Deep Vein Thrombosis & Pulmonary Embolism
Deep Vein Thrombosis
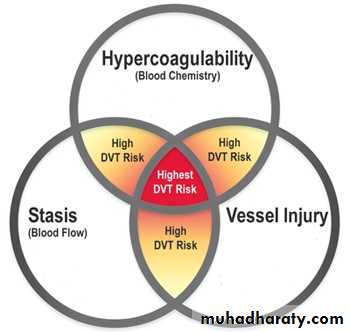
Etiology:According to Virchow’s triad
• Changes in the vessel wall (endothelial damage)
• Changes in the blood flow (stasis)
• Changes in blood composition (hypercoagulation)
Clinical Presentation:
AsymptomaticPain, redness, swelling with difficulty in walking
Features of pulmonary embolism may be the presenting feature in 30% of the patients
On examination:
• Pitting oedema of the ankle,• Dilated surface veins,
• A stiff calf
• Tenderness.
• Homans’ sign
• A low-grade pyrexia may be present
• Signs of pulmonary embolism or pulmonary hypertension
Investigations:
D-dimer measurementDuplex ultrasound
Ascending and descending venographyLow risk: young, with minor illnesses, who are to undergo operations lasting 30 min or less.
Moderate risk: over 40 or with a debilitating illness or are to undergo major surgery.
High risk: over 40 who have serious medical conditions, or undergoing major surgery with an additional risk factor.
Prophylaxis:
Mechanical methods:
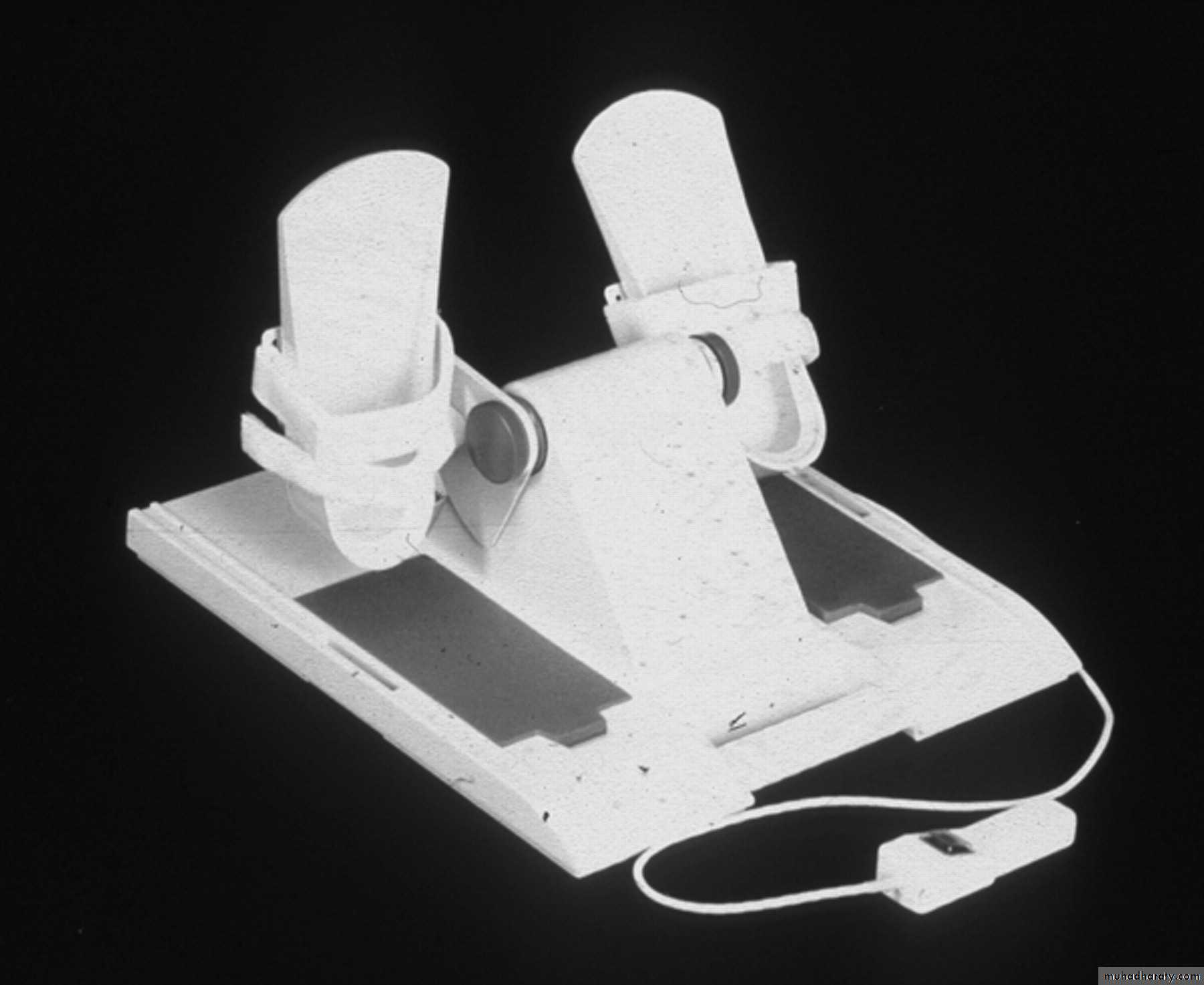
• graduated elastic compression stockings• external pneumatic compression
• passive foot movement (foot paddling machine)
• simple limb elevation
Pharmaceutical methods:
• low molecular weight heparin
• unfractionated heparin
• warfarin
