1
Fifth stage
Medicine
Lec-8
د . منوع
1/1/2014
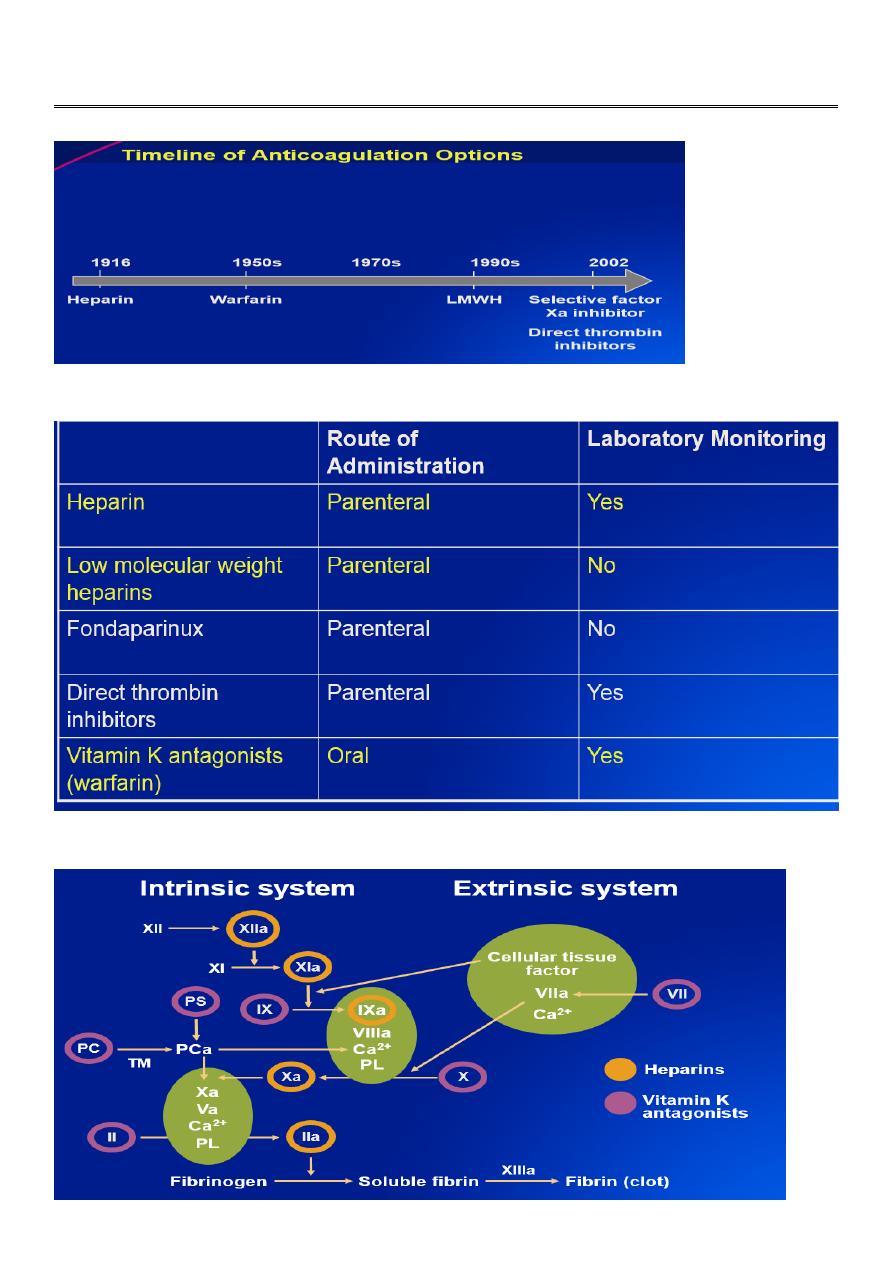
Current Anticoagulants
Current antithrombotic agents: multi-targeted
2
Advantages of LMWH (low molecular weight heparin) over UFH
(unfractionated heparin)
Better bioavailability and predictable pharmacokinetics
VTE treatment using weight-
