
1
Fifth stage
Medicine
Lec-3
.د
منوع
1/1/2014
Rehabilitation
Rehabilitation:
Is the whole process of restoring a disabled person to a condition in which he is
able, as early as possible, to resume a normal life.
The World Health Organization developed the International Classification of disease,
Impairments, Disabilities and Handicaps” in 1980.
Disease: a condition of altered pathophysiology.
Impairment: loss or abnormality of an organ in structure or function .
Disability: limitation of performing tasks, activities and roles to the expected level
considered normal for a human being.
Handicap: lack of societal role fulfillment for an individual due to a disability.
Rehabilitation team:
Attending physician.
Occupational therapist .
Physical therapist.
Rehabilitation nurse.
Psychologist.
Social worker.
Vocational counselor.
Prosthetist - orthotist.
Speech - language pathologist.
Other “functional specialists” e.g.(audiologist, electro physiologist).
2
Physical therapists:
Work principally with gross motor functions:
Range of motion.
Strengthening to facilitate ambulation, mobility and balance.
Evaluate and fit manual wheel chairs.
Train the individual in the use of orthotics and prosthetic limbs.
Evaluate home environments.
Use of modalities such as heat, cold, ultrasound and massage.
Occupational therapists:
Work principally with fine motor function:
Upper extremity range of motion and strengthening to facilitate grooming, feeding,
