1
Fifth stage
Surgery
Lec-2
.د
سيف
1/1/2014
Venous disorders
Deep vein thrombosis:
Etiology: exact cause is unknown but three factors contribute (Virchow's triad):
1- Changes in the vessel wall (endothelial damage)
2- Changes in the blood flow (stasis)
3- Changes in blood composition (hypercoagulation)
Clinical presentation:
1- Asymptomatic
2- Pain, redness, swelling with difficulty in walking
3- Features of pulmonary embolism may be the presenting feature in 30% of the
patients
On examination:
1. Pitting oedema of the ankle,
2. Dilated surface veins,
3. A stiff calf
4. Tenderness.
5. Homans’ sign – resistance (not pain) of the calf muscles to forcible dorsiflexion – is
not absolute and should be abandoned.
6. A low-grade pyrexia may be present
7. Signs of pulmonary embolism or pulmonary hypertension
Investigations:
1) D-dimer measurement: if levels are normal, there is no indication for further
investigations as the possibility of DVT is very remote.
2) Duplex ultrasound: loss of normal vein compressibility with filling defects in the flow
3) Ascending and descending venography; only indicated when surgical intervention is
needed.
Prophylaxis:
Patients who are being admitted for surgery can be graded as low, moderate or high risk.
Low-risk patients are young, with minor illnesses, who are to undergo operations lasting 30
min or less.

2
Moderate-risk patients are those over the age of 40 or those with a debilitating illness or
who are to undergo major surgery.
High-risk patients are those over the age of 40 who have serious accompanying medical
conditions, such as stroke or myocardial infarction, or who are undergoing major surgery
with an additional risk factor such as a past history of venous thromboembolism or known
malignant disease.
Mechanical prophylaxis include:
a. graduated elastic compression stockings
b. external pneumatic compression
c. passive foot movement (foot paddling machine)
d. simple limb elevation
Pharmaceutical prophylaxis:
a. low molecular weight heparin
b. unfractionated heparin
c. warfarin
Patients with low risk need no prophylaxis other than early postoperative mobilization.
Those with moderate risk need either pharmaceutical or mechanical prophylaxis while
those with high risk need both mechanical and pharmaceutical prophylaxis.
Medical treatment:
1) admission to hospital and bed rest
2) anticoagulant therapy (heparin and warfarin)
3) leg elevation
4) elastic compressive bandage from the toes to the upper thigh
5) patients with phlegmasia cerulea dolens need thrombolytic therapy
Surgical Treatment:
A- Venous thrombectomy: only indicated in patients with phlegmasia cerulea dolens
with contraindication to thrombolytic therapy
B- Inferior vena cava filter: indicated in patients with:
1. Recurrent thromboembolism despite adequate anticoagulation
2. Progressing thromboembolism despite adequate anticoagulation
3. Complication of anticoagulants
4. Contraindication to anticoagulants
Pulmonary embolism:
Pulmonary thromboembolism is a significant cause of morbidity and mortality worldwide
.
After an acute, major thromboembolic episode, approximately 15–20% of patients die
within 48 hours. So invasive therapy for acute pulmonary embolism should be considered in
those 15-20% of patients with fatal outcomes.
3
Pathophysiology of pulmonary embolism
The hemodynamic response to a large, sudden pulmonary embolus relates to a variety of
factors,
1. the size of the embolus,
2. the degree of obstruction that it produced in the pulmonary vascular bed,
3. the underlying function of the lung that remains perfused.
In addition to the mechanical factor of pulmonary artery obstruction, there are hormonal
factors that can increase pulmonary vascular resistance (PVR) at the time of acute
pulmonary embolism due to products released from the platelets within the embolus, the
neutrophils and the blood vessel endothelial cells. Thus some patients with a relatively
small embolus may have an exaggerated response to the degree of pulmonary vascular
obstruction.
In patients without preexisting cardiac or pulmonary disease, only when the acute
pulmonary obstruction exceeds 50–60% of the pulmonary vascular bed that cardiac and
pulmonary compensatory mechanisms are overcome and cardiac output begins to fall.
With the sudden pulmonary artery obstruction, right ventricular failure occurs, which is
accompanied by systemic hypotension as the amount of blood reaching the left ventricle
decreases.
