1
Fifth stage
Medicine
Lec-9
د . منوع
1/1/2014
Oxygen Therapy and Airway Management, Ventilator therapy
• Oxygen was discovered independently by the Swedish apothecary Karl W.Scheele, in
1772, and by the English amateur chemist Joseph Priestly,in August 1774.
• Priestley first liberated oxygen by intensely heating 'mercurius calcinatus' (mercuric
oxide) placed over liquid mercury in a closed vessel. He called this new gas
"dephlogisticated air, "oxygenated."
Basic Concepts of Oxygen
Oxygen Cascade:
Oxygen Cascade:
Inspired = 150 mmHg at Sea Level
↓ Alveolar PO
2
= 103
↓ Arterial=100
↓ Capillary= 51
↓ Mitochondrial= 1-10 ↓ Mitochondrial= 1-10
(FiO
2
expressed as 0.21-1.0 or 21- 100%)
Oxygen content of blood
The theoretical maximum oxygen carrying capacity is 1.39 ml O2/g Hb, but direct
measurement gives a capacity of 1.34 ml O2/g Hb.1.34 is also known as Hüfner’s constant.
The oxygen content of blood is the volume of oxygen carried in each 100 ml blood.
It is calculated by: (O2 carried by Hb) + (O2 in solution) = (1.34 x Hb x SpO2 x 0.01) + (0.023
x PaO2)
2
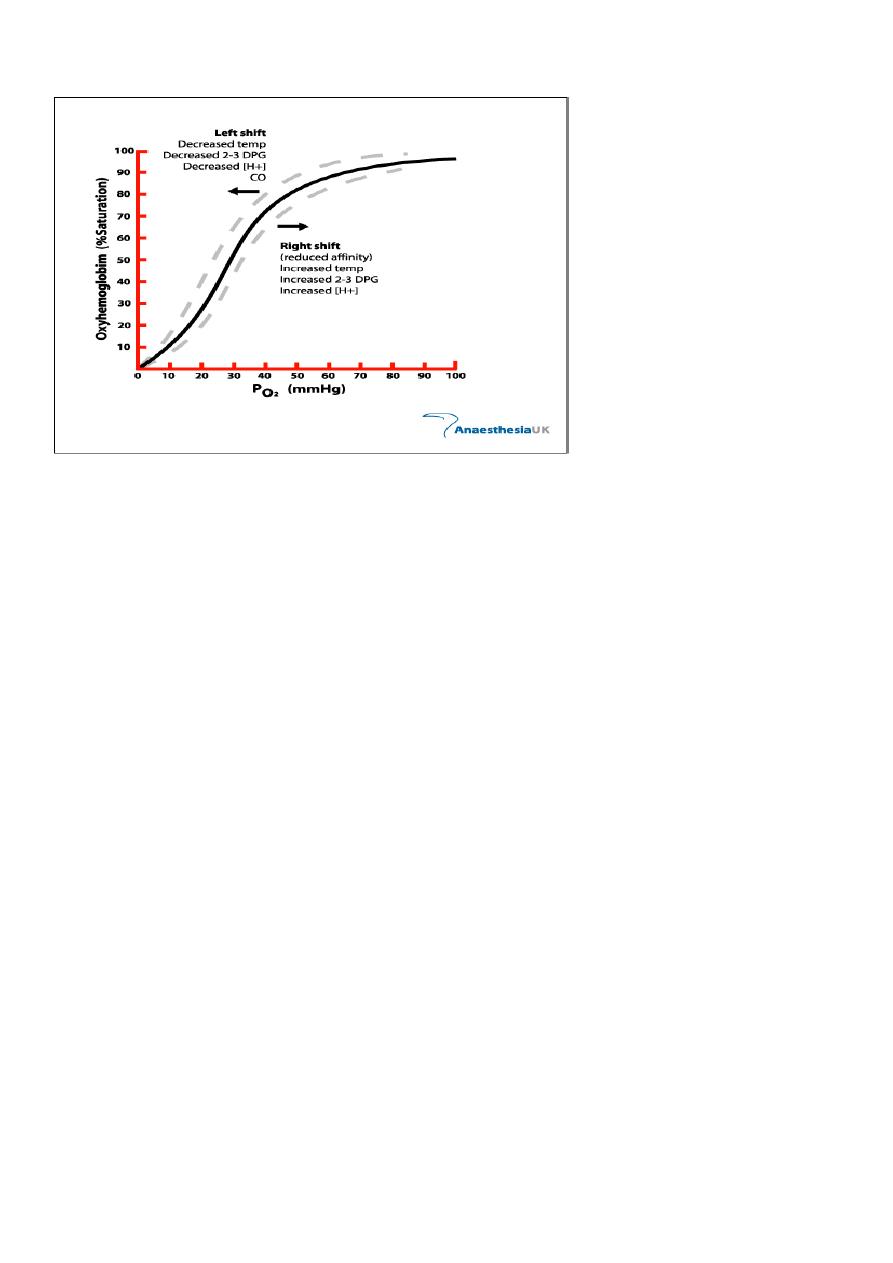
Oxygen dissociation curve (ODC)
Indications for Oxygen Therapy
Tachypnea
Cyanosis
Restlessness
Disorientation
Cardiac arrhythmias
Slow bounding pulse
Tachycardia
Hypertension
Dyspnea
Coma
Labored breathing (use of accessory muscles, nasal flaring)
Lethargy
Tremors/seizure activity
Oxygen Therapy
“Generally speaking”, a patient who is breathing less than 12 and more than 24 /minute
needs oxygen of some kind

3
A. THREE CLINICAL GOALS OF O2 THERAPY
OXYGEN THERAPY
1. TREAT HYPOXEMIA
2. DECREASE WORK OF BREATHING (WOB)
3. DECREASE MYOCARDIAL WORK
B. FACTORS THAT DETERMINE WHICH SYSTEM TO USE
1. PATIENT COMFORT
2. THE LEVEL OF FIO2 THAT IS NEEDED
3. THE REQUIREMENT THAT THE FIO2 BE CONTROLLED
