1
Fifth stage
Surgery-Ortho
Lec-5
د. يقضان
29/11/2015
CHRONIC OSTEOMYELITIS
Introduction
It could be the sequels of acute osteomyelitis , but more common it follows an open
fracture or infected operation .
The usual organism is usually staph. aureus ,E.coli , strepto.pyogen , proteus and
psudomonas ; with time the infection become mixed .
In the presence of foreign implant, staph. Epidermidis is the commonest .
pathology
Bone destroyed and devitalized at the focus area of infection or more diffusely along the
surface area of the foreign implant .
Cavities containing sequestrum and pus surrounded by vascular tissue (granulation tissue)
and beyond it there is area of sclerosis due to chronic reactive bone formation .
The sequestrum act as foreign body so the bacteria will adhere to it and the infection will
persist until it removed .
Sinus may stop it’s discharge for weeks or even months giving the appearance of healing ,
but it recur again , so the condition will be as ON and OFF .
Bone destruction and brittle sclerosed bone may lead to pathological fracture .
Clinical feature
Pain , pyrexia, redness, tenderness and discharging sinus represent a flare up of the
condition ; it take a time and then subside to recur again later on .
So there is periods of flare up and remission and so on .
In long standing cases the skin and tissue is thickened and adhere to the bone .
Deformity of the bone , pathological fracture and non union of the fracture when
complicated with the chronic osteomyelitis are the complication of this disease
2
Imaging :
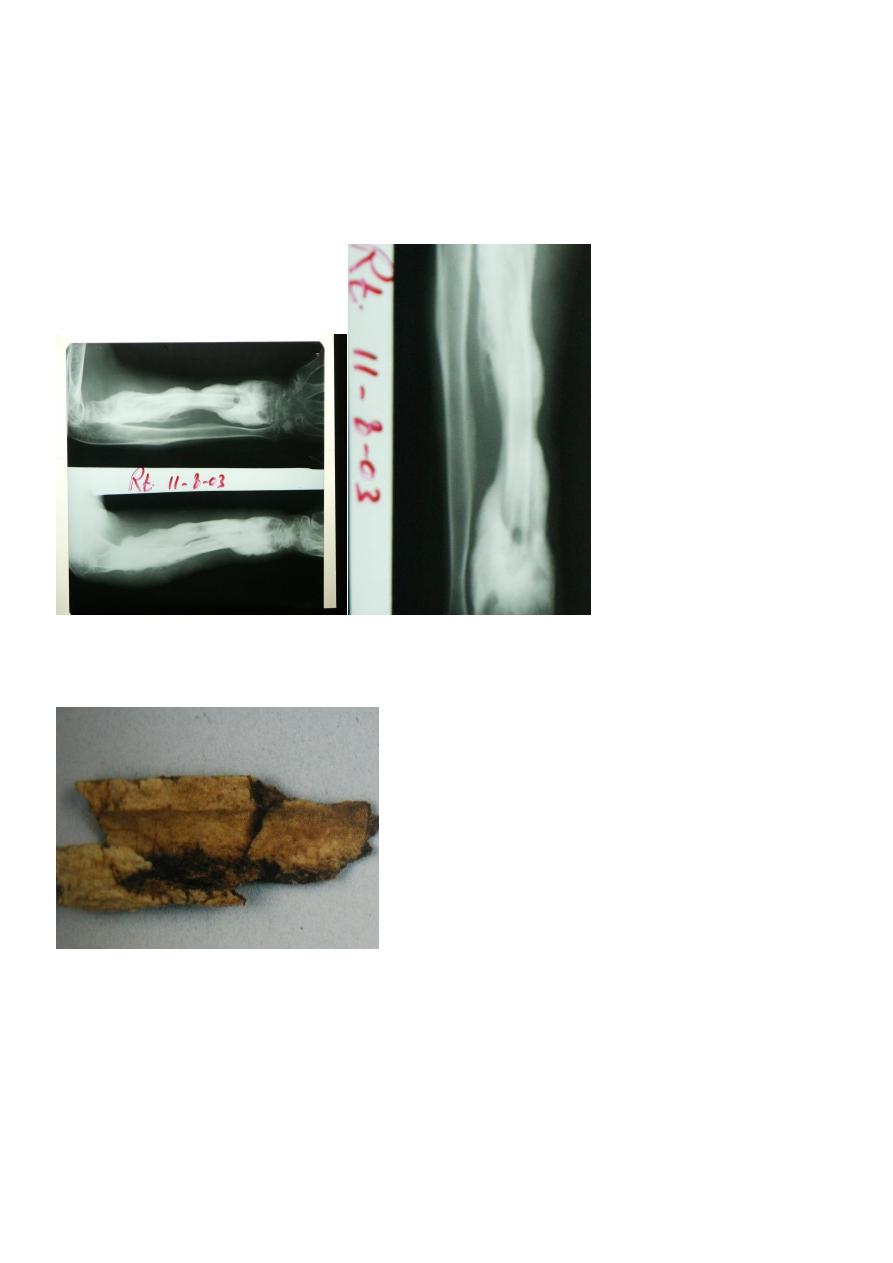
X-ray (plain) show areas of bone resorption either as patchy loss of density or as frank
excavation with thickening and sclerosis of the bone around it .