based dosing with no need for laboratory monitoring
Longer half-life
twice or once daily subcutaneous dosing
Lower rate of heparin-induced thrombocytopenia
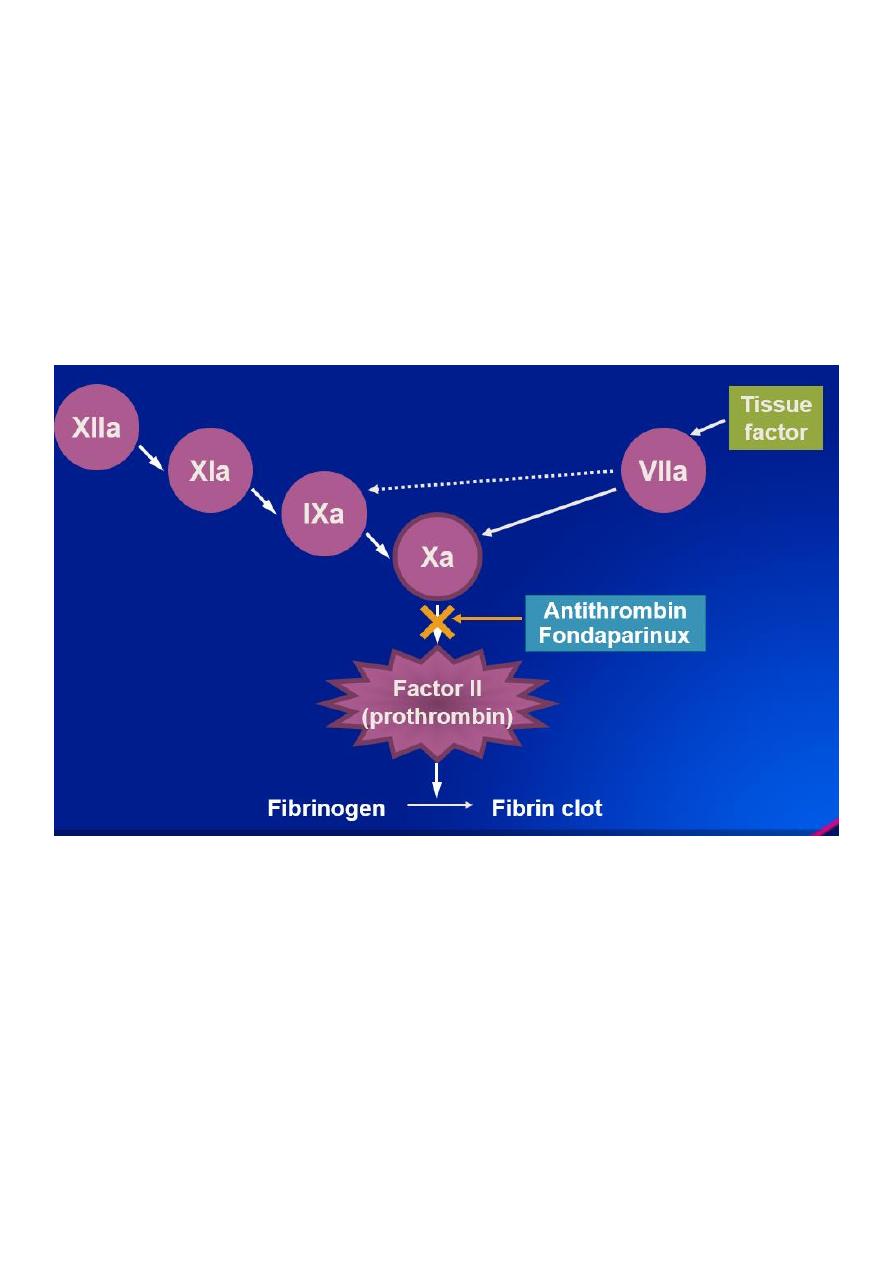
Selective Indirect Factor Xa inhibition
Fondaparinux
– Synthetic pentasaccharide
– Longer half-life than LMWH
– No laboratory monitoring required