BE CONTROLLED WITHIN A CERTAIN RANGE.
4. THE LEVEL OF HUMIDIFICATION AND OR NEBULIZATION
Oxygen therapy To ensure safe and effective treatment
Oxygen is required for the functioning and survival of all body tissues and deprivation for
more than a few minutes is fatal.
In immediately life threatening situations oxygen should be administered.
Hypoxaemia. Acute hypotension.
Breathing inadequacy. Trauma. Acute illness. CO poisoning. Severe anaemia. During the
peri-operative period.
Oxygen is a prescription drug.
Prescriptions should include – Flow rate.
Delivery system.
Duration.
Instructions for monitoring.
Monitoring resps oxygen sats not definitive tool need to be looking at other things
acccessory muscles etc

4
Oxygen therapy
Oxygen therapy Humidification Is recommended if more than 4 litres/min is delivered.
Helps prevent drying of mucous membranes.
Helps prevent the formation of tenacious sputum.
Oxygen concentrations will be affected with all delivery systems if not fitted correctly or
tubing becomes kinked and ports obstructed.
Methods of Oxygen Delivery
Most common methods of oxygen delivery include
Nasal Cannula
Venturi Mask
100% Non-Rebreather Mask
Mechanical Ventilation
Hyperbaric Oxygen Therapy
(HBOT)
Oxygen Delivery Methods
Nasal Cannula
Comfortable, convenient, mouth breathing will not effect % of O2 delivered
Liters/min = %
2 l/m = 24-28%
3 l/m = 28-30%
4 l/m = 32-36%
5 l/m = 36-40%
6 l/m = 40-44%
Cannot administer > 6 liters/minute (44%)

5
Nasal Cannula
Provides limited oxygen concentration
Used when patients cannot tolerate mask
Prongs and other uses
Concentration of 24 to 44%
Flow rate set between 1 to 6 liters
For every liter per minute of flow delivered, the oxygen concentration the patient inhales
increases by 4%
Simple facemask Easy to use.