dressing, and toileting.
They provide and train individuals to use adaptive equipment to facilitate the functions
mentioned.
They evaluate and manage the powered wheel chair.
Home environment evaluations and educate on energy-conserving methods of self-care
and home management tasks.
The Rehabilitation psychologists: They addressing psychological issues related to an
injury.
Mandate includes the patient’s and family’s needs .
They address issues related to adjustment of disability for the patient and their family,
depression and sexuality issues.
They also provide a variety of testing to evaluate personality issues and cognitive
functioning.
The Rehabilitation Nurses:
Wound care and skin management.
Adjustment of disability.
3
Bowel and bladder rehabilitation.
Goal setting.
Psychological support and medication management.
Nurses encourage patients to be maximally independent with their care, to be involved
with the goal setting process and ultimately to self-direct their care.
Speech pathologists:
They are experts in speech function such as pronunciation and word finding.
They also evaluate swallowing function and safety.
They provide cognition and communication evaluations, identifying deficits and
providing compensatory strategies for the patients, care givers and team members.
Social workers:
They provide emotional support for families.
Evaluate living situations and coordinate disposition.
They identify community services available for patients.
Vocational counselors:
Optimize the health and abilities of potential disabled employees.
Provide an expert reports for the individual and their present or future employers, or
the vocational service working on behalf of the individual
Promote knowledge to specialist vocational services and social services.
Assist and facilitate the individual to achieve a successful work and participation in
this work in any possible and reasonable way.
The prosthesis' / orthotist works:
They evaluate, design, and make prosthetic limbs and orthoses.
They also evaluate their fit and function after fabrication.
4
General treatment lines:
Define disability
Measure the disability.
Medical care : treat causative illness.
prevent additional disability
Enhance / support functional capacity of affected organ (e.g. device & equipments).
Get family support as well as social & institutional.
Modify social & vocational environment.
Deal with psychological values to improve opinions, beliefs& performance.
Use the best education techniques.
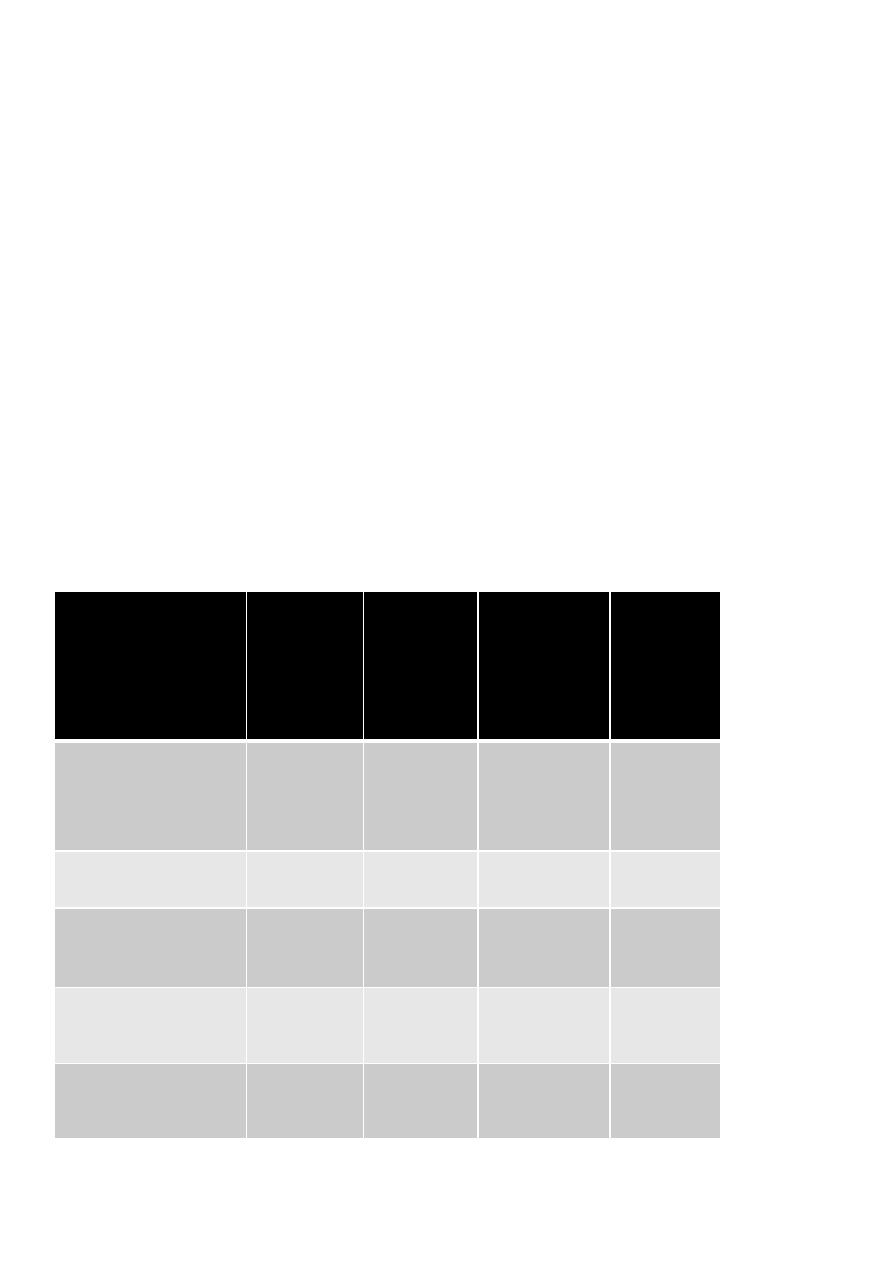
An example of disability measurements \ health assessment questionnaire
(HAQ):
At this moment ,
are you able to
Without
any
difficulty
(=1)
With
some
difficulty
(=2)
With much
difficulty
(=3)
Unable to
do (=4)
Dressing yourself,
Including tying
shoelaces & doing
buttons
----------
----------
--------
----------
Get in & out of bed
?
----------
----------
---------
----------
Lift a full cup or
