
1
Fifth stage
Surgery-Ortho
Lec-1
د
.
ه
ش
ا
م
القطان
8/3/2016
The Hip
CLINICAL ASSESSMENT OF THE HIP
History
Pain arising in the hip joint is felt in the groin, down the front of the thigh and,
sometimes, in the knee; occasionally knee pain is the only symptom.
Pain at the back of the hip is seldom from the joint: it usually derives from the lumbar
spine.
Stiffness may cause difficulty with putting on socks sitting in a low chair.
Limp is common, and sometimes the patient complains that the leg is 'getting
shorter'.
Walking distance may be curtailed or, reluctantly. the patient starts using a walking
stick.
CLINICAL EXAMINATION
*SIGNS WITH THE PATIENT UPRIGHT
The gait is noted.
o Antalgic gait.
o Shortening (short-leg limp).
o Abductor weakness (Trendelenburg Lurch).
The Trendelenburg test
The patient is asked to stand, unassisted, on each leg in turn; while standing on one
leg, he or she has to lift the other leg by bending the knee
Normally
the weight-bearing hip is held stable by the abductors and the pelvis rises on the
unsupported side.
if the hip is unstable, or very painful, the pelvis drops on the unsupported side.

2
A positive Trendelenburg test is found in:
Dislocation or subluxation of the hip.
Weakness of the abductors.
Shortening of the femoral neck.
Painful disorder of the hip.
*SIGNS WITH THE PATIENT LYING SUPINE
Look
if one leg seems to be shorter than the other.
Look for scars or sinuses, swelling or wasting and any obvious deformity or
malposition of one of the limbs.
(In babies) Asymmetry of skin creases may be important.
Feel
Bone Contour are felt when leveling the pelvis and judging the height of the greater
trochanters.
Move
The assessment of hip movements is difficult because any limitation can easily be
obscured by movement of the pelvis.
Hip Range of Motion:
1. FLEXION
2. EXTENSION
3. Internal Rotation
4. External Rotation
5. Adduction
6. Abduction
7. Abduction

3
*SIGNS WITH THE PATIENT LYING PRONE
THE DIAGNOSTIC CALENDAR
Hip disorders are characteristically seen in certain well-defined age groups.
Age of onset
Age years
birth
10-20
0-5
5-10
Adults
Historical review FOR DDH
Dupuytren – Paris (1800’s)
Dissected DDH specimens. he did not think condition could be treated.
Paletta – Milan – 1820
First anatomic description of congenitally dislocated hip(15 day old boy –Bilateral
DDH).
Diagnosing DDH Early
La Damanay –Rennes – 1908.
Ortolani – Italy –1937.
Normal Growth and Development
Embryologically the acetabulum, femoral head develop from the same primitive
mesenchymal cells cleft develops in precartilaginous cells at 7th week and this
defines both structures 11wk hip joint fully formed.
femoral head deeply seated in acetabulum by surface tension of synovial fluid and
very difficult to dislocate.
in DDH this shape and tension is abnormal in addition to capsular laxity.
Probable diagnosis
Developmental dysplasia.
Infections.
Perthes' disease.
Slipped epiphysis.
Arthritis.

4
The condition formerly known as congenital dislocation of the hip and now called
developmental dysplasia of the hip (DDH).WHY?
DDH Comprises a spectrum of disorders:
Frank dislocation during the neonatal period; Subluxation (partial displacement)
o Shallow acetabulum (acetabular dysplasia) without actual displacement.
o dislocatable.
o dislocation.
Incidence of neonatal hip
instability is 5-20 per 1000 live births.
o however, most of these hips stabilize spontaneously.
Re-examination 3 weeks after birth the incidence of instability is only 1 or 2 per 1000
infants.
Girls are much more commonly affected than boys, The ratio being about 7: l.
The left hip is more often affected than the right.
in 1 in 5 cases the condition is bilateral
Risk Factors
80% Female
First born children
Family history: 6% one affected child, 12% one affected parent, 36% one child + one
parent
Oligohydramnios.