Allows administration of variable concentration dependant on flow of fresh gas up to 40%.
Nasal cannulae Easy to use. Well tolerated. Comfortable for long periods. Patient can eat
and talk easily.
Possible to deliver oxygen concentrations of 24-40% at flow rates of 1-6 litres/min.
Flow rates in excess of 4 litres/min might cause discomfort and drying of mucous
membranes and are best avoided.
Flow Rate: 10 L/Min
O2 Conc.: 40 – 60 %
Use: moderate FiO2, mouth breathers
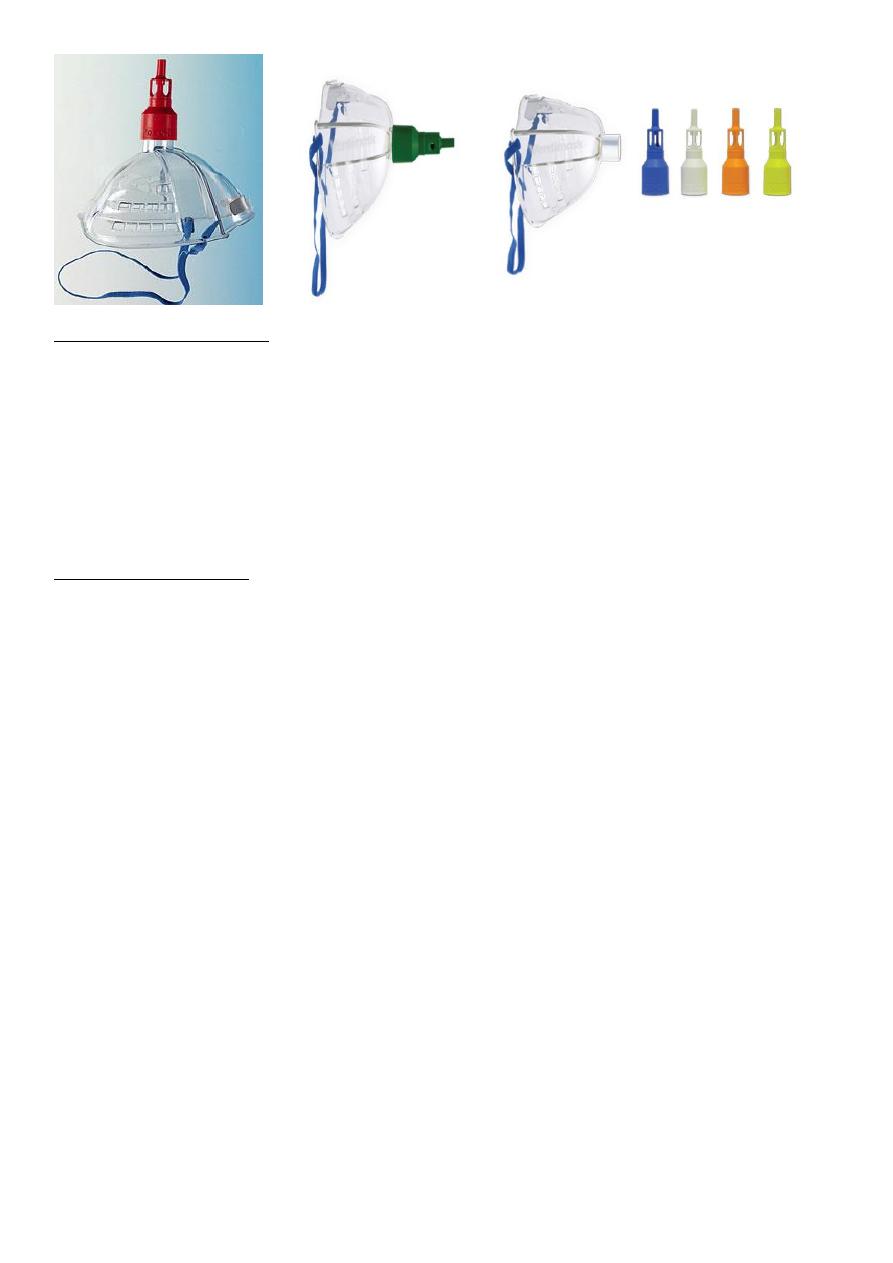
Venturi Mask
FiO2 Delivery
Blue 24% Yellow 28%
White 31% Green 35%
Pink 40%
Provides precise concentrations of oxygen
Entrainment valve to adjust oxygen delivery
Mostly used in the hospital setting for COPD patients
Concerns
Tight seal is a must Interferes with eating/drinking Condensation collection
6
Partial rebreathing mask
• 6-10L /min
• FiO
2
0.35-0.60
• Has no valves
• Inspiration –O
2
flows to mask and patient
• Expiration – source O
2
and expired gas enters the bag
Non rebreathing mask
• 6-10L/min
• FiO
2
0.55-0.70
• Has 2 one way valves
• Insp- insp valve opens provides O
