
1
Forth stage
Surgery (Urology)
Lec- 4
1
د.محمد فوزي
11/1/2016
Retention of Urine
Acute or Chronic
Acute Retention
Causes of Acute Retention: most frequent are
• Male : 1-BOO 2-Urethral stricture 3-postoperative 4-Acute urethritis or
prostatitis 5-phimosis
• Female :1-Retroverted gravid uterus 2-Multiple Sclerosis
• both :
1-Blood clot in the bladder 6-smooth muscle dysfunction with aging
2-Urethral calculus 7-faecal impaction
3-Rupture of urethra 8-Anal pain (hemorrhoidectomy )
4-Neurogenic (SCI) 9- Some drugs
5-fecal impaction 10-Spinal anesthesia
Clinical Features of Acute Retention of urine
• No urine is passed for several hours
• The bladder may be visible & is tender to palpation & dull to percussion.
• Rarely caudaequina lesion due to prolapsed lumber disc is a cause ( check reflexes in
lower limbs &perineal sensation).
2
Treatment
• In most patients the correct treatment is to pass a
fine urethral catheter & to arrange further urological
management
• occasionally post-op. Retention treated
conservatively.
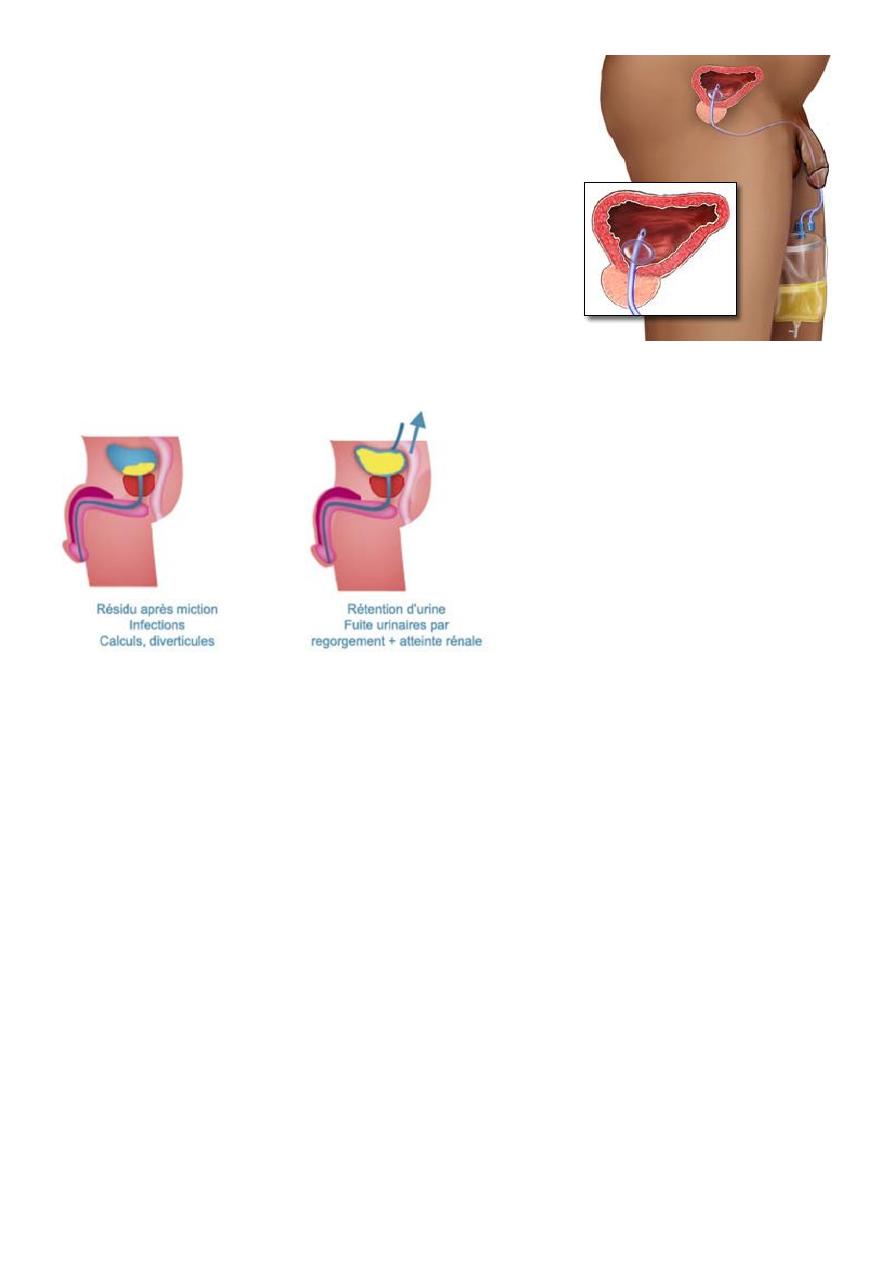
Chronic Retention of Urine
Chronic Vs Acute
-The distention of the bladder is
almost painless
-Risk of upp. Tract dilation
because of high intravesical
tension due to large Residual
urine.