Breech (sustained hamstring forces).
Swaddling cultures.
Left 60% (left occiput ant),
o Right 20%.
o both 20%
foot deformity
5
Aetiology and pathogenesis
Genetic factors
must be important, for DDH tends to run in families and even in entire populations
(e. g, along the northern.
Hormonal changes
in late pregnancy may aggravate ligamentous laxity in the infant.
Intrauterine malposition
especially a breech position with extended legs, would favor dislocation.
Postnatal factors
play a particular in maintaining any tendency to instability.
Clinical features
The ideal, still unrealized, is to diagnose every case at birth.
When there is a family history of congenital dislocation, and with breech
presentations (presence of risk factors).
For this reason, every newborn child should be examined for signs of hip instability.
*Neonatal diagnosis
There are several ways of testing for instability.
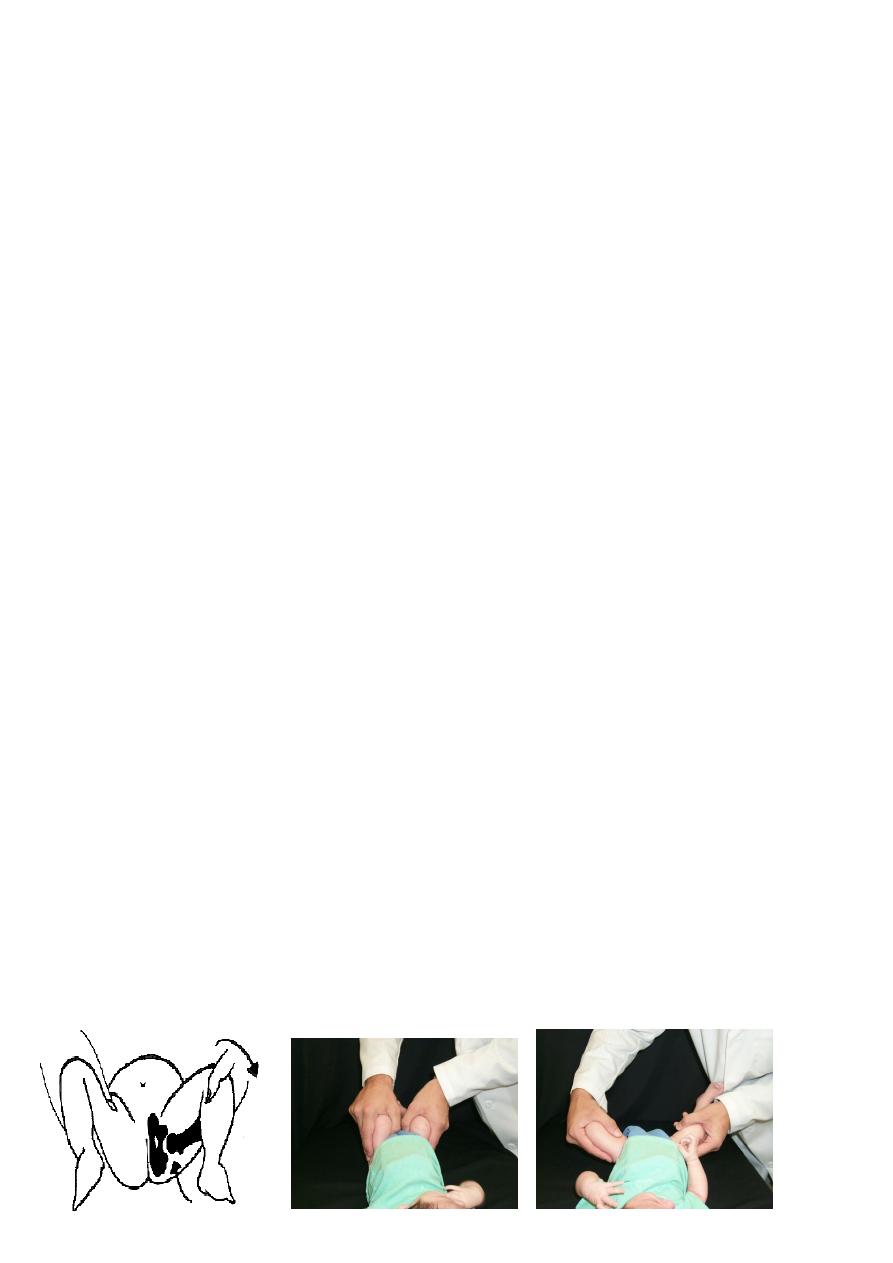
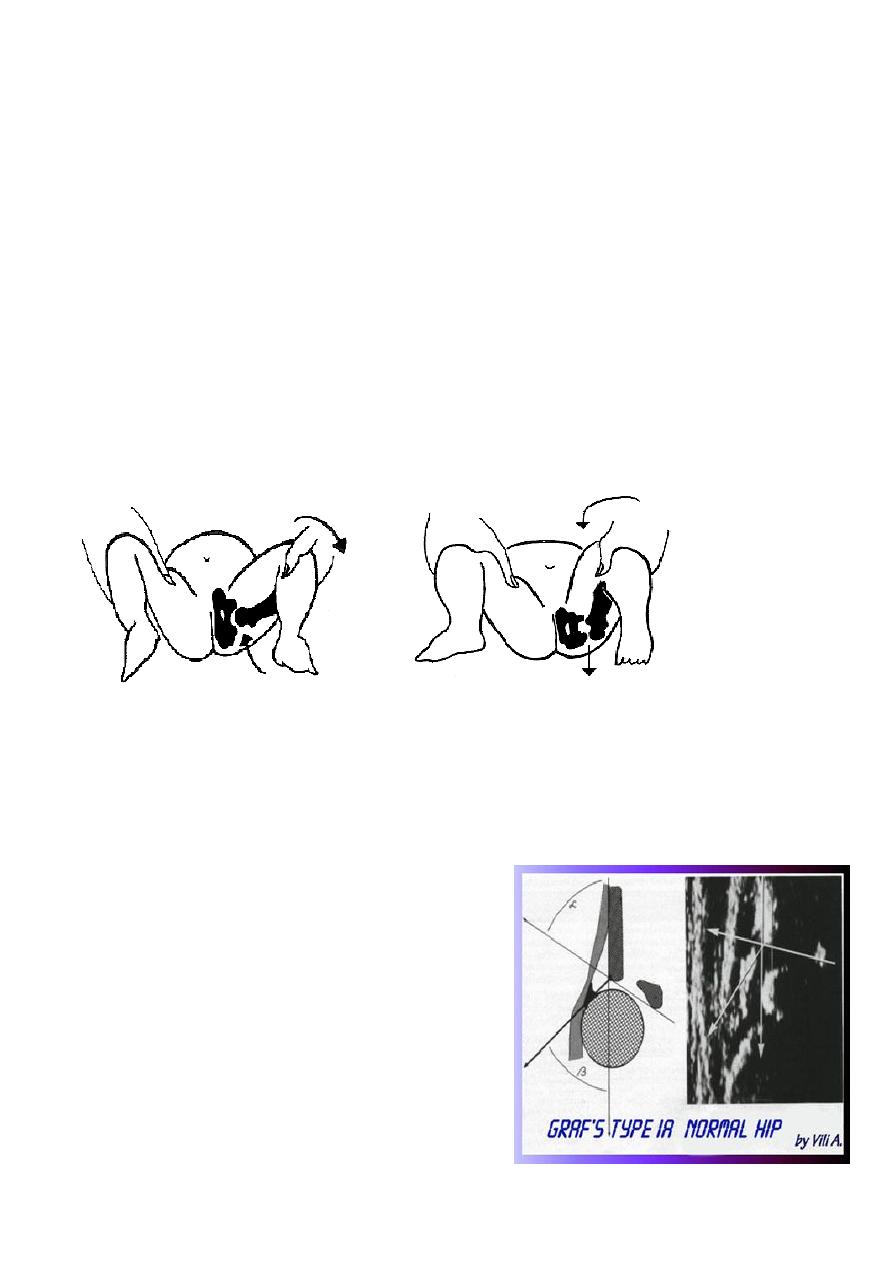
1-Ortolani’s test
the baby's thighs are held with the thumbs medially and the fingers resting on the
greater trochanters;
the hips are flexed to 90 degrees and gently abducted.