2
to patient
• Exp- exp valve opens divert exp gas to atmosphere
• Large air leaks
Non-rebreathing mask Allows the delivery of high concentrations of oxygen (85% at 15
litres/min).
Has a reservoir bag to entrain oxygen. One way valves prevent room and expired air from
diluting the oxygen concentration. A tight seal is essential.
Reservoir bag must be seen to expand freely.
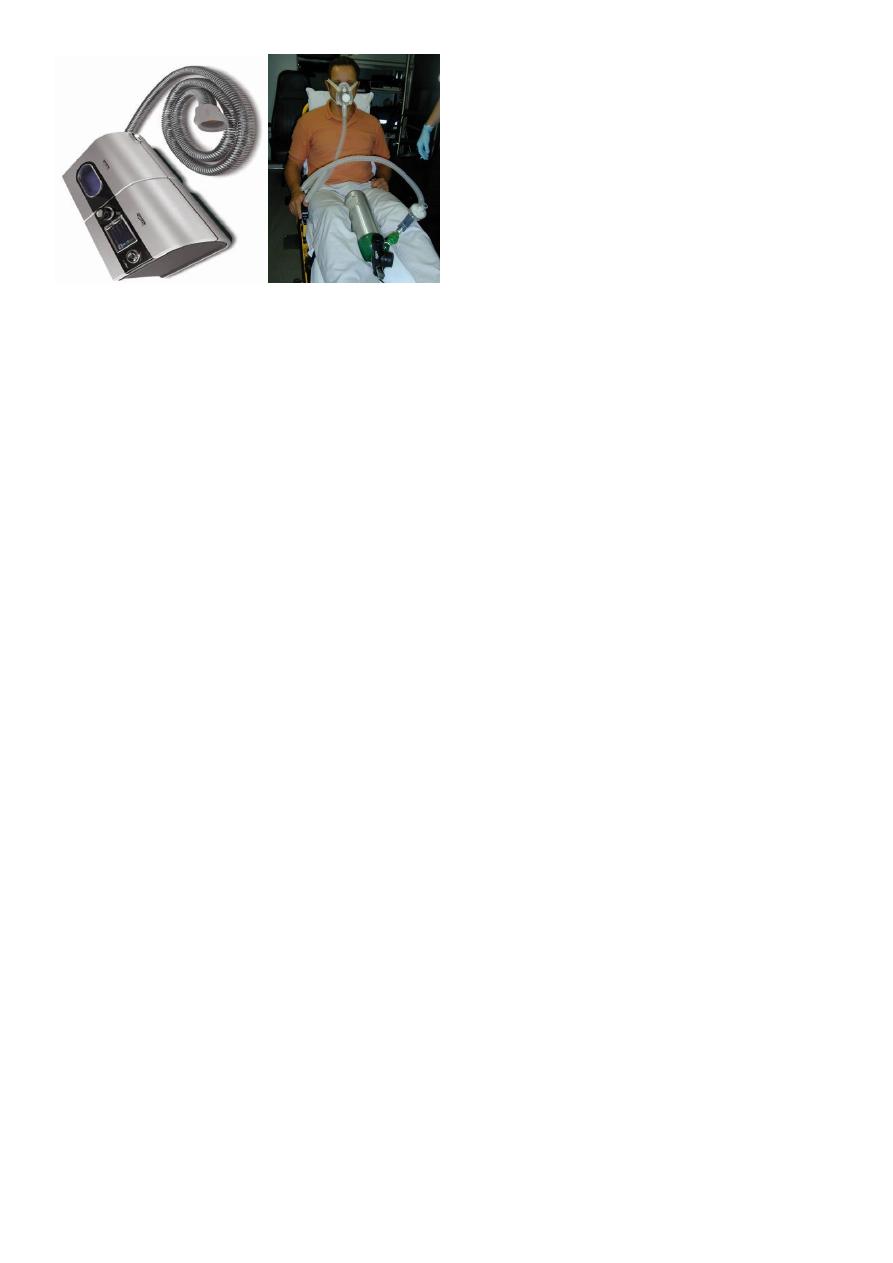
Oxygen Delivery MethodsMechanical Ventilation
Allows administration of 100% oxygen
Controls breathing pattern for patients who are unable to maintain adequate ventilation
Is a temporary support that “buys time” for correcting the primary pathologic process

7
Indications for Mechanical Ventilation
Mechanical Failure
Ventilatory Failure
Oxygenation Failure
General Anesthesia
Post-Cardiac Arrest
Two categories of ventilators
Negative pressure ventilators
Iron lung
Cuirass ventilator
Positive pressure ventilators
Two categories
Volume-cycled (volume-preset)
Pressure-cycled (pressure-preset)
Iron Lung
Mechanical Ventilation PEEP
Description
