1
Forth stage
surgery
Lec-6
Dr.Ahmed
4/10/2015
Pruritis Ani
This is intractable itching around the anus. Usually the skin is reddened
hyperkeratotic and may become cracked and moist.
The causes are numerous:
1. pus,
2. polypus,
3. parasites,
4. piles,
5. psyche’.
-Lack of clean lines, excessive sweating, and wearing rough or woolen
underclothing are common causes
-An anal or perianal discharge which renders the anus moist
-The causative lesions include an anal fissure, fistula in ano, prolapsed
internal or external haemorrhoids, genital warts and excessive ingestion of liquid
paraffin
.
-A mucous discharge is an intense pruritic agent and a polyp can be the cause
-A vaginal discharge, especially due to the Trichomonas vaginalis

2
-Parasitic causes: Threadworms in Children should wear gloves at night, less
they scratch the perianal region and are reinfested.
-Scabies and pediculosis pubis may infest the anal region.
-Allergy is sometimes the cause, in which case there is likely to be a history of
other allergic manifestations, such as urticaria, asthma or hay fever.
-Antibiotic therapy may be the precipitating factor.
-Skin diseases localised to the perianal skin : psoriasis, lichen planus and
contact dermatitis.
-Bacterial infection. Intertrigo due to a mixed bacterial infection.
-A psychoneurosis. neurotic individuals become so immersed in their
complaint that a pain pleasure complex develops, the pleasure being the
scratching.
-Diabetes can sometimes present with pruritus ani and the urine should be
tested in all patients.
TREATMENT :
The cause is treated
Other methods include the following :
1- Hygienic measures:
Cotton wool should be substituted for toilet paper.
Soap is avoided .
If there is much anal hair trapping the moisture and discharge, shaving
can be very helpful.
2-Hydrocortisone.
in cases with dermatitis, and only in cases with dermatitis, prednisolone, applied
topically.
3-Operative treatment
This may be necessary for a
concomitant lesion of the anorectum which is thought to initiate or contribute to
the pruritis, Otherwise,surgery is not indicated

3
Hypertrophied Anal Papilla
-Anal papillae present at the dentate line
-As these papillae are present in 60 per cent of patients examined
proctologically, they should be regarded as normal structures
-Anal papillae can become elongated, as they frequently do in the presence of
an anal fissure
-Occasionally, an elongated anal papilla may be the cause of pruritus.
-An elongated anal papilla associated with pain and/or bleeding at defecation
is sometimes encountered in infancy.
-Haemorrhage into a hypertrophied anal papilla can cause sudden rectal pain.
TREATMENT :
Using a proctoscope, elongated papillae without haemorrhoids should be
crushed and excised after injecting the base with local anaesthetic.
Proctalgia Fugax
-This disease is characterised by attacks of severe pain arising in the rectum,
recurring at irregular intervals and apparently unrelated to organic disease.
-The pain is described as cramp-like, often occurs when the patient is in bed at
night, usually lasts only for a few minutes and disappears spontaneously.
-It may follow straining at stool, sudden explosive bowel action or ejaculation.
It seems to occur more commonly in patients suffering from anxiety or undue
stress, and also it is said to afflict young doctors.
-The pain may be unbearable.
-It is unpleasant, incurable, but fortunately harmless and gradually subsides.
4
Non Malignant Strictures
Congenital
Patients who have had an operation for imperforate anus in infancy may
require periodic anorectal dilatation.
Spasmodic
An anal fissure causes spasm of the internal sphincter.
Rarely, a spasmodic stricture accompanies secondary megacolon , possibly due
to chronic use of laxatives.
Organic
Postoperative stricture :
sometimes follows
haemorrhoidectomy performed incorrectly, low coloanal anastomoses, especially
if a stapling gun is used, can narrow down postoperatively.
Irradiation stricture :
Senile anal stenosis :
a condition of chronic internal sphincter contraction is sometimes seen in the
aged. Increasing constipation is present with pronounced straining at stool.