glass to your mouth
?
-----------
----------
---------
----------
Walking outdoors on
flat ground ?
-----------
----------
---------
----------
Wash & dry your
entire body ?
-----------
----------
---------
----------
5
Bend down to pick up
clothing from floor ?
-----------
----------
---------
----------
Turn regular faucets
on & off ?
-----------
----------
---------
----------
Get in & out of a
car ?
-----------
----------
---------
----------
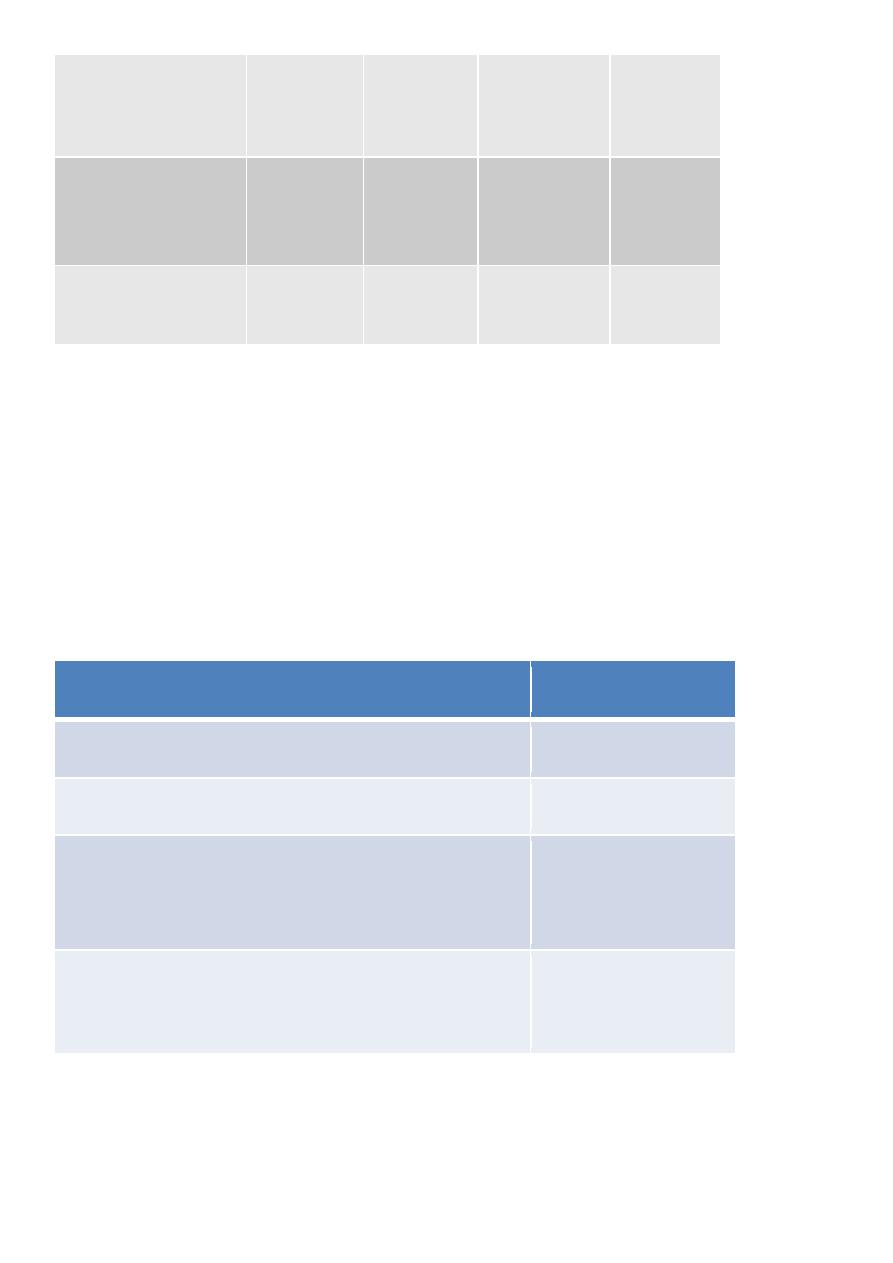
Activities of daily living (ADL)
1) Self care: Transfer & home mobility, eating, bathing, toileting, dressing and
grooming.
2) Communication (speaking, listening, reading, writing)
3) Duties : Vocational and non-vocational (e.g. shopping , house keeping).
Functional independence measure (FIM)\\ For each ADL performance a number is
given:
ADL performance
Complete independence
7
Modified independence (device)
6
Modified dependence :-
Supervision
Minimal assist (subject =75% )
Moderate assist (subject =50%)
5
4
3
Complete dependence :-
Maximal assist (subject =25%)
Total assist (subject =100)
2
1
6
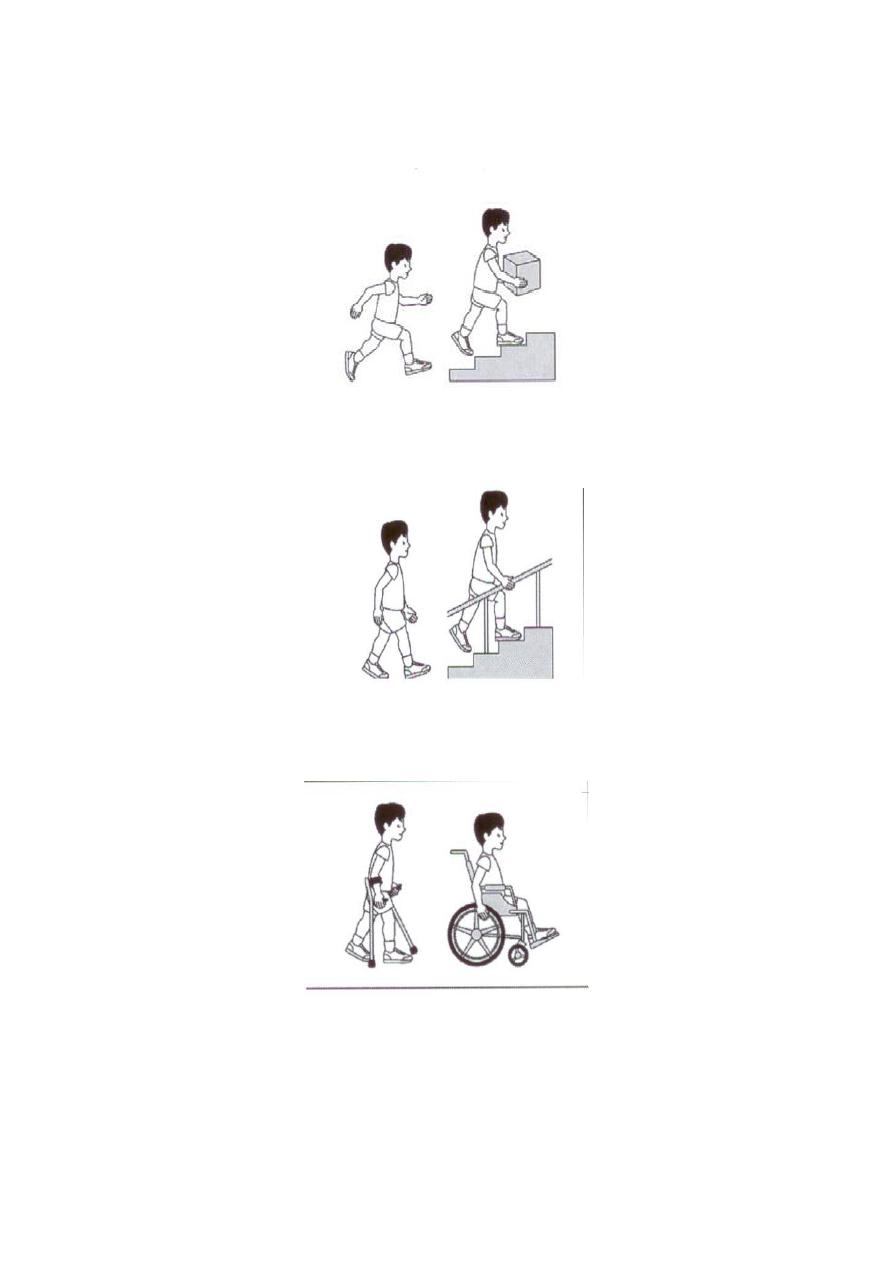
Level of motor abilities; Gross motor functions classification system (GMFCS):
I) walks independent, runs, climbs stairs, jumps.
II) walks independent, hang on when climbs stairs.
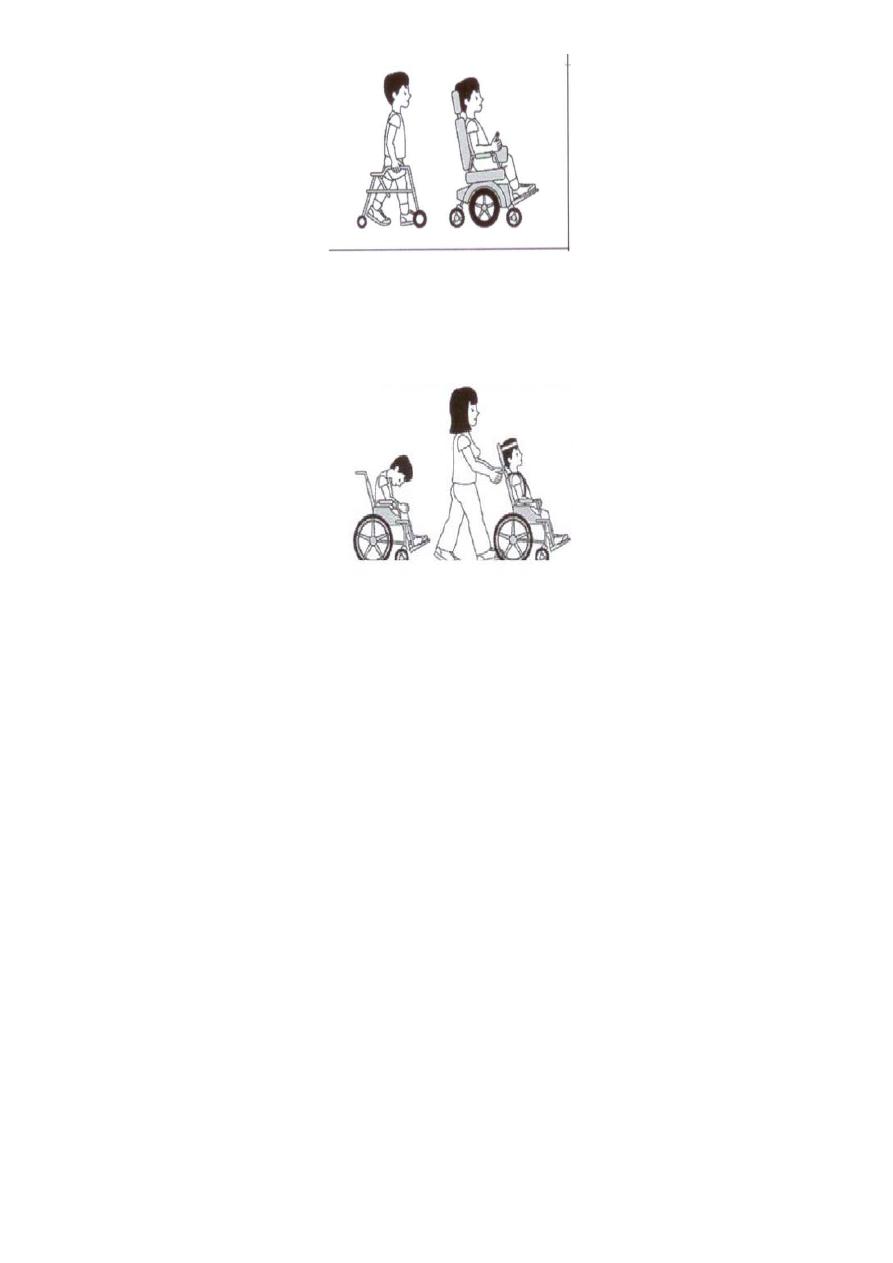
III) Walks independent with aid(crutches,stick,rollator) for long distance uses wheelchair
(propels independent).
