1
4th stage
Medicine
Lec-16
د.جاسم
8/3/2016
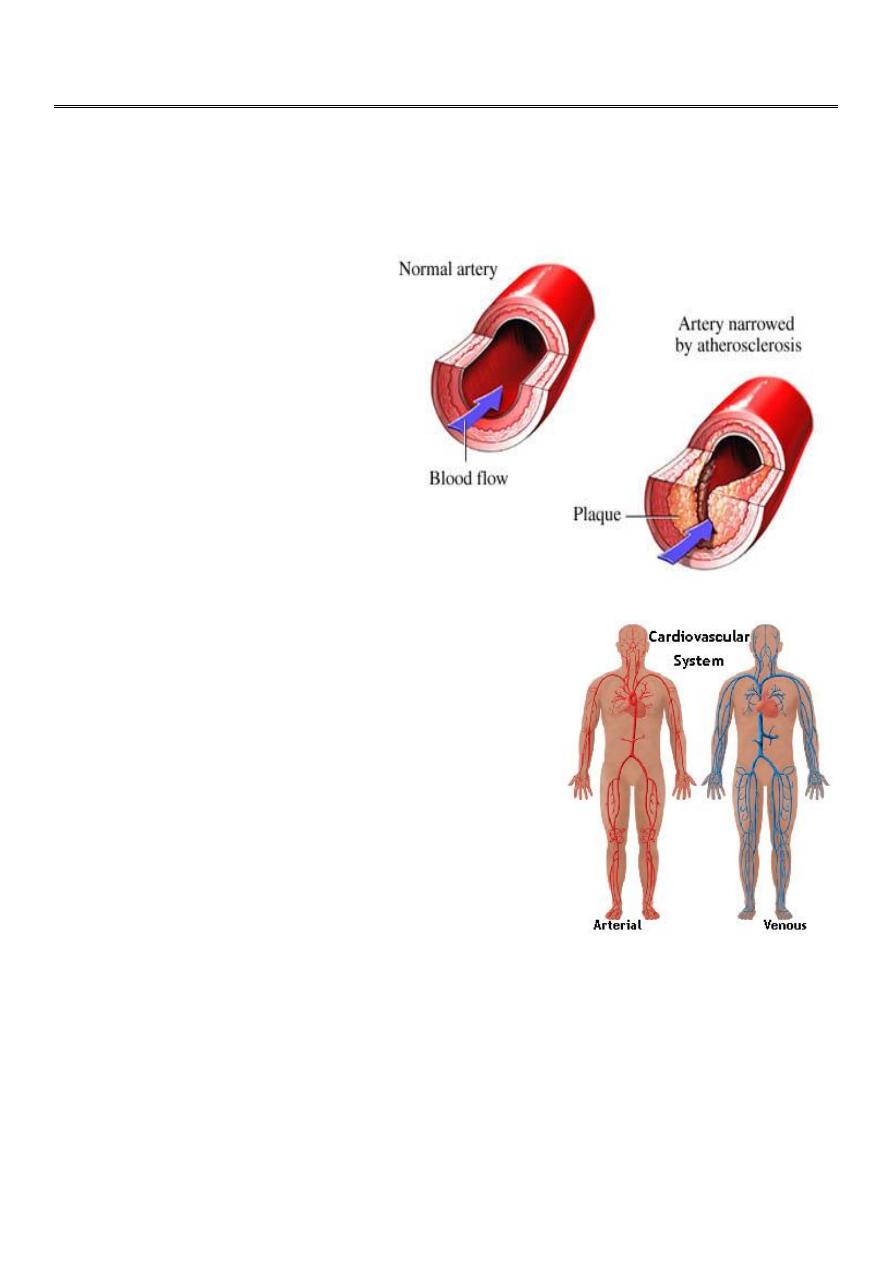
Peripheral Artery Disease
ETIOLOGY :
Risk factors
- Smoking
- Diabetes Mellitus
- Dyslipidemia
- Hypertension
Increased Risk:
50 years old
Male
African American
Obese
Personal history of vascular disease, MI, or
stroke
Chronic lower limb arterial disease
• PAD affects the leg eight times more often
than the arm. Lower limb ischaemia presents
as two distinct clinical entities: intermittent claudication (IC) and critical
limb ischaemia (CLI). The presence and severity of ischaemia can be
determined by clinical examination and measurement of the ankle-brachial
pressure index (ABPI), which is the ratio between the (highest systolic)
ankle and brachial blood pressures. In health the ABPI is > 1.0, in IC
typically 0.5–0.9 and in CLI usually < 0.5.