Normally there is smooth abduction to almost 90 degrees.
6
2-Barlow's test
In DDH the movement is usually impeded, but if pressure is applied to the greater
trochanter .there is a soft 'clunk' as the dislocation reduces, and then the hip abducts
fully (the 'jerk of entry').
3-Barlow’s Provocative test
Performed in a similar manner but here the examiner's thumb is placed in the groin and,
by grasping the upper thigh, an attempt is made to lever the femoral head in and out of
the acetabulum during abduction and adduction.
If the femoral head normally in the reduced position, can be made to slip out of the
socket and back in again.
the hip is classed as 'dislocatable' (i.e. unstable).
Investigations
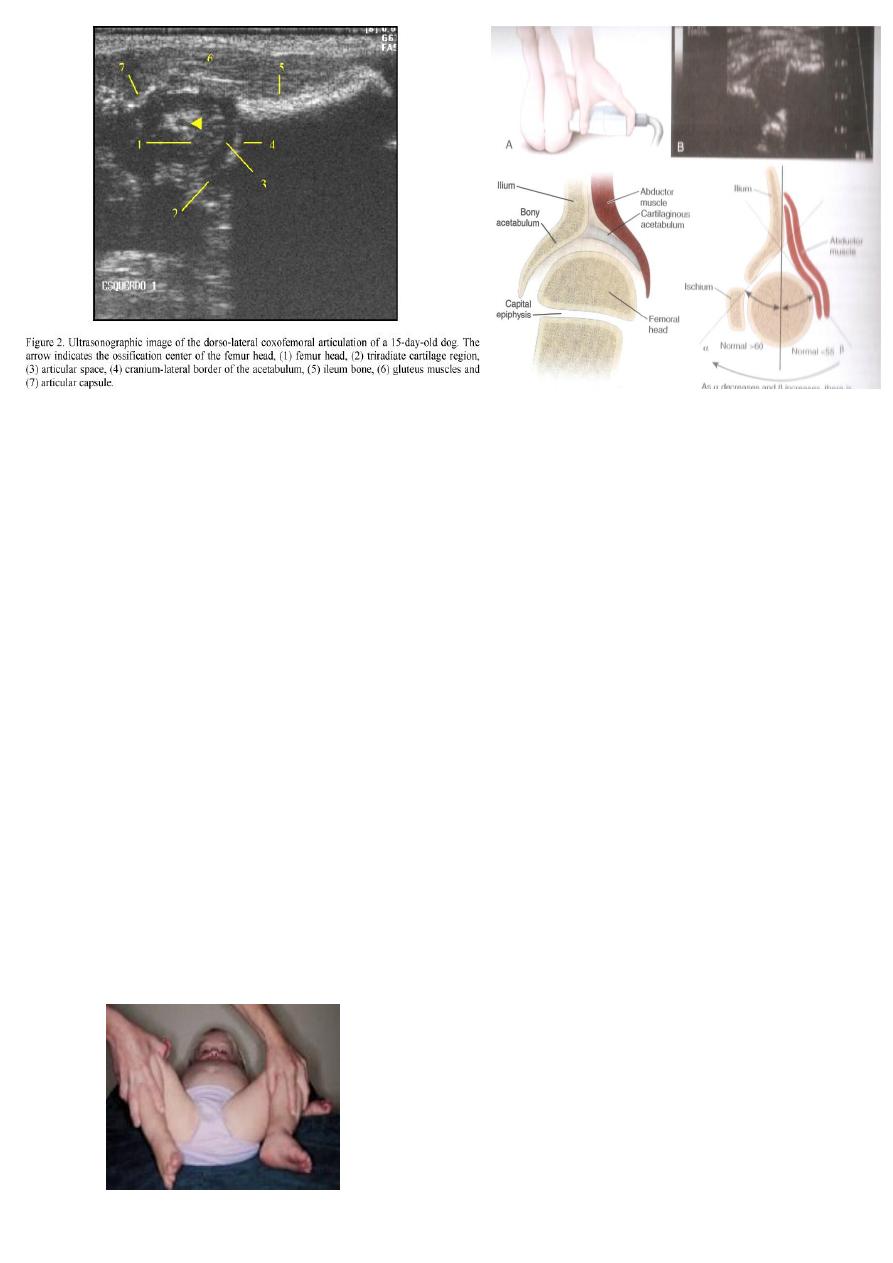
*in early infancy
Every hip with signs of instability – however
slight - should be examined by
ultrasonography.
