1
Fifth stage
Medicine
Lec-3
د . منوع
1/1/2014
Drugs used in respiratory diseases
B2-Agonists
Short-acting β
2
-agonists (as salbutamol)
They should be used for all patients with asthma.
Have a rapid onset of action (5 – 30 minutes) and effectively relieve bronchoconstriction
(for 4 – 6 hours)
Protect against exercise- and cold air–induced asthma.
Have no anti-inflammatory effect and should not be used as the sole therapy (alone),
except for mild intermittent asthma
Should be used as needed rather than on a regular scheduled basis.
Using β
2
-agonists by metered-dose inhaler is an effective means of drug delivery to the
lung.
Some patients may have difficulty mastering inhaler technique, particularity older
patients and those with musculoskeletal or neurologic disorders.
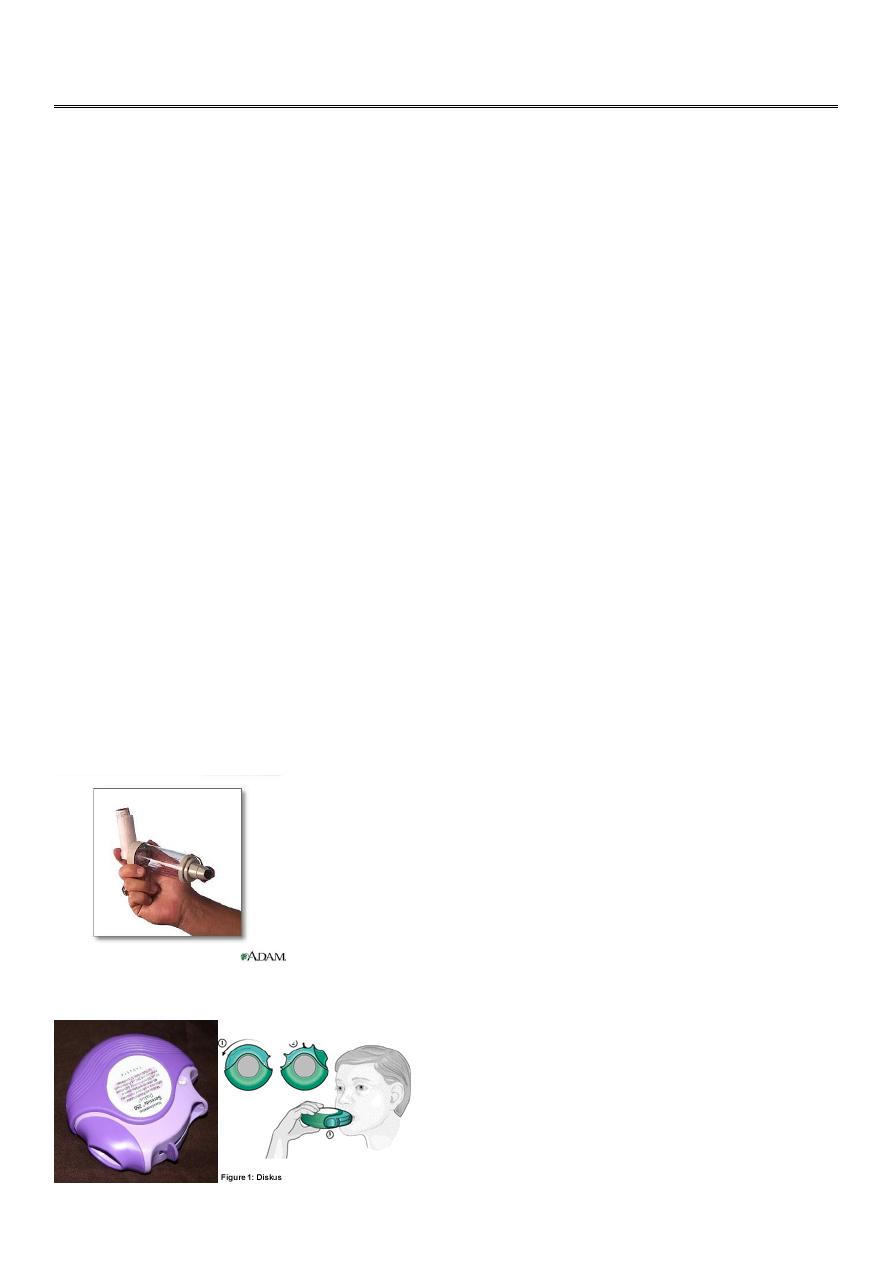
In such patients, inhalation aids or other modes of delivery (turbuhaler and diskus)
should be considered.
