
1
Fifth stage
pediatric
Lec-3
د.اثل
1/11/2015
CHRONIC DIARRHEA & Malabsorption
Chronic diarrhea is defined as a diarrheal episode that lasts for ≥14 days.
Etiology
1. INFECTIOUS ETIOLOGIES
– Enteric infections
– Small intestinal bacterial overgrowth
– Postenteritis syndrome
2. DIARRHEA ASSOCIATED WITH EXOGENOUS SUBSTANCES
Excessive intake of laxatives containing lactulose
3. ABNORMAL DIGESTIVE PROCESSES:
– Cystic fibrosis
– Chronic cholestasis
4. NUTRIENT MALABSORPTION:
– Congenital or acquired lactase deficiency
5. IMMUNE AND INFLAMMATORY:
– Food allergy (cow's milk or soy proteins, others)
– Celiac disease
6. STRUCTURAL DEFECTS
– Microvillus inclusion disease
– Lymphangiectasia
7. DEFECTS OF ELECTROLYTE AND METABOLITE TRANSPORT:
– Congenital chloride diarrhea
– Congenital sodium diarrhea
8. MOTILITY DISORDERS
– Hirschsprung disease
– Thyrotoxicosis
9. NEOPLASTIC DISEASES
– Neuroendocrine hormone-secreting tumors ( VIPoma)
10. CHRONIC NONSPECIFIC DIARRHEA
– Functional diarrhea (toddler's diarrhea)
– Irritable bowel syndrome

2
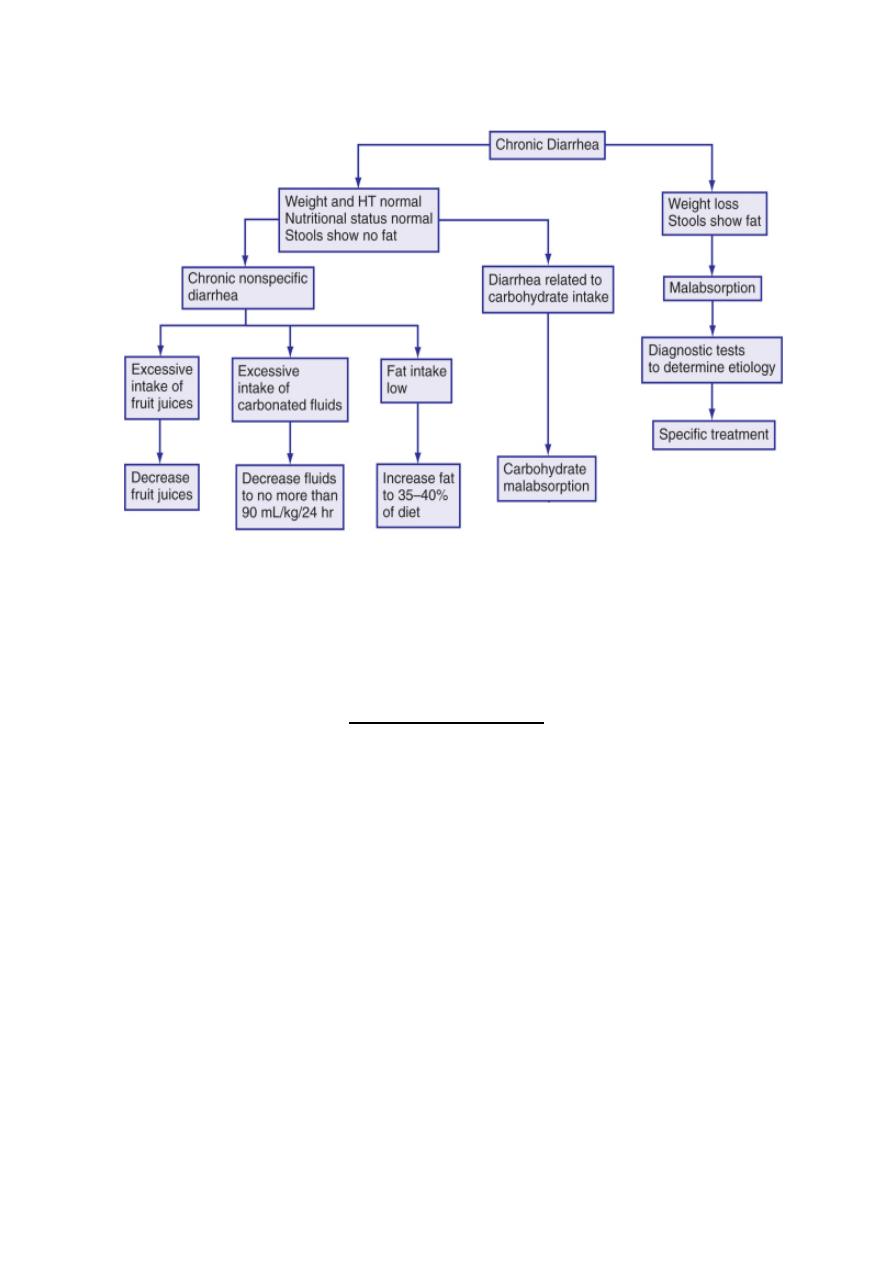
Evaluation of Patients
medical approach should be based on diagnostic algorithms :
– clinical and epidemiologic factors:
– History
Age
Personal & family history(cong, allergy, inflam)
Previous episode of acute GE.
