
1
Fifth stage
Surgery
Lec-2
.د
أركان
29/3/2016
Monitoring in Anesthesia
OXYGENATION
• Oxygenation is monitored clinically by providing adequate illumination of the
patient's color and by pulse oximetry
• pulse oximeter measure :
1. The oxygen saturation of haemoglobin in arterial blood - which is a measure of the
average amount of oxygen bound to each haemoglobin molecule. The percentage
saturation is given as a digital readout together with an audible signal varying in pitch
depending on the oxygen saturation
2. The pulse rate - in beats per minute .
VENTILATION
Ventilation is monitored clinically by verification of a correctly positioned endotracheal
tube as well as by observing chest excursions, reservoir bag displacement, and breath
sounds over both lung fields.
Ventilation is quantitatively monitored using end tidal carbon dioxide (ETCO2) analysis
as well as an audible disconnection alarm on all mechanically ventilated patients
CIRCULATION
palpation of the pulse
auscultation of heart sounds
Blood pressure measurement :
-Automated non-invasive BP measurements NIBP
-lnvasive BP monitoring :The radial artery at the wrist is the most common site for an
arterial catheter insertion. The femoral, brachial, and dorsalis pedis arteries are
alternative sites
A central venous pressure (CVP) catheter provides an estimate of the right atrial and
right ventricular pressures. The CVP reflects the patients blood volume, venous tone,
and right ventricular performance. CVP 1 - 10 mmHg
Electrocardiogram (ECG)
The ECG monitors the conduction of electrical impulses through the heart. It is used to
determine the heart rate and to detect and diagnose arrhythmias, myocardial ischemia,
pacemaker function, and electrolyte abnormalities

2
Temperature :
- Core temperature: measured through tympanic membrane, nasopharynx,
esophagus,rectal , urinary bladder , pulmonary artery.
- Peripheral temperature
Urinary output
: should be monitored hourly
Oliguria:- urinary output <0.5 ml/kg/h
Peripheral nerve stimulator :
