1
Forth stage
Surgery (Urology)
Lec-16
د.محمد فوزي
21/2/2016
SCROTAL SWELLINGS
Anatomy
-Testicle supplied by testicular artery from aorta and drained by spermatic or testicular vein
to the inferior vena cava in the right, and left renal vein in the left.
-Lymphatic drainage to the para aortic lymph nodes.
Common localized swellings:
Hydrocele
Indirect inguinal hernia
Varicocele
Torsion of testes
Infection (orchitis& epididymitis)
Tumors
Trauma
Torsion of testicular or epididymal appendeges
Less common causes:
Hematoma
Idiopathic scrotal edema
Sebaceous cyst
2
Epididymal cyst
spermatocele
Fournier gangrene
Treatment:
-ABCDE
-Scrotal wound suturing in minor cases.
-Testicular exploration under GA and tunica albuginea repair or unilateral orchiectomy in
distructed testis. In bilateral testicular injury some testicular tissue should be saved for
hormonal ( androgen) supply.
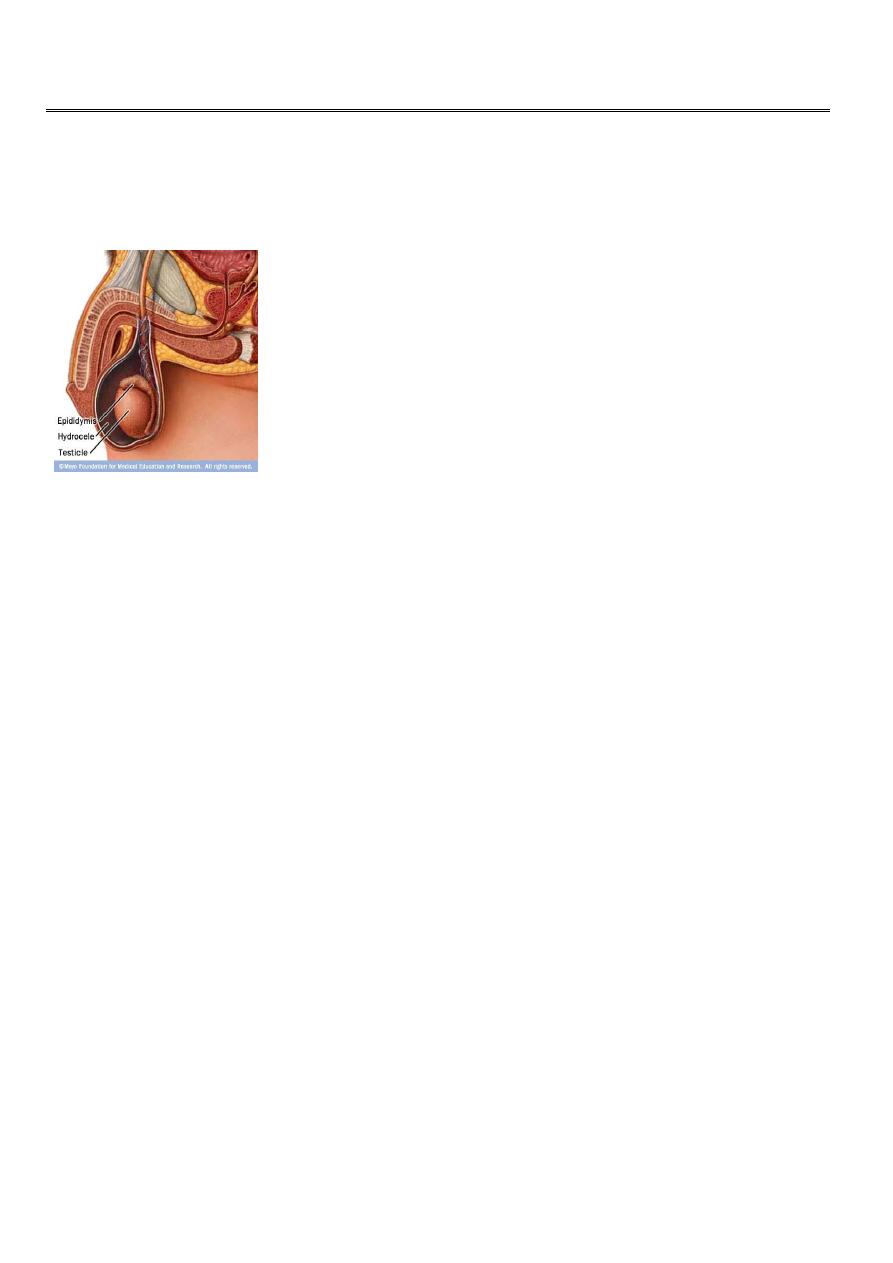
Hydrocele
Excessive collection of clear serous fluid within tunica vaginalis.
Types:
Primary: (idiopathic) most common.
Secondary: infection, tumour, trauma, patent processus vaginalis (communicating) or post
operativeeg. hernia or varicocele.