Association with specific foods
Polyhydromnios
Specific amount of fluid ingested /day
Examination:
General & nutritional status
NOTE: Nutritional evaluation: include
• Diatery hx
• Nutritional state, growth parameters, anthropometric
evaluation→estimate the severity of diarrhea
• Biochemical markers
• Nutritional inv
Biochemical markers assist in grading malnutrition, the half life of serum
proteins can differentiate between short & long term malnutition.
Stepwise diagnostic work-up for children with chronic diarrhea
step 1
Intestinal microbiology (GSE, microscopy for parasites, viruses, stool cultures), stool
electrolytes, pH & reducing substances, H
2
breath test
Blood studies (CBC, ESR, electrolytes, blood urea, creatinine)
Screening test for celiac disease
Noninvasive tests for:
• Intestinal function
• Pancreatic function and sweat test
• Intestinal inflammation
Tests for food allergy
3
• Prick/patch tests
STEP 2
Intestinal morphology
- Standard jejunal/colonic histology
-Morphometry
STEP 3
Special investigations
• Intestinal immunohistochemistry
• Hormonal studies
• Autoantibodies
• Brush border enzymatic activities
• others
Treatment
Replacement of fluid and electrolyte
-
Empirical antibiotic therapy
-
nutritional rehabilitation
-
Human immunoglobulins
-
Zinc
-
-
Treatment of underlying cause
-
4
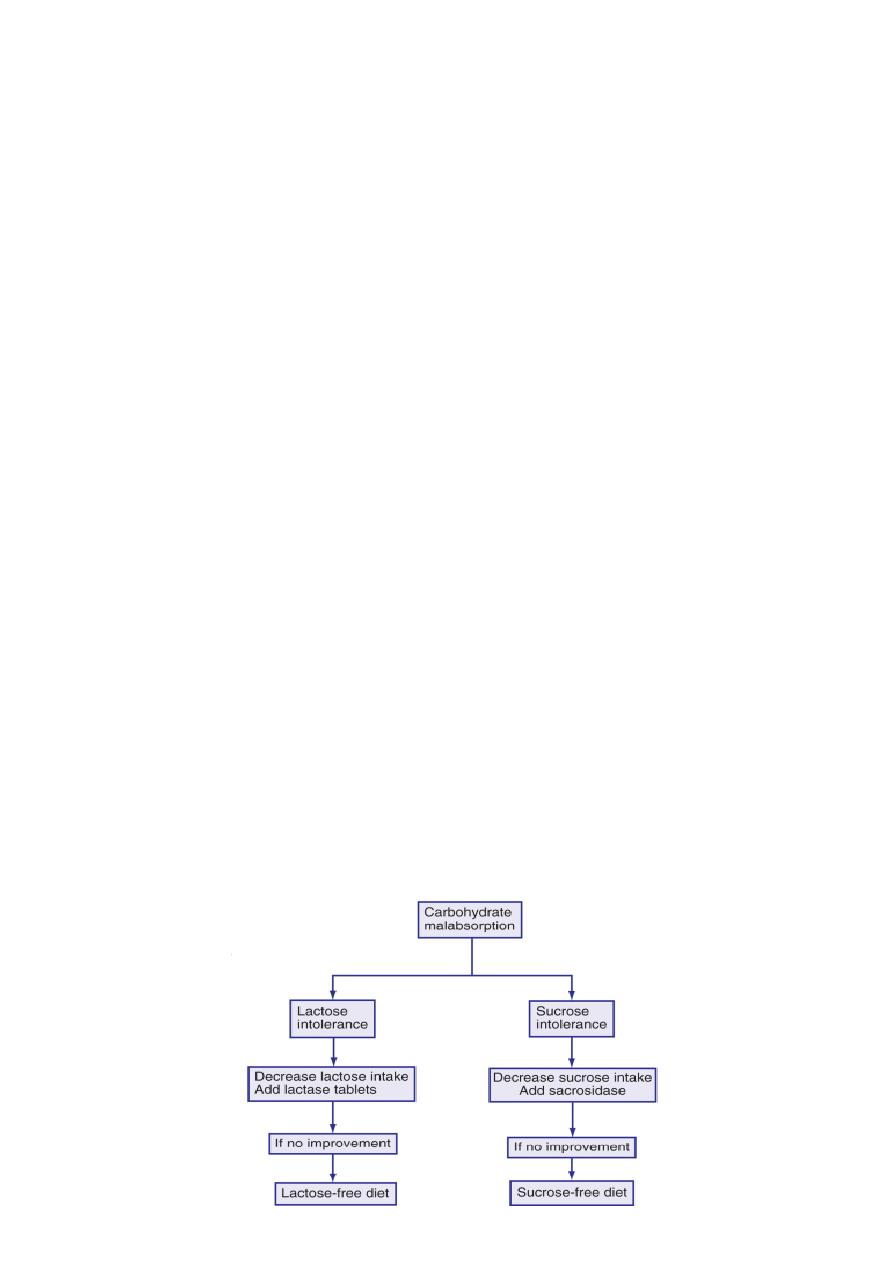
General therapeutic approaches to management of chronic diarrhea
Lactose Intolerance
What is Lactose Intolerance?
• Inability to digest significant amounts of lactose, which is the predominant sugar in
milk
• A result of lactase insufficiency, the enzyme essential for the conversion of lactose
into glucose and galactose
Types of Lactose Intolerance
– Congenital ( Very rare)
– Primary ( Develops after 2 years of age)
– Secondary (Usually resolves in 1-2 weeks)
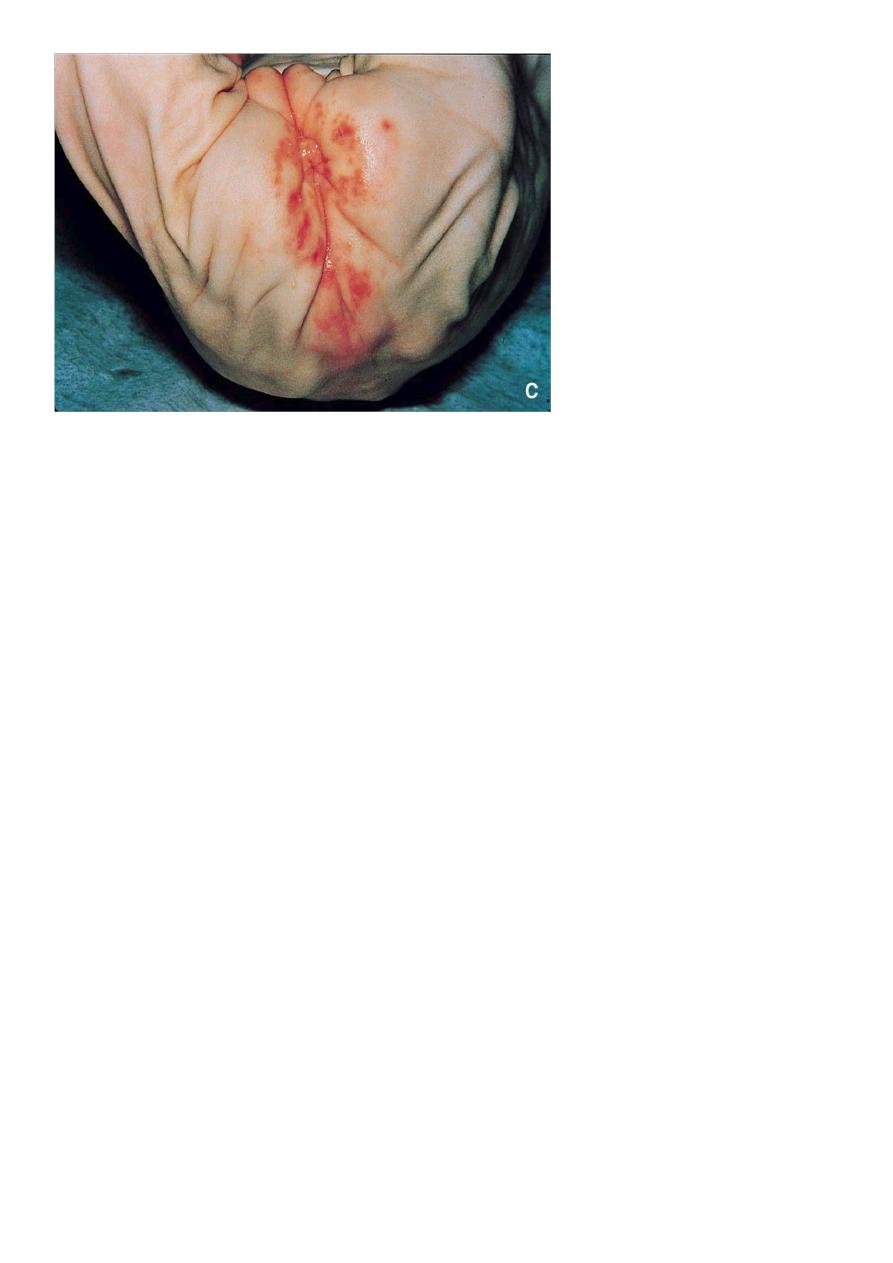
Clinical Manifestation
• Nausea, cramping, bloating, abdominal pain, gas, diarrhea, perianal
excoriation
5
DIAGNOSIS:
Stool
pH < 5.5
.
Positive
reducing
substance in stool
.
Low
lactase activity in
