1
Fifth stage
Medicine
Lec-7
د . منوع
1/1/2014
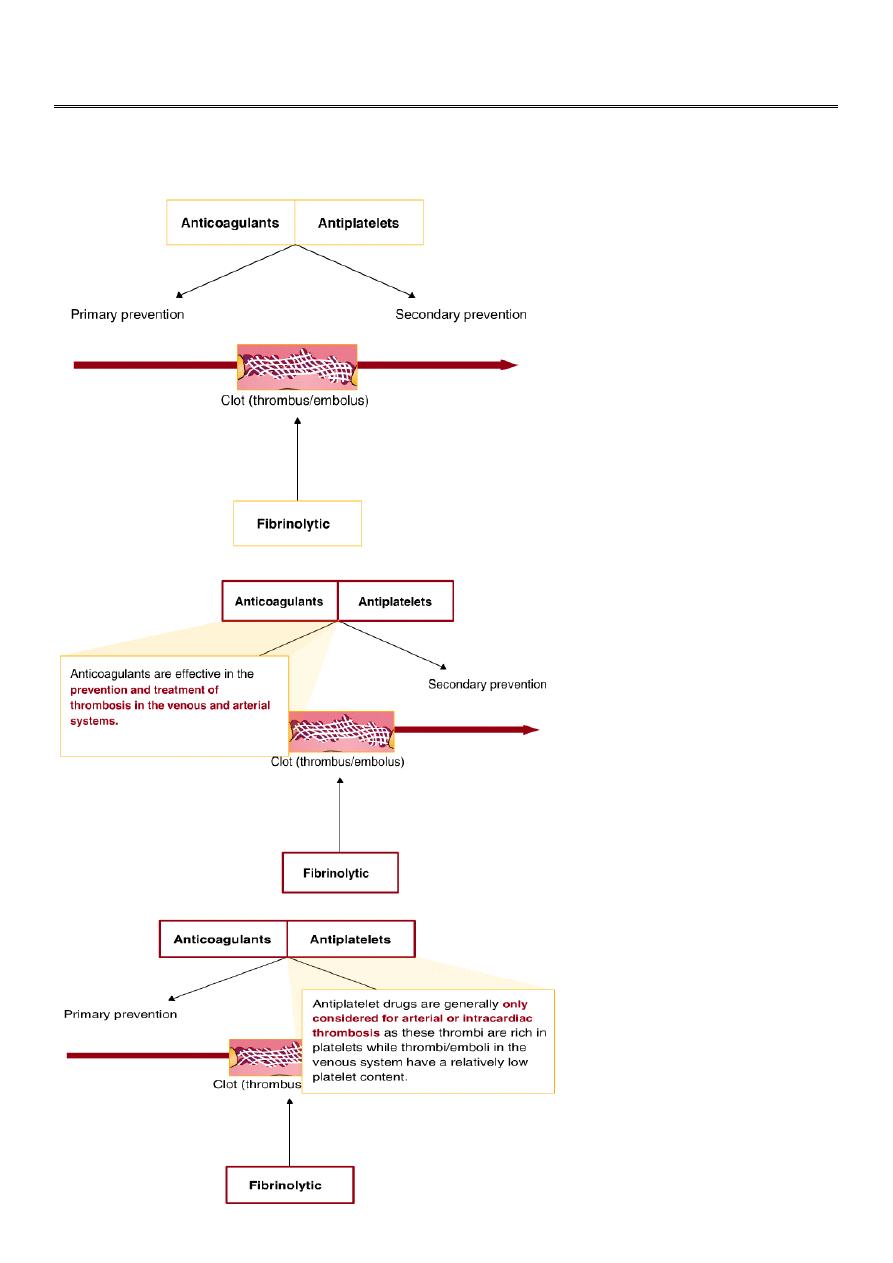
Antithrombotic drugs
2
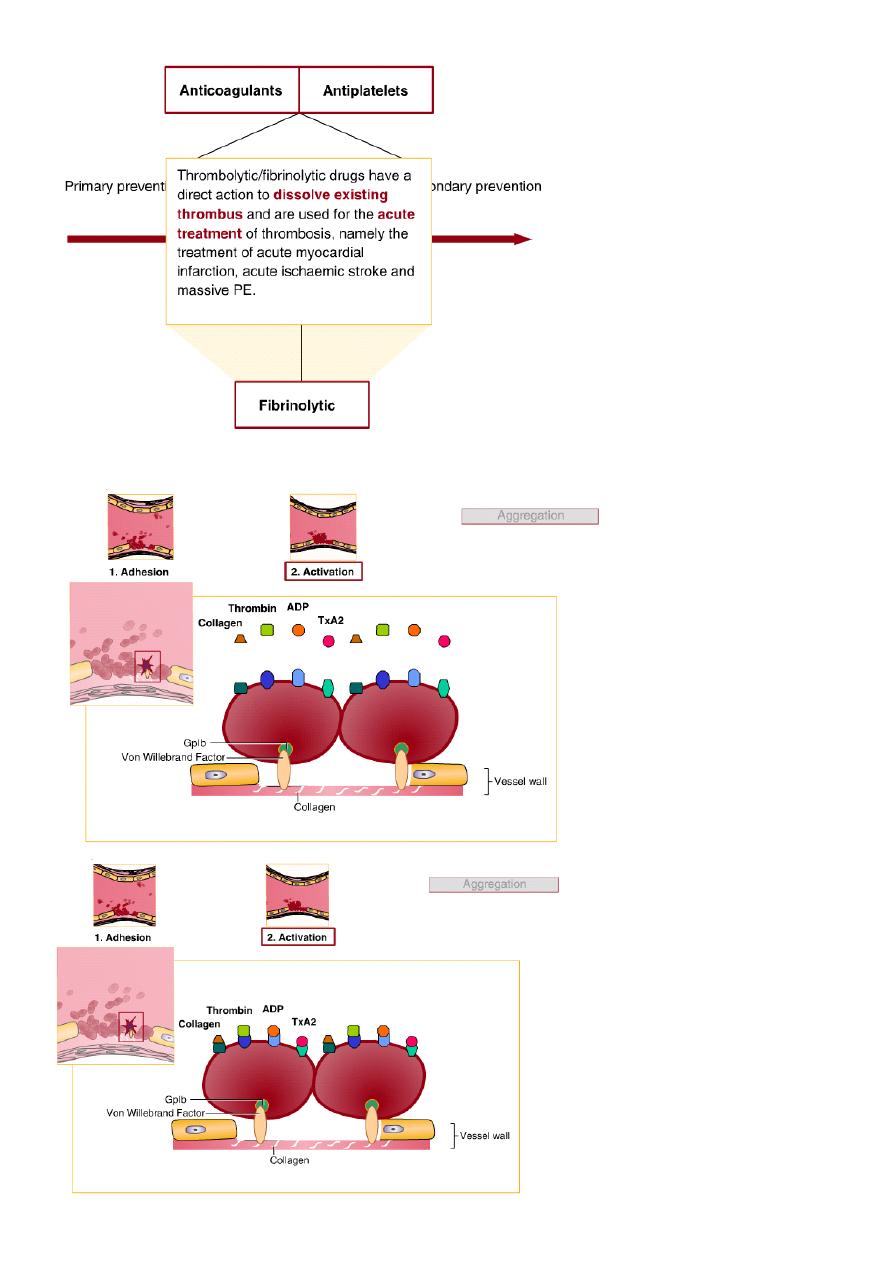
The role of platelets
3
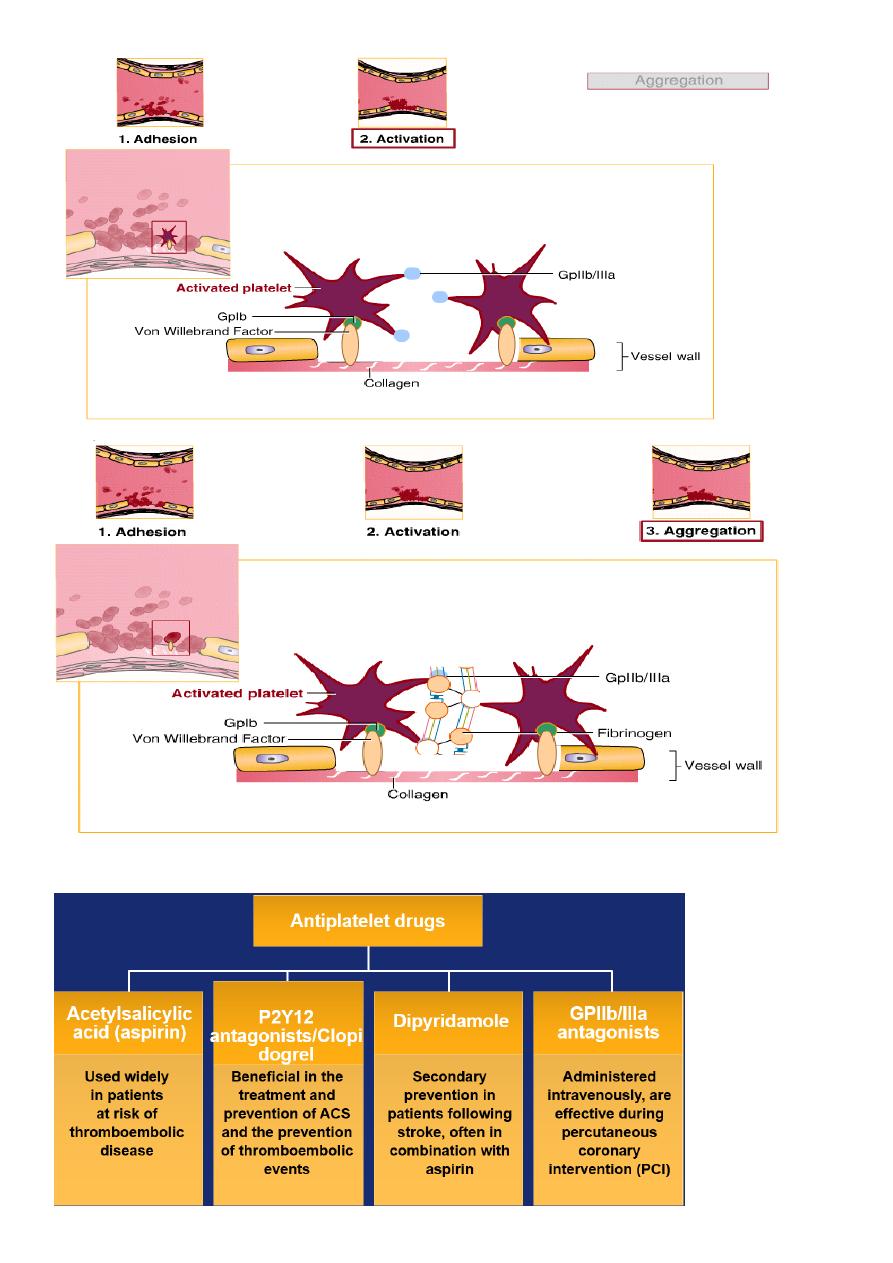
Antiplatelet drugs
4
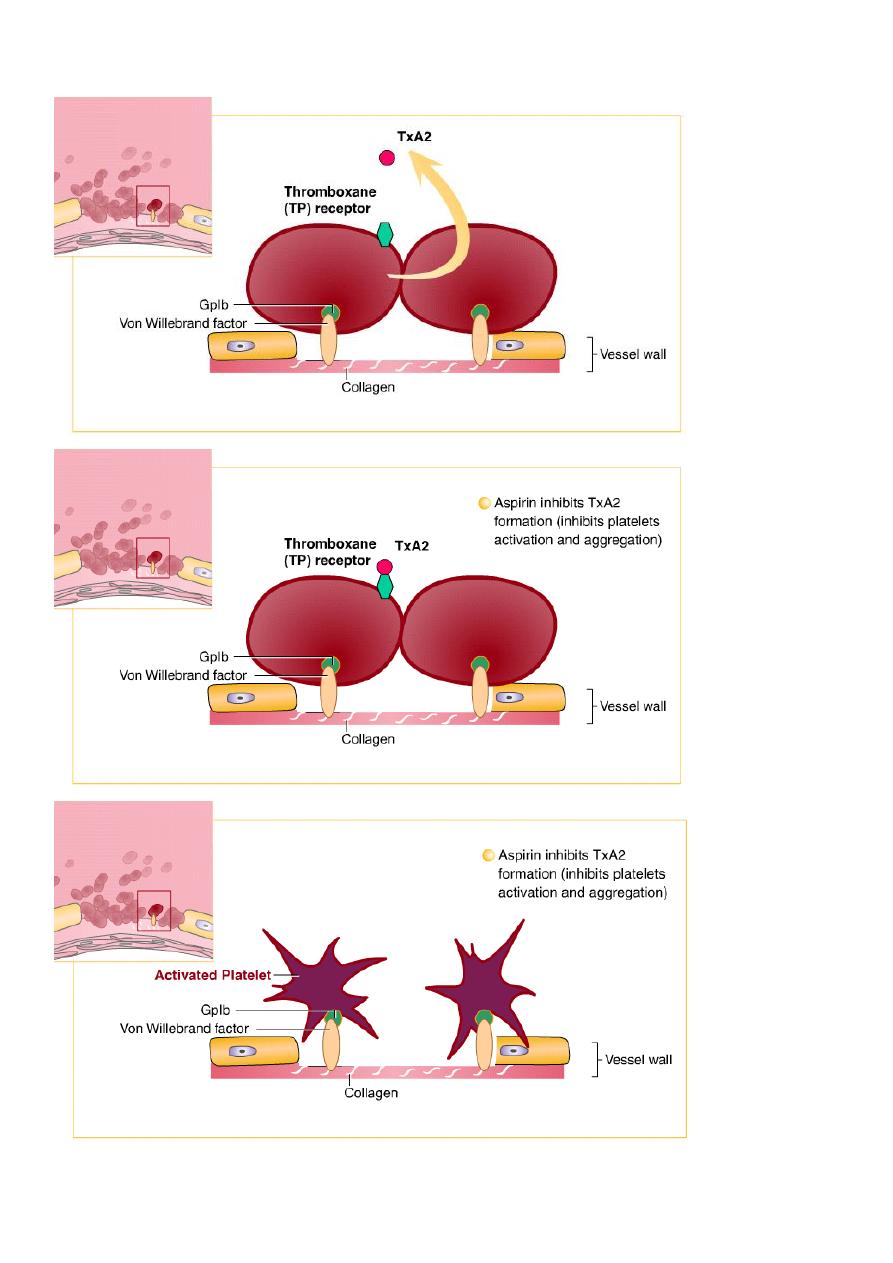
Acetylsalicylic acid – mechanism of action
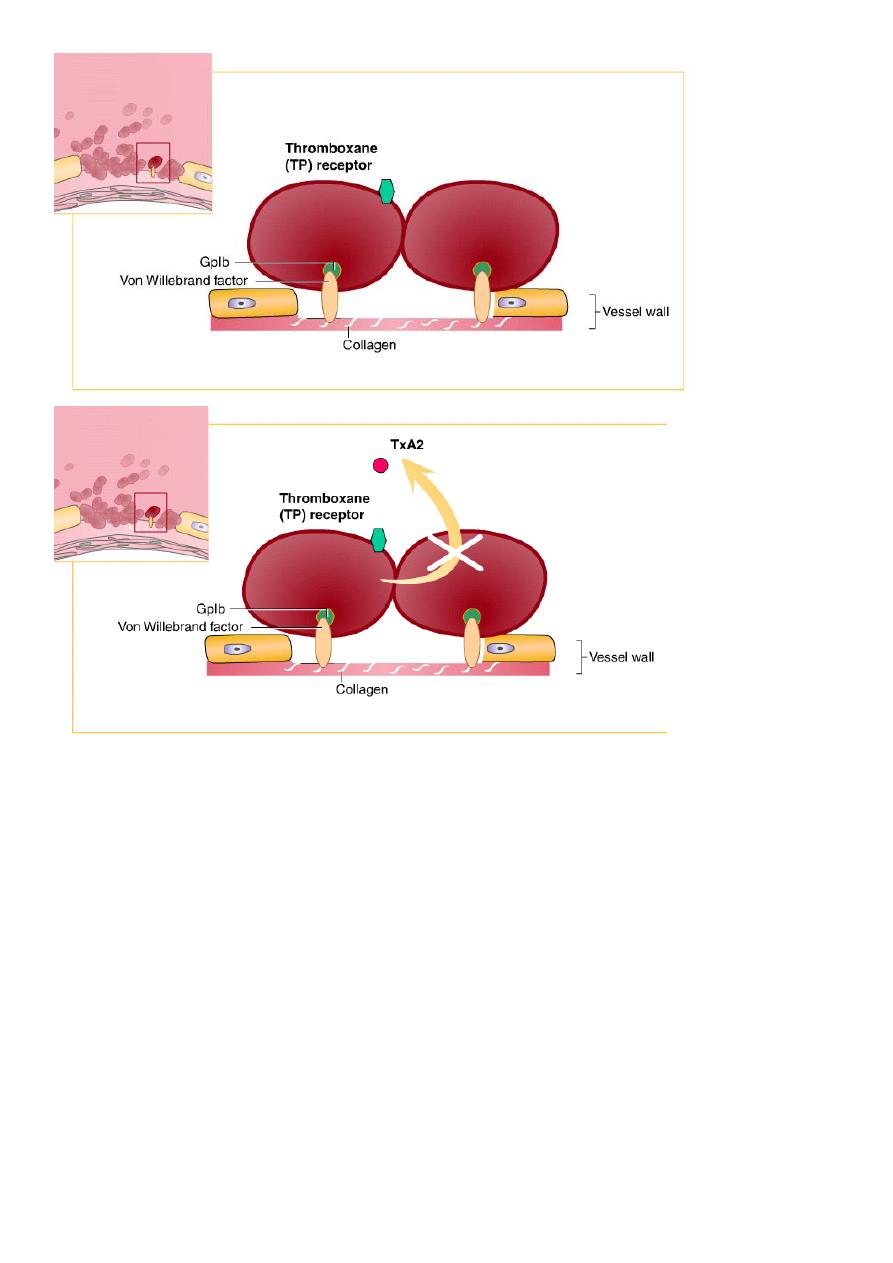
5
Acetylsalicylic acid – pharmacokinetics
Rapid absorption of aspirin occurs in the stomach and upper intestine, with the peak
plasma concentration being achieved 15-20 minutes after administration
The peak inhibitory effect on platelet aggregation is apparent approximately one hour
post-administration
