1
Forth stage
Surgery
Lec-4
د.هيثم النجفي
1/1/2014
Rectal Prolapse
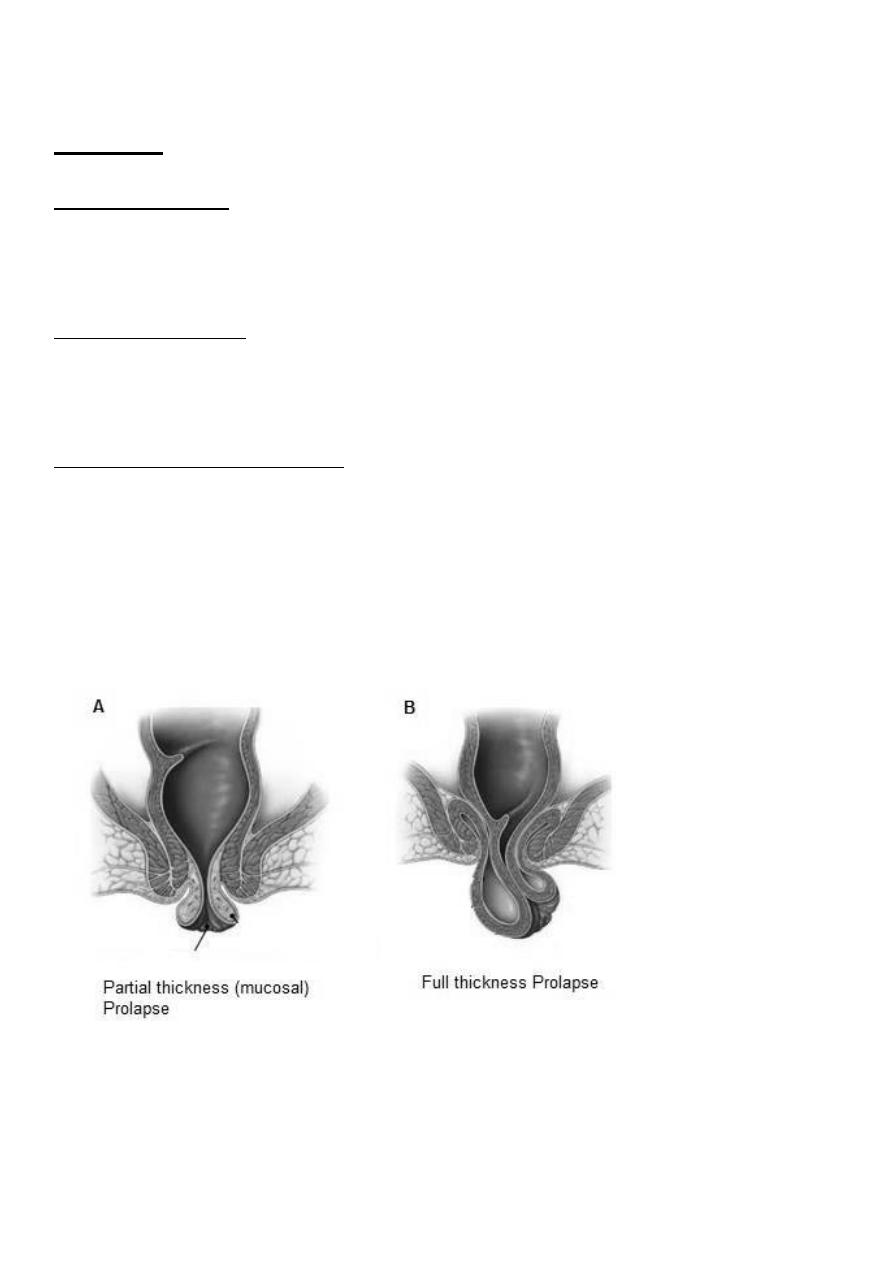
- It may be mucosal or full thickness
- If full thickness, the whole wall of the rectum is included
- It commences as a rectal intussusception
- In children, the prolapse is usually mucosal and should be treated conservatively
- In the adult, the prolapse is often full thickness and is frequently associated with
incontinence
- Surgery is necessary for full-thickness rectal prolapse
- The operation is performed either via the perineum or via the abdomen
Causes
Cause in infants: incomplete development of sacrum (straight sacrum, not curved) as does
the reduced resting anal tone, which offers diminished support to the mucosal lining of the
anal canal.