-Painful.
-no risk of upper tract dilation.
-Those with serum creatinin level
>200 mic.mol/l are at risk of
developing a post obstructive
diuresis & haematuria following
catheterisation so careful
monitoring + replacement of
inappropriate urine loss+slow
decompress
-No increase in serum creatinin
3
Retention with overflow
The patient has no control of his or her urine
small amount of urine passing involunterily from time to time from a distended
bladder
it may follow neglected acute or chronic retention
treatment principle similar to acute retention
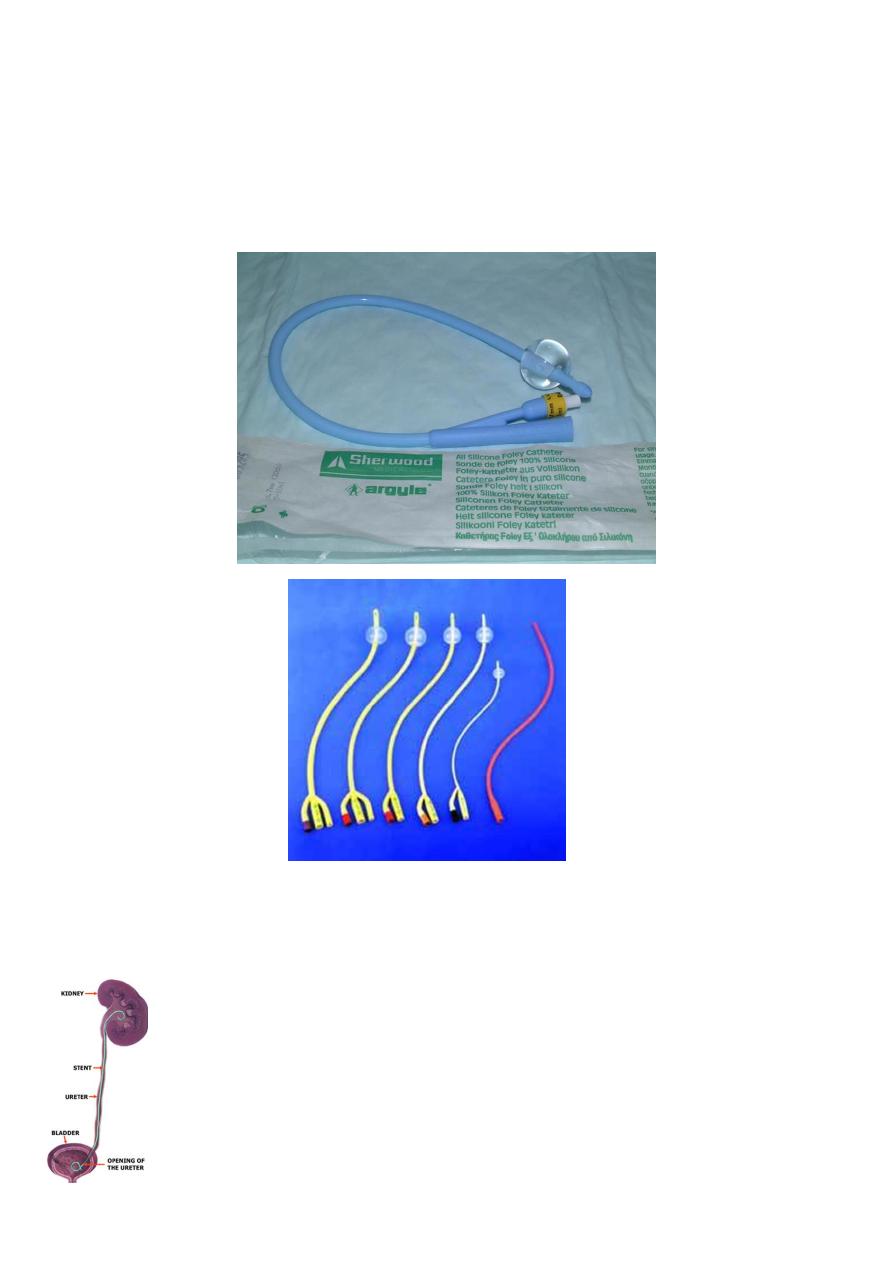
Catheters
Ureteric stent jj
4
Indication
To bypass ureteric obstruction
After ureteric surgery
