
1
Forth stage
Medicine
Lec-14
د
.
ج
ا
س
م
م
ح
م
د
8/3/2015
Aortic Diseases
Aortic Aneurysm
• Defined as an abnormal dilatation of the aortic lumen;
• A true aneurysm involves all the layers of the wall, whereas a false aneurysm does
not.
• Categorized morphologically as either fusiform or saccular
• Categorized anatomically by location
Anatomic Classification
Ascending aneurysms:
(60%)
Aortic arch:
(10%)
Descending aorta
: (40%)
Thoracoabdominal aorta
(10 %)
Aneurysm Etiology
• Cystic medial degeneration leading to weakening of the aortic wall..***
• Associated with normal aging.
• Accelerated by hypertension
• Associated with connective tissue disorders when found in younger age patients
• Descending aortic aneurysms are highly associated with atherosclerosis and, hence,
atherosclerosis risk factors:
Hypertension
Hypercholesterolemia
Smoking
• Genetic factors
• Aortitis

2
Marfan’s syndroMe
This disorder of connective tissue is inherited as an autosomal dominant trait.
Affected systems include:
1. The skeleton:
arachnodactyly,
Joint hypermobility,
Scoliosis
Chest deformity and high arched palate).
1. The eyes (dislocation of the lens) and
2. The cardiovascular system (aortic disease and mitral regurgitation).
Weakening of the aortic media leads to aortic root dilatation aortic regurgitation and
aortic dissection
Thoracic aortic aneurysm
These may produce:
• Chest pain,
• Aortic regurgitation,
• Compressive symptoms such as stridor (trachea, bronchus) and hoarseness
(recurrent laryngeal nerve), and
• Superior vena cava syndrome .If they erode into adjacent structures
• E.g. aorto-oesophageal fistula, massive bleeding occurs.
Abdominal aortic aneurysms (AAAs)
AAAs are present in 5% of men aged over 60 years and
80% are confined to the infrarenal segment..
Men are affected three times more commonly than women.
AAA can present in a number of ways.
The usual age at presentation is 65–75 years.
Ultrasound is the best way of establishing the diagnosis, and
Of following up patients with asymptomatic aneurysms.
CT provides more accurate information.
3
Aneurysm Management
• Surgery indicated in:
>5.5cm requires consideration for repair
>6 cm has a 50% rupture rate in 5 years
Mortality for acute rupture repair approaches50%
Elective repair has a much lower mortality
Distal embolisation is a strong indication for repair.
As experience with endovascular stenting and repair increases, recommendations
may change
•
Medical therapy
during observation involves:
– SMOKING CESSATION
– ß blockade
– Other antihypertensive?
–
Statin therapy
4
2
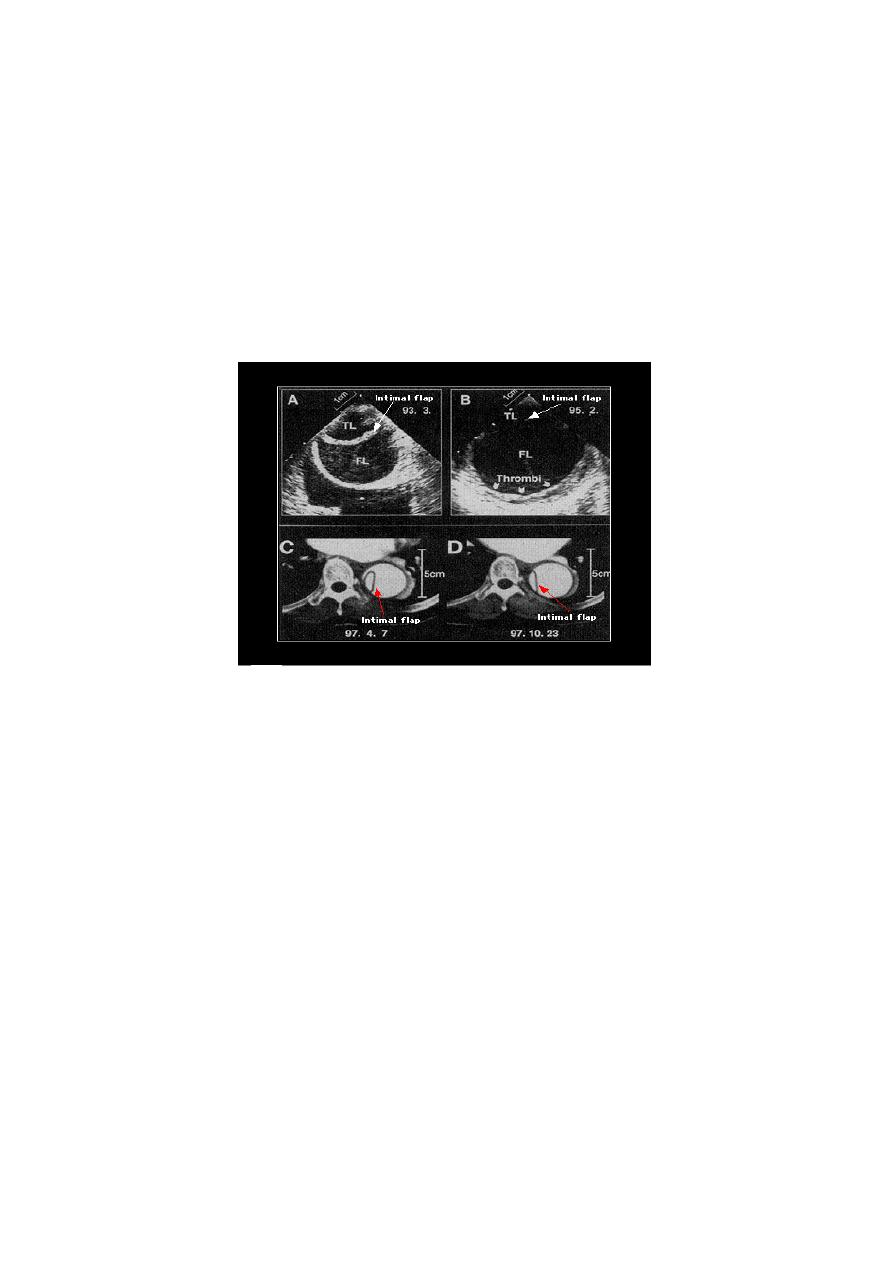
-Aortic Dissection