Methods of prophylaxis:
Graduated elastic compressive stocking
External pneumatic compression
Foot Paddling Machine
Treatment:
Medical conservative treatment:Bed rest
Elevation
Bandage
anticoagulation
Thrombolytic therapy (phlegmasia cerulea dolens )
Surgical treatment
Venous thrombectomy
IVC filter
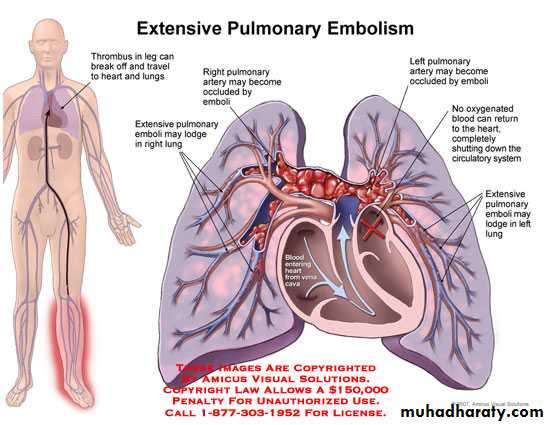
Pulmonary embolism
½ times as common as MI3 times more common than CVA
3rd most common cause of death
Majority are silent
Acute major PE 15-20%
• die within 48 hours
Pathophysiology:
Hemodynamic effect depends on• the size of the embolus,
• the degree of PA obstruction
• the pre-embolus pulmonary function
The degree of PA obstruction depends on
Mechanical obstruction
Hormonal obstruction
50-60% of PA obstructed symptoms
PA obstruction RV failure Cardiac output
Clinical presentation:
Minor Pulmonary Embolism:
Tachycardia, rales, low-grade fever, pleural rub.
Heart sounds and systemic blood pressure are often normal.
ABG are normal.
Pulmonary angiograms: less than 30% occlusion of the pulmonary arterial vasculature
Major (submassive) Pulmonary Embolism:
Dyspnea, tachypnea, dull chest pain, ± syncopeTachycardia, mild to moderate hypotension, and elevation of central venous pressure.
Adequate cardiac output.
ABG: moderate hypoxia, and mild hypocarbia.
Echocardiograms may show right ventricular dilatation.