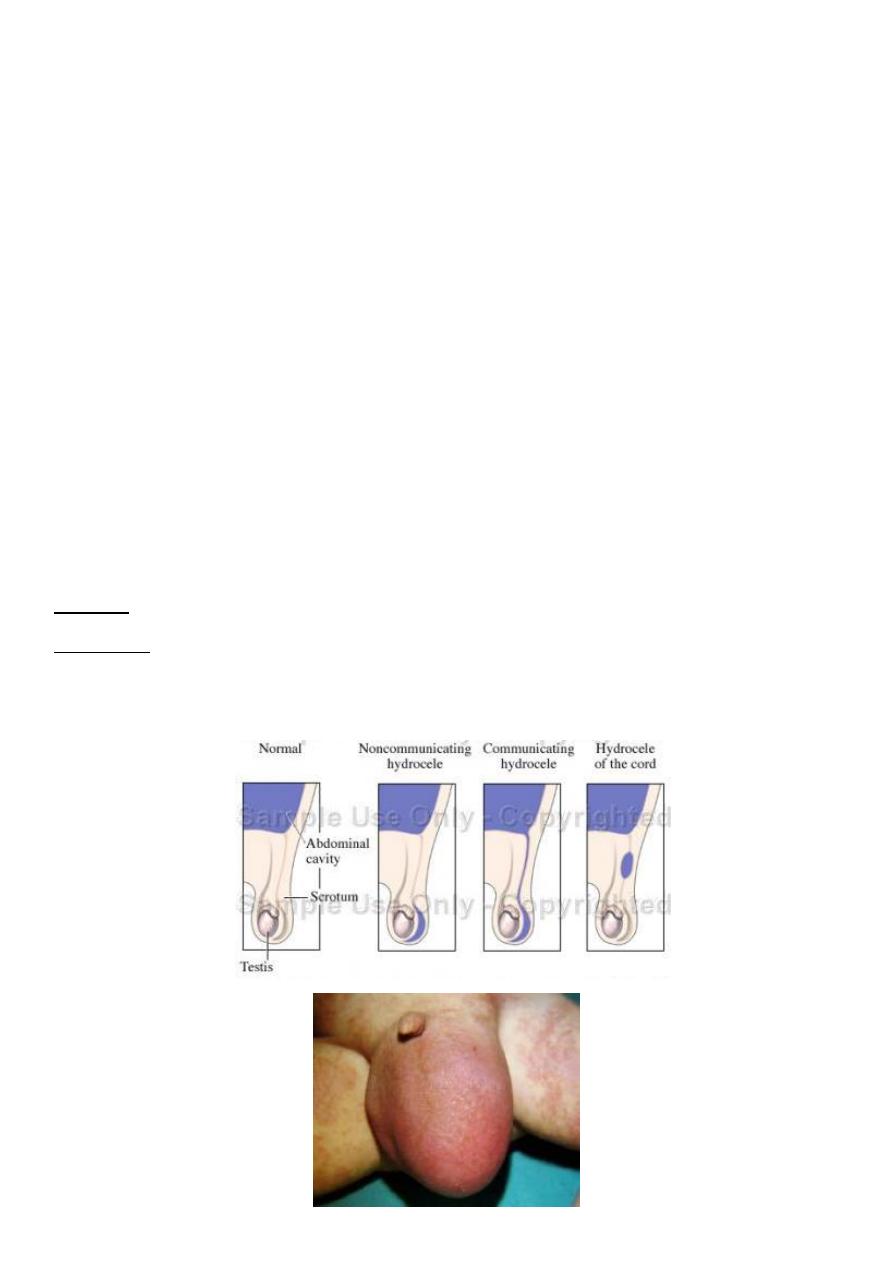
Types of hydrocele
3
Primary (idiopathic) hydrocele
Most common type, occurs in middle age, gradual onset, takes long time and reaches a very
large distressing size.
Pathology: (unknown), diminished fluid absorption by tunica vaginalis.
Tunica may be thickened and calcified.
Complications:
1- Rupture after trauma.
2- Infection after aspiration (pyocele).
3- Change into hematocele after trauma.
4- Calcification of the sac.
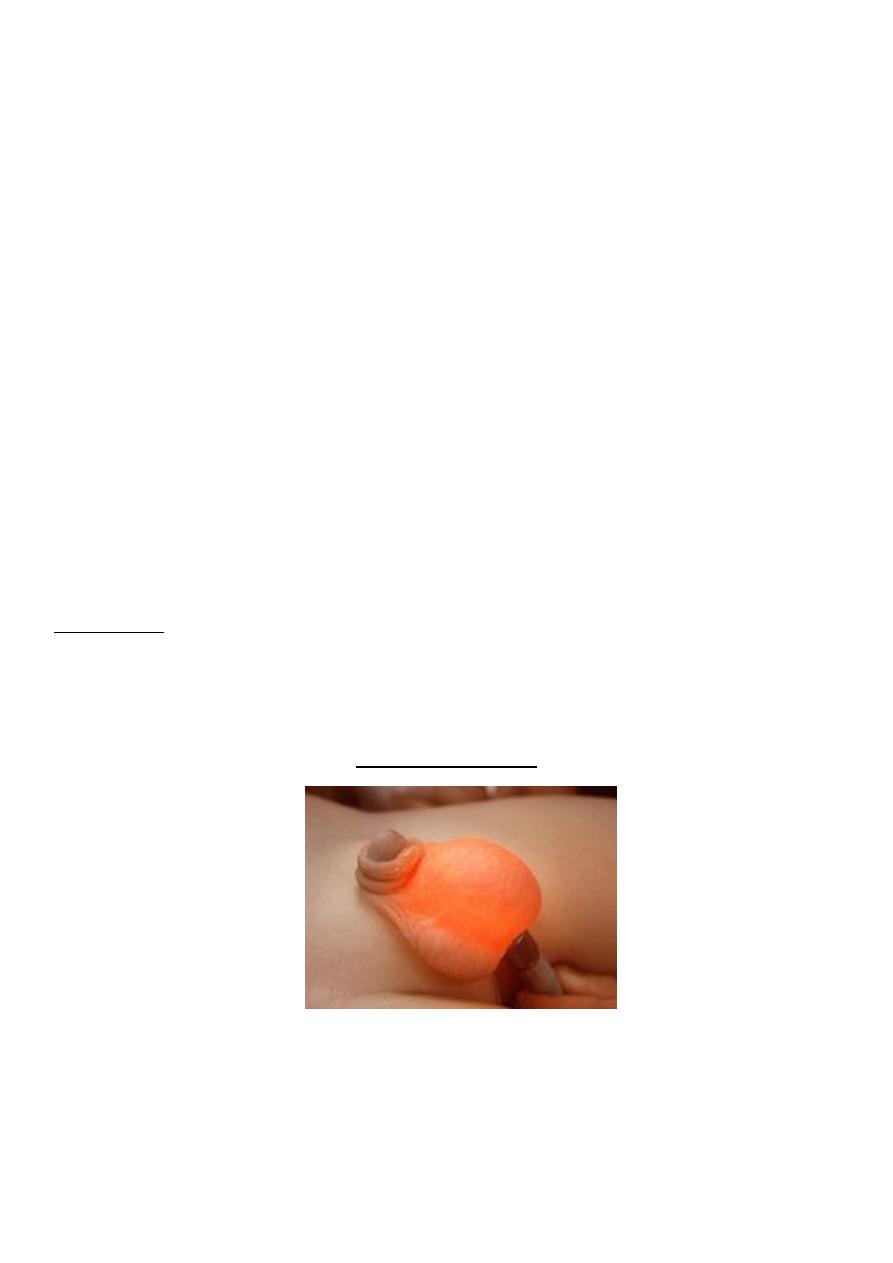
Clinical picture
Gradual onset of unilateral scrotal swelling.
