
1
Fifth stage
Pediatric
Lec-1
.د
أ
ثل
1/1/2016
DIARRHOEA in INFANCY & CHILDHOOD
Objectives
To define diarrhea & gastroenteritis.
To differentiate between the types of diarrhea.
To know the mechanism of each type.
To know the etiologies of GE.
To know the risk factors of GE.
To know the clinical features of GE & how clinically evaluate the degree of
dehydration.
How can investigate a patient with GE?
Acute Gastroenteritis in Children
The term gastroenteritis captures the bulk of infectious cases of diarrhea. The term
diarrheal disorders is more commonly used to denote infectious diarrhea in public health
settings, although several noninfectious causes of gastrointestinal illness with vomiting
and/or diarrhea are well recognized.
The term gastroenteritis denotes infections of the gastrointestinal tract caused by
bacterial, viral, or parasitic pathogens
Diarrhea
Refers to:
Abnormal increase in frequency and liquidity of fecal discharges.
OR
Stool output >10 g/kg/24 hr, or more than the adult limit of 200 g/24 hr.
EPIDEMIOLOGY OF CHILDHOOD DIARRHEA
Diarrheal disorders in childhood account for a large proportion (18%) of childhood deaths.
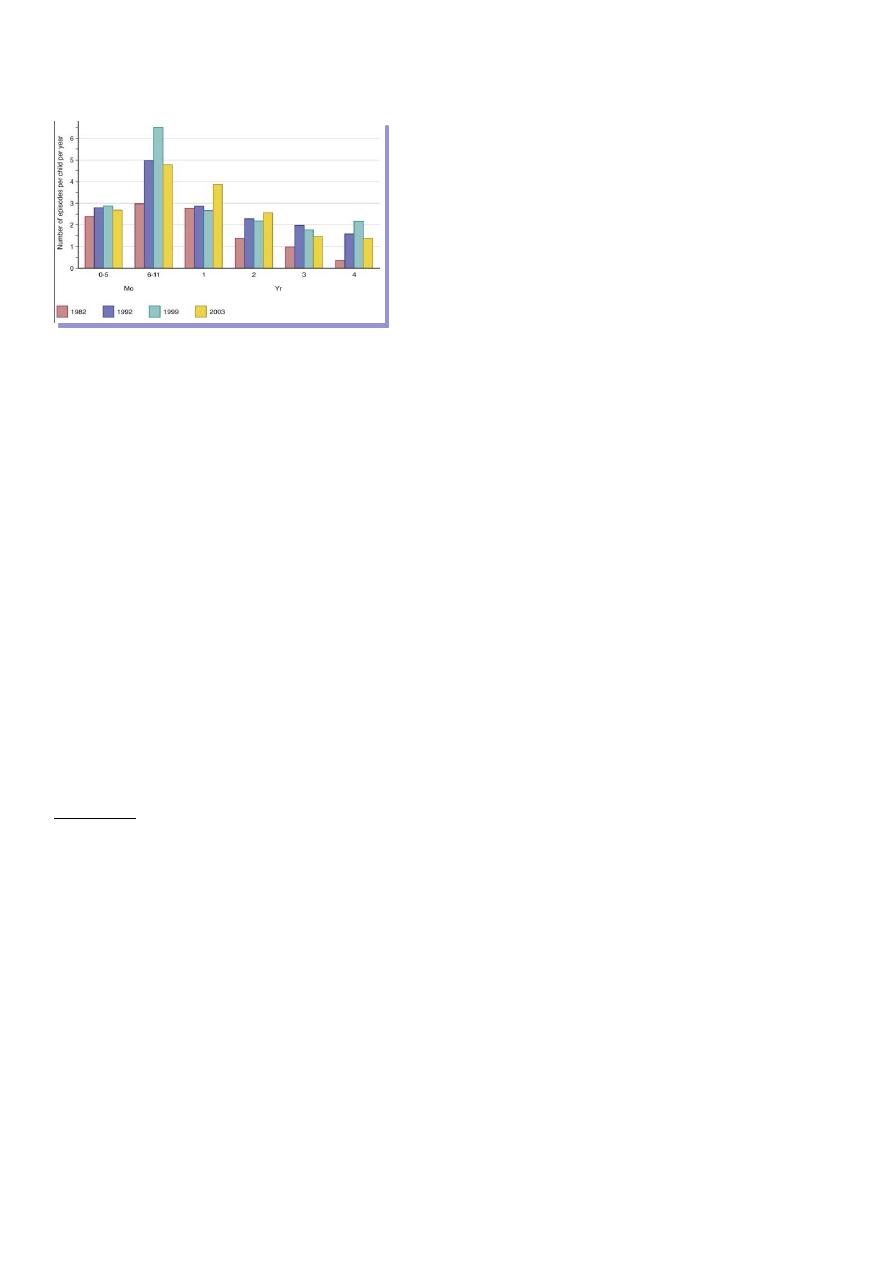
2
with an estimated 1.5 million deaths per year globally, making it the second most common
cause of child deaths worldwide..
TYPES OF DIRRHEA
i.
Acute watery diarrhea (<14 days
ii.
Dysentery (visible blood in stool.
iii.