2
Intermittent claudication (IC) :
Ischaemic pain affecting the muscles of the leg upon walking. The pain is usually
felt in the calf because the disease most commonly affects the superficial femoral
artery. However, the pain may be felt in the thigh or buttock if the iliac arteries
are involved. Typically, the pain comes on after a reasonably constant
‘claudication distance’, and rapidly subsides on stopping walking
Clinical features of chronic lower limb ischaemia :
• Pulses: diminished or absent
• Bruits: denote turbulent flow
• Reduced skin temperature
• Pallor on elevation and rubor on dependency (Buerger’s sign)
• Superficial veins that fill sluggishly and empty (‘gutter’) upon minimal
elevation • Muscle-wasting
• Skin and nails: dry, thin and brittle
• Loss of hair
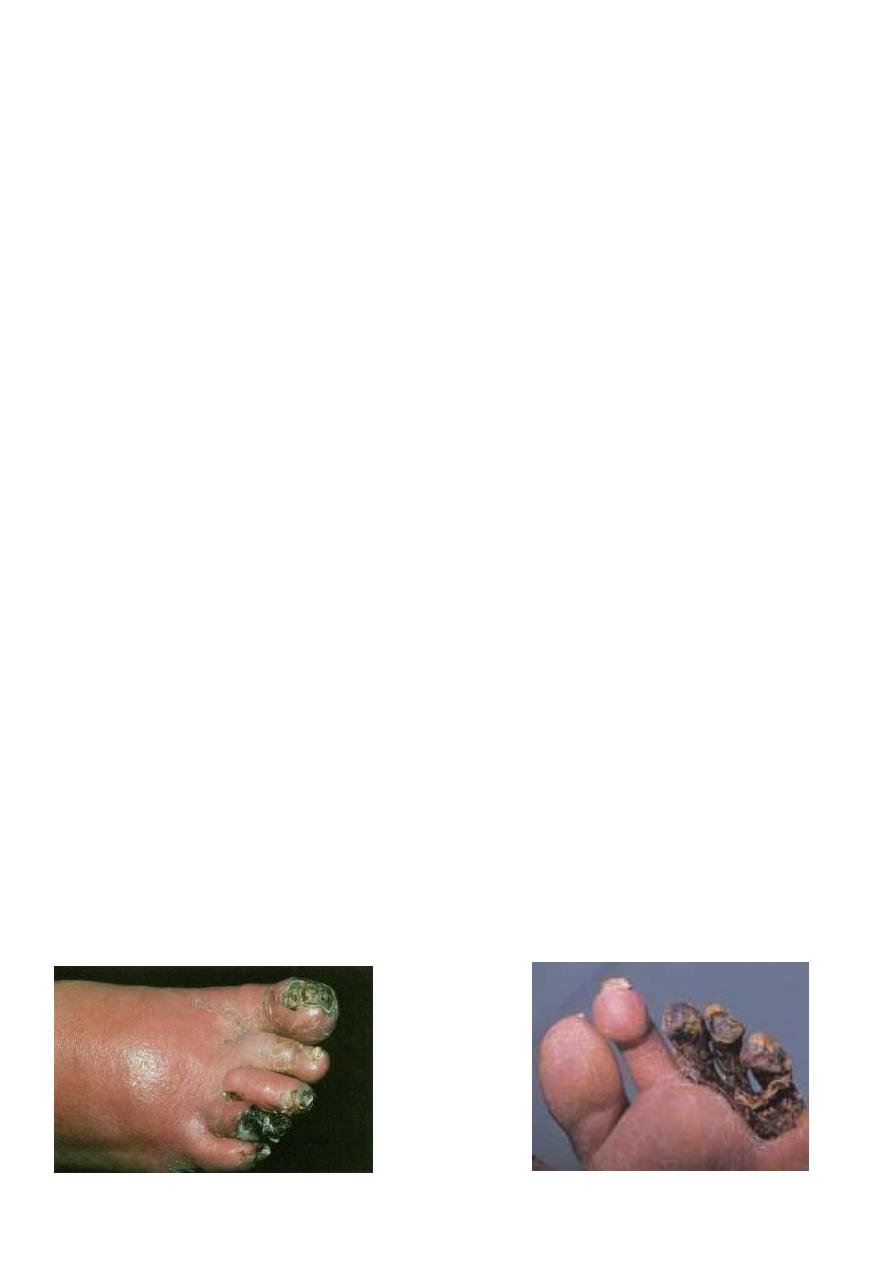
Critical limb ischaemia (CLI):
• Rest (night) pain, requiring opiate analgesia, and/or tissue loss (ulceration
or gangrene), present for more than 2 weeks, in the presence of an ankle BP
of < 50mmHg
• at high risk of losing their limb, and sometimes their life, in a matter of
weeks or months without surgical bypass or endovascular revascularisation
by angioplasty or stenting.