IV) Mobility mainly by wheelchair (power chair), indoors walks with rollator.
7
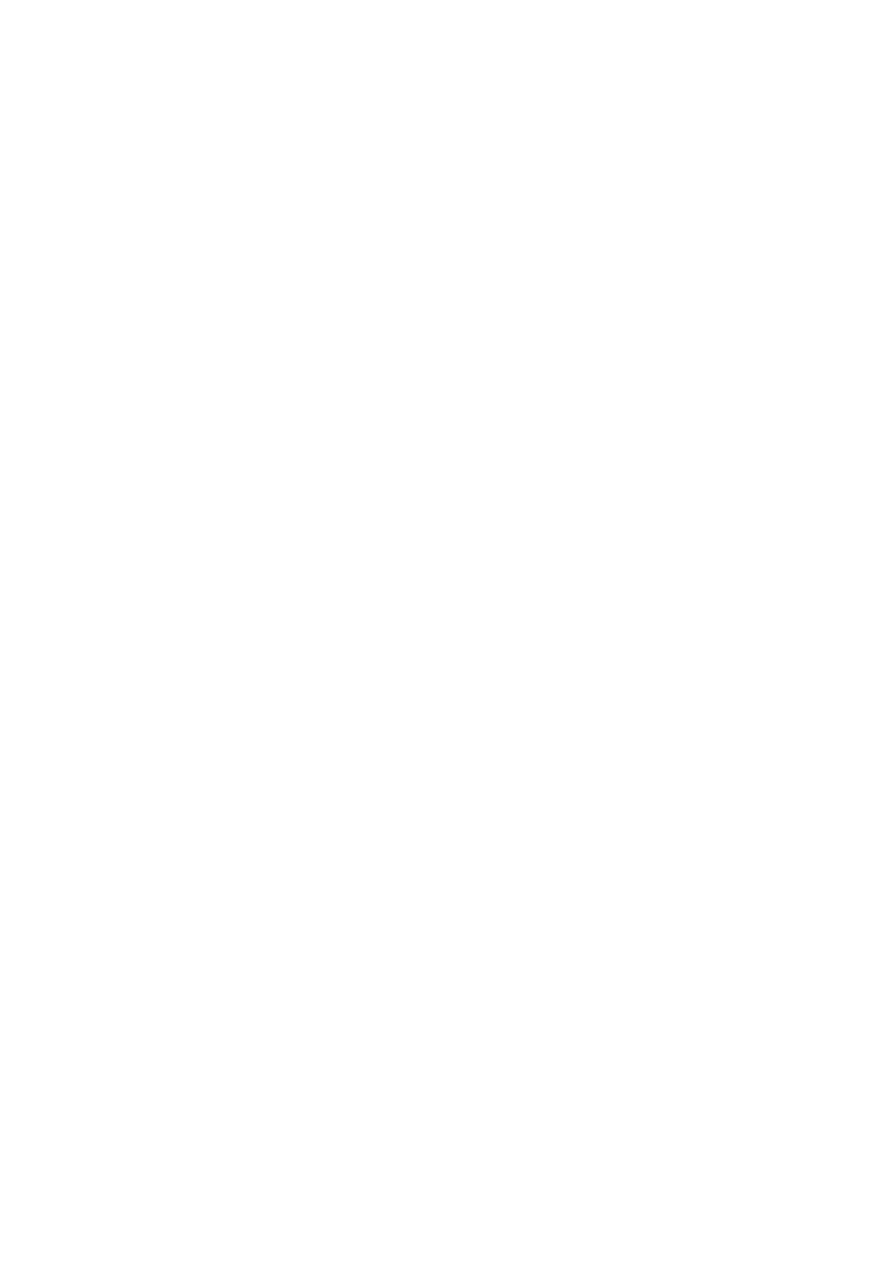
V) No independent mobility, abnormal postural control (no stable head support),
needs help in all self-care domains.