jejunal
mucosa
.
Increased in expired air
H2
.
TREATMENT
• Reduce lactose in diet . (SOY PROTEIN FORMULA) ISOMIL
ISOMIL
Isomil/Prosobee
– 20cal/oz
– palm olein, soy, coconut, sunflower oil
– Corn syrup/sucrose
– Protein, 17 g/L
soy isolate and L-MET
– Iron 12mg/L
– Vitamin D 405 IU/L
– 200 mOsm/kg H2O
– DHA and AA added (docosahexaenoic acid and arachidonic acid)
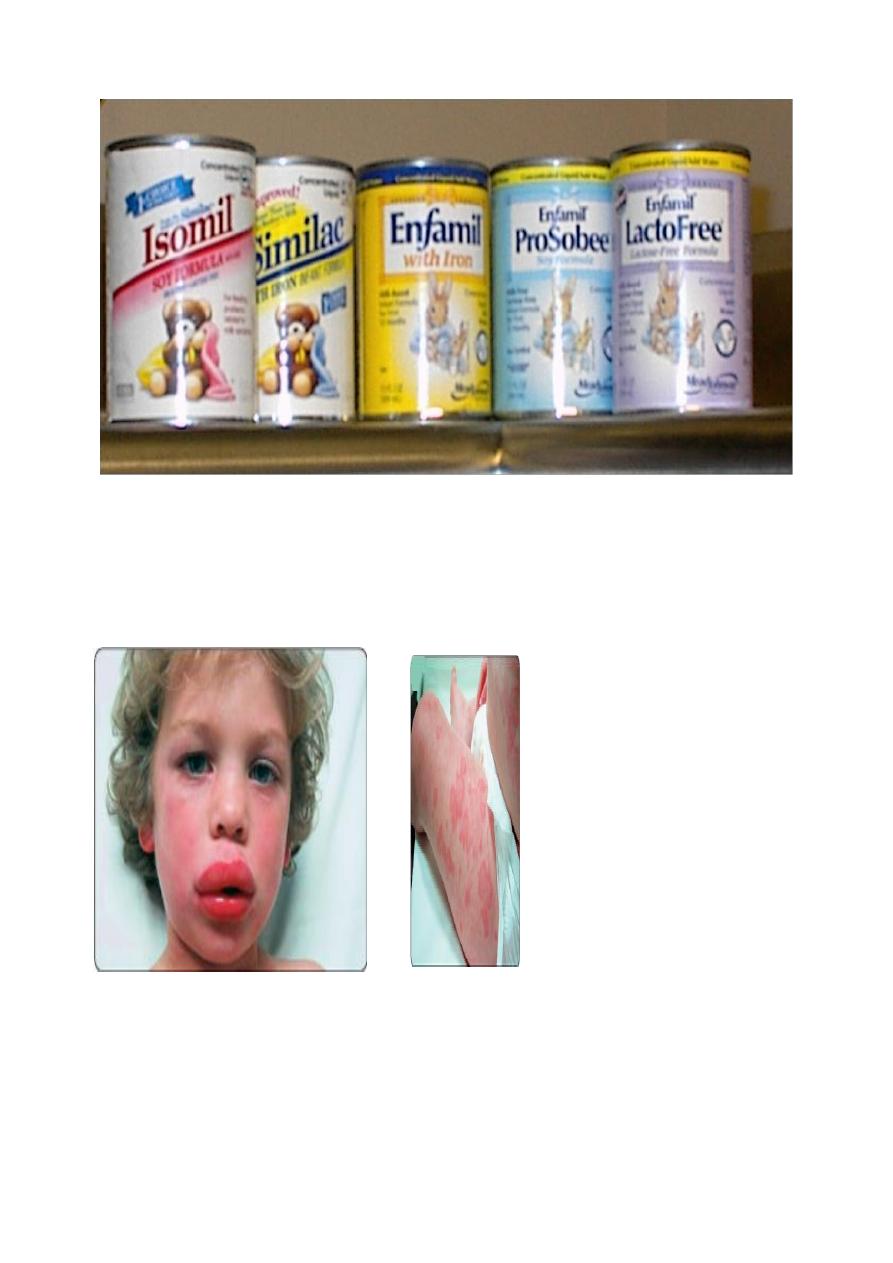
6
SOY PROTEIN FORMULA
COW’S MILK ALLERGY
7
What is Milk Allergy?
• An abnormal immune system reaction to proteins in the cow’s milk
• Triggered by a combination of genetically inherited factors and early introduction of
cow’s milk or soy protein into an infant’s diet
Symptoms of Milk Allergy
- An immune system reaction
- Gastrointestinal Manifestations :vomiting , diarrhea malabsorption ,protein losing
enteropathy , colic, GIT bleeding , FTT
- Systemic Manifestations : anaphylaxis, rhinitis, wheezing, pulmonary hemosiderosis,
peripheral eosinophilia, IDA 2ry to GIT bleeding.
DIAGNOSIS
Mainly Clinical
– Symptoms disappear after withdrawal of cow’s milk .
– Very cautious CHALLENGE WITH FEW CC of cow’s milk produces the
symptoms again.
TREATMENT
• SOY PROTEIN [ (30-50%) are also allergic to soy protein.
• HYDROLYSED MILK FORMULA
) Pregestemile).
HYDROLYSED MILK FORMULA

8
Protein Hydrolysate Formulas
-Alimentum Advance
-Pregestimil/Pregestimil Lipil
-Nutramigen Lipil
-Protein Casein hyrolysate + free AA’s
-Fat (Alimentum and Pregestimil) Medium chain + Long chain triglycerides;
(Nutramigen) Long chain triglycerides
-Carbohydrate: Lactose free
PROGNOSIS
- Most cases recover spontaneously within 1-2 years.
TODDLERS DIARRHOEA
• A pattern of intermittent loose stools, occurs commonly between 1 and 3 yr of age.
These otherwise healthy growing children often drink excessive carbohydrate-
containing beverages. The stools typically occur during the day and not overnight.
The volume of fluid intake is often excessive; limiting sugar-containing beverages and
increasing fat in the diet often leads to resolution of the pattern of loose stools.