Monitoring neuromuscular function of patient receiving neuromuscular blocking agent
Arterial Blood Gas Interpretation ABG
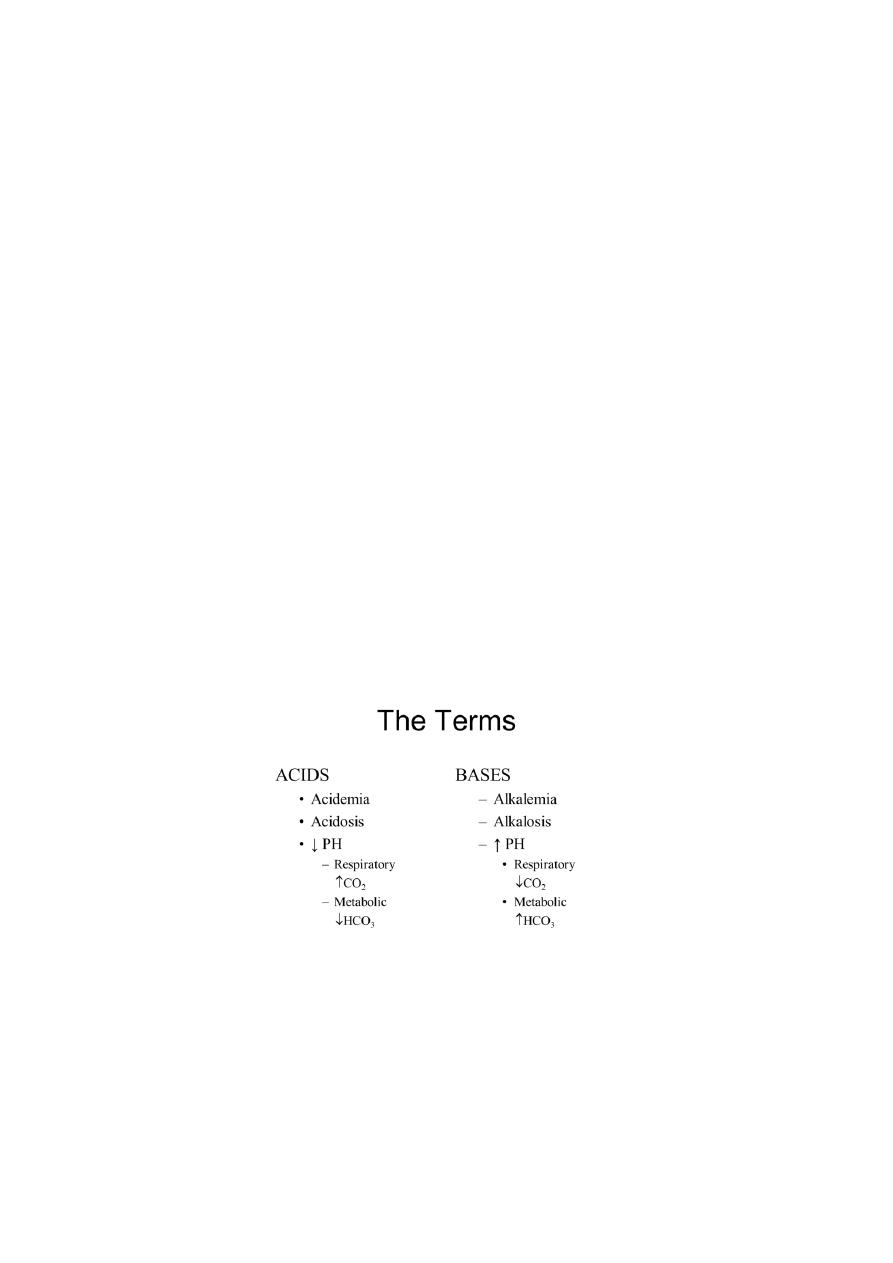
• Acid- base disturbances are indicators of serious underlying pathology
• Arterial blood gas examination is a useful investigation in patients with suspected
respiratory or metabolic disease
• serial blood gas investigation can monitor the progress or treatment of the
underlying disease.
• PH is the negative log of the H+ ion concentration
• PH is important because H+ ions react highly with cellular proteins resulting in
alterations in their function. Therefore, avoiding acidemia and alkalemia by tightly
regulating [H+] is essential for normal cellular function
Blood samples :
• Radial artery
• Brachial a.
• Axillary a.
• Dorsalis pedis a.
• Femoral a
Blood gas normal values
• PH: 7.35- 7.45; measures blood acidity & concentration of hydrogen ions
• PaCO2: 35- 45 mm Hg; measures partial pressure of carbon dioxide
3
• HCO3: 22- 26 mEq/L; measures amount of bicarbonate
• Base excess (BE) (-2.0 to +2.0 mEq/L) The base deficit (BD) is the number of mEq/L
of base (or acid) needed to titrate a serum pH back to normal at 37°C while the
PaCO2 is held constant at 40 mmHg, thus eliminating the respiratory component
.Therefore, the BD represents only the metabolic component of an acid-base
disorder
• PaO2: 80- 100 mm Hg; measures partial pressure of oxygen (at sea level , FiO2 = 21%
, Age-dependent)
• SaO
2
93-98%
ABG provides an assessment of the following:
• Oxygenation (PaO2 , O2 saturation). The PaO2 is the amount of oxygen dissolved in
the blood and therefore provides initial information on the efficiency of oxygenation.
• Ventilation (PaCO2). The adequacy of ventilation is inversely proportional to the
PaCO2, so that when ventilation increases, PaCO2 decreases, and when ventilation
decreases, PaCO2 increases.
• Acid-base status (pH, HCO3, and base deficit).
ABG
• PH → 7.35 – 7.45
• PaCO2 → 35 – 45 mmHg
• HCO3 → 22 – 26 mEq/L
• BE → - 2 ─ +2
• PaO2 → 80 – 100 mmHg (at sea level , FiO2 = 21%)
• SaO2 → 93 – 98%