Resettlement:
The process of returning the patient to the most appropriate social situation.
Disable resettlemet office ( DRO):
Responsible for place the disable person in a suitable social work( if necessary after
employment rehabilitation or vocational training).
DRO main function:
1- It act as intermediary between industry and client.
2- Act as employment adviser to the disabled person.
3- Advice the clinical and social team about the possibility and suitability of employment
for the patient.
Resettling a disable patient on work depend on many factors:
1- Severity of the disability.
2- Age of the patient.

8
3- Education and conjugal back ground of the patient.
4- Nature of the work.
5- Social and economic factors.
6- Time elapse from onset of disability till definite plans to return to work or training.
Physiotherapy techniques
Physiotherapy (physical therapy):
Is a health profession concerned with the assessment, diagnosis and treatment of disease
and disability through physical means.
Role of physiotherapy:
1. It provides psychological support for the patient in depression.
2. It is useful in treating psychosomatic conditions.
3. It helps in treating deformities and making them functionally independent.
4. It plays a role in treating neuromuscular disorders.
5. It improves the walking abilities.
6. It relieves the pain, spasm…. etc.
Principle of treatment:
1. To relieve pain and spasm.
2. To increase joint range of motion.
3. To reduce the stiffness or contractures.
4. To improve muscle power.
5. To prevent deformities.
6. To relieve spasticity.
7. To remove the secretions from the lungs.
8. To improve the breathing capacity.
9. To improve the aerobic capacity.
10. Improve gait pattern …. etc.
9
Classification:
Heat therapy(superficial and deep).
Cold and ice therapy.
Hydrotherapy.
Electrotherapy (Gelvanic and Faradic stimulation).
Spinal traction.
Physical exercise.
Orthoses & other aids & devices.
Prostheses.
Education & training.
Invasive techniques.
Superficial Heat Therapy (HT):
• It’s a passive procedure of physical treatment.
• It can be done by two way:
1) Changing the heat of the environment.
2) Applying the heat to the skin (wax bath, electrical lump, hot pack, heat lump).
Time is 3-30 minutes, Its wiser to observe the thermal sensitivity of the skin (otherwise
it may be burn), It can be used effectively at home.
Indications
Painful conditions : muscle spasm ,tension myalgia, chronic stage of tendinitis & bursitis.
To reduce joint stiffness & improve range of movement(ROM).
Physical treatment of contracture.
Induction of reflex vasodilatation.
precautions & contraindications
1) Acute inflammation, trauma or hemorrhage.

11
2) Bleeding disorders e.g. hemophilia.
3) Insensitive skin e.g. complete spinal cord injury.
4) Inability to communicate or respond to pain.
5) Malignancy.
6) Ischemia.
7) Edema.
8) Atrophic skin.
9) Scar tissue.
10) Poor thermal regulation.
Wax-bath:
Wax is melt at 130°F(45-50°C),and remain liquid at 120°F , Its heated by thermostatically
controlled tanks. Dipping the affected part 10 time in it, so there is 6-7 coating of wax, the
hand remains covered by wax for 20 min.The wax easily peeled off after a treatment period,
Its useful for arthritis and hand injury, It follows by active exercise to mobilize stiff
finger.
Deep Heat therapy
Ultrasound (U.S.).
Short wave diathermy (SWD).
Microwave diathermy (MWD).
Ultrasound
Its effect by mechanical, chemical and heating effect,It applied in contact with the patient
body, It can be repeated daily, twice-three time weekly, it used easily, safe, not expensive,
treated for few min.(5-10 min.), no burn caused by it.
Indications:
1. Acute sprain and strain.
2. Ligament infl., tenosynovitis.

11
3. Scaring after burn.
4. Fibrosis ( duputeryn contracture).
5. Traumatic athletic injury.
6. Chondromalacia patellae.
Contra indication:
1. Malignancy and benign tumor.
2. Previous irradiated skin.
3. Avoid in: fluid filled cavities (e.g. eyes & gravid uterus), heart , brain , testes.
4. Acute infection.
5. Hemophilia.
6. Pregnancy.
Short wave diathermy (SWD):
Its depth of penetration is half body, Application time 15- 30 minutes,Its heating effect is
produced by putting the patient with in electrical field, Patient should be on a non conductive
table, Its impossible to measure the input on the patient, so only observe the skin sensation of
patient (it may cause burn),It relief joint pain.
Contra indication:
1) Malignancy.
2) Acute infection and inflammation.
3) Venous thrombosis and arterial insuffiency.
4) Hemorrhage.
5) Loss of skin sensation.
6) Metal in tissue.