Clinical presentation:
Acute pulmonary embolism usually presents suddenly. Symptoms and signs vary with the
extent of blockage, the magnitude of humoral response, and the pre-embolus reserve of
the cardiac and pulmonary systems of the patient. The acute disease is conveniently
stratified into minor, major (submassive), or massive embolism.
For patients with minor pulmonary embolism, physical examination may reveal
tachycardia, rales, low-grade fever, and sometimes a pleural rub. Heart sounds and
systemic blood pressure are often normal. Arterial blood gases are normal. Pulmonary
angiograms typically show less than 30% occlusion of the pulmonary arterial vasculature.
Major pulmonary embolism is associated with dyspnea, tachypnea, dull chest pain,
syncope and some degree of cardiovascular changes manifested by tachycardia, mild to
moderate hypotension, and elevation of central venous pressure. In contrast to massive
pulmonary embolism, patients with major embolism are hemodynamically stable and have
adequate cardiac output. Blood gases reveal moderate hypoxia, and mild hypocarbia.
Echocardiograms may show right ventricular dilatation. Pulmonary angiograms indicate
that 30–50% of the pulmonary vasculature is blocked.
Massive pulmonary embolism is truly life-threatening and is defined as a pulmonary
embolism that causes hemodynamic instability. It is usually associated with occlusion of
more than 50% of the pulmonary vasculature, but may occur with much smaller occlusions,
particularly in patients with preexisting cardiac or pulmonary disease. Patients develop
acute dyspnea, tachypnea, tachycardia, and sweating and may lose consciousness. Both
hypotension and low cardiac output are present. Cardiac arrest may occur. Neck veins are
4
distended, and central venous pressure is elevated. Blood gases show severe hypoxia,
hypocarbia, and acidosis. Urine output falls, and peripheral pulses and perfusion are poor.
Investigations:
1) ECG: tachycardia and nonspecific changes. The major value of the electrocardiogram
is excluding a myocardial infarction.
2) X-ray may show oligemia or linear atelectasis, both of which are nonspecific findings.
3) Ventilation–perfusion (V/Q) scans may provide confirmatory evidence, but these
studies may be unreliable because pneumonia, atelectasis, previous pulmonary
emboli, and other conditions may cause a false positive result. But a negative V/Q
scan exclude the diagnosis of clinically significant pulmonary embolism.