Pulmonary angiograms indicate that 30–50% of the pulmonary vasculature is blocked
Massive pulmonary embolism:
Dyspnea, tachypnea, sweating ± loss of consciousnessUrine output falls, and peripheral pulses are poor
Tachycardia, hypotension, CVP with distended neck veins
Low cardiac output and cardiac arrest may occur
ABG: severe hypoxia, hypocarbia, and acidosis
Echo.; Dilated RV and RV failure
Pulmonary angiography: more than 50% occlusion of pulmonary vasculature
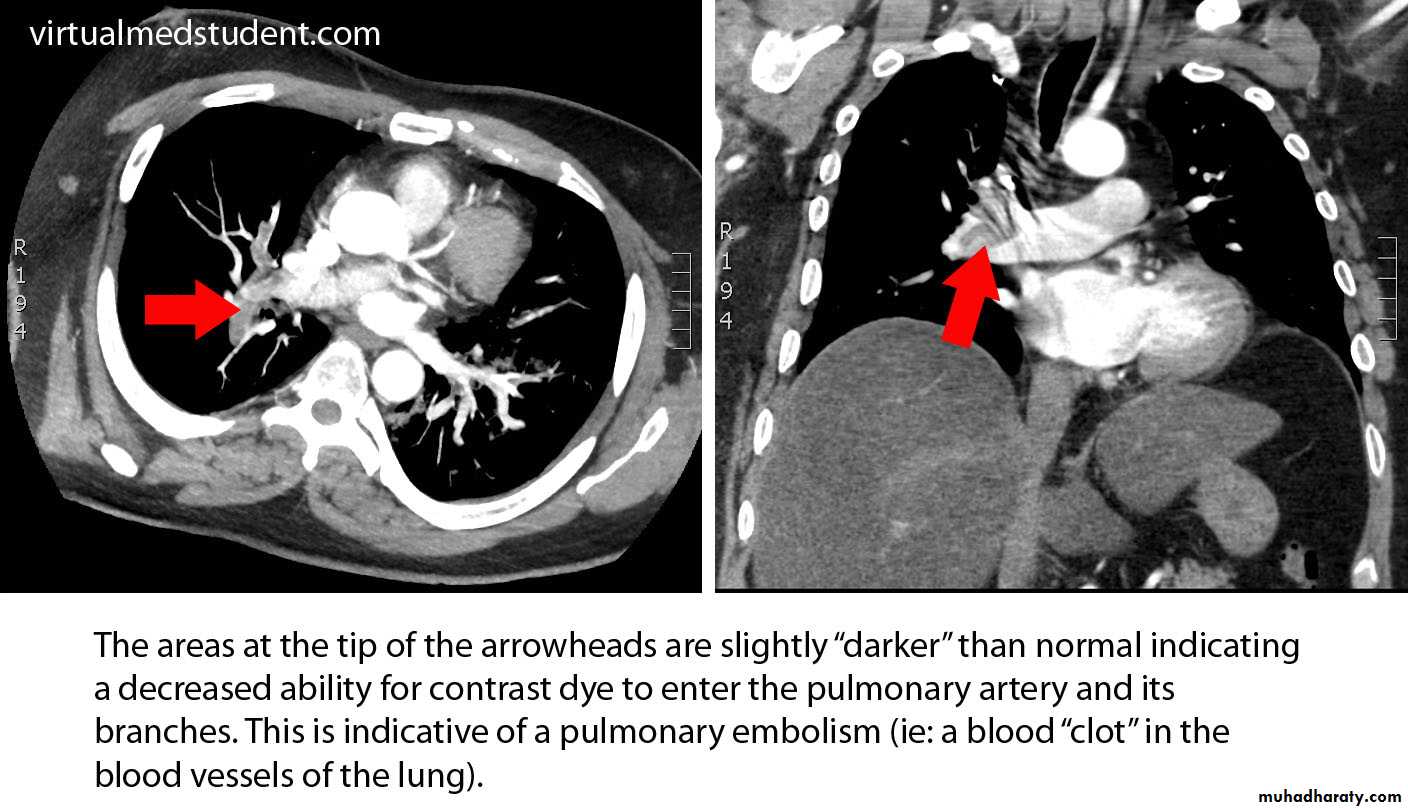
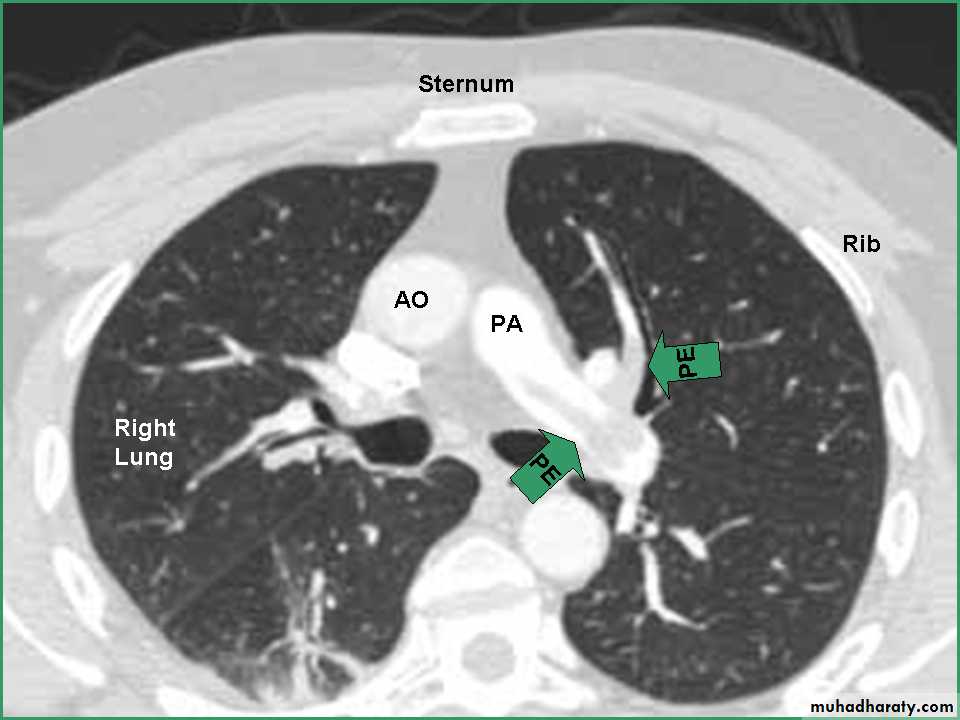
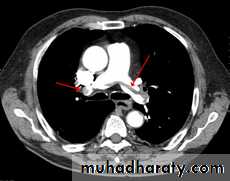
Investigations:
• ECG: tachycardia and nonspecific changes.
• CXR oligemia or linear or triangular consolidation,
• Ventilation–perfusion (V/Q) areas of normal ventillation with poor perfusion.