Aspirin produces the irreversible inhibition of the enzyme cyclo-oxygenase and
therefore causes irreversible inhibition of platelets for the rest of their lifespan (7 days)
Acetylsalicylic acid – major use
Secondary prevention of transient ischaemic attack (TIA), ischaemic stroke and
myocardial infarction
Prevention of ischaemic events in patients with angina pectoris
Prevention of coronary artery bypass graft (CABG) occlusion
6
Acetylsalicylic acid – major drawbacks
Risk of gastrointestinal adverse events (ulceration and bleeding)
Allergic reactions
Is not a very effective antithrombotic drug but is widely used because of its ease of use
Lack of response in some patients (aspirin resistance)
The irreversible platelet inhibition
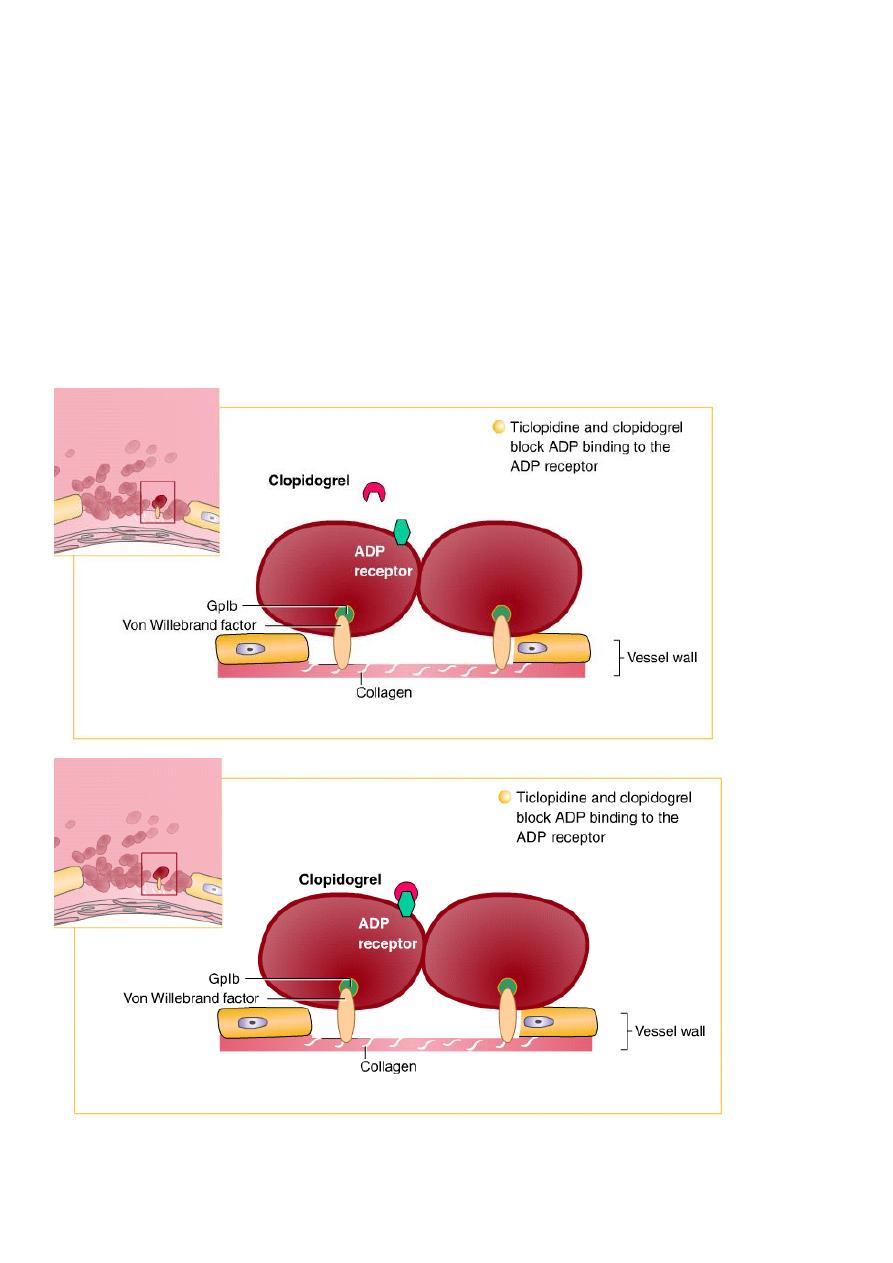
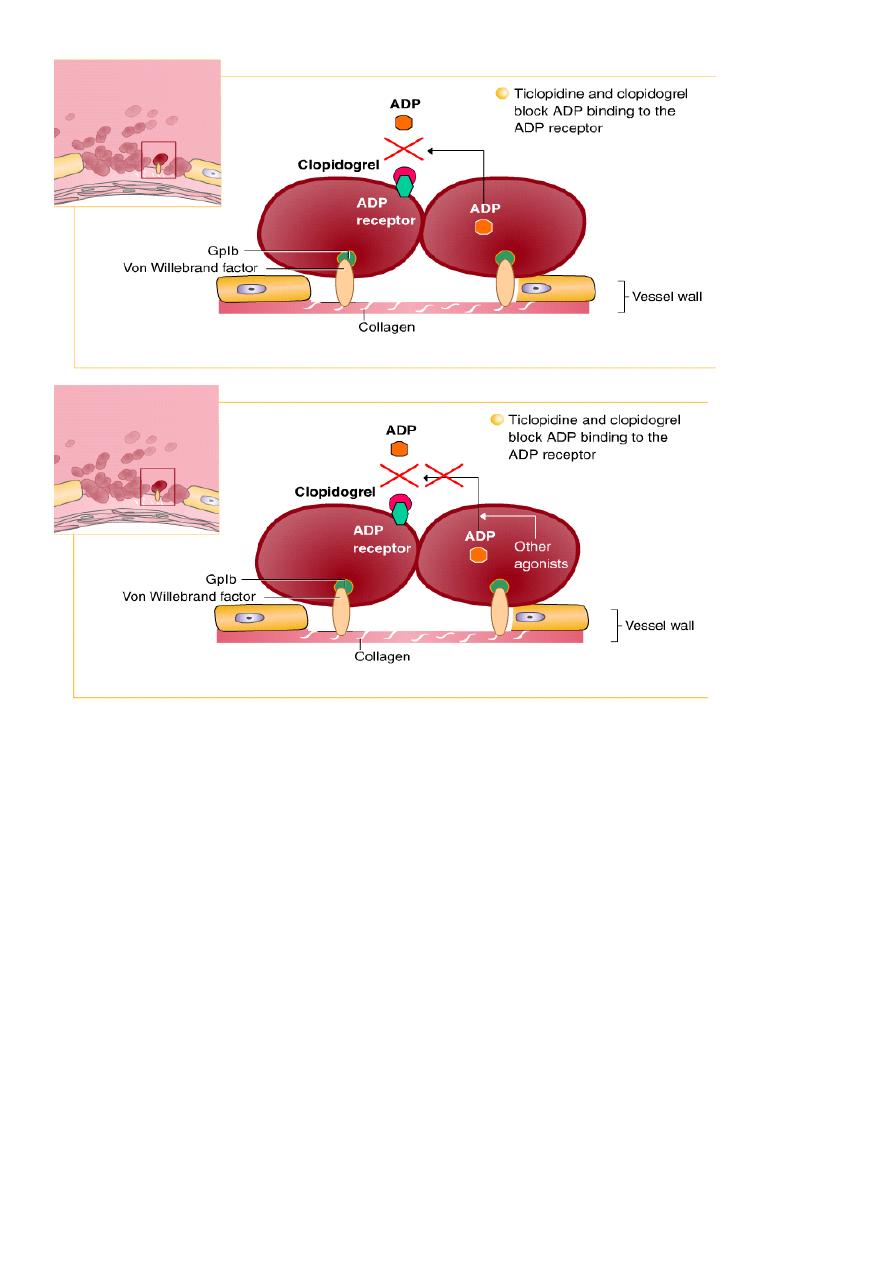
ADP-receptor antagonists – mechanism of action
7
ADP-receptor antagonists – pharmacokinetics
Both currently available ADP-receptor antagonists are thienopyridines that can be
administered orally, and absorption is approximately 80-90%
Thienopyridines are prodrugs that must be activated in the liver
ADP-receptor antagonists – major use
Secondary prevention of ischaemic complications after myocardial infarction, ischaemic
stroke and established peripheral arterial disease
Secondary prevention of ischaemic complications in patients with acute coronary
