1
Fifth stage
Neuro-Surgery
Lec-3
د. عبدالرحمن
2/5/2016
HYDROCEPHALUS
Definition:
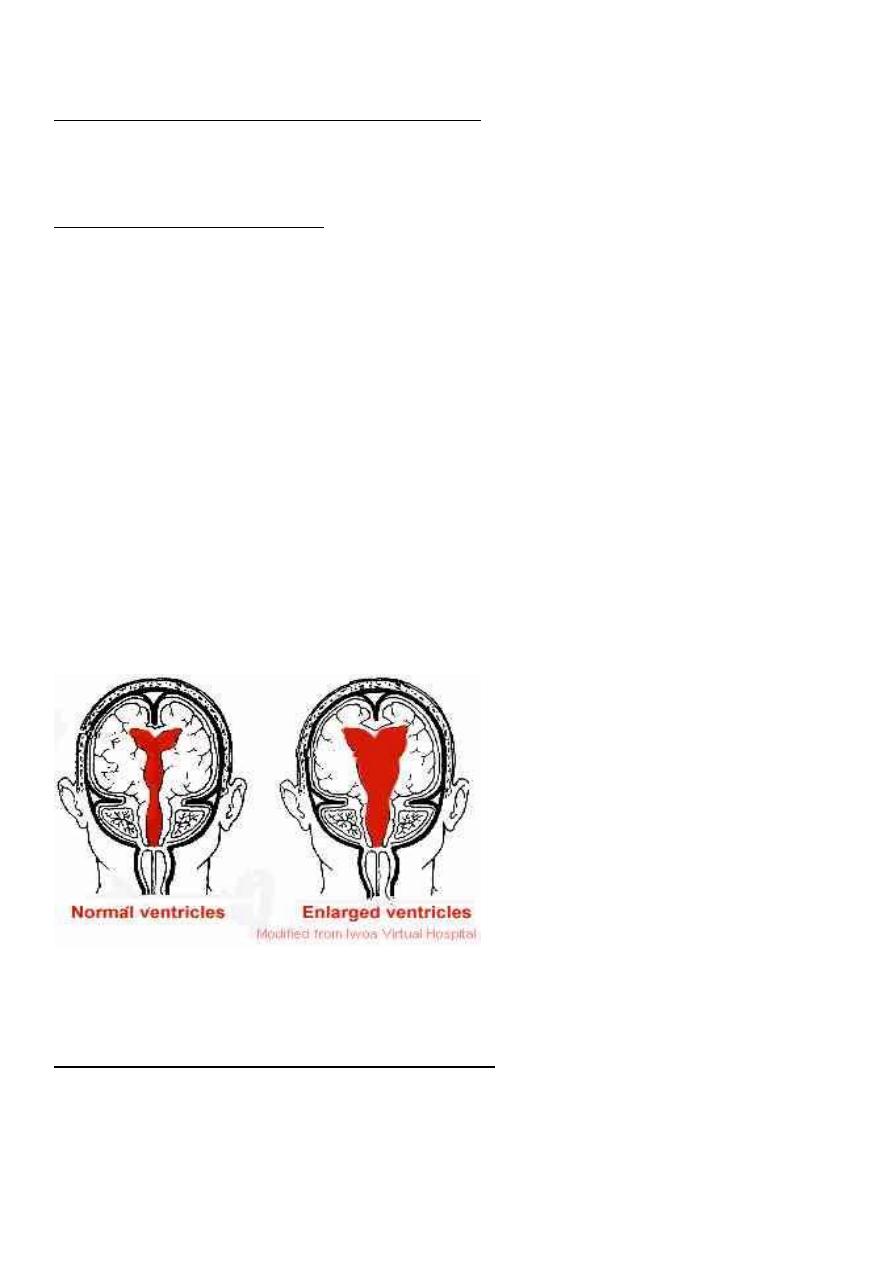
Hydrocephalus is defined as abnormal accumulation of cerebrospinal fluid (CSF) within the
ventricles and subarachnoid spaces. It is often associated with dilatation of the ventricular
system and increased intracranial pressure (ICP).
Physiology and circulation of CSF:
The normal volume of circulating CSF is about 150 ml.
The daily production of the CSF is about 450 ml, so the CSF volume is replaced
approximately three times daily.
CSF is produced by an active process independent of inracranial pressure (ICP).
80% of CSF is produced by the choroid plexus, and the rest is from the parenchyma
Functions of the CSF:
1. Protect and support the brain and spinal cord.
2. Maintain homeostasis by acting as a transport medium for transmitters and as a
method of removing the end-products of metabolism.