end to end anastomosis
pyeloplasty for PUJ obstruction
reimplantation of ureter
After uteteroscopic manipulation
With ESWL in a single kidney
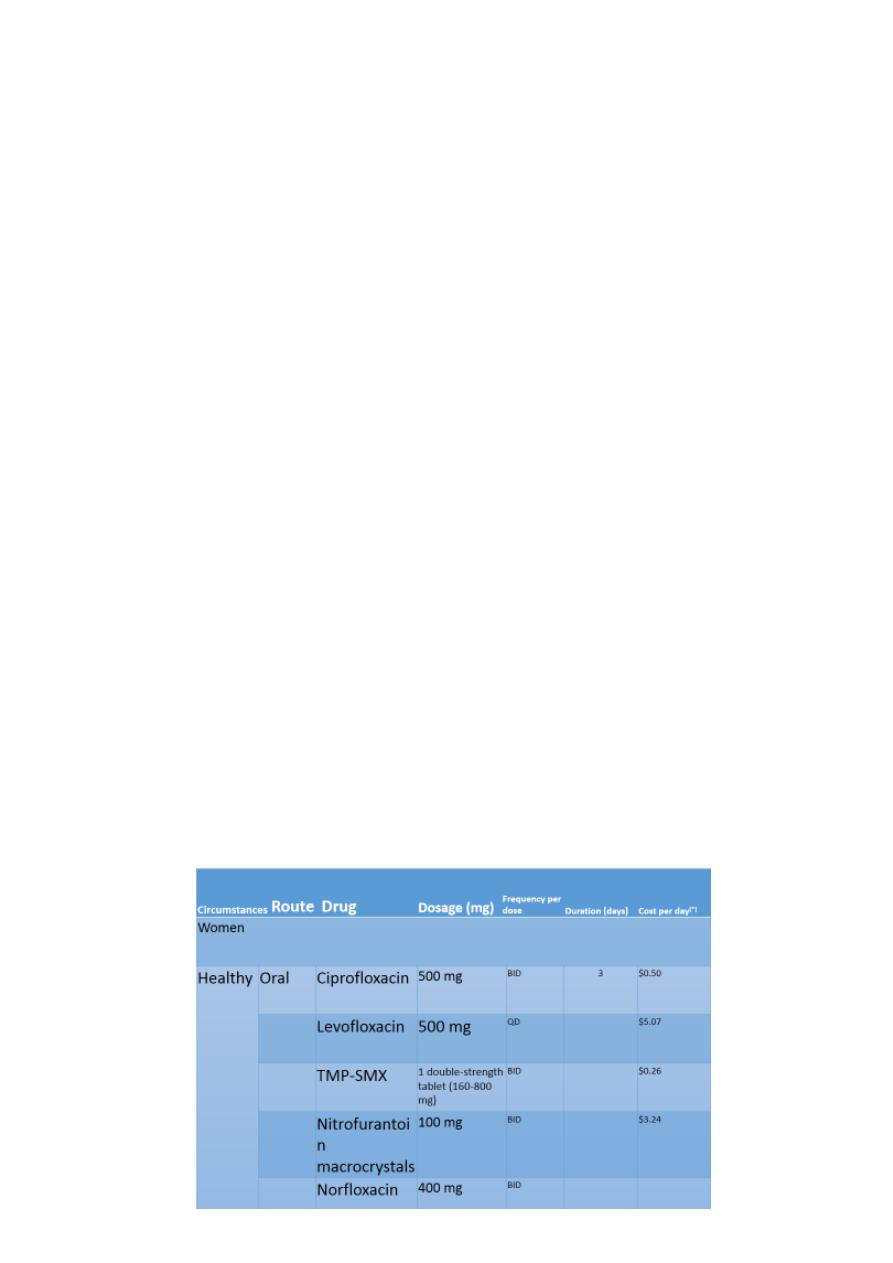
BLADDER INFECTIONS
Uncomplicated Cystitis
.
Clinical Presentation:dysuria, frequency or urgency, and suprapubic pain .Hematuria or
foul-smelling urine may develop.
Because acute cystitis, by definition, is a superficial infection of bladder mucosa, fever,
chills, and other signs of dissemination are not present.
Diagnosis:
a urinalysis that is positive for pyuria, bacteriuria, or hematuria, or a combination
should provide sufficient documentation of UTI and a urine culture may be omitted
.