Maintains a preset positive airway pressure at the end of expiration
Increases PaO2 so that FiO2 can be decreased
Increases DO2 (amt of delivered O2 to tissue)
Maximizes pulmonary compliance
Minimized pulmonary shunting

8
Indications
PaO2 < 60 on FiO2 > 60% by recruiting dysfunctional alveoli
Increases intrapulmonary pressure after cardiac surgery to decrease intrathoracic
bleeding (research does not support this idea)
Advantages
Improves PaO2 and SaO2 while allowing FiO2 to be decreased
Decreases the work of breathing
Keeps airways from closing at end expiration (esp. in pts with surfactant deficiency)
Disadvantages
Increased functional residual capacity (increases risk for barotrauma)
Can cause increased dead space and increased ICP
In pts with increased ICP, must assure CO2 elimination
Contraindicated: hypovolemia, drug induced low cardiac output, unilateral lung disease,
COPD
Mechanical Ventilation CPAP
Description
Constant positive pressure is applied throughout the respiratory cycle to keep alveoli
open
Indications
To wean without having to remove the ventilator and having to connect to additional
equipment
9
Advantages
Takes advantage of the ventilator alarm systems providing psychological security of the
ventilator being there
Disadvantages
Patient may sense resistance as he breathes through the ventilator tubing
Mechanical Ventilation Complications
1. Respiratory arrest from disconnection
2. Respiratory infection (VAP)
3. Acid-base imbalances
4. Oxygen toxicity
5. Pneumothorax
6. GI bleeding
7. Barotrauma
8. Decreased cardiac output
Ventilator Weaning
Vital Capacity at least 10 – 15 ml/kg
Tidal Volume > 5 ml/kg
Resting minute volume > 10 L per minute
ABG’s adequate on < 40% FiO2
Stable vital signs
Intact airway protective reflexes (strong cough)
Absence of dyspnea, neuromuscular fatigue, pain, diaphoresis, restlessness, use of
accessory muscles
10
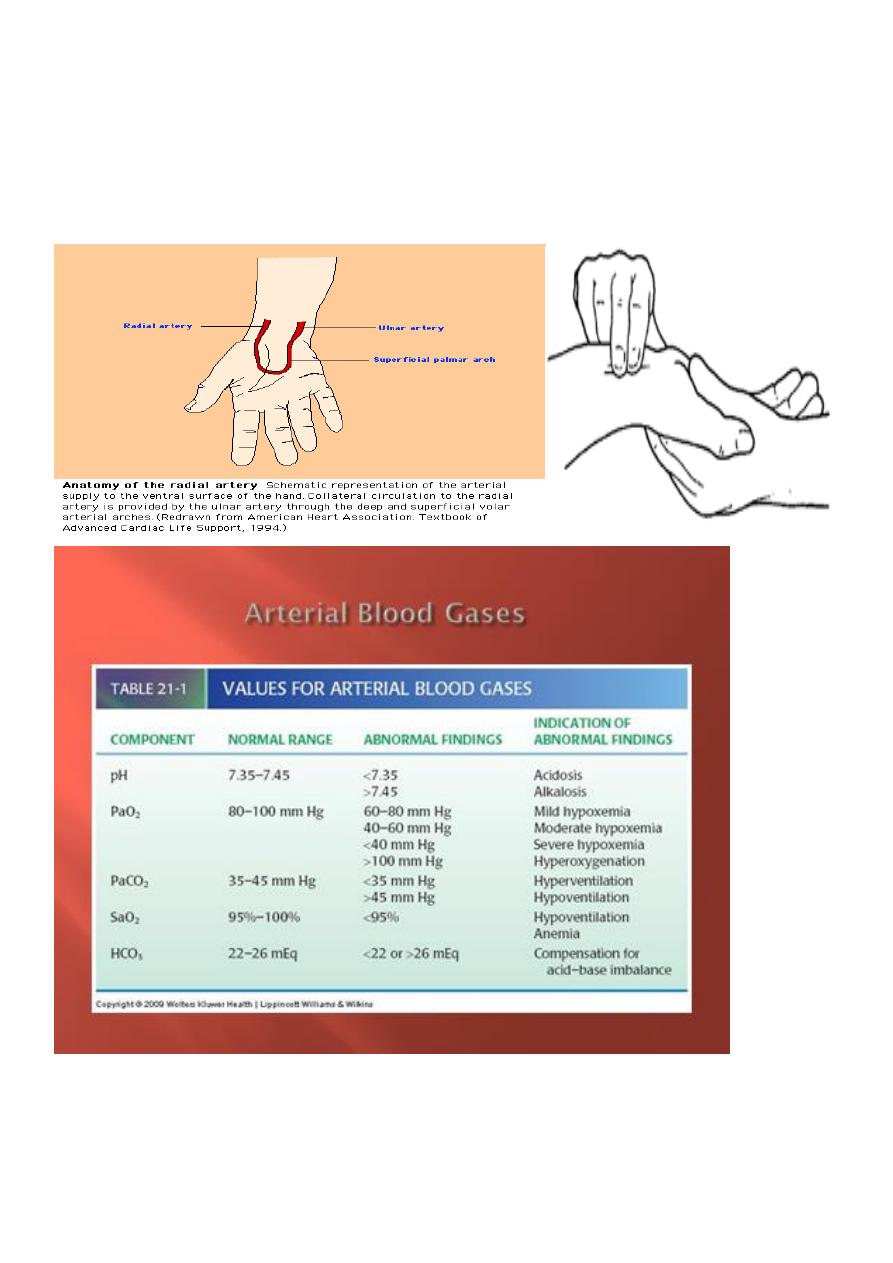
Arterial blood gas Analysis
• Which Artery to Choose?
• The radial artery is superficial, has collaterals and is easily compressed. It should almost
always be the first choice.
• Other arteries (femoral, dorsalis pedis, brachial) can be used in emergencies.