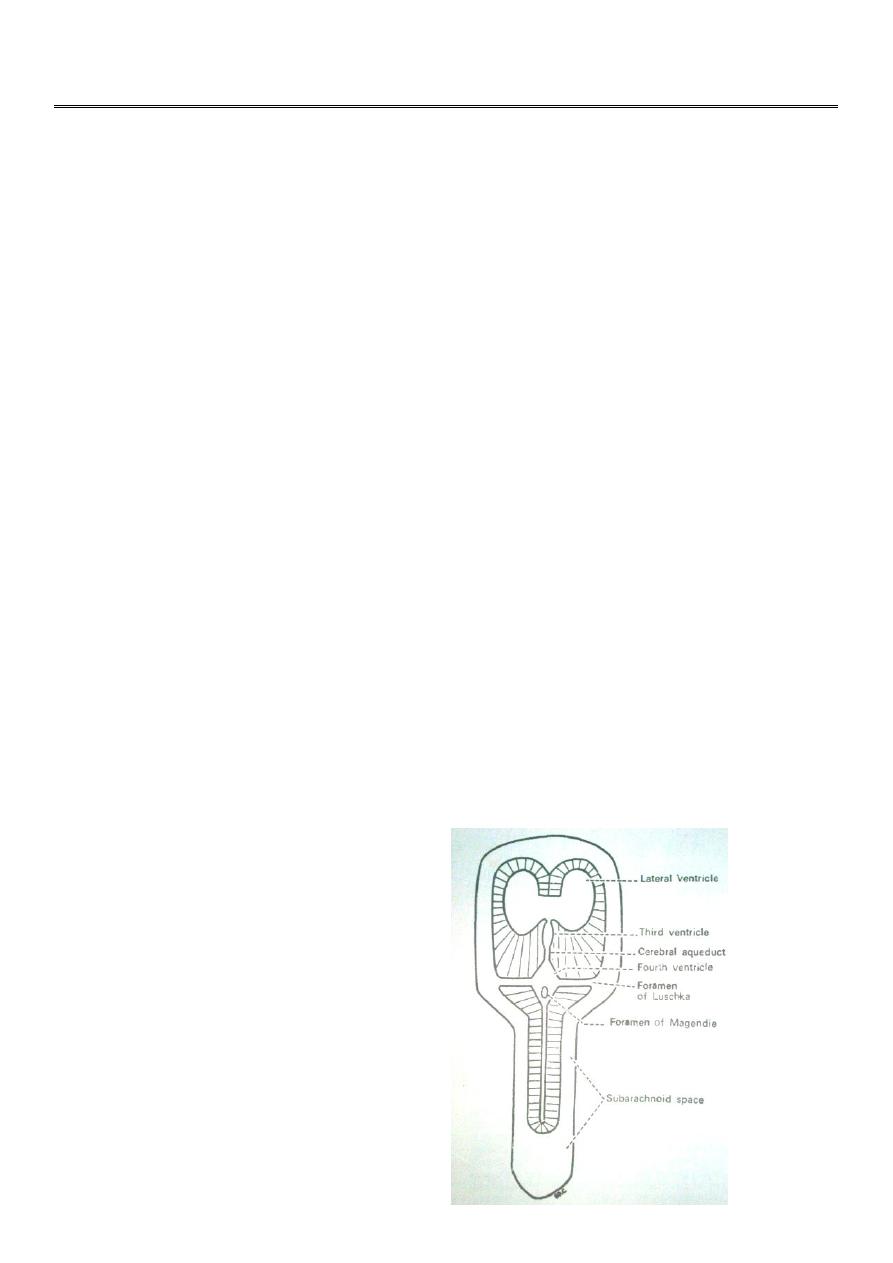
CSF Circulation:
lateral ventricles.
foramen of Monro
third ventricle
aqueduct of Sylvius
fourth ventricle
two foramina of Luschka
foramen of Magendie
subarachnoid space
arachnoid villi
venous blood
blood stream.
2
Classification of Hydrocephalus
Non-communicating hydrocephalus (Obstructive):
results from lesions that obstruct the CSF pathways from the lateral ventricles to the fourth
ventricle.
Communicating hydrocephalus:
refers to circumstances in which the intracerebral CSF pathways are patent but there is
accumulation of CSF, usually due to impaired CSF absorption.
Epidemiology of Hydrocephalus:
The incidence of infantile hydrocephalus is about 3 to 4 per 1000 live birth
Aetiologty of Hydrocephalus:
In patients with hydrocephalus, an imbalance has occurred between the normal
physiological production of CSF and its absorption.
This imbalance can be as a result of overproduction of CSF, an obstruction, or impaired
absorption.
Aetiologty of Hydrocephalus
Non-communicating hydrocephalus (Obstructive):
Lateral ventricle obstruction by tumours, e.g. basal ganglia glioma, thalamic glioma.
Third ventricular obstruction, due to colloid cyst of the 3rd ventricle or glioma of the
3rd ventricle
3
Occlusion of the aqueduct of Sylvius (either primary stenosis or secondary to a
tumour)
Forth ventricular obstruction due to posterior fossa tumour, e.g. medulloblastoma,
ependymoma, acoustic neuroma.
Communicating hydrocephalus:
Failure of absorption of CSF through the arachnoid granulations over the cerebral
hemispheres.