A urine culture should be obtained for patients i
Treatment:
5
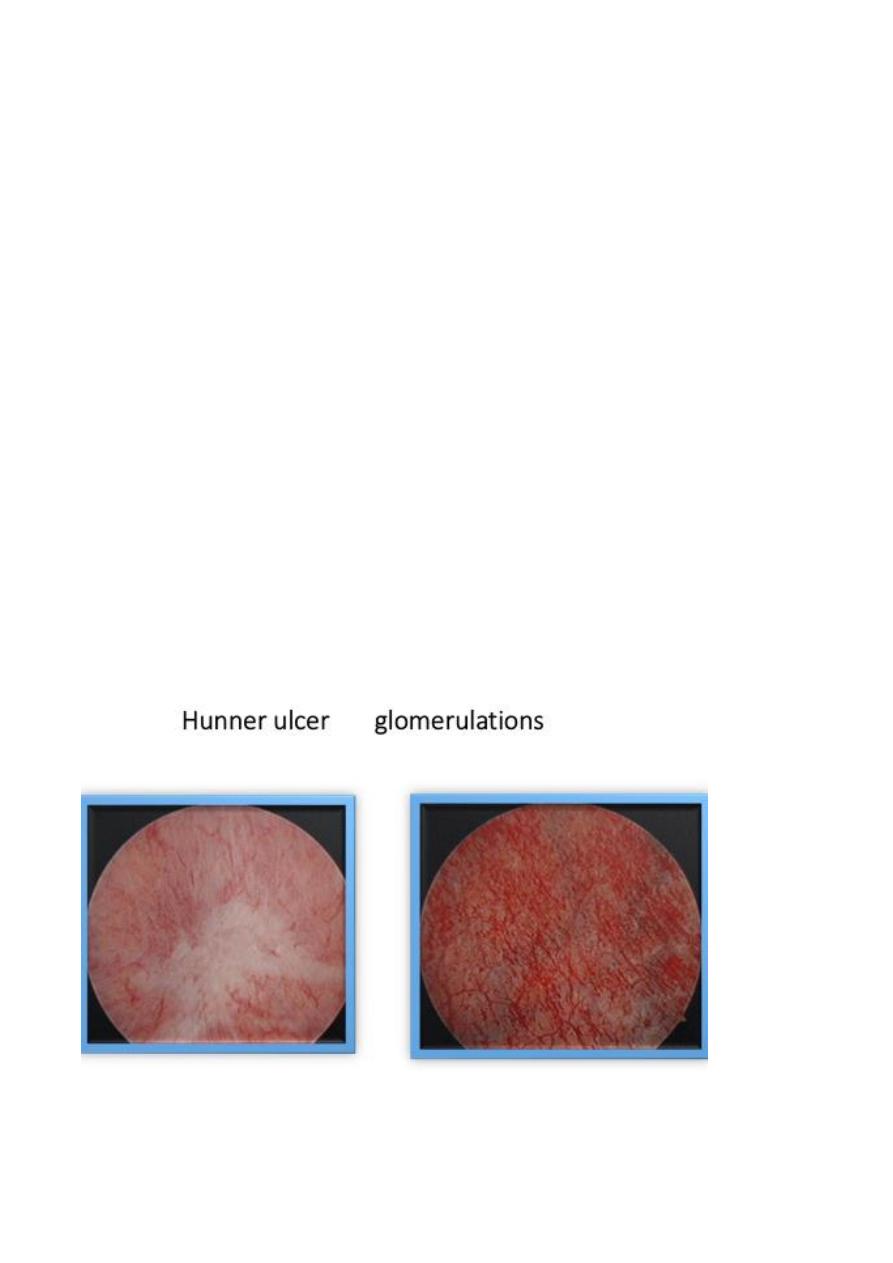
Interstitial cystitis (IC)
Interstitial cystitis (IC) or painful bladder syndrome (PBS), defined as “the complaint
of suprapubic pain related to bladder filling, accompanied by other symptoms such as
increased daytime and night-time frequency, in the absence of proven urinary
infection or other obvious pathology”
Female to male ratio = 5:1
Median age at onset is 40 years .
PBS/IC can be considered one of the chronic visceral pain syndromes, affecting the
urogenital and rectal area, These include vulvodynia, orchialgia, penile pain, perineal
pain, and rectal pain.
IC is a diagnosis of exclusion , laboratory tests include urine dipstick ,urine culture in
all patients .
urine cytology done in risk group only
Urodynamic study .
Kcl PARSON TEST.
Cystoscopy under general or spinal anesthesia.