Examination variable size, cystic and smooth swelling. Can get above it. Negative cough
impulse. Trans-illumination positive. Dull in percussion. The testicle is difficult to palpate
non reducible
ULTRASOUND,,,,diagnostic
Trans-illumination in
Treatment
Indicated when it is large and cause patient discomfort.
4
Surgical operations:
Lord’s operation
Jabolley’s
Subtotal excision it for s
Tapping (aspiration): rarely indicated ,mainly for patient who is unfit for surgery
because f of recurrence and complication like infection and bleeding
Infantile (communicating) hydrocele
Present as scrotal swelling at or after birth due to failure of obliteration of the processus
vaginalis.
The swelling increases at crying and decrease at sleeping time.
The condition may subside spontaneously during first year of life otherwise surgical
ligation of the processus vaginalis is indicated to treat the condition.
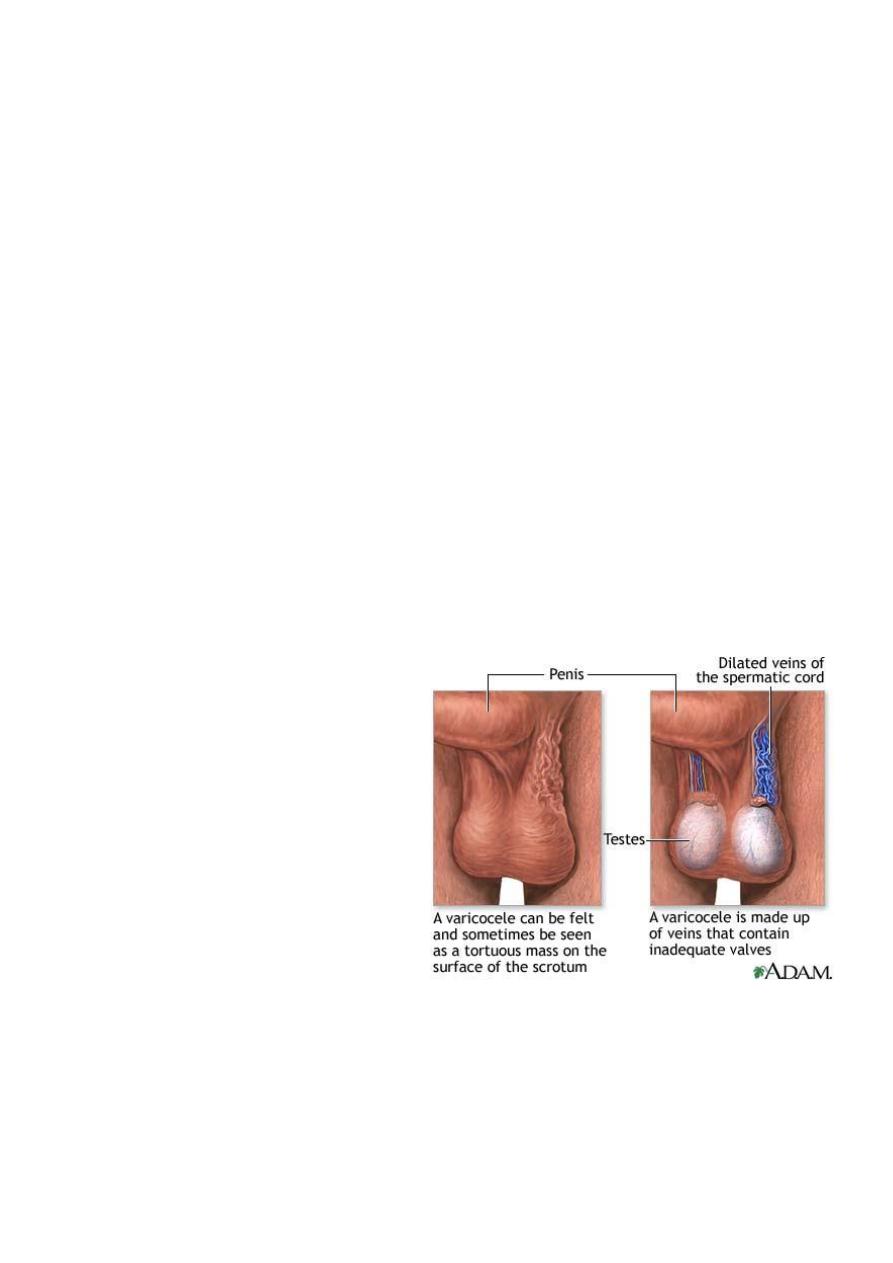
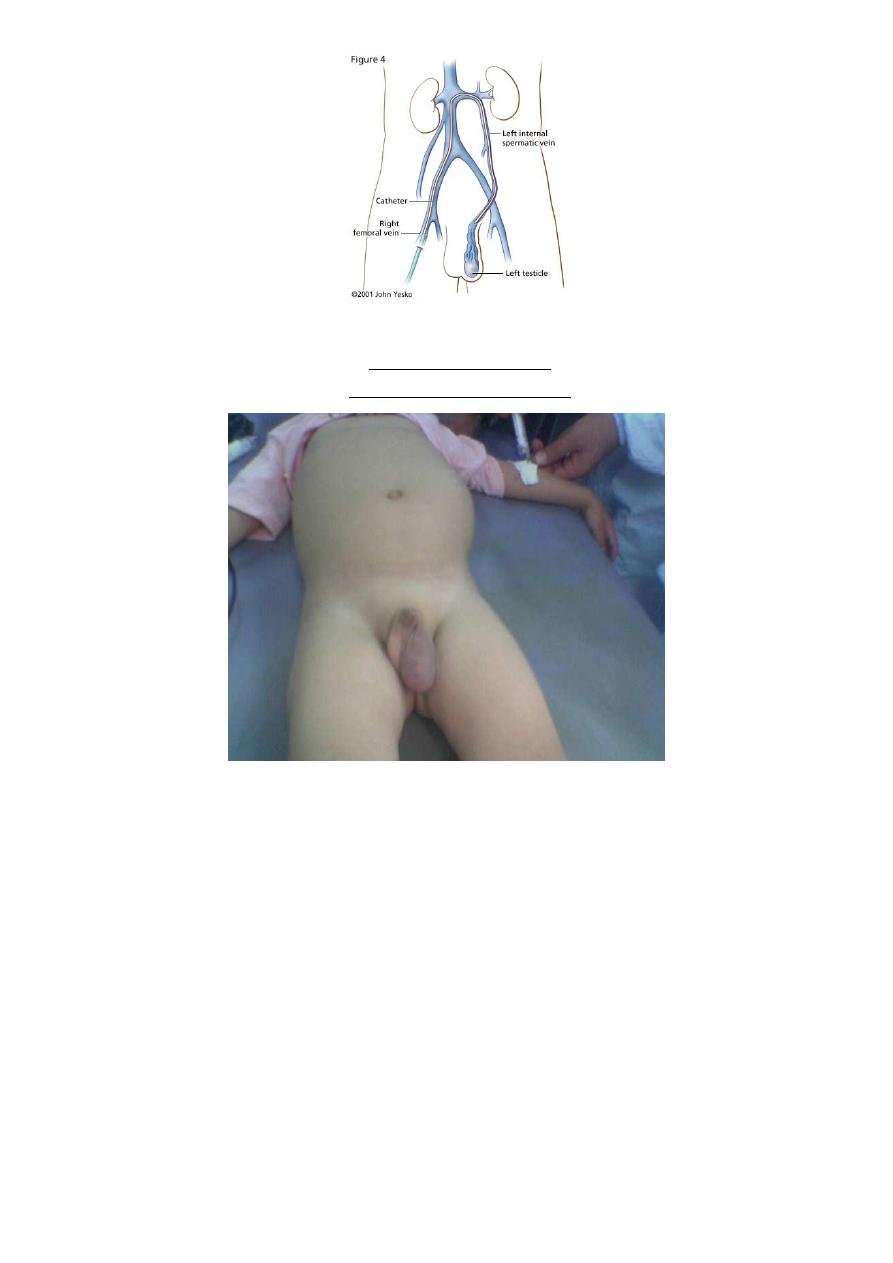
Varicocele
Abnormal dilatation and toruosity of the pampiniform plexus of veins.
Primary: (idiopathic) more common.
Secondary: (due to renal tumor) rare.
Primary varicocele
Affects tall young adults (15-30 y).
Causes: congenital weakness of the venous valves, prolong standing, chronic increase
intra abdominal pressure.