Sclerosis or scarring of the arachnoid granulations can occur after meningitis
(bacterial or tuberculous), subarachnoid haemorrhage (either spontaneous, traumatic
or postoperative), or trauma.
Oversecretion of CSF (choroid plexus papilloma).
Clinical Features of Hydrocephalus
Neonatal Hydrocephalus (Infantile):
1. Failure to thrive and feeding problems.
2. Enlargement of the head with increasing head circumference.
3. Craniofacial disproportion with expansion of the dome and "low set" ears and eyes.
4. The scalp is thin and glistening.
5. The veins of the scalp are distended.
6. The anterior fontanelle is enlarged, tense, and bulging.
7. Weakness of upward gaze (the setting-sun sign)(3rd ventricular pressure on midbrain
tectum).
8. Diastasis of the cranial sutures.
9. Transillumination of the head is usually positive (if cortical mantle is less than 1cm
and the patient is under 9 months age).
10. Bradycardia can be seen in extreme cases.
Hydrocephalus in older children and adults:
1. Headache.
2. Nausea and vomiting.
3. Deterioration in the level of consciousness.
4. May be associated ataxia.
5. Visual disturbance.
4
Investigations of Hydrocephalus:
A. Skull x-ray: can show
Separation of sutures.
Features of increased intracranial pressure
B. Ultrasound of the brain:
can be done through opened anterior fontanelle to see the ventricular system.
C. CT scan of the Brain:
Ventricular dilatation.
Can show the cause of obstruction as tumour.
D. MRI of the brain: same as CT but no radiation so can be used for follow up.
E. Lumbar puncture:
Can be done in communicating hydrocephalus for both diagnostic and therapeutic
aims.
Management of Hydrocephalus:
A. Medical management of Hydrocephalus:
By using methods to reduce CSF production, but till now no definite medical treatment is
satisfactory.
B. Surgical management:
1. Removal of obstructing lesion e.g. removal of tumour will resolve hydrocephalus.
2. Bypassing obstruction: either by:
a. Endoscopic third ventriculostomy
b. External drainage of CSF
c. Internal diversion (Shunting)
Types of Internal Shunts
Ventriculo-Peritoneal Shunts.
Ventriculo-Atrial Shunts.
Ventriculo-Pleural Shunts.
5
The complications of shunting
Shunt obstruction:
Shunt infection.
Intracranial haemorrhage either:
o Intracerebral haemorrhage, or
o Subdural haematoma.
Complications of Ventriculo-Atrial Shunts
Infective Endocarditis.
Volume Overload (Heart Failure).
Arrhythmias (SA node).
Complications of Ventriculopleural Shunts:
Pneumothorax and Haemopneumothorax.
Pleural Effusion.
Pleural Empyema.
Benign intracranial hypertension:
Benign intracranial hypertension, also known as pseudotumour cerebri, is, as its
name implies, a disease of raised intracranial pressure, which usually runs a self-
limiting course.
Although termed ‘benign’, this condition can cause blindness due to severe
papilloedema.
The pathogenesis is poorly understood.
The condition usually occurs in obese females.
Aetiology:
Hypoparathyroidism.
Vitamin A excess (used to treat acne)
Pernicious anaemia.
Drug reaction—tetracycline, nalidixic acid, sulfamethoxazole, indomethacin,
danazole, lithium carbonate, oral contraceptive steroids.
A similar condition results from venous sinus thrombosis.
Clinical features:
Headaches
6
Visual disturbance.
The headaches have the features of raised intracranial pressure in that they are
worse in the morning and exacerbated by straining, stooping and coughing.
The visual problems result from:
Papilloedema
Secondary optic atrophy
Diplopia due to sixth cranial nerve palsy.
Investigations
The CT and/or MRI scan will show no cause for the papilloedema and the ventricles
will often be smaller than usual.
Digital subtraction cerebral angiography or magnetic resonance venography may be
performed to exclude thrombosis of a venous sinus as the cause.
If the CT scan or MRI shows no mass or lesion a lumbar puncture is usually
performed; the pressure will be raised. CSF examination is normal in benign
intracranial hypertension but biochemistry and cytological investigations should be
performed to exclude underlying pathology.
Medical (Conservative) Treatment
Benign intracranial hypertension is usually a self-limiting disease and most cases respond to
simple conservative treatment. The usual measures undertaken are:
A. Conservative Treatment:
1. Weight loss (the patients are usually obese).
2. Stopping any medication that may have led to the disease, e.g. oral contraceptives,
tetracycline.
3. Diuretic therapy.
4. Acetazolamide (reduces CSF production).
5. If there is no improvement with the above measures, treatment with glycerol or
steroids may be tried.
Surgical Treatment
The major indications for surgical treatment are:
1. Persistent severe papilloedema despite conservative measures
2. Failing vision.
3. Intractable headaches despite conservative measures.
The surgical procedures that can be performed are:
• Optic nerve sheath decompression
• Lumboperitoneal shunt.