– No reactivity with HIT antibodies
– Approved for prophylaxis of VTE following major orthopedic and abdominal surgery and
for treatment of VTE
3
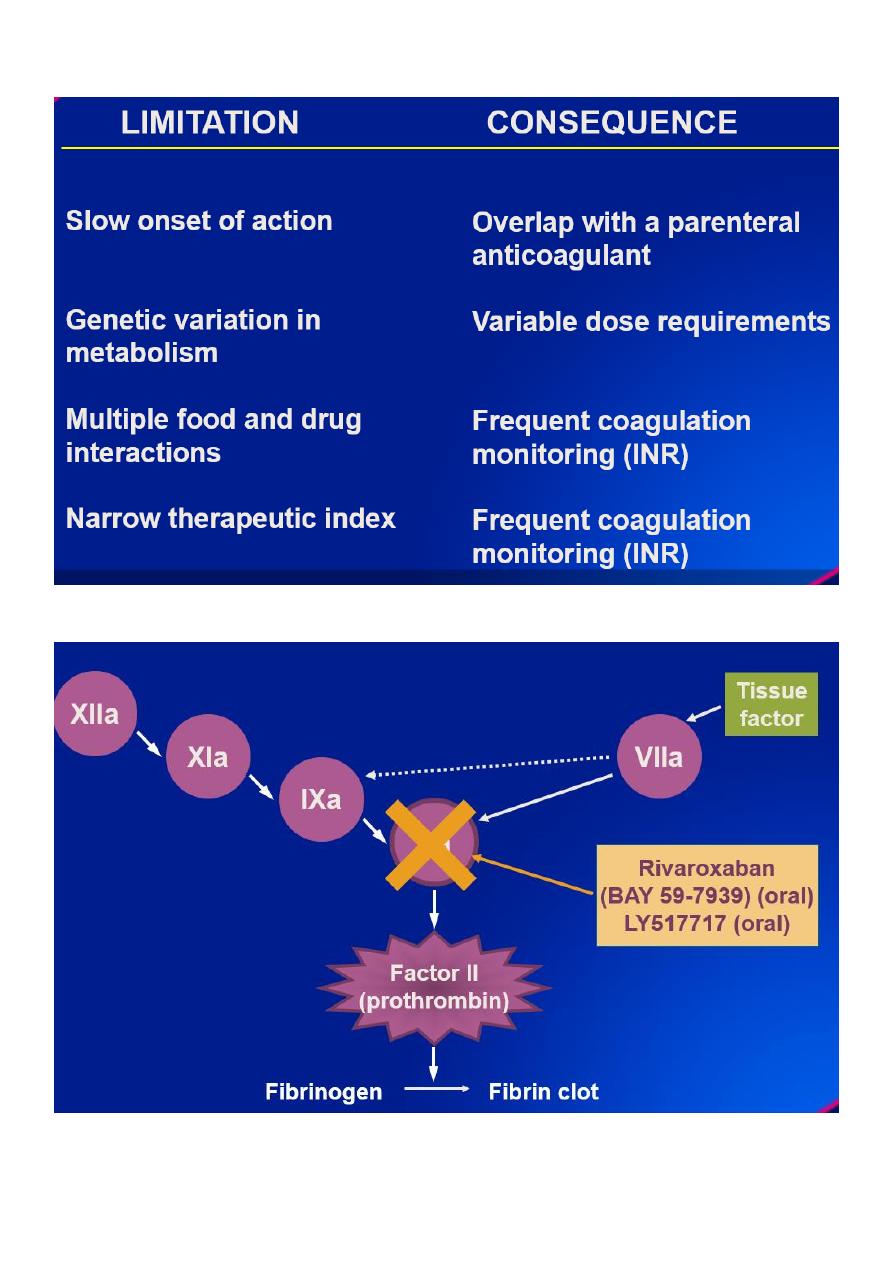
Limitations of Warfarin (Vitamin K Antagonists)
Direct Factor Xa Inhibition

4
Direct Thrombin Inhibition
Anticoagulant Treatment of Venous Thromboembolism
1.