syndrome (ACS) without ST-segment elevation
ADP-receptor antagonists – major drawbacks
Clopidogrel is only slightly more effective than aspirin
As with aspirin, clopidogrel binds irreversibly to platelets
In some patients there is resistance to clopidogrel treatment
8
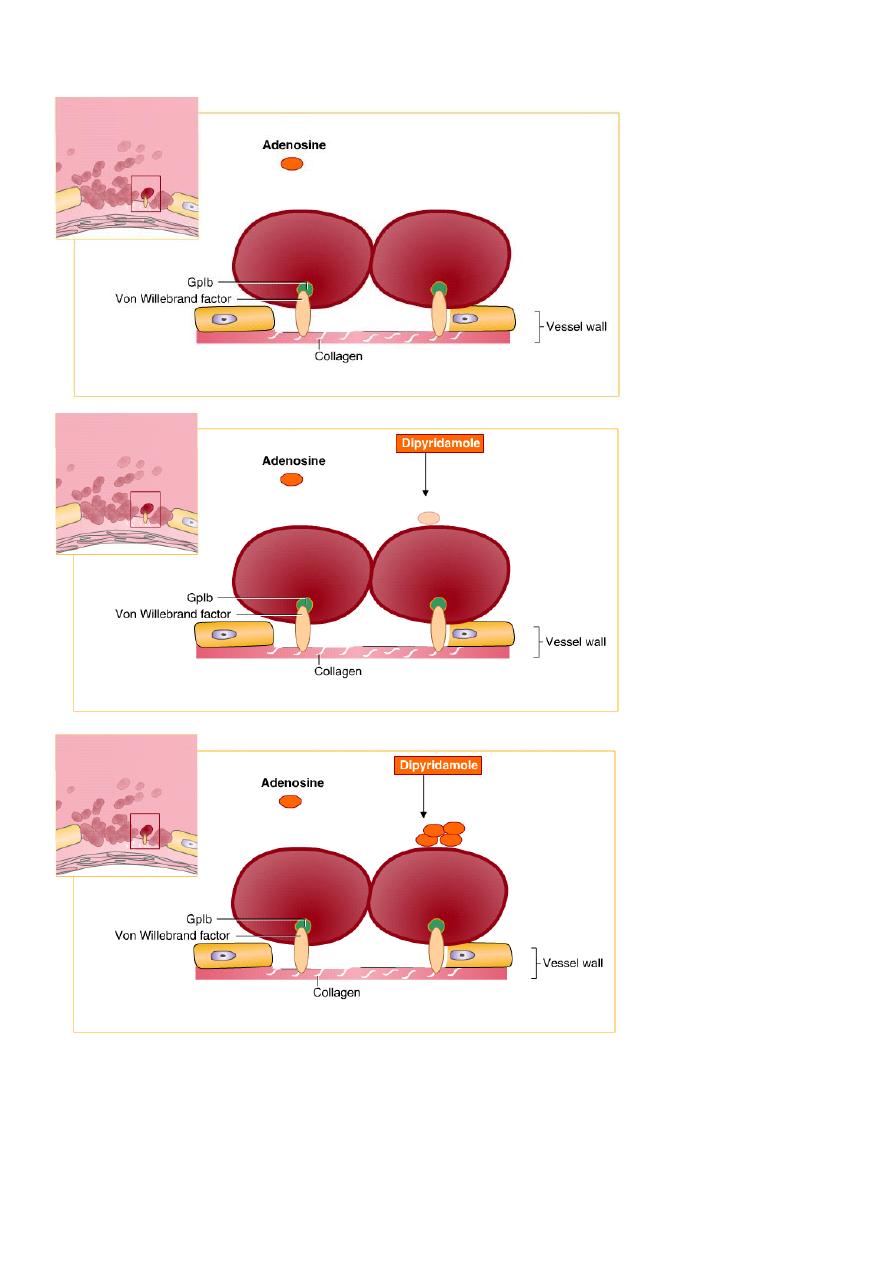
Dipyridamole – mechanism of action
Dipyridamole – pharmacokinetics
Incompletely absorbed from the gastrointestinal tract with peak plasma concentration
occuring about 75 minutes after oral administration
More than 90% bound to plasma proteins
9
A terminal half-life of 10 to 12 hours
Metabolised in the liver
Mainly excreted as glucuronides in the bile;