7) Cardiac pace maker.

12
Microwave diathermy (MWD):
It is an Electro magnetic radiation, commonly used for small joints & superficial muscles,
Application time is 15-30 minutes.
Contra indication:
avoiding active or acute inflammatory and infective site.
Children are better avoided.
Precaution on edematous tissue and fluid filled cavity.
Protective glasses (goggles) are used by the patient & therapist because MWD can cause
cataract.
Skin loss of sensation.
Hemorrhage.
Malignancy.
Cold (cryo-) therapy :
Application time 20 minutes & repeated few to several time / day. It includes:
Ice packs, Cold water sacs, Whirl pools.
Indications:
1) Acute skeletal trauma.
2) Chronic Skeletal pain .
3) Exercising spastic muscle.
Precautions & contraindications:
1) Ischemia ( even distant exposure ).
2) Reynaud’s phenomenon.
3) Unhealed wound.
Hydrotherapy: Use of water (specially warm water ) in treatment of a disease, Total body
or part of it is treated in water.

13
Effect of hydrotherapy:
1) Increase of peripheral circulation (at 96°F).
2) Relief pain , muscle spasm, joint stiffness, decrease sensitivity of muscle spindle
to stretching.
3) Buoyancy of water decrease body weight to 10% and this is utilized in walking
and standing.
4) Hydrostatic pressure is the force acting on body surface (by the water)=40.7 pound
\inches, and it increaseed by 0.86 pound for each 2 feet depth. This Pressure is sufficient
to support the body in standing.
5) Dynamic pressure: is resistance which body encounter in moving in water, it depending
on size of moving part and its speed.
Indications:
1. Muscle weakness (poliomyelitis).
2. Amputation to strength the stamp.
3. Hemiplegia, cerebral palsy.
4. Spinal cord injury.
5. RA , OA.
6. Ankylosing spondylitis.
7. After joint injury.
Contra indication:
1. Pop.
2. Infection and inflammation.
3. Incontinence.
4. Opened wound.
5. Cardiac and respiratory diseases.

14
Light therapy:
Infra-red therapy:
It emit electromagnetic wave travel through air and penetrate skin and S C T, causing
peripheral vasodilatation, It applied from special distance from the body for 10-30 min.,It
relief pain and muscle spasm,It gives relax and rest for patient before the next part of
treatment.
Contra indication:
1) Loss of skin sensation.
2) Skin disease.
3) Vascular insuffiency.
4) Hemorrhage.
Electrotherapy:
Is the therapeutic use of electricity to stimulate nerve, muscle or both using surface
electrodes.
Biological effects :
Increase muscle strength.
Retard muscle atrophy.
pain relief.
Enhance wound healing.
Enhance osteo -genesis.
Electrotherapy:
Contraindications:
Circulatory impairment & dysrhythmia.
Over carotid sinus.
Across the heart specially over a demand pace maker.
Pregnancy.
Epilepsy.

15
Fresh fracture.
Active hemorrhage.
Muscles which are peripherally denervated (avoid neuro-muscular electrical stimulation).
Spinal traction:
Traction is pulling.
Generally limited to cervical & lumber (pelvic) traction.
It has an elongation (separation) effect.
CT-scan study during traction of disc herniation showed size reduction or
disappearance of prolapsed disc during traction.
Spinal traction-common methods:
Mechanical (pulley system ).
• Continuous traction : for 24 hr. and more if pain is severe( small wt.).
• Intermittent: traction is applied and removed alternatively ( using more weight).
• Sustained traction: for 20-30 min.
Spinal traction- application:
• Enhance muscle relaxation by superficial heat before or during traction.
• Starting with lower force.
Recommended force:
Cervical: 10% of body weight.
Lumber : 35 -50 % of body weight.
Position :
Cervical: sitting ,flexed neck to 20-30 degree.
Lumber : supine with flexed hips.
Session time : about 20 min. repeated 3-4 times / week.

16
Evaluation: during & after the course & if symptoms worsen.
Indication: Disc herniation with or without root symptoms.
Precautions:
1) lack of experience therapist.
2) Sever O.A.
3) Suspicion of local malignancy.
4) Significant Osteopenia.
5) Acute soft tissue injury .
6) Old age .
7) Congenital spinal deformity.
8) Cardiovascular disease.
contraindications:
cervical traction :
1 – Cervical instability (R.A. ,sever O.A. ,hyper mobility).
2- Carotid & vertebrobasilar insufficiency.
For lumber traction :
1 - Pregnancy.
2 - Sever spinal canal compression.
3- Inability to stabilize chest(sever cardio-respirator disease).
4- Active peptic ulcer , aortic aneurysm ,hiatal & other hernias (making pelvic brace
difficult).