Cause in children: weight loss, so loss of fat pads in ischiorectal fossa or may be caused by
sever gastroenteritis (an attack of diarrhea)
Cause in adults: The condition in adults is often associated with third-degree haemorrhoids
or hemorrhoidectomy or fistula (over cutting).
Cause in old: both mucosal and full-thickness prolapse are associated with weakness of the
sphincter mechanism (atonicity).
1. Partial (Mucosal) prolapse
The mucous membrane and submucosa of the rectum protrude outside the anus for
approximately 1–3 cm. When the prolapsed mucosa is palpated between the finger and
thumb, it is evident that it is composed of no more than a double layer of mucous membrane
Clinical Picture:
Symptoms:
Something protruding from the anus at defecation:
- Early: it reduces spontaneously.
- Late: it requires manual repositioning.
Mucous discharge.
O/E
In children mucosa of the rectum protrude outside the anal verge either circular or lunar
and not more than 1-3 cm.
2
In old anus is patulous (not like anal fissure which is tight), and when ask the patient to
squeeze it will protrude out.
Treatment
In infants
Digital repositioning
:
Tissue paper around the finger, then introduce your finger to the anal
canal, stick it on the mucosa, pull ur finger and leave the tissue paper inside. The parents
should be taught.
In children
Submucousal injection of 5% phenol in almond oil under general anesthesia, with protoscope
guide, As a result of the aseptic inflammation following these injections, the mucous
membrane becomes tethered to the muscle coat.
In adults
Excision of the prolapsed mucosa: When the prolapse is unilateral, the redundant mucosa can
be excised or, if circumferential, an endoluminal stapling technique can be used.
Thiersch operation. This procedure, which aimed to place a steel wire or, more commonly,
a silastic or nylon suture around the anal canal, just like circlage but on the anus. Also causes
inflammation lead to fibrosis.
If this didn’t work, the retrorectal space is entered, parasagittal incision are made, and the
rectum is sutured to the sacrum and support levator ani muscle.
2. Complete (Full thickness) Prolapse: procidentia
The protrusion consists of all layers of the rectal wall. On palpation between the finger and
thumb, the prolapse feels much thicker than a mucosal prolapse, and obviously consists of a
double thickness of the entire wall of the rectum. Any prolapse over 5 cm in length consider
as full thickness prolapse.
3
Differential Diagnosis
Intussusception of rectum on itself or sliding hernia.
Prolapse of the rectum must be distinguished from ileocaecal intussusception. In ileocecal
intussusception there is a deep groove (5 cm or more) between the emerging protruding mass