This provides a dynamic assessment of the
shape of the cartilaginous socket and the
position of the femoral head
7
Late features
Ideally, all children should be examined again at
o 6 months.
o 12 months .
o and 18 months of age, so as to be sure that late-appearing signs of DDH are
not missed.
With unilateral dislocation are asymmetrical creases.
the hip does not abduct fully .
the leg is slightly short and rotated internally.
Bilateral dislocation is more difficult to detect because there is no asymmetry and the
characteristic waddling gait may be mistaken .
Perineal gap is abnormally wide and abduction is limited.
hyperlordosis in bilateral cases
Galleazi sign flex both hips and one side shows apparent femoral shortening
8
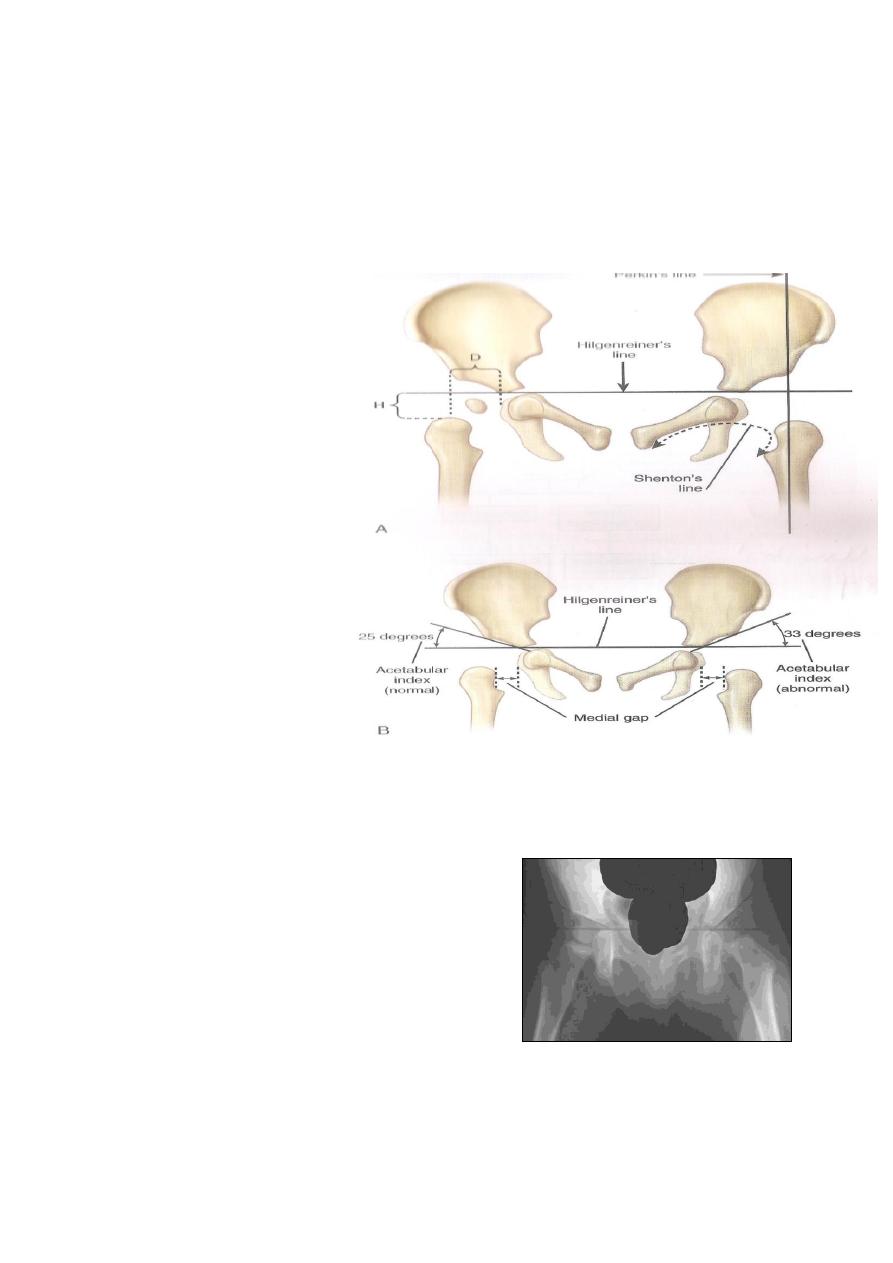
**Investigations in late DDH For diagnosis
X-ray examination is helpful in older children.
The ossific centre of the femoral head is underdeveloped, and from its position it
may be apparent that the head is displaced upwards and outwards
Plain Radiographs
Hilgengreiner’s line is
across the triradiate
cartilage.
Perkins line is vertical
along the lateral border of
the acetabulum.
Shenton’s line.
Acetabular index is the
angle between the
acetabulum and
hilgenreiner’s line
It should be less than 30
degrees in a newborn
The Limping Child: Age 1 – 3 DDH
X-ray findings
Delayed appearance of ossific nucleus
Small ossific nucleus
Dysplastic acetabulum
Proximal displacement of femur

9
TREATMENT
*Treatment under 6 months of age
The simplest and safest policy is to regard all infants with a positive Ortolanis or
Barlow test as DDH .
SO
Nurse them in double napkins.