5 - Spondylolisthesis.

17
Rehabilitation
Management techniques
Physical Exercises:
Performance of planned physical movements, postures or activities intended to enable the
person to:
Remediate or prevent impairment.
Enhance function.
Reduce risk.
Improve overall health.
Enhance fitness & wellbeing.
Biology effect of active exercise: It includes:
Increased oxygen demand, increase rate & depth of respiration.
Increased heart rate.
Increased B.P. (heavy exercise).
Decreased insulin secretion &increased glucagon secretion to maintain blood sugar level.
Increased catecholamine secretion.
Fatigue & muscle soreness if ability is exceeded.
The beginning & the end:
Sudden vigorous exercise may cause ECG abnormalities & syncope. Therefore a warm-up
period is needed, Abrupt cessation of active rhythmic exercise may cause a sudden drop in
B.P., hence a cool-down period is needed.
Practical therapeutic classification:
Mobility exercises.
Range of motion exercises.
Stretching exercises.

18
Resistance exercises.
Isometric (static) resistance exercise.
Dynamic resistance exercise.
Cardio pulmonary endurance exercises.
Aerobic.
Anaerobic.
Motor coordination & skill exercises.
Benefits of ROM exercises:
• Maintaining joint mobility
• Nutrition to a joint
• Prevention of tissue adhesion & contracture
Contraindications to ROM exercises:
Shortly after acute tears & surgery.
Acute local inflammation.
A serious precluding illness.
Stretching exercises:
Usually passive. Can be done by the other hand, as assistant or by a mechanical device.
Used to overcome adhesions or contractures, e.g. in shoulder adhesive capsulitis
and joint flexion deformities.
Contraindications to stretching exercises:
Bony obstacle.
Recent & local inflammation or infection.
Active healing process.

19
Risk of stretch rupture (e.g. rotator cuff in old diabetics),
Bone fragility.
Resistance exercises:
It is any active exercise when a dynamic or static (isometric) muscle contraction is
resisted by an outside force applied manually or mechanically.
Types:
Isometric (static) resisted exercise.
Dynamic resisted exercise.
They have few long term cardiovascular effects. There is a little or no change in resting:
heart rate, B.P., stroke volume & myocardial oxygen consumption.
Isometric (static) resistance exercise:
General features:
• Tension is generated in the muscle without visible joint movement or appreciable change
in muscle length. It can also be done against no resistance.
• It does not cause muscle hypertrophy.
• Is less effective than dynamic exercise in developing muscle endurance.
• In cardiac patients they can cause arrhythmias & B.P. increase during exercise.
Uses of isometric resistance exercises:
To prevent or minimize muscle atrophy due to external immobilization (splints, casts,
traction……..).
To activate muscles while protecting tissue healing.
To improve muscle strength when dynamic exercise is not advisable.
To develop static muscle strength at particular points in the ROM consistent with specific
task needs.

21
Dynamic resistance exercises:
It is a muscle contraction causing joint movement it can be:
Concentric: muscle excrusion & shortening e.g. lifting a load.
Eccentric: muscle lengthening under tension e.g. lowering a load.
Is the most effective to improve muscle performance & functional abilities.
Orthoses, aids & devices:
is an external device applied to body part for a preventive or therapeutic purpose.
Aims (uses) of orthoses:
Restriction of activity.
Protection or stabilization.
Correct flexible deformities.
Prevent progression of deformities.
Load transfer.
Improve function.
Orthoses criteria:
1) Gains acceptance regarding:
Comfort (e.g. weight, size, tightness……etc).
Function.
Appearance.
1) Reasonable durability.
2) Easy maintenance.
3) Easy to don & off correctly.
4) Adjustable.
5) Low risk.

21
Orthoses structure:
Metal:
Stainless steel: common for lower limbs.
Aluminum alloys: common for upper limbs.
Titanium: very light weight & corrosion resistant. Desirable though more expensive.
Plastic:
Thermo setting plastics: develop permanent shape when heated & pressure is applied (can
not be softened when reheated).
Thermoplastics (thermoforming): soften & moldable when heated & harden when cooled.
Others: leather, fabrics, rubber…….etc.
Prostheses:
An artificial substitute for a missing body part.
Aims of a prosthesis:
Functional: as usual in artificial legs.
Cosmetic: e.g. artificial eye ball & where ever the patient is not a functional candidate.
In young children a prosthesis is often necessary to maintain normal development.
Temporary prosthesis is sometimes used for the initial training evaluation (usually a socket
design to accept full weight bearing).
Prostheses Criteria:
Reasonable durability.
Light weight.
Adjustable.
Easy maintenance.
Easy to don & doff correctly.
Acceptable functionally &/or cosmetically.