• Pulmonary angiograms: filling defects or obstruction of pulmonary arterial branches.
• Echocardiography
Medical treatment:
• Supplementary O2• Mechanical ventilation
• Invasive cardiac monitoring
• Pharmaceutical myocardial support, mechanical myocardial support
• Immediate anticoagulation with i.v. heparin
• Consider thrombolysis in patients with major-to-massive pulmonary embolism.
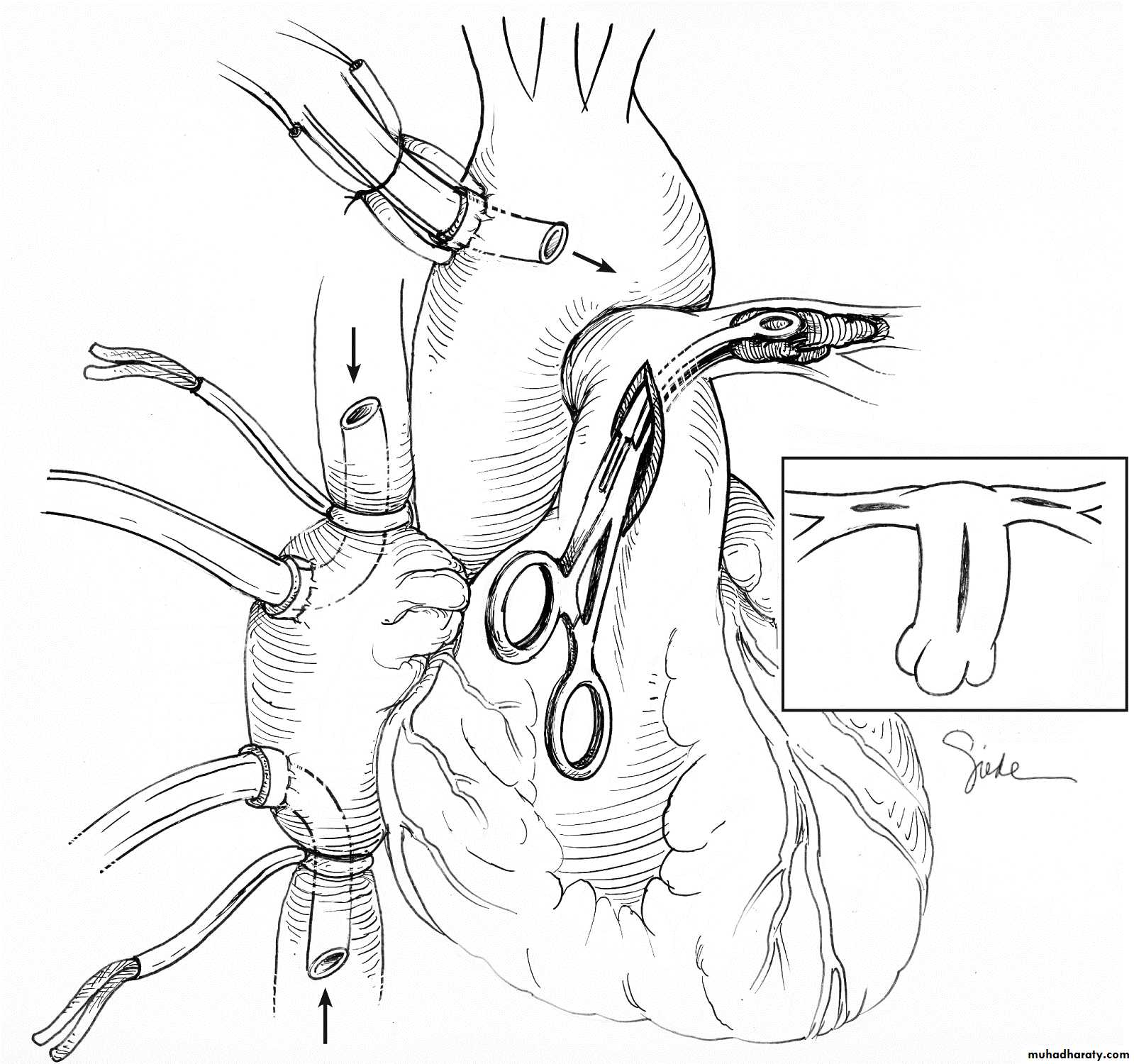
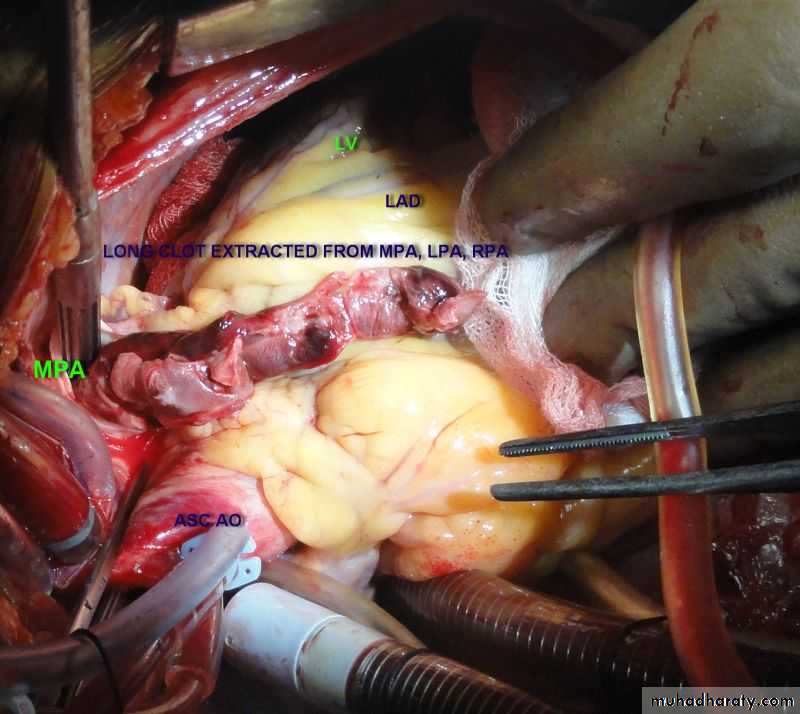