It involves left side mostly because of more perpendicular course of the left
testicular vein to the left renal vein.
Rarely bilateral.
5
Secondary varicocele
note left side renal tumor
Clinical presentation:
Asymptomatic.
Pain: dragging sensation specially on standing or hot weather.
Sterility.
Examination:
Affected side hangs lower than normal.
Varicocele disappear at lying down so ex. to be taken at standing position or during
Valsalva maneuver ,
usually felt as a compressible cords ( bag of worms)..
The affected testis is soft and atrophic.
Abdominal ex is essential to exclude renal tumor
6
Complications:
Sterility: higher scrotal temp. may result in low sperm count, asthenospermia (low
motility) and testicular atrophy.
Secondary hydrocele.
Repeated thrombosis..
Investigations:
Doppler u/s.
Seminal fluid analysis.
Abdominal u/s to exclude renal pathology.
Treatment:
Reassurance, scrotal support and avoidance of the hot places. Analgesia for pain.
Surgical treatment indicated in:
Pain not responding to treatment.
Infertility (30-60% improvement)
Associated conditions eg hernia
adolescent age
Types of surgery:
Sub inguinal microscopic approach (best).
Inguinal approach.
Retroperitoneal (Paloma
’
s).
Laparoscopic
Radiologically controlled embolization
For secondary varicocele the treatment directed to the cause.