Sequestrum appear as unusual dense fragments in contrast to the vascularized bone .
Sinogram : may help to localized the site of infection
Ch.osteo.(bone sequestrum)
Bone sequestrum
Radio-isotope scan(bone scan):
It is sensitive but not specific Tc99,Ga67,In111 , all show increase density in both perfusion
and bone phase .
C.T and MRI are also helpful .
Other invest. :ESR , wbc count both are increased .
3
Treatment
Antibiotics : bactericidal drugs should be used , and it is chosed according to culture and
sensitivity ; the drug should also be capable to penetrate the sclerosed bone ;e.g. fucidic
acid , cephalosporin and clindamycin .
Local treatment :
By dressing the sinus and use the colostomy cream for the skin excoriation ; acute abscess
should be drained .
Operative treatment :
Under antibiotic cover all necrotic tissue and sequestrum should be removed .
Dead tissue can be identified by preoperative injection of sulphan blue which stain the
living tissue green leaving the dead tissue unstained .
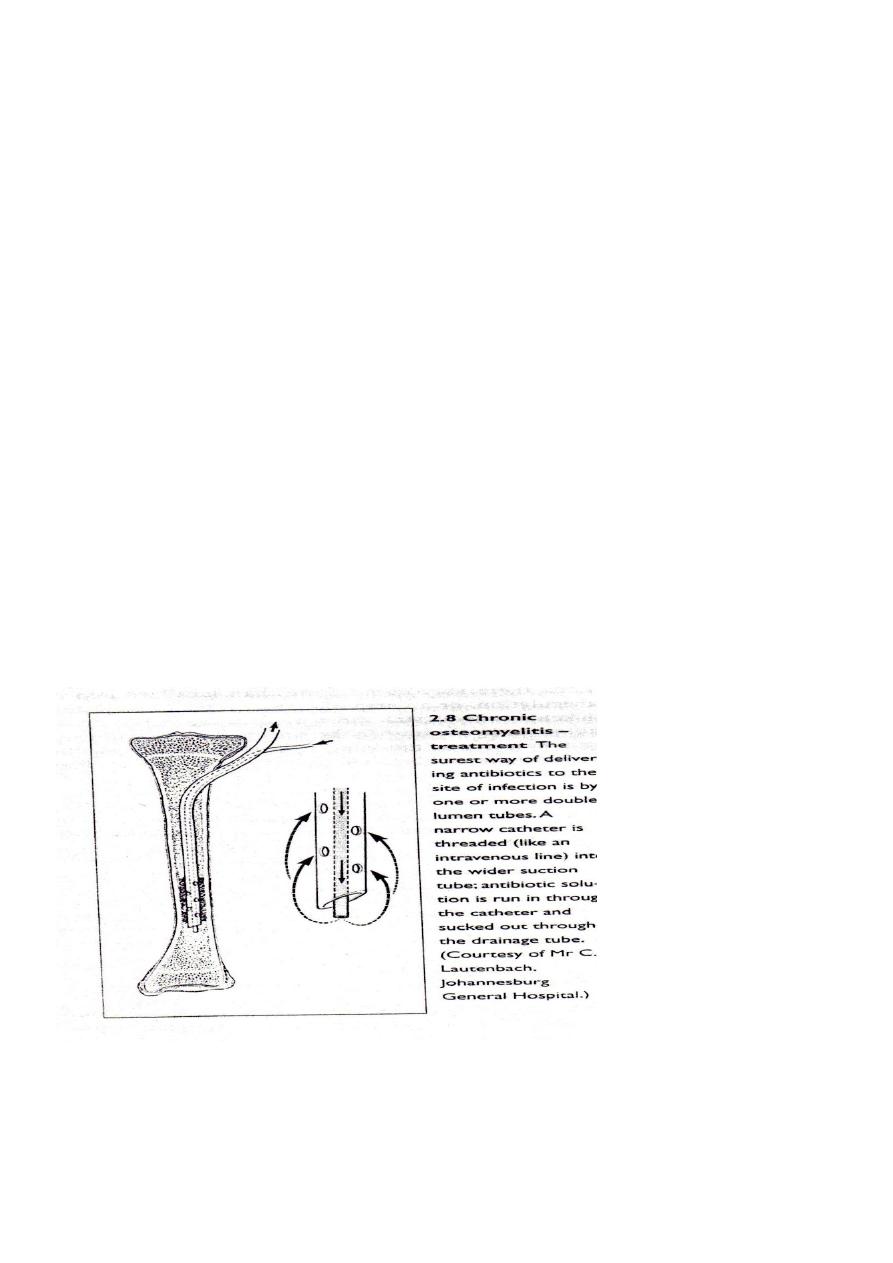
Double lumen catheter :
Can be used for injection of antibiotic for 4 hours then aspirated to reinject other dose , and
so on , continue for 2-3 weeks .
Antibiotics inform of beads also can be used .
Other way of preventing recurrence is by filling the space inside the bone which is
developed from removal of the necrotic tissue by living or potentially living material like
flap of muscle or cancellous bone graft (papinean technique)
Acute pyogenic arthritis
The way of infection can be :
a – direct invasion .

4
B – direct spread of infection from bone abscess .
C – by blood stream from distant site .
The commonest M.O. is staph. Aureus , in infants H. inflauanzae , streptococcus, E.coli ,
proteus .
Pathology
Infection started in the synovium ,lead to acute inflammatory reaction, lead to exudate and
pus formation ; the pus then invade the articular cartilage and destroy it by bacterial
enzymes and synonvial enzymes .
In infants the epiphysis is destroyed .
The pus may spread to the bone or open as sinus .
Prognosis
With healing there may be :
A – complete resolution and return to normal
B – partial loss of articular cartilage lead to fibrosis of the joint .