A breach in the integrity of the aortic wall allows arterial blood to enter the media,
which is then split into two layers, creating a ‘false lumen’ alongside the existing or ‘true
lumen’.
The aortic valve may be damaged and the branches of the aorta may be compromised.
Typically, the false lumen eventually re-enters the true lumen, creating a double-
barrelled aorta, but it may also rupture into the left pleural space or pericardium with
fatal consequences.
Factors that may predispose to aortic dissection
• Hypertension (80% of cases)
• Aortic atherosclerosis
• Non-specific aortic aneurysm
• Aortic coarctation
• Collagen disorders (e.g. Marfan’s syndrome)
• Previous aortic surgery (e.g. CABG, aortic valve replacement)
• Pregnancy (usually third trimester)
• Trauma
• Iatrogenic (e.g. cardiac catheterization).
5
Clinical Manifestations
1.
Involvement of the ascending aorta typically gives rise to anterior chest pain, and
involvement of the descending aorta to intrascapular pain.
2.
The pain is typically described as ‘tearing’ and very abrupt in onset; collapse is
common.
3.
There may be asymmetry of the brachial, carotid or femoral pulses and signs of
aortic regurgitation.
4.
Occlusion of aortic branches may cause MI, stroke, paraplegia, mesenteric infarction
with an acute abdomen, renal failure (renal) and acute limb (usually leg) ischaemia
.
Investigations
• The chest X-ray characteristically shows broadening of the upper mediastinum.
• ECG may show left ventricular hypertrophy (LVH) in patients with hypertension, or
rarely changes of acute MI (usually inferior).
• Doppler echocardiography may show
Aortic regurgitation,
A dilated aortic root and, occasionally,
The flap of the dissection.
Transoesophageal echocardiography is particularly helpful because transthoracic
echocardiography can only image the first 3–4 cm of the ascending aorta).
• CT and MRI angiography are both highly specific and sensitive.
Aortic Dissection Classification
• Stanford Classification
• Type A, involving the ascending aorta, regardless of point of entry.
• Type B, involving the descending aorta,(ie from the left subclavian artery distal).
Aortic Dissection Treatment
Ascending (type A) dissections are surgical emergencies
• Mortality rate is 1 to 2 %/hr. once diagnosis is made
• 50% in hospital mortality if unoperated

6
Type B (descending aortic) dissection can be:
Managed medically
• ICU admission
• Blood pressure control
– IV ß blockers
– Labetalol (α&β blocker)
– nitroprusside
Indications to proceed to
surgery
Complications including:
• Branch occlusion
• Continued aortic expansion
• Dissection extension
• Aortic rupture
• Marfan syndrome
A.L.Y