a small amount is excreted in the urine
Dipyridamole – major use
Secondary prevention of ischaemic complications after transient ischaemic attack (TIA)
or ischaemic stroke (in combination with aspirin)
Dipyridamole – major drawbacks
Is not a very effective antithrombotic drug
Dipyridamole also has a vasodilatory effect and should be used with caution in patients
with severe coronary artery disease; chest pain may be aggravated in patients with
underlying coronary artery disease who are receiving dipyridamole
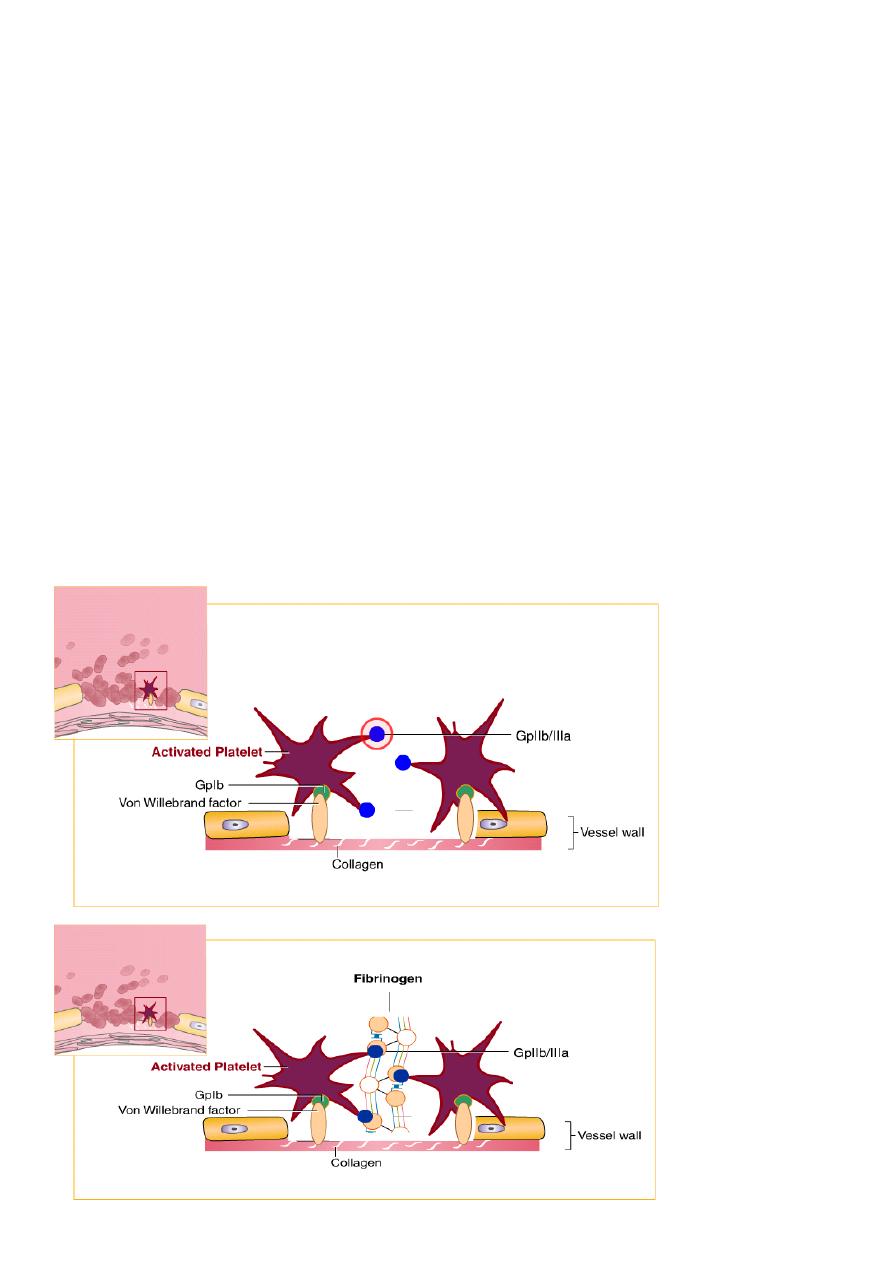
GPIIb/IIIa-receptor antagonists – mechanism of action
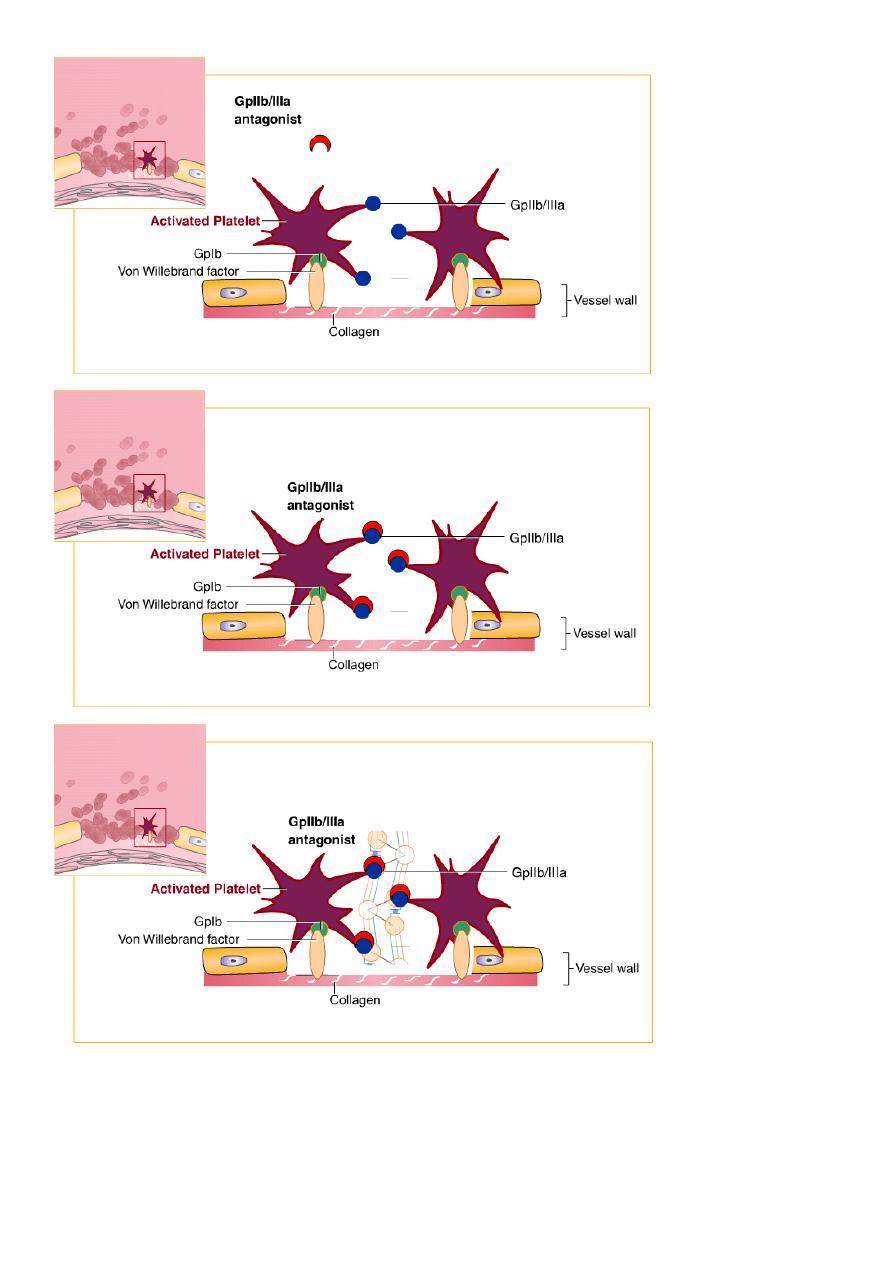
11