7
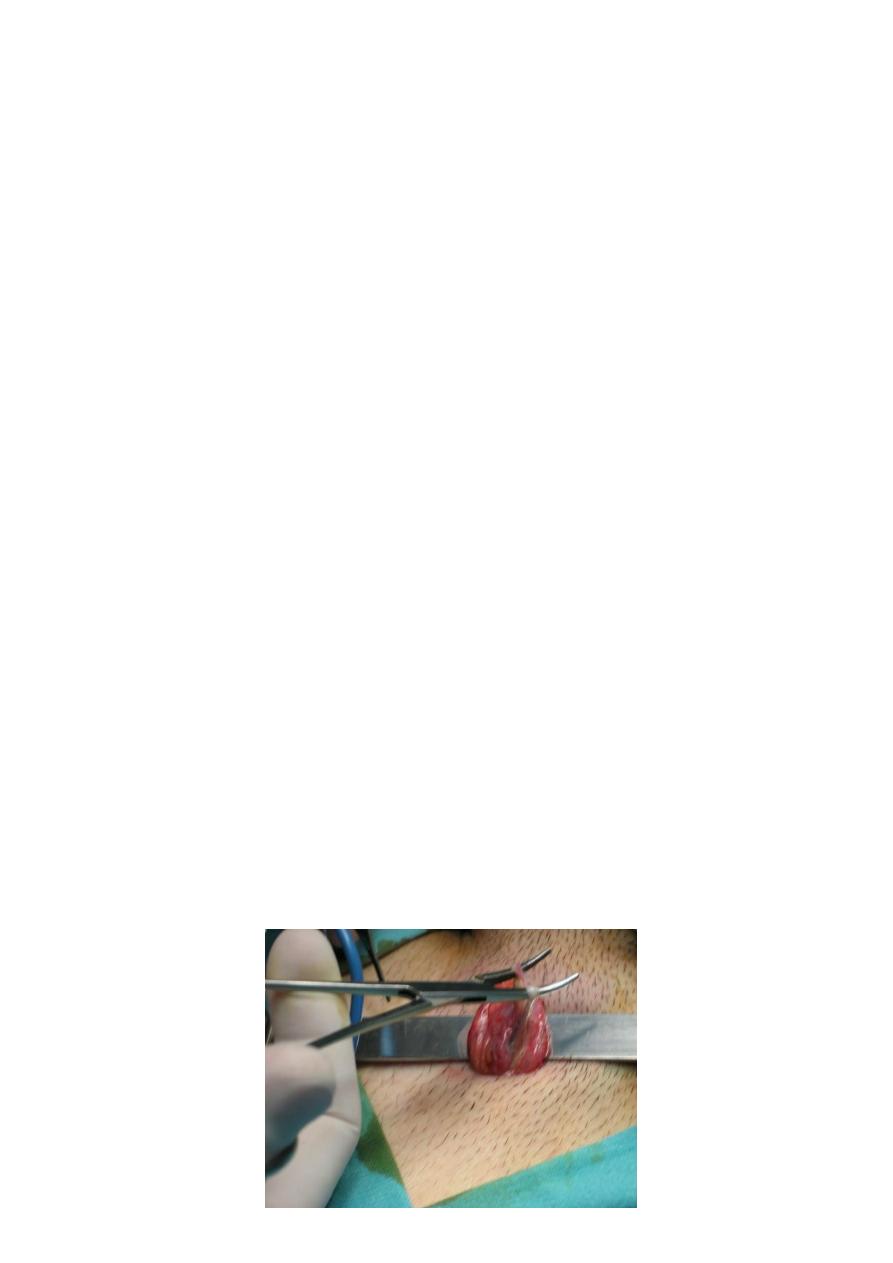
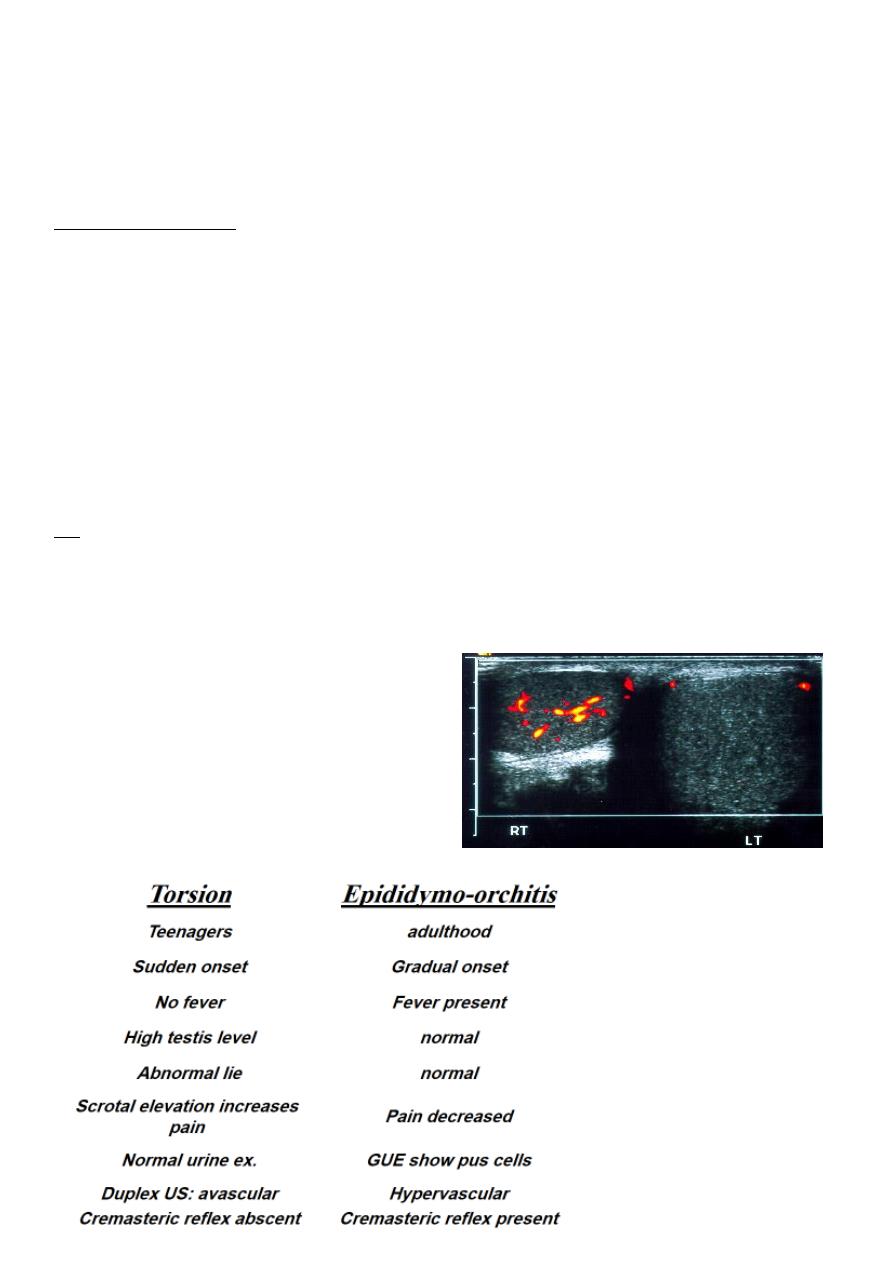
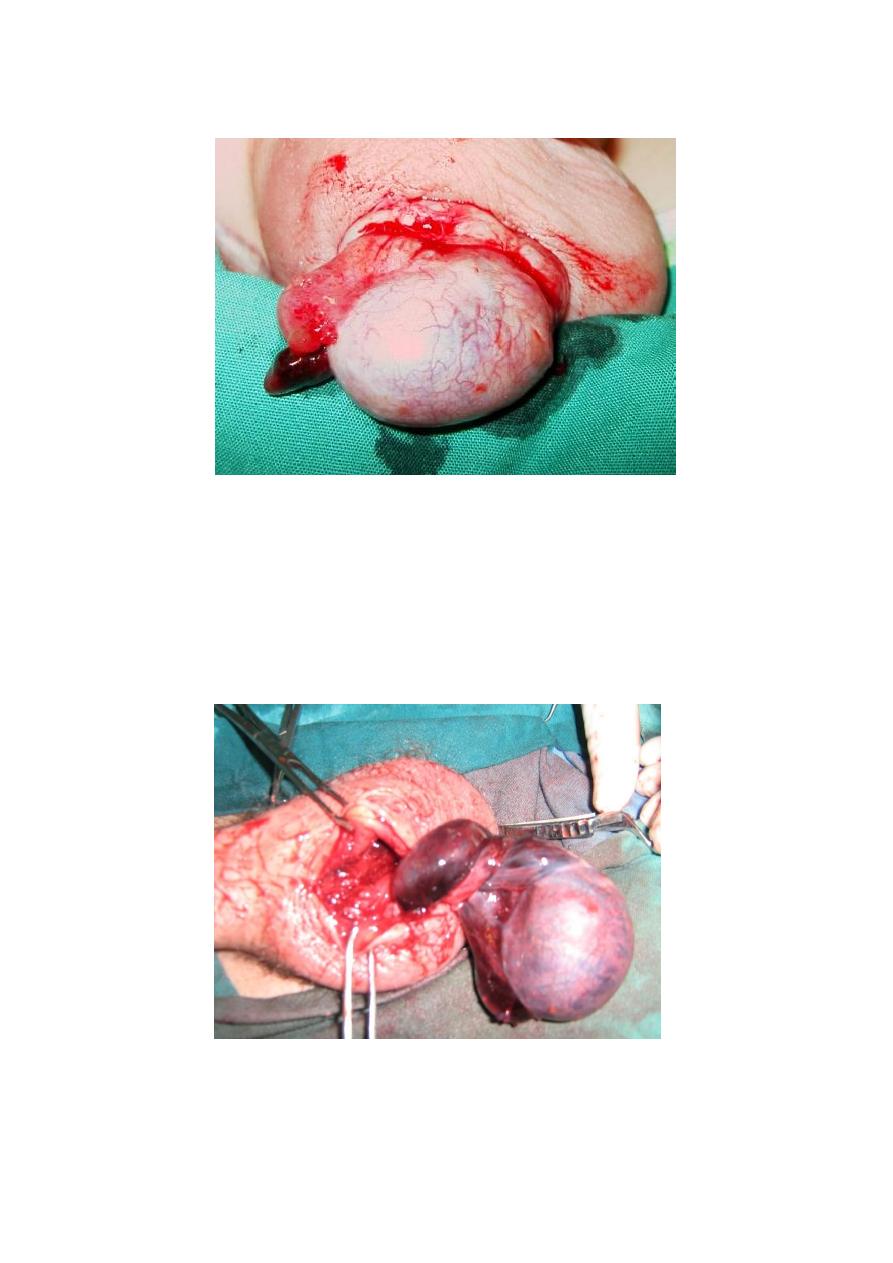
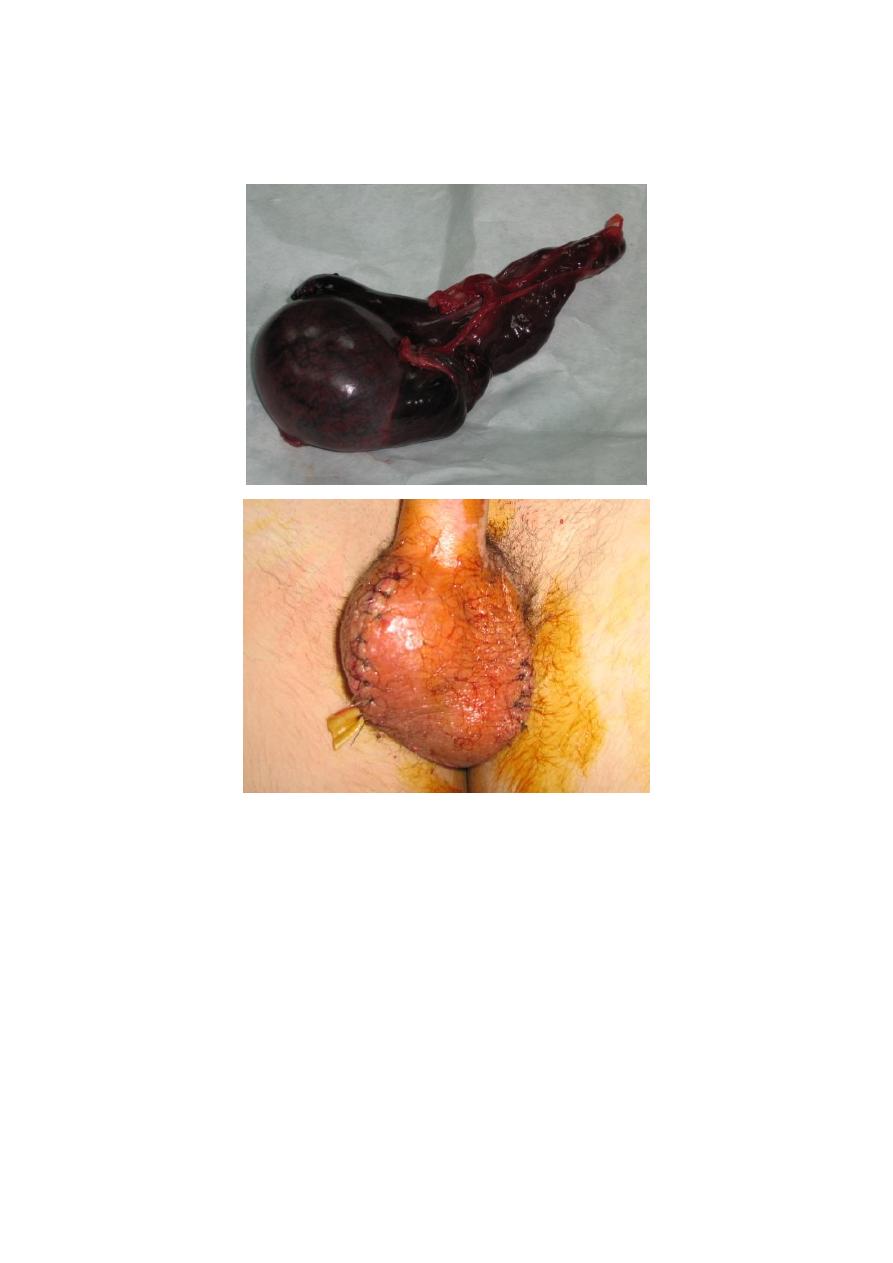
Torsion of the testis (spermatic cord)
Torsion of the testis & epididymis around the axis of the spermatic cord. Resulting in
ischemia and testicular gangrene.
Predisposing factors:
Imperfect descent.
Long mesorchium.
Abnormal lie.
Clinical picture:
Usually involve early teenagers. Sudden severe agonizing scrotal pain radiate to the lower
abdomen or loin associated with vomiting and sweating.