and the margin of the anus, into which the finger can be placed, while in prolapse there is no
groove so finger can’t be placed.
Clinical Picture
The patient usually presented - either partial or complete – with incontinence, pain not very
much common, so as bleeding unless there is complication (ulceration of the mucosa).
N.B. Sigmoidoscopy or barium enema are done: to exclude polyps, masses or any underlying
cause, especially in old age patients.
Treatment
Surgery is required, and the operation can be performed via the perineal or the abdominal
approaches.
1- Transperineal approach
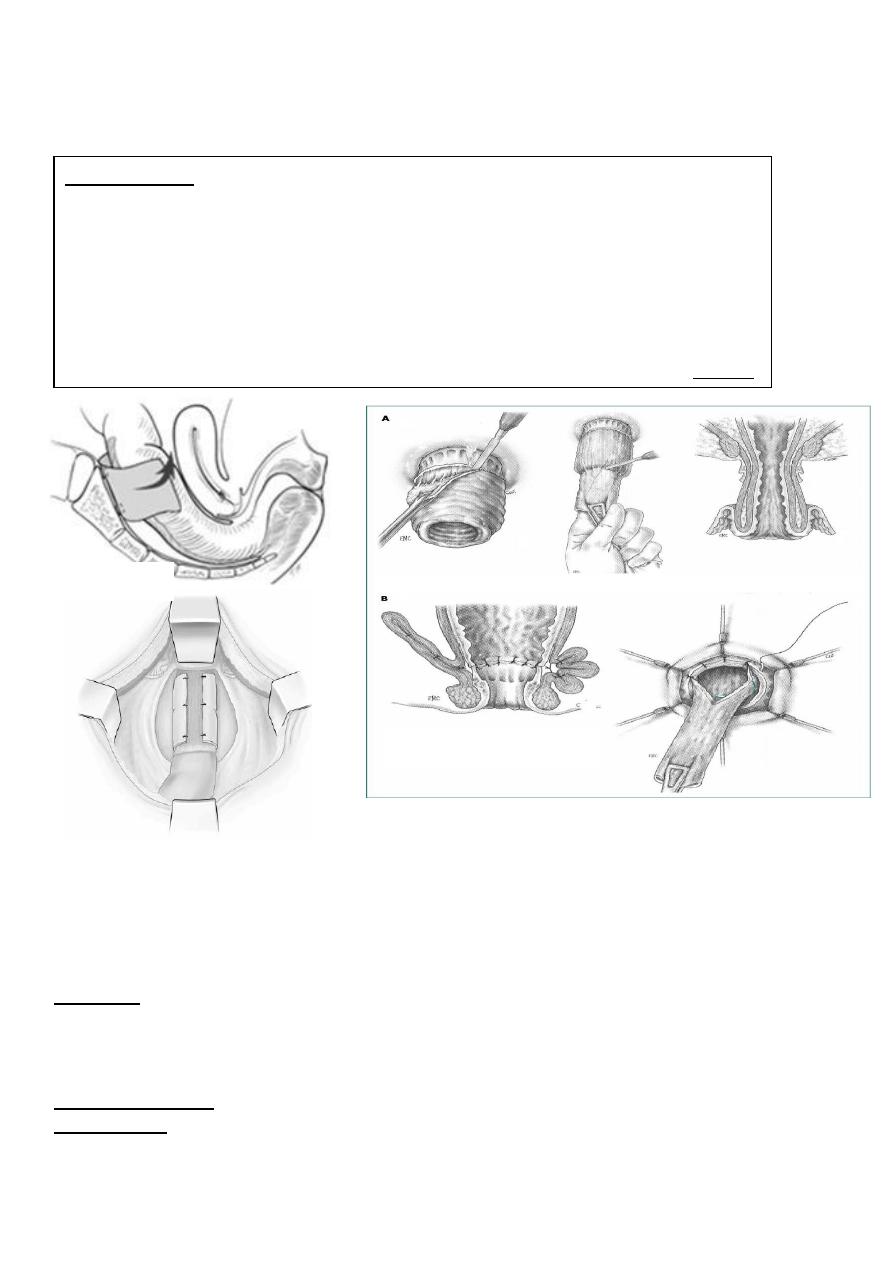
Delorme’s operation. In this procedure, the rectal mucosa is removed circumferentially
from the prolapsed rectum over its length. The underlying muscle is then plicated with a
series of sutures, so that, when these are tied, the rectal muscle is concertinaed towards
the anal canal. The anal canal mucosa is then sutured circumferentially to the rectal
mucosa remaining at the tip of the prolapse. The prolapse is removed (and
incontinence), and a ring of muscle is created above the anal canal, which prevents
recurrence.
Altemeier’s procedure. This consists of excision of the prolapsed rectum and
associated sigmoid colon from below, and construction of a coloanal anastomosis.
2- Transabdominal approach
Well’s operation: midline suprapubic incision is made, then open the pelvic floor
around the rectum by dissection. A sponge like piece called polyvinyl alcohol sponge
(PVA) curled around the rectum posteriorly in 270˚ degree then sutured on the
periostum of the sacrum, so the rectum is fixed on the sacrum by the sponge, after all,
pelvic floor should be sutured very tightly. Dissolving of PVA can cause adhesion and
intestinal obstruction. In this operation 100% there is no recurrence.
Ripstein operation: abdominal incision is made and pull the rectum as much as can.
Transfixation of the rectum to the junction of sacrum with 5
th
lumbar vertebra
(promontory of the sacrum) by taking a partial thickness in the rectum then a tape
(Teflon sling) on spatulated needle (wide point surgical needle) inserted strongly on the
periosteum of the sacrum at promontory of the sacrum. This restores and maintains the
normal posterior curve of the rectum and prevents intussusception with subsequent
prolapse.
4
Lahoot operation: Exteriorization of whole colon and suturing the rectum on rectus
muscle then suturing the anterior abdominal wall above it. This may lead to intestinal
obstruction.
Solitary Rectal ulcer
It an ulcer on the anterior wall of the rectum. In this form, it can be mistaken for a rectal
carcinoma or inflammatory bowel disease, particularly Crohn’s disease.