Inhalation aids
Diskus
2
Turbuhalor
Long-acting β
2
-agonists (LABA)
Salmeterol and formoterol provide bronchodilation for up to 12 hours and prevent
exercise-induced asthma.
Formoterol has a rapid onset of action while salmeterol has a relatively slow onset.
Adding LABA inhalers in patients whose disease is not controlled on low- to medium-
dose inhaled corticosteroids is superior to doubling the dose of inhaled corticosteroids
with regard to improving symptom control and reducing exacerbations.
LABA control asthma symptoms but have no anti-inflammatory effects. and should not
be used as single-agent therapy in asthma because this can lead to masking
inflammation and worsening of asthma control with increased risk for asthma-related
complications.
Fixed combination inhalers (containing both ICS and LABA) ensure better compliance
and prevent using LABAs as monotherapy
Inhaled β
2
-agonists are well tolerated in most patients; side effects may include tremor,
arrhythmias, and hypokalemia
Ipratopium is less effective than β
2
-agonists agonists in asthma and are restricted to
patients who can not tolerate these drugs.
Inhaled Corticosteroids (ICS)
Inhaled corticosteroids (ICS) exert an anti-inflammatory effect by reducing the number
of mast cells, eosinophils, and lymphocytes and by reducing cell activation.
As such, they reduce generation of cytokines by airway cells and block the late allergic
response to allergens.
Corticosteroids can also up-regulate β-adrenergic receptor function, thereby enhancing
the effectiveness of β
2
-agonists.

3
The regular use of ICS in patients with asthma improves lung function, decreases airway
hyperresponsiveness, reduces asthma exacerbations, and reduces asthma-related
mortality.
No other medications are as effective as ICS in the long term control of asthma.
If appropriately prescribed and used ICS therapy would reduce or eliminate the use of
oral steroids in severe asthma.
Beclomethasone, budesonide and fluticasone are commonly prescribed (500 µg
beclomethasone is the usual starting dose). Add-on therapy should be considered when
1000 µg is prescribed with persistent symptoms.
ICS dose can be increased to a maximum of 2000µg when the patient is still
symptomatic despite adding LABA, leukotrein modifier and theophylline.
Most side effects of inhaled corticosteroid therapy are local, such as dysphonia (in part
from myopathy of small muscles of phonation), oral thrush, and cough.
Regular and careful mouth-rinsing after the use of inhalers and the use of inhalation aid
devices can significantly reduce or eliminate the occurrence of these local side effects.
When these effects do occur, they can be managed with dose reduction (which often
alleviates dysphonia) and topical antifungal therapy for oral thrush.
However, some patients cannot tolerate the side effects and require alternative
controller medications.
The systemic side effects of inhaled corticosteroids are relatively uncommon but do
occur in patients on high-dose therapy.
These effects include adrenal suppression, reduced growth velocity in children, weight
gain, glaucoma, cataracts, osteopenia, and skin thinning.
Therefore, the lowest dose consistent with disease control should always be used.
Step-down therapy should be considered at regular intervals, perhaps every 3 months, if
the disease is adequately controlled.
Leukotriene Modifiers
leukotrienes have important effects in asthma, including vasodilatation, mucus
secretion, and inflammation.
Leukotriene-modifying drugs include the leukotriene receptor antagonists montelukast
and zafirlukast and the 5-lipoxygenase inhibitor zileuton.
In patients with asthma, leukotriene modifiers reduce symptoms, reduce the need for
short-acting β2-agonists, and prevent exercise-induced asthma.

4
These agents have only a modest anti-inflammatory effect, particularly compared with
that of inhaled corticosteroids
Leukotriene modifiers can be used as an alternative to corticosteroids (but are not
preferred therapy) for mild persistent asthma.
Patient response to leukotriene modifiers varies significantly, with a subset of patients
showing significant response and many others showing limited or no response.
Leukotriene modifiers may be appropriate for patients with aspirin-sensitive asthma,
exercise-induced asthma, and virus-induced wheezing.
Because of the need for close monitoring of liver function in patients treated with
zileuton and difficulty in maintaining adherence to therapy with this medication, which
is given four times a day, its use has been limited.
Leukotriene modifiers have been associated with the development of the Churg-Strauss
syndrome in patients with asthma who are tapering the dosage of oral corticosteroids. It
is unclear whether this is due to unmasking preexisting Churg-Strauss syndrome or a
direct causal relationship of the drug.
Recently, neuropsychiatric side effects, including agitation, depression, and suicide, have
been reported in patients taking leukotriene modifiers..
Theophylline
Theophylline is an inhibitor of phosphodiesterase.