Tissue necrosis a.k.a gangrene

3
Critical limb ischaemia (CLI) :
• Rest (night) pain, requiring opiate analgesia, and/or tissue loss (ulceration
or gangrene), present for more than 2 weeks, in the presence of an ankle BP
of < 50mmHg
• at high risk of losing their limb, and sometimes their life, in a matter of
weeks or months without surgical bypass or endovascular revascularisation
by angioplasty or stenting.
Buerger’s disease (thromboangiitis obliterans) :
• Inflammatory obliterative arterial disease usually presents in young (20–30
years) male smokers. It is most common in those from the Mediterranean
and North Africa. It characteristically affects distal arteries, giving rise to
claudication in the feet or rest pain in the fingers or toes. Wrist and ankle
pulses are absent but brachial and popliteal are present.. It often remits if
the patient stops smoking; sympathectomy and prostaglandin infusions may
be helpful. Major limb amputation is the most frequent outcome if patients
continue to smoke.
Raynaud’s phenomenon and Raynaud’s disease :
• Cold (and emotional) stimuli may trigger vasospasm, leading to the
characteristic sequence of digital pallor due to vasospasm, cyanosis due to
deoxygenated blood, and rubor due to reactive hyperaemia.
• Primary Raynaud’s phenomenon (or disease) This affects 5–10% of young
women aged 15–30 years in temperate climates and may be familial. It does
not progress to ulceration or infarction, and significant pain is unusual. The
underlying cause is unclear. The patient should be reassured and advised to
avoid exposure to cold. Long-acting nifedipine may be helpful.
Secondary Raynaud’s phenomenon (or syndrome) :
• This tends to occur in older people in association with connective tissue
disease (most commonly systemic sclerosis ,vibration induced injury and
thoracic outlet obstruction (e.g. cervical rib). Unlike primary disease, it is
often associated with fixed obstruction of the digital arteries, fingertip
ulceration, and necrosis and pain. The fingers must be protected from cold
and trauma,. Sympathectomy helps for a year or two. Prostacyclin infusions
are sometimes helpful.

4
Acute limb ischaemia :
This is most frequently caused by acute thrombotic occlusion of a pre-existing
stenotic arterial segment, thromboembolism, and trauma which may be
iatrogenic. All patients with suspected acutely ischaemic limbs must be discussed
immediately with a vascular surgeon; a few hours can make the difference
between death/ amputation and complete recovery of limb function
Symptoms/signs :
1. Pain
2. Pallor
3. Pulselessness
4. Perishing cold Unreliable, as the ischaemic limb takes on the ambient
temperature
5. Paraesthesia
6. Paralysis Important features of impending irreversible ischaem
Investigations :
Duplex ultrasonography,
MRI or CT with intravenous injection of contrast agents.
Intra-arterial digital subtraction angiography is usually reserved for those
undergoing endovascular revascularisation.
Diabetic vascular disease ‘diabetic foot :
• Approximately 5–10% of patients with PAD have diabetes
• Arterial calcification Resistant to angioplasty Immunocompromise
• Multisystem arterial disease Coronary and cerebral arterial disease increase
the risk of intervention
• Distal disease Diabetic vascular disease has a predilection for the calf
vessels.
• Sensory neuropathy Even severe ischaemia and/or tissue loss may be
completely painless. often present late with extensive destruction of the
foot an deformity (Charcot joints) .
5
• Motor neuropathy Weakness of the long and short flexors and extensors
leads to abnormal foot architecture, abnormal pressure loads, callus
formation and ulceration.
• Autonomic neuropathy This leads to a dry foot deficient in sweat that
normally lubricates the skin and contains antibacterial substances. Scaling
and fissuring create a portal of entry for bacteria.
Treatment :
- Smoking cessation
-Drugs antiplatlets,cilostazol,Statins
-Regular exercise
-Angioplasty/PTCA
-Bypass grafting
-Sympathectomy
-Digit/Limb Amputation
Happy womEn’s day ^_*
SH.J