Etiology
Proctographic studies indicate that it is due to internal intussusception of rectum on itself or
anterior rectal wall prolapse through the pelvic diaphragm or may be due to homosexuality.
Clinical Picture
Presentation
Mainly bleeding per rectum, and if infected the patient may present with purulent discharge
and pain.
sacrum using four to six
the mobilized rectum to the
Suturing
External N.B:
interrupted non-absorbable sutures – called ‘sutured rectopexy’. Recently, the
technique has been performed laparoscopically, as an abdominal rectopexy may
lead to severe constipation, some surgeons recommend combining this procedure
with resection of the sigmoid colon, so-called ‘resection rectopexy’. Recently, an
anterior mesh rectopexy has gained favor. In this procedure, a piece of mesh is
fixed to the upper sacrum. The plane between the rectum and vagina is dissected,
)
Read it
rectum. (
ed into it and sutured to the
plac
and the mesh
Delorme’s operation
Well’s operation
5
O/E
- Ulcer or nodular mass (just like carcinoma).
- Biopsy show non-significant inflammatory cells and fibrin tissue.
Treatment
- Very difficult often insufficient
- Anti-inflammatory
hydrocortisone
- Cautery
- Per anal submucosal resection (it will recur)
- Multiple cautery
- Laparotomy and excision
N.B: after healing, the ulcer becomes nodule-like which will breakdown to form ulcer again.
Neoplasm of the rectum:
Premalignant agents
- Post cholecystectomy because of undigested fat or because of high concentration of
sodium taurocholtae and sodium glycocholate, so cancer of the rectum is common in
such a patient.
- Meat especially beef meat
- Smoked fish causes mainly ca of the stomach and secondary rectum and anus
- HIV, Parvovirus, homosexual
Premalignant conditions
Prognostic index of polyp’s malignant change
- Size > 2cm
- Sessile (attached to the mucosa without pedicles)
- Multiple
- Family history
- Shape ( angry looking, indurated base, fragile, or cauliflower)
1-
Juvenile solitary polyp
- Bright-red glistening pedunculated with long pedicle, grape-like polyp (‘cherry
tumour’).
- Found in infants and children 2-3 years.
- Protrude outside the anus after defecation, it is 2-3 cm in size.
- May be presented as pain and bleeding due to congestion.
- Never cut without general anesthesia
- Transfixation, ligation and cutting.
- It is not premalignant,
6
- But if it is hereditary (autosomal dominant) it is premalignant and need repeated
investigation by endoscope and resection
2- Villous polyp (adenoma)
- These have a characteristic Frond-like appearance.
- This may be very large and partial or complete circumference of rectum is covered,
sometimes it causes occlusion.
- It is premalignant.
Presentation
Mucous diarrhea rich in potassium, sometimes bleeding, and hypokalemia due to long term
loss of potassium.
O/E
PR reveal fragile mass, if hard mass is felt this mean malignant infiltration.
Investigation
Endoscopy and scan biopsy (the area we suspect).
Treatment
If benign
endoscopic spatulation and cautery.
If malignant
resection
- Above 7 cm in size
sphincter saving operation.
- Below 7 cm in size
rectoanal using stapler or abdominoperineal approach.
3- Familial adenomatous polyposis
- Autosomal dominant.
- Multiple polyps of variable size from sigmoid to rectum.
- Sessile and pedunculated.
Presentation
Diarrhea, weight loss, bleeding, and positive family history.
Diagnosis
Endoscopy, sgmoidscopy, and colonoscopy to exclude cancer.
Treatment
Treatment of choice is colonectomy and iliorectal anastomosis.
4- Pseudo polyp (inflammatory polyp)
It occurs in ulcerative colitis, bacillary dysentery or amoebic dysentery, there will be patches
of ulceration due to lysis of mucosa, and the area of mucosa in between these ulcers, will
suffer inflammation, induration, hypertrophy, and hyperplasia. It is premalignant
7
Investigation
General stool exam and endoscopy.
Treatment
Treat the underlying cause
N.B: other polyps like hemangioma, lymphoma and dysplastic are not premalignant.
Single polyp: (
Write short notes on the treatment of single polyp?)
It must be removed by snaring then cautery (hot biopsy), never fulgurated so on to send for
histopathology. If the histopathology results indicate malignancy:
If malignant in the head with free stalk
If both malignant but base of stalk is free
Snaring