It is a mild bronchodilator with limited anti-inflammatory effect. Other possible effects
of theophylline include improved respiratory muscle contraction and enhanced
respiratory ciliary function.
The therapeutic serum concentration of theophylline is between 5 and 12 µg/ml; such
side effects as tremor, palpitations, headache, nausea, and vomiting can occur in the
high therapeutic to slightly supratherapeutic range.
More serious side effects, such as life-threatening arrhythmias and seizures, can occur at
concentrations greater than 20 µg/ml.
Because of significant drug-drug interaction, these toxic concentrations can be reached
in a patient who previously had stable serum theophylline levels but who begins taking
an interfering medication, such as a fluoroquinolone antibiotic (for example,
ciprofloxacin).
Theophylline levels should therefore be monitored regularly and adjusted when patients
are given other medications that can interfere with the metabolism of this agent.

5
Because of these side effects, theophylline is not recommended as a first-line therapy
for chronic asthma. It should be considered as an add-on option in patients who do not
respond adequately to other controller treatments.
The use of theophylline in acute asthma exacerbation is not recommended because of
its limited added benefit as a bronchodilator and significant risk for toxicity.
Anti-IgE Antibody (OMALIZUMAB)
Omalizumab, a recombinant monoclonal antibody that binds to the Fc portion of IgE
antibody, preventing its binding to mast cells amd basophils
It is approved for use in patients with moderate to severe, persistent allergic asthma.
Omalizumab is given as a subcutaneous injection every 2 to 4 weeks based on patients’
weight and serum IgE levels.
It should be reserved mainly for patients with severe, poorly controlled asthma who do
not respond to other treatments.
Oral corticosteroids
Side effects of systemic steroids
1. Suppression of hypothalamic-pituitary-adrenal (HPA) axis: A dose of 7.5 mg prednisolone
(or equivalent) given for more than 3 weeks is likely to suppress the HPA axis and should
be reduced gradually at a rate that depends on the duration of therapy.
2. Osteoporosis: the most common side effect, caused by suppression of calcium
absorption, bone mineralization and sex hormone synthesis.
3. Cushing like syndrome: central obesity, mooning of the face, hirsutism, acne, striae (skin
thinning), bruises, wasting and weakness of proximal muscles.
5. Mood disturbance: depression, euphoria, insomnia or psychosis, mainly related to rapid
changes in steroid levels.
6. Hyperglycaemia and diabetes mellitus
7. Increase in blood pressure
8. Increase susceptibility to infections: including activation of latent TB.
9. Masking the inflammatory response to infection: perforation of a viscus may be masked
and there may be no febrile response to infection

6
COPD
Bronchodilators
The three types of commonly used bronchodilators are β
2
-agonists, anticholinergic
agents, and methylxanthines reduce symptoms and improve exercise performance.
Anticholinergic agents block the effect of acetylcholine on muscarinic receptors. Short-
acting agents, such as ipratropium, produce effects for 4 to 6 hours; long-acting agents
(also known as long-acting muscarinic antagonists), such as tiotropium, produce effects
for 24 hours. The primary side effect of the inhaled anticholinergic agents used for COPD
is dry mouth. Anticholinergic agents should be used with caution in patients with urinary
obstruction and narrow-angle glaucoma.
Short-acting β
2-
agonists are recommended at all stages of COPD for the alleviation of
symptoms such as dyspnea and treatment of exacerbations. Long-acting β
2
-agonists are
recommended when patients require regular and frequent bronchodilatory
management
Because they have a narrow therapeutic window, methylxanthines are usually used only
after other long-acting bronchodilators have been tried.
Combination bronchodilator therapy using medications with different durations and
mechanisms of action may increase the amount of bronchodilation achieved.
Combining a β2-agonist with an anticholinergic agent and/or a methylxanthine may
produce additional and more sustained therapeutic effects
Corticosteroids
Regular use of inhaled corticosteroids in patients with severe COPD (FEV
1
< 50%) who
experience recurrent exacerbations reduces the frequency of further exacerbations.
Inhaled corticosteroids should be added to bronchodilator therapy.
Combinations of inhaled corticosteroids and long-acting bronchodilators are more
effective than either therapy alone in reducing exacerbations and improving health
status.
The use of inhaled corticosteroids in the elderly must be carefully monitored because of
the risk of adverse effects such as osteopenia, cataracts, hyperglycemia, and
pneumonia, all of which may be particularly debilitating in elderly patients.
The use of short-term oral corticosteroids is beneficial only in exacerbations of COPD.
Long-term treatment is associated with significant side effects and is not recommended.