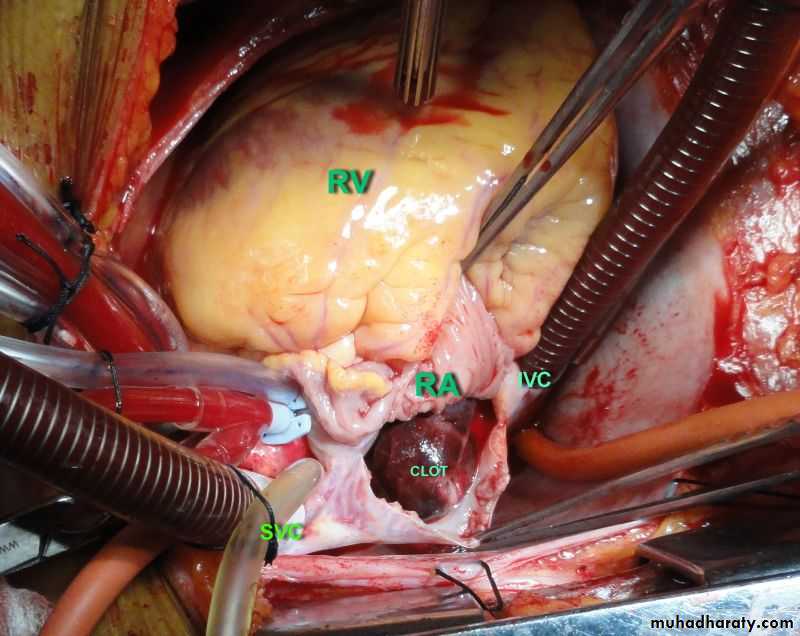
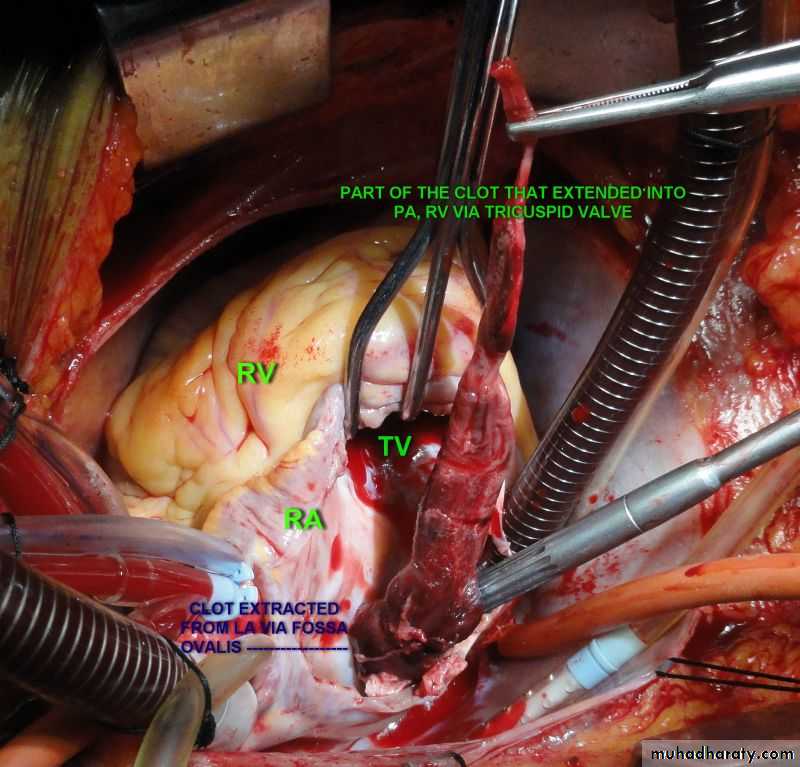
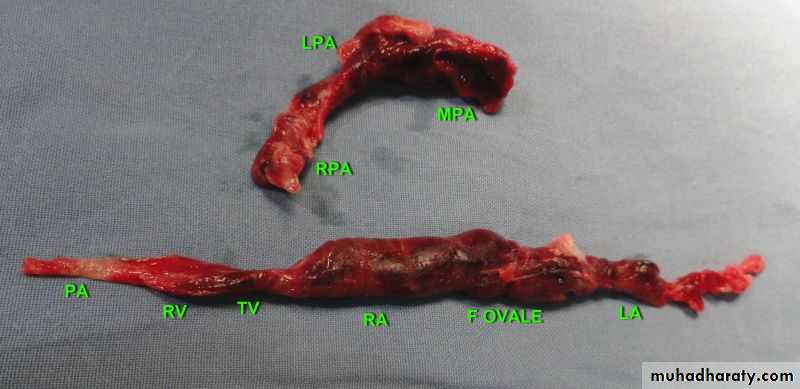
Surgical treatment:
Emergency pulmonary embolectomy is indicated in• Critical hemodynamic instability or severe respiratory distress
• thrombolytic or anticoagulation therapy is contraindicated,
• The presence of a large clot trapped within the right atrium or ventricle