Initial treatment with adequate doses of heparin is important.
2.
Warfarin can be initiated early.
3. Antithrombotic effect of warfarin requires reduction of
prothrombin levels: this effect requires at least 4 days
of treatment and the need for overlap with heparin.
4.
DVT can be treated at home with LMWH/fondaparinux.
5.
Unprovoked (“idiopathic”) VTE is a chronic disease.
6.
What is the optimal duration of initial treatment? Which patients require long term
anticoagulant therapy and what should the INR intensity be?
5
The Importance of DVT Prophylaxis in Patients With Cancer
VTE is one of the leading causes of death in cancer patients, occurring in 4% to 20% of
patients
Hospitalized patients with cancer and cancer patients receiving active therapy are at
greatest risk for VTE
– Cancer increased the risk of VTE 4.1-fold
– Chemotherapy increased the risk 6.5-fold
Major risk factors include older age, comorbid conditions, recent surgery or
hospitalization, active chemotherapy or hormonal therapy
All hospitalized cancer patients should be considered for prophylaxis
Patients with cancer undergoing surgery should be considered for prophylaxis
LMWH is the preferred drug
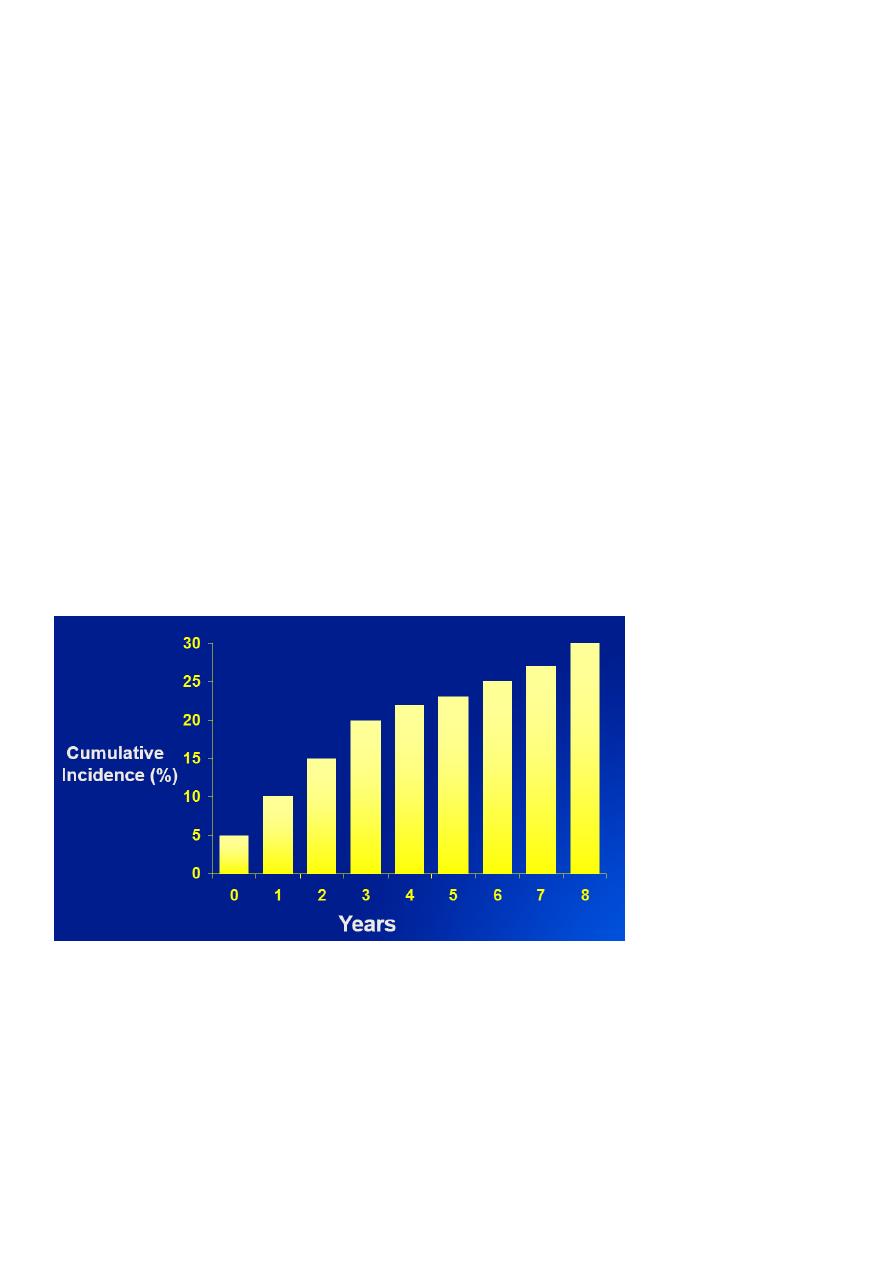
Recurrent Venous Thrombosis is Common Following a First Episode of
Symptomatic DVT
Duration of Anticoagulant Therapy
First event with reversible or time limited risk factor
– 3-6 months at INR 2-3
Unprovoked VTE, first or second event
– 6-12 months at INR 2-3, then consider indefinite anticoagulation at INR 2-3
weighing recurrence versus bleeding risk (? INR 1.5-2)

6
Special Situations - indefinite anticoagulation
– First event with
• Cancer until resolved (consider chronic LMWH)
• Antiphospholipid antibody syndrome
• Antithrombin deficiency or multiple genetic defects,
?deficiencies of protein C or protein S
ANTICOAGULANT DOSING
Subcutaneous Heparin Dosing for Treatment of Acute Venous
Thromboembolism
General Considerations
1. Round weight-based dose to nearest prefilled syringe size.
2. Consider monitoring anti-Xa heparin levels for weight >120 kg or <60 kg.
3. Repeat CBC day 7 to assess for heparin-induced thrombocytopenia.
a. If heparin exposed in prior 6 months, CBC on day 3.
4. LMWH not recommended if creatinine clearance (CrCl) <30 ml/min.
