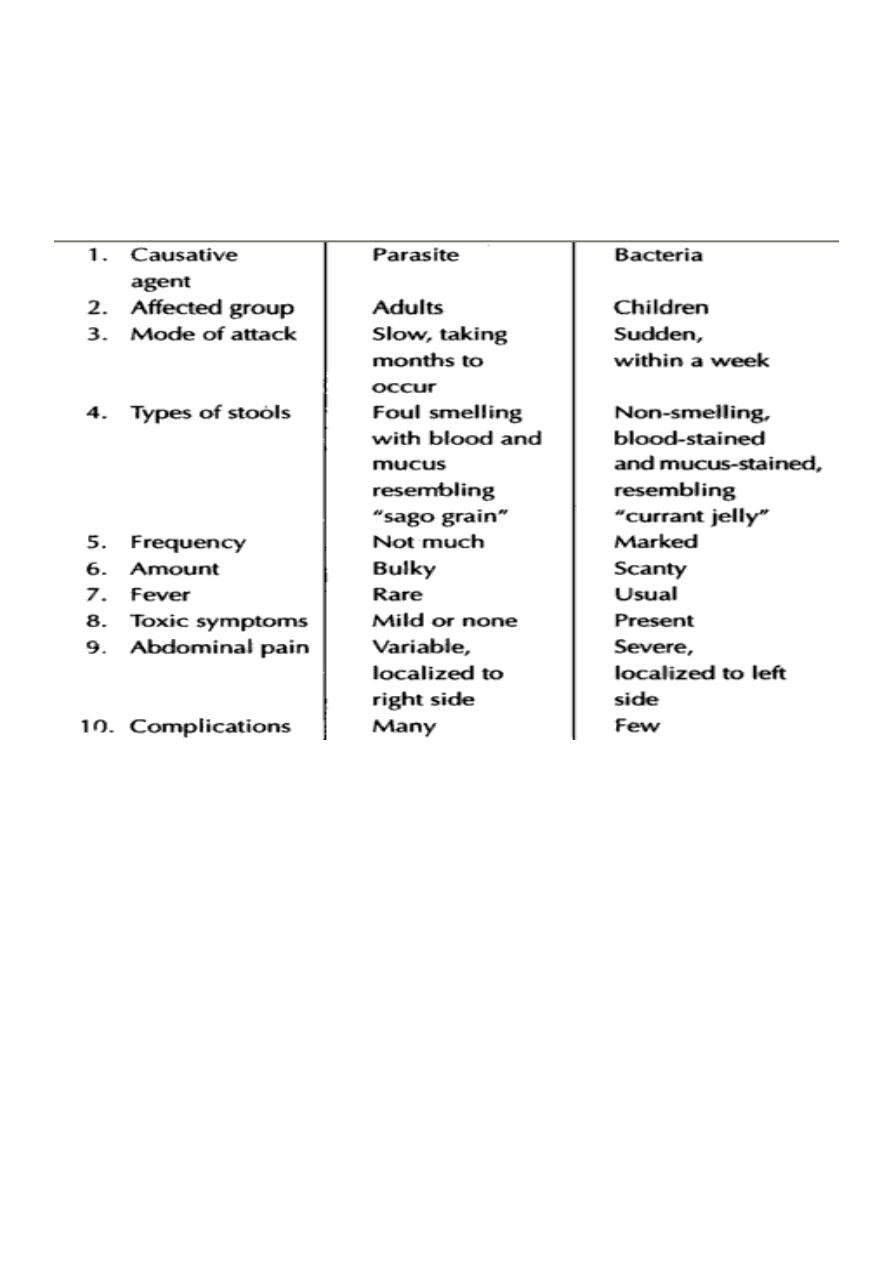
Differences Between Amebic &Bacillary Dysentery