Ex. Swollen, red and severely tender scrotum.
The testicle is higher in position and abnormal lie (transverse or oblique) (Angle’s sign).
Scrotal elevation increases the pain,prehn sign.
Diagnosis:
Depends on the clinical picture, no fever.
GUE: normal.
Duplex U/S: avascular testis.
8
Appendicular torsion
Treatment
Urgent surgical exploration, even in suspicious cases because time factor is very important.
The testis detorted if it is viable, and fixation to the dartuos muscle, or orchiectomy if it is
gangrenous because antibodies may be formed against the healthy testis.
Fixation of the
other testis
because of the
presence of same
predisposing
factors.
9
Epididymo–orchitis
Acute infection of the testis and epididymis
Routs of infection:
1- Ascending: in UTI, instrumentation, catheterization, or after cystoscope and TUR.
2- Blood borne infection. (post mumps).
E.coli, proteus, staph, strept, and gonococcus.
Clinical picture
History of lower urinary symptom, instrumentation or mumps.
11
Acute scrotal and groin pain.
Constitutional symptoms of fever, rigor & malaise.
Swollen red and edematous scrotal skin.
Testis and epididymis are swollen tender and matted together, mild hydrocele is
present.
Scrotal elevation relieves pain (Prehn’s sign +ve)
Treatment
Rest & hydration.
Scrotal support.
Analgesia and antipyretics (NSAID).
Broad spectrum A.B. (2-3 wks).
Surgical drainage of the abscess.
Residual swelling may remain for a month.
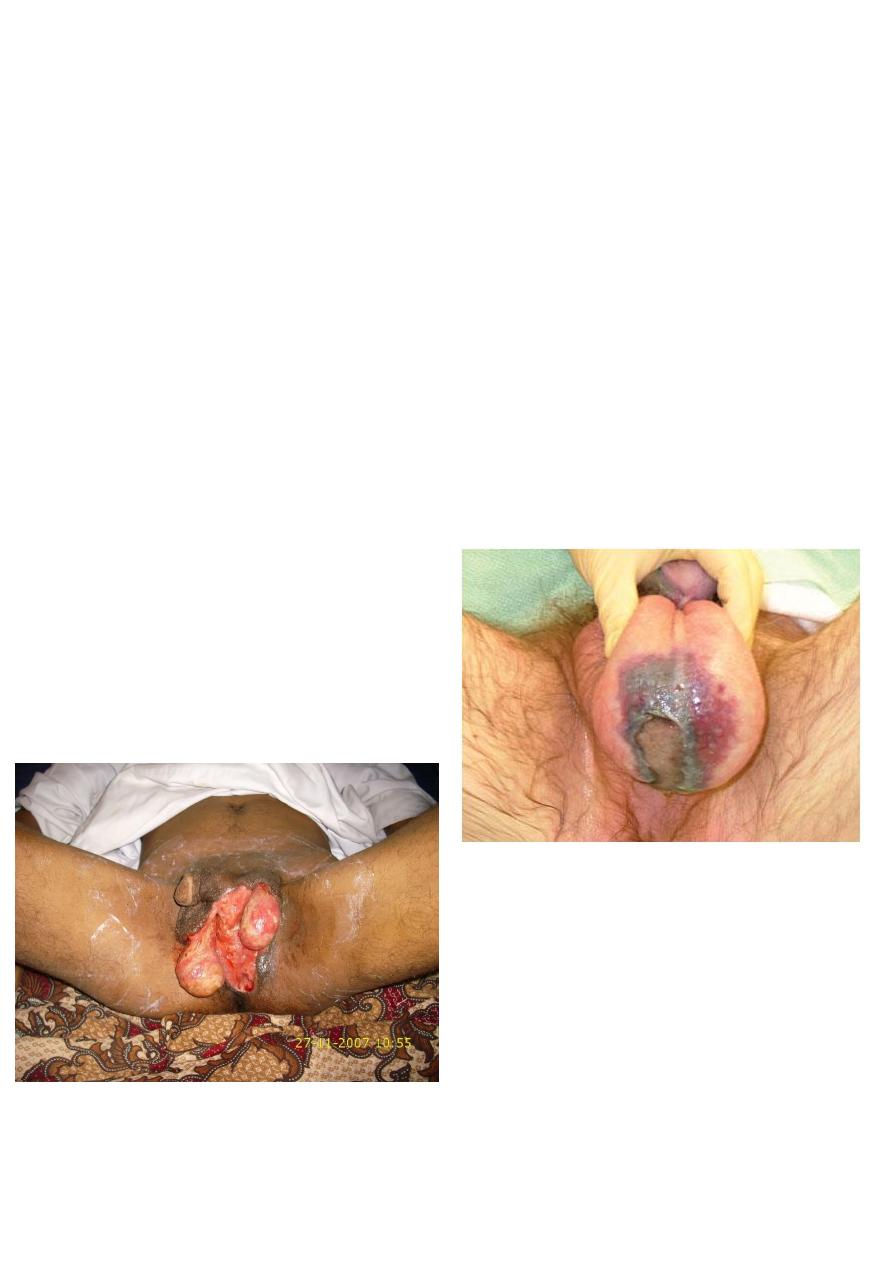
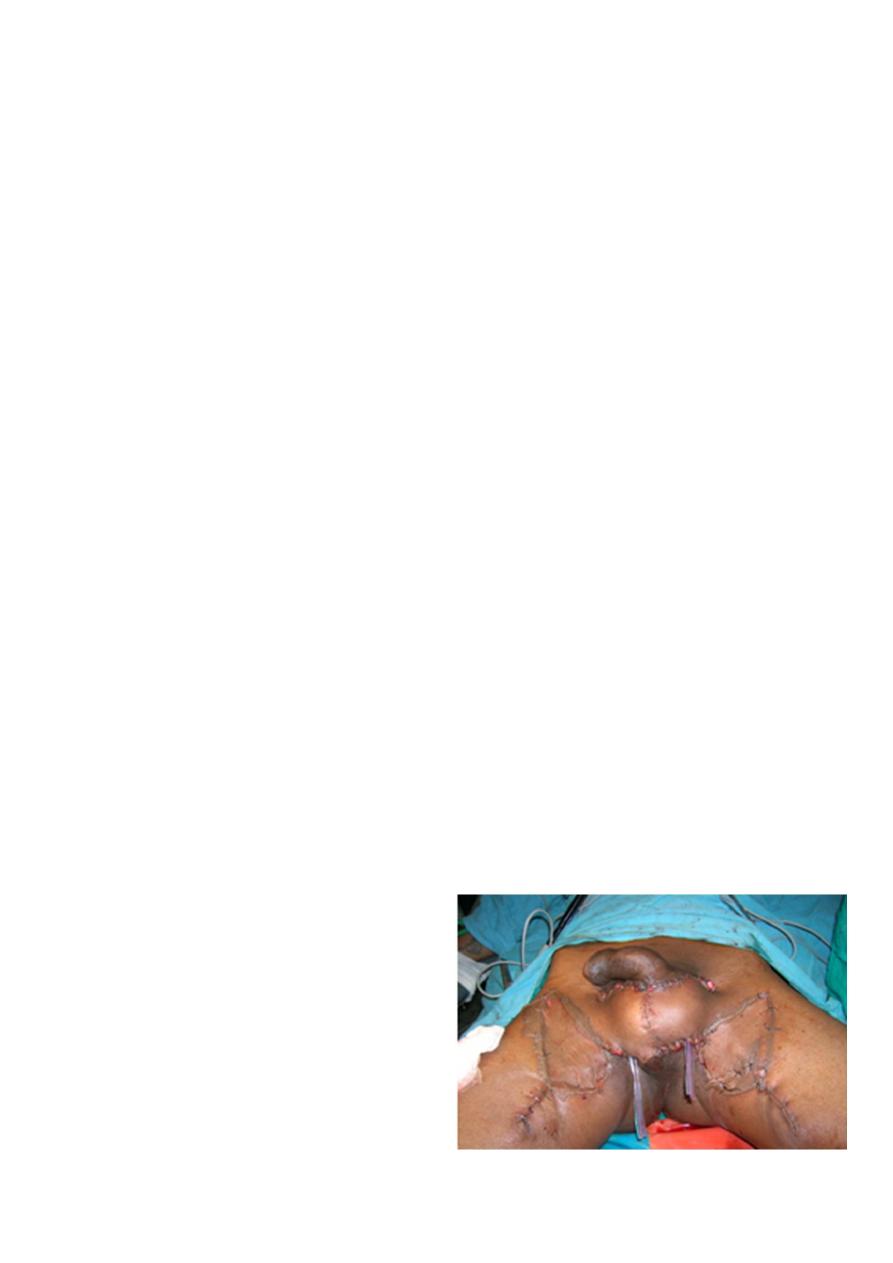
Fournier gangrene
Its necrotsing fasciitis of scrotal skin
Usually occurs in elderly with DM
Rapidly progressive with high mortality
Treatment…urgent
-Admission
-Wound debridment and daily dressing
Parenteral broad spectrum antibiotic
-
11