4) Pulmonary angiograms (conventional angiography or CT angiography) provide the
most definitive diagnosis for acute pulmonary embolism as it appears as filling
defects or obstruction of pulmonary arterial branches.
5) Echocardiography both transthoracic or transesophageal may show an embolus
obstructing the main pulmonary artery but will not visualize the lobar pulmonary
arteries
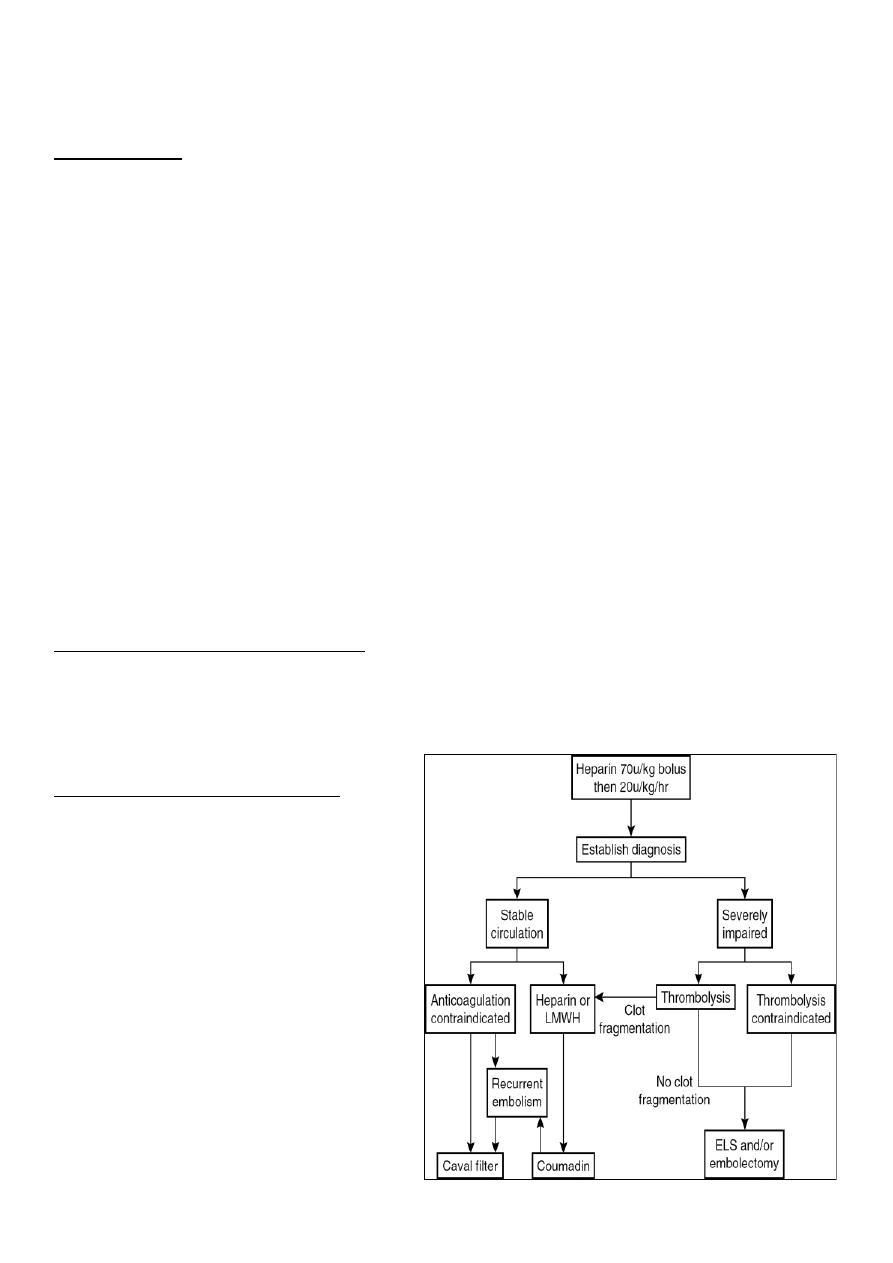
Treatment of pulmonary embolism:
The majority of patients who die of pulmonary embolism do so within 2 hours of the initial
acute event, before the diagnosis can be firmly established, and before effective therapy
can be instituted
.
Conservative medical treatment:
1)
Supplementary O
2
(usually
such patients are already in an
ICU, if not need to
immediately do so)
2)
Patients in respiratory distress
will need mechanical
ventilation
3)
Invasive cardiac monitoring
through both arterial line and
central venous line for
estimation of cardiac output
and serial arterial blood gas
measurement.
5
4)
Pharmaceutical myocardial support
(positive inotropic agents) and sometimes
even mechanical myocardial support (like
intra-aortic balloon pump).
5)
Immediate anticoagulation with i.v. heparin preferably by infusion technique.
6)
Consider thrombolysis in patients with major-to-massive pulmonary embolism. Still,
thrombolytic therapy is contraindicated in patients with fresh surgical wounds,
anemia, recent stroke, peptic ulcer, or bleeding dyscrasias.
Surgical treatment:
Emergency pulmonary embolectomy is indicated for suitable patients with life-threatening
circulatory insufficiency, where the diagnosis of acute pulmonary embolism has been
established.
Indications for acute surgical intervention include the following:
(1)
Critical hemodynamic instability or severe pulmonary compromise
(2)
Patients in whom thrombolytic or anticoagulation therapy is absolutely
contraindicated,
(3)
The presence of a large clot trapped within the right atrium or ventricle
Pulmonary embolectomy is done through a median sternotomy with total anticoagulation, a
cardiopulmonary bypass machine, and mild to moderate hypothermia. The main pulmonary
artery is opened and the embolus with its propagating thrombus removed by forceps,
suction, and embolectomy catheter. After which the patient is weaned off the
cardiopulmonary machine and the chest is closed. Dramatic improvement in his
hemodynamics is noted immediately.