Dosing
Enoxaparin: 1 mg/kg every 12 hours or 1.5 mg/kg daily
For cancer patients and those at high bleeding or thrombosis
risk, favor twice-daily dosing
Dalteparin: 200 IU/kg daily
In cancer patients for long-term treatment: 200 IU/kg daily
for 4 weeks (cap at 18,000 IU), then:
a. <56kg: 7,500 IU daily
b. 57-68 kg: 10,000 IU daily e. >98 kg: 18,000 IU daily
c. 69-82 kg: 12,500 IU daily
d. 83-98 kg: 15,000 IU daily
Tinzaparin: 175 IU/kg daily
Fondaparinux: Daily dose: <50 kg: 5 mg. 50-100 kg: 7.5 mg. >100 kg:10 mg
7
Unfractionated heparin: 333 IU/kg x 1, then 250 IU/kg every 12 hours
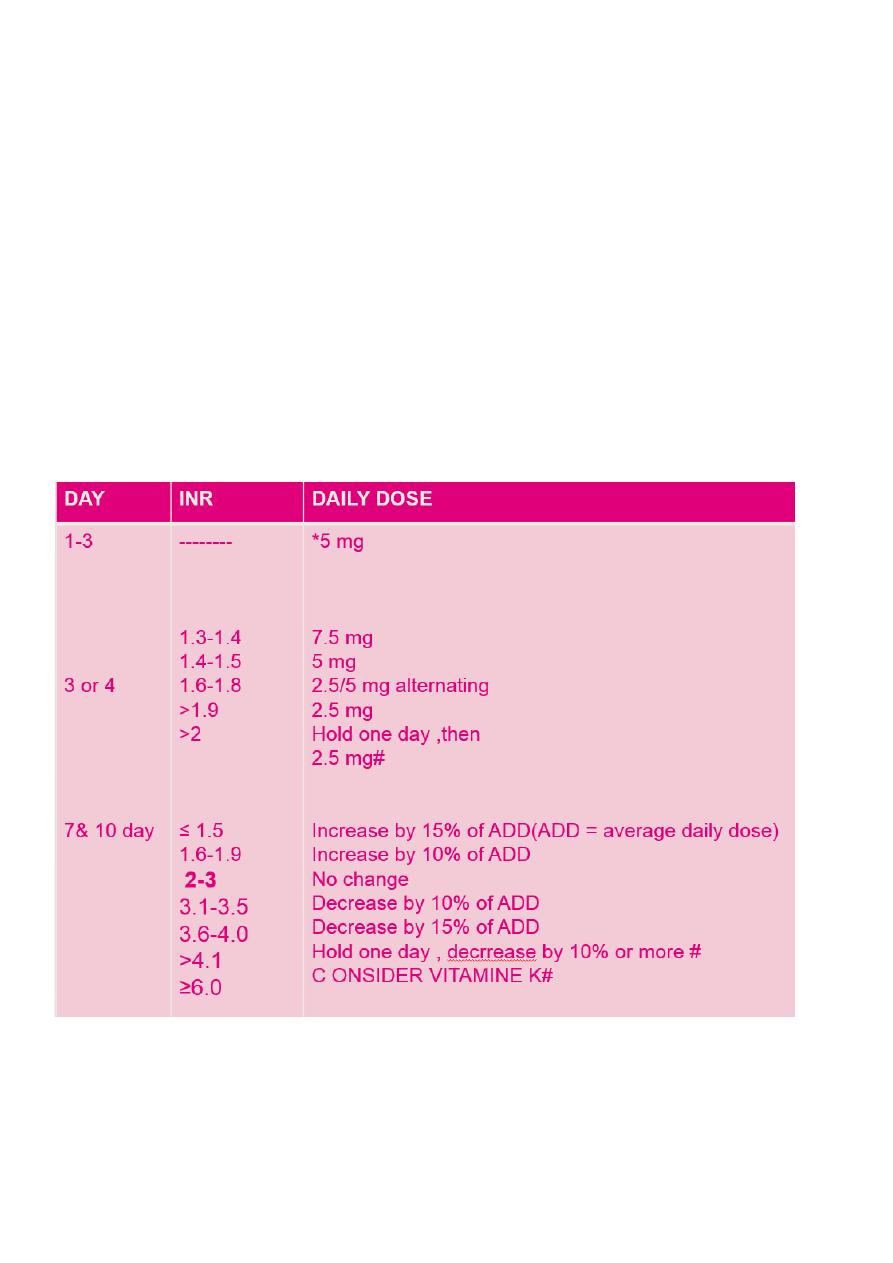
Initial Warfarin Dosing for Venous Thromboembolism or Atrial
Fibrillation in Ambulatory Outpatients, Target INR 2.0-3.0
General Considerations
1. Obtain baseline PT/INR and investigate if abnormal.
2. Determine use of potential warfarin interacting medications.
3. Document target INR and prescribed warfarin tablet strength.
4. Provide patient education on safety, monitoring, drug and food interactions.
5. For acute thrombosis, overlap with heparin/LMWH/fondaparinux for 5+
days until INR therapeutic.