or with an abduction pillow between the legs for the first 6 weeks.
those with persistent instability are treated by more formal abduction splintage until
the hip is stable. and x-ray shows that the Acetabular roof is developing satisfactorily
(usually 3-6 months).
Splintage
Arnold Pavlik 1902-1962
Pavlik’s Father – Harness Maker
Pavlik and his Harness
1946 –Pavlik introduces his leather harness : Czech Ortho Society, Prague
Modern Day Pavlik –San Diego
*Treatment of persistent dislocation; 6 months to 6 years
If, after early treatment, the hip is still incompletely reduced,
or if the child presents late with a 'missed' dislocation,
the hip must be reduced and held reduced until acetabular development is
satisfactory this done by
Closed reduction
Manipulation under anaesthesia carries a high risk of femoral head necrosis.
To minimize this risk.
reduction must be gradual traction is applied to both legs, preferably on a vertical
frame, and abduction is gradually increased until, by 3 weeks by gallows traction,
to over come A vascular necrosis Then Splintage
10
If concentrically reduced, the hips (both) are held in a plaster spica at 60 degrees of
flexion, 40 degrees of abduction and 20 degrees of internal rotation.
After 6 weeks, the plaster is replaced by a splint that prevents adduction but allows
movement.
If failed Open reduction
at any stage, concentric reduction has not been achieved by conservative methods.
open operation is needed.
*Treatment after the age of 6 years
For unilateral dislocation
operative reduction is still feasible.
it may be necessary to combine this with corrective osteotomy of the femur or
innominate osteotomy of the pelvis.