C – complete loss of articular cartilage lead to bony ankylosis (bony fusion of the joint) .
D – bone destruction and deformity .
Clinically
According to the age :
In infant : the condition appear as septicemia rather than joint pain; baby irritable , refuse
feeding , fever may present or not .
The joint should be examined for local sign of infection ; umbilical vein should be examined
for infection .
In children :
The usual feature is acute pain in single large joint , the child refuse to move the joint .
The child look ill , tired , swinging fever ;in addition to the local signs of infection .
All movements are restricted or completely abolished .
In adult :
We should think for gonococcal infection ,or
Drug abuse .
Patient with rheumatoid arthritis especially

5
With corticosteroid treatment may develop silent infection .
Investigation
Imaging :
In early stage the x-ray look normal , apart from increase joint space .
In late stage the x-ray show joint destruction.
Ultrasound and MRI show joint effusion .
Blood invest. :
Increase WBC count , increase ESR, blood culture may be +ve .
Aspiration from the joint and immediate ex. By gram stain : in normal synovial fluid ,cell
count about 300 cell / ml ; 10000 cell / ml in non infective inflammatory disorders ;
50000 cell / ml is highly suggestive of infection .
The aspirated fluid can be send for culture and sensitivity .
Differential diagnosis
1- acute osteomyelitis .
2- traumatic synovitis .
3- irritable joint (pt. has pain , stiffness but he is not ill, no sign of infection) .
4- haemophilic bleed .
5- rheumatic fever (pain migrating) .
6-gout and pseudo gout (crystals) .
Treatment
It should be started immediately after the diagnosis has been settled as acute osteomyelitis
.
1 – general supportive care (analgesic and i.v. fluid) .
2 – splinting the limb by p.o.p. or skin traction .
3 – antibiotic :older children give anti staph. for 2-7 days i.v. then orally for 3 weeks . in
children below 4 years give cephalosporin.
4 – drainage under G.A. by open incision , wash the joint by normal saline and then do
antibiotic irrigation for 2-3 days ; arthroscopic drainage and irrigation now is possible .