6. Recommend first INR check on day 3-4.
Warfarin dosing (cont )
* 2.5 mg for frailty, liver disease, malnutrition, drugs that enhance warfarin activity, or
Asian
ethnicity; 5-7.5 mg for young healthy patients
#Check INR more frequently
8
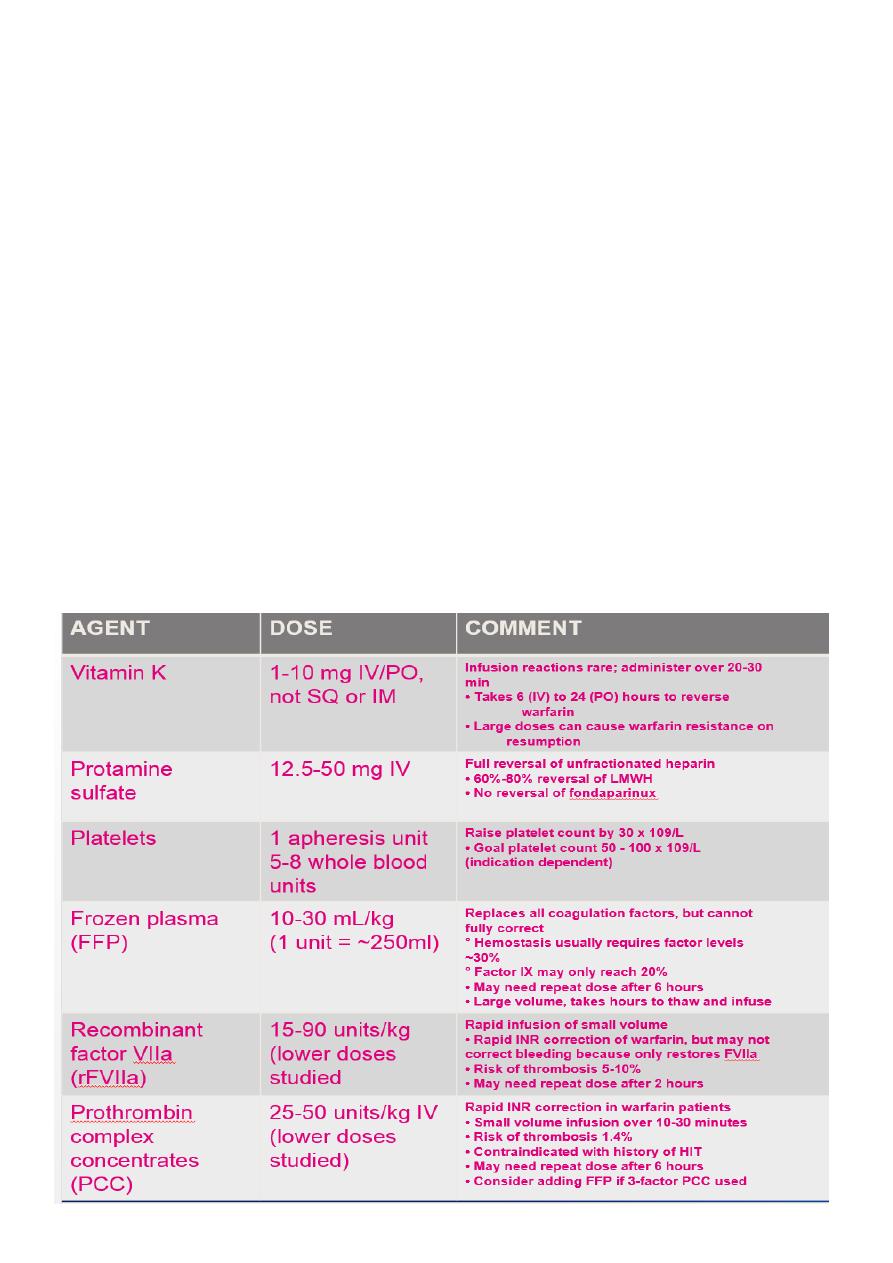
ANTICOAGULANT REVERSAL
A. General Principles of Management of Anticoagulant-Associated Bleeding
HASHTI
1. Hold further doses of anticoagulant
2. Consider Antidote
3. Supportive treatment: volume resuscitation, inotropes as needed