With bilateral dislocation
the deformity is symmetrical and therefore less noticeable; Therefore, most surgeons
avoid operation unless pain or deformity is unusually severe.
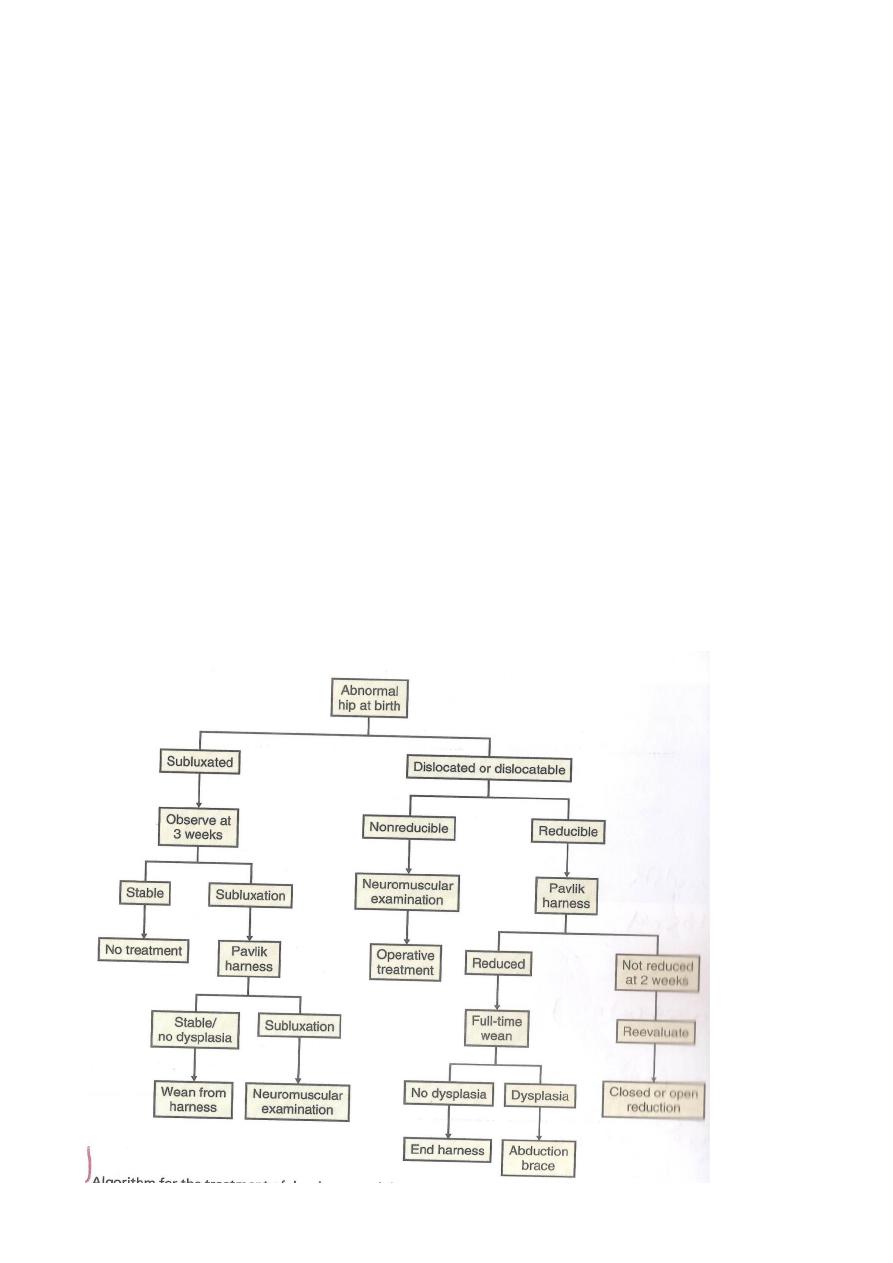
ALGORITHM
FOR
TREATMENT
OF DDH