5
Inflammatory bowel disease :
Stricture of the anorectum also complicates ulcerative proctocolitis and most
commonly large bowel Crohn’s disease, A carcinoma should be suspected if a
stricture is found, until a biopsy is obtained.
Endometriosis :
of the rectovaginal septum may present as a stricture. There is usually a history
of frequent menstrual periods with the appearance of severe pain during the first
2 days of the menstrual flow
Neoplastic :
Clinical features
1-Increasing difficulty in defecation is the leading symptom
2-The patient finds that increasingly large doses of aperients are required, and
if the stools are formed, they are ‘pipe-stem’ in shape
.
3-In cases of inflammatory stricture, tenesmus, bleeding and the passage of
mucopus are superadded
.
4-Sometimes the patient comes under observation only when subacute or
acute intestinal obstruction has supervened
.
Rectal examination
.
The finger encounters a sharply defined shelf-like interruption of the lumen
A biopsy of the stricture must be taken
TREATMENT :
Prophylactic
-The passage of an anal dilator during convalescence after haemorrhoidectomy
greatly reduces the incidence of post-operative stricture
-Dilatation by bougies For anal and many rectal strictures at regular intervals is
all that is required
Anoplasty
This technique is particularly useful for postoperative strictures.

6
Colostomy
-Colostomy must be undertaken when a stricture is causing intestinal obstruction,
and in advanced cases of stricture complicated by flstulae in ano
.
-Rectal excision and coloanal anastomosis
-When the strictures are at or just above the anorectal junction, and with a normal
anal canal, but irreversible changes necessitate removal of the area., Eg. post
irradiation
.
Malignant lesions of the anus and anal canal
Carcinoma of the anus differs from carcinoma of the rectum in histological
structure, behavior and types of treatment
.
This is mainly because of its accessibility, its sensitivity and its abundant lymph
drainage, both superficial and deep
.
07
%
of anal tumours arise in the anal canal
.
07
%
are carcinomas of the anal verge
.
Metastases may develop in the inguinal lymph nodes , if the tumour below the
dentate line or in the paraaortic lymph nodes if the tumour above dentate line .
Pathological types
Squamous cell carcinoma : Because of its superficial situation, the presence
of this lesion is frequently recognized by the patient, who often presents
early.
Basaloid carcinoma : is a form of nonkeratinising squamous carcinoma. It
can metastasise to lymph nodes and can be highly malignant. It is not very
sensitive to irradiation.
Mucoepidermal carcinoma : This tumour arises near the squamocolumnar
cell junction and is of average malignancy. It is radiosensitive.
Basal cell carcinoma : These are ‘skin tumors' and behave accordingly.