GPIIb/IIIa-receptor antagonists – pharmacokinetics
Available only for intravenous administration
Intravenous administration of a bolus dose followed by continuous infusion produces
constant free plasma concentration throughout the infusion. At the termination of the
11
infusion period, free plasma concentrations fall rapidly for approximately six hours then
decline at a slower rate. Platelet function generally recovers over the course of 48 hours,
although the GP IIb/IIIa antagonist remains in the circulation for 15 days or more in a
platelet-bound state
GPIIb/IIIa-receptor antagonists – major use
Prevention of ischaemic cardiac complications in patients with acute coronary syndrome
(ACS) without ST-elevation and during percutaneous coronary interventions (PCI), in
combination with aspirin and heparin
GPIIb/IIIa-receptor antagonists – major drawbacks
Can only be administered by intravenous injection or infusion and are complicated to
manufacture
Oral drugs have been investigated but were not effective and have therefore not
reached the market
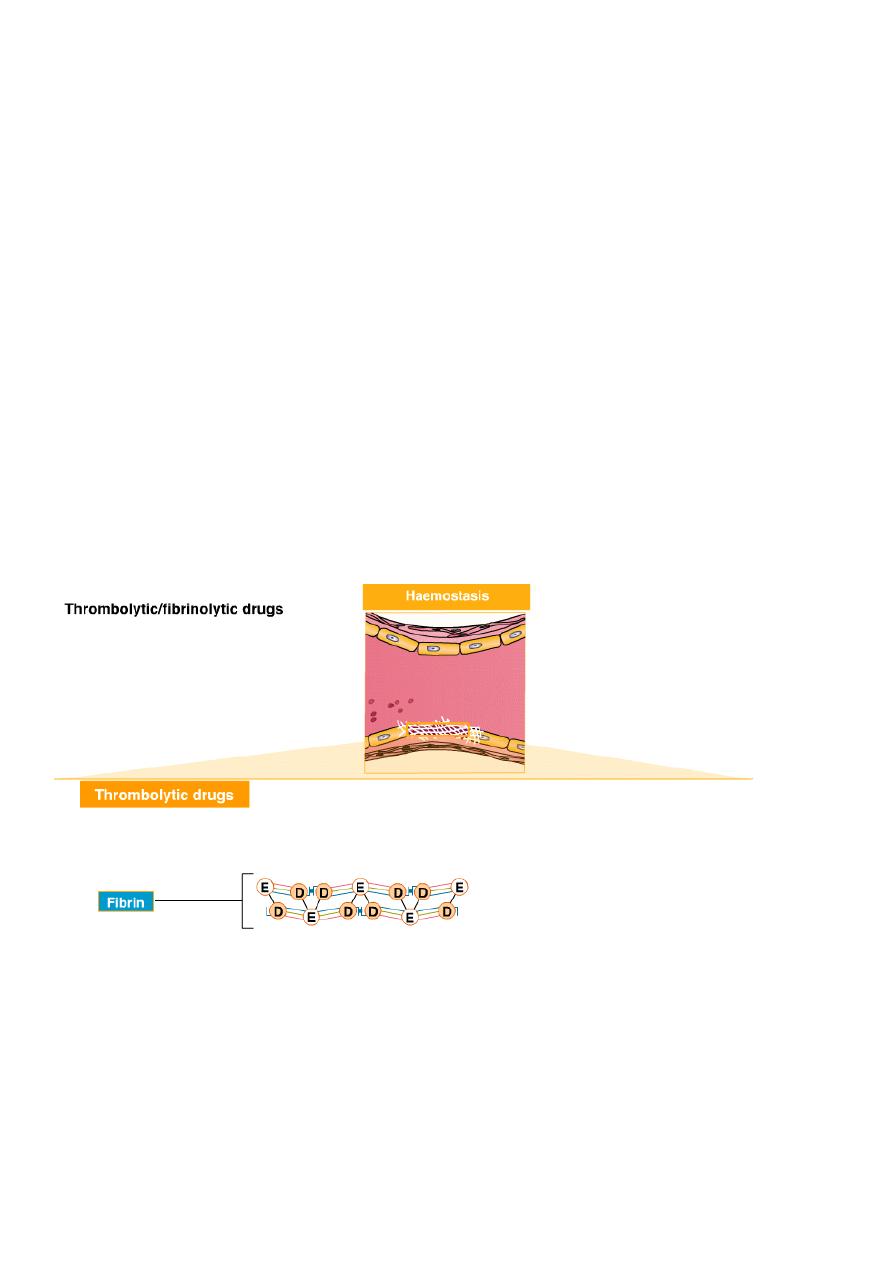
Thrombolytic drugs – mechanism of action
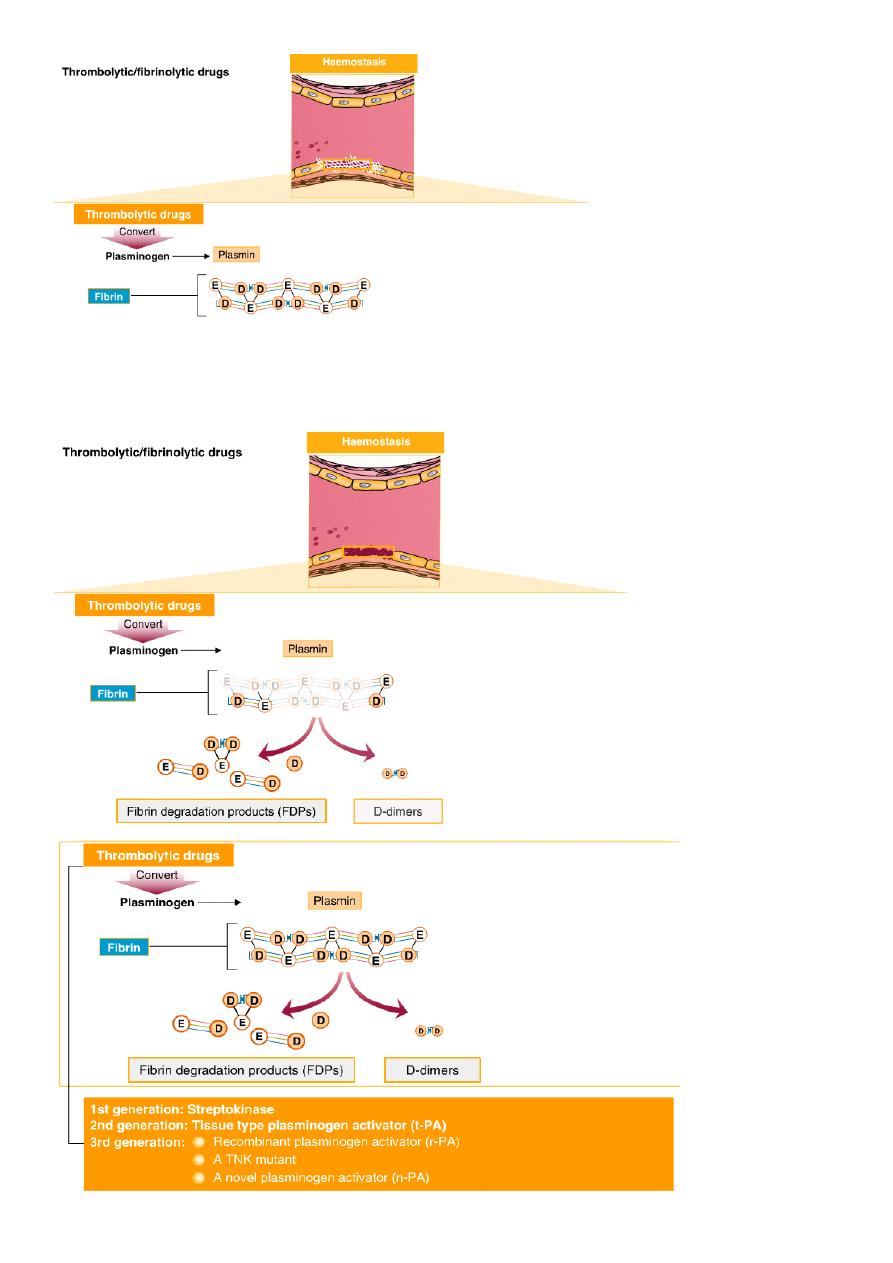
12

13
Thrombolytic drugs – pharmacokinetics
The plasma half-life of the third generation drugs is 14-45 minutes, allowing
administration as a single or double intravenous bolus. This is in contrast to second
generation t-PA, which with a half-life of 3-4 minutes, must be administered an initial
bolus followed by infusion
Thrombolytic drugs – major use
Thrombolysis in patients with acute myocardial infarction (MI)
Thrombolysis in patients with ischaemic stroke
Thrombolysis of (sub)acute peripheral arterial thrombosis
Thrombolysis in patients with acute massive pulmonary embolism
Thrombolysis of occluded haemodialysis shunts
Thrombolytic drugs – major drawbacks
Treatment is limited to acute in-hospital treatment. There is a high risk of bleeding
inherent in this treatment
Patients using anticoagulants are contraindicated for treatment with thrombolytics