4. Local or surgical Hemostatic measures: topical agents (aminocaproic acid,
tranexamic acid)
5. Transfusion (red cells, platelets, FFP as indicated)
6. Investigate for bleeding source
Definitions Used for Reversal Situations
Non-urgent: Reversal is elective (procedures >7 days away)
Urgent (without bleeding): Reversal needed within hours
Urgent (with bleeding): Emergency reversal
9
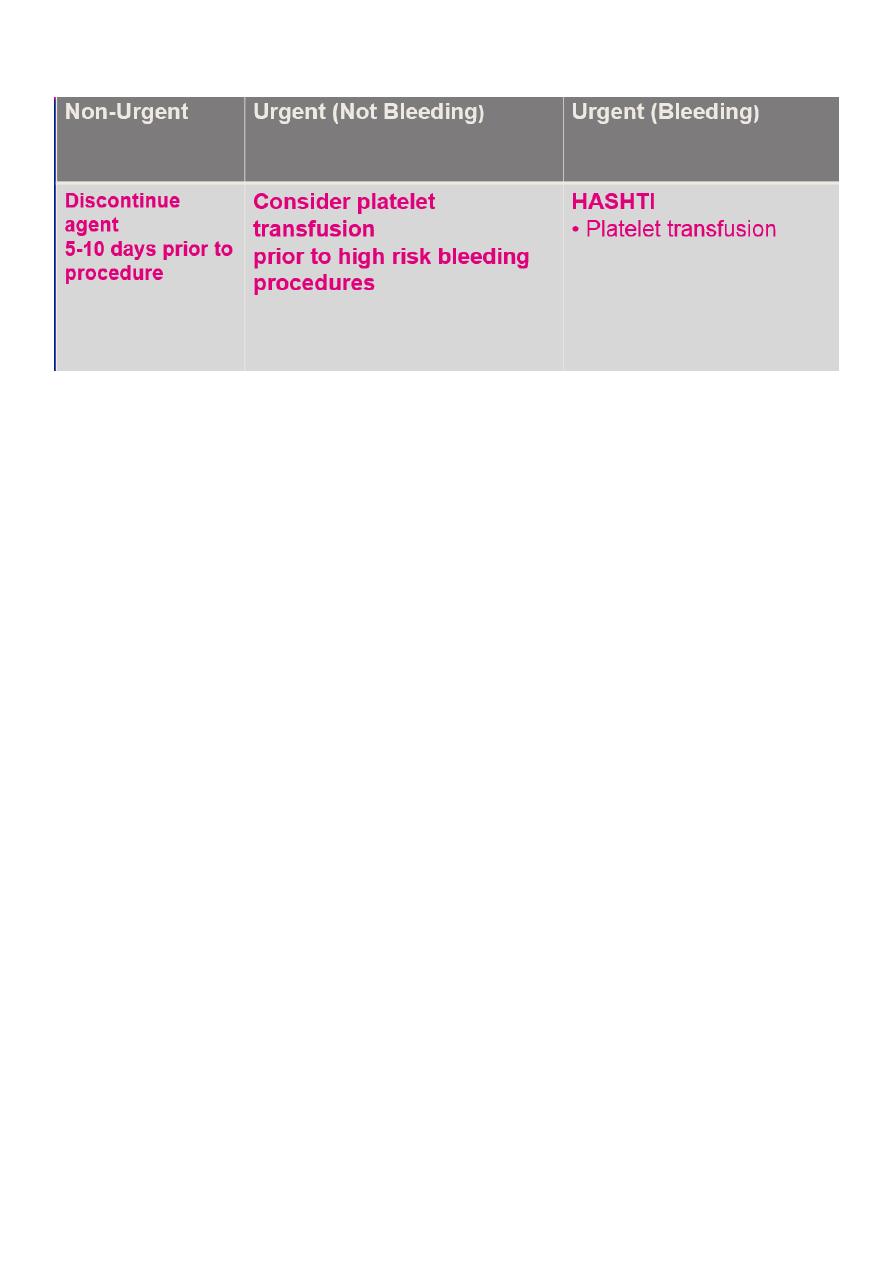
Reversal of Antiplatelet Agents