7
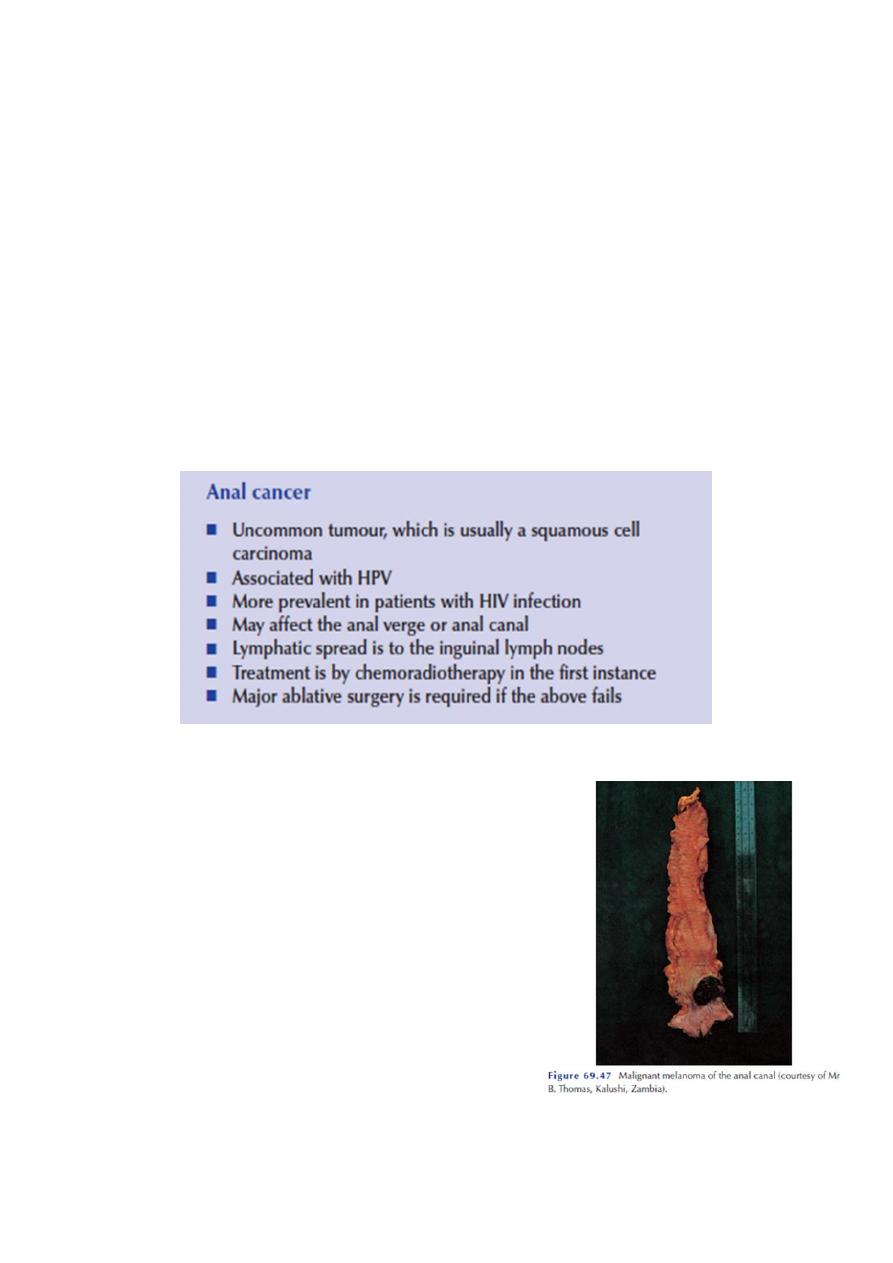
Malignant melanoma :
Melanoma of the anus presents as a bluish-black soft mass that is confused
with a thrombotic pile, and therefore unfortunately incised, Such trauma,
followed by the trauma of defecation, incites the tumour to rapid
metastasis
.
Left undisturbed, it ulcerates and the colour of the tumour changes
from blue to black
.
The inguinal lymph nodes are soon involved
.
Unless a melanoma is excised at an early stage
,
it disseminates by the bloodstream
.
The tumour is radioresistant and has a very poor prognosis
Anal intraepithelial neoplasia (AIN) :
This may rarely affect the anal region and may be part of a more widespread
lymphomatous condition.
Clinical features :
1-Anal cancer can occur at almost any age, but is usually found in the 6th and 7th
decades
.
2-It is a rare condition, accounting for approximately 2 per cent of all colorectal
cancers
.
3-Symptoms include rectal bleeding, mucus discharge, tenesmus, the sensation of
a lump in the anus and a change in bowel habit
4-Occasionally, a patient may present with a mass in the inguinal region due to
metastatic lymph nodes
.
5-Rectal examination may reveal an ulcerating, hard, tender, bleeding mass in the
anal canal or at the anal verge
.
6-The lesion may fungate through the anal canal and appear on the anal skin, or
present through a chronic anal fistula
.
Predisposing conditions :
1-There appears to be a relationship between anal condylomata caused by the
human papilloma virus, particularly type 16, and anal cancer
.
8
2-The disease is more prevalent in patients infected with the human
immunodeficiency virus
.
3-Higher incidence of anal cancer in patients with Crohn’s disease.
TREATMENT :
Historically, early anal margin tumours were treated by local excision and anal
canal tumours by abdominoperineal excision
Carcinoma of anal verge :
Nowadays, primary treatment is by chemoradiotherapy [combined modality
therapy (CMT), the chemotherapy usually including a combination of 5-
fluorouracil (5-FU) with mitomycin C or cisplatin
.
Carcinoma of anal canal :
One of two lines
1-Abdominoperineal resection
Resection of anal canal and rectum with
terminal colostomy
.
2-Chemo-radation
A coarse of combination of chemotherapy
followed by raddation , residual tumour after 4-
6 weeks A-P resection done .
SH.J