Persistent diarrhea (>14 days .
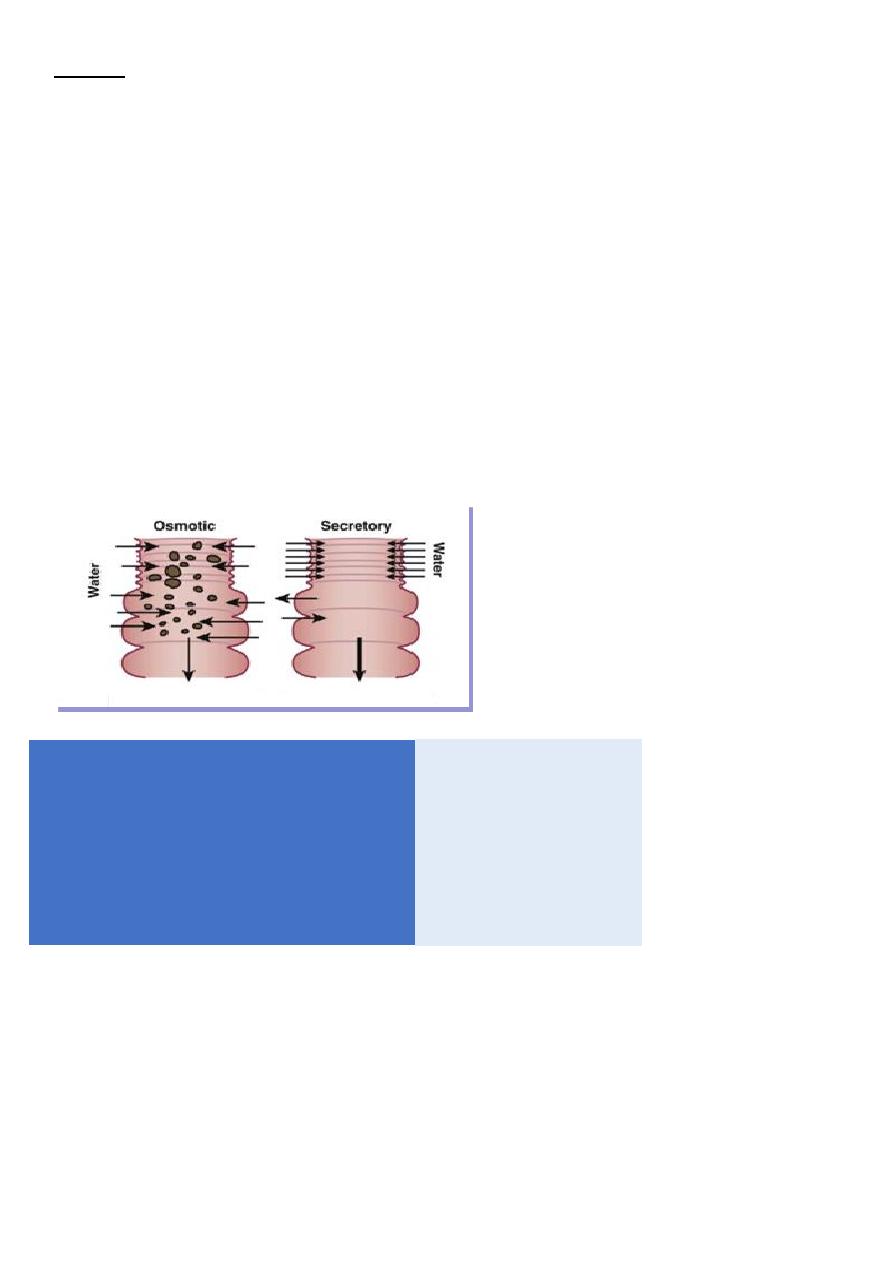
MECHANISM OF DIARRHEA
The basis for all diarrhea is disturbed intestinal solute transport; water movement across
intestinal membranes is passive and is determined by both active and passive fluxes of
solutes, particularly sodium, chloride, and glucose .
The pathogenesis of most episodes of diarrhea can be explained by secretory, osmotic, or
motility abnormalities or a combination of these
Secretory:
Defect
Increased secretion
Decreased absorption
Examples
Activation of cAMP: Cholera, toxinogenic E.coli(LT )
Shigella, Salmonella, Campylobacter jejuni
Pseudomonas aeruginosa
Activation of cGMP: E. coli (ST) , Yersinia enterocolitica toxin
Comments
Persists during fasting
No stool leukocytes
3
Osmotic
Defect present
Digestive enzyme deficiencies
Ingestion of unabsorbable solute
Examples
Malabsorption: Disaccharidase deficiencies (lactase )(rota virus cause lactase def)
Excessive intake of carbonated fluid
Excessive intake of non absorbable solute: Lactulose
Comments
Stop with fasting
No stool WBCs
•
Large volume
>200ml/24h
•
>70
•
Diarrhea continue
•
< 100
•
>6
•
-ve
• Moderately
increase
<200ml/24h
• < 70mEq/l
• diarrhea stop
• >100mosm/kg
• < 5
• +ve
• Stool volme
• Stool Na
• Fasting
• Ion gap
• Stool PH
• Reducing
subst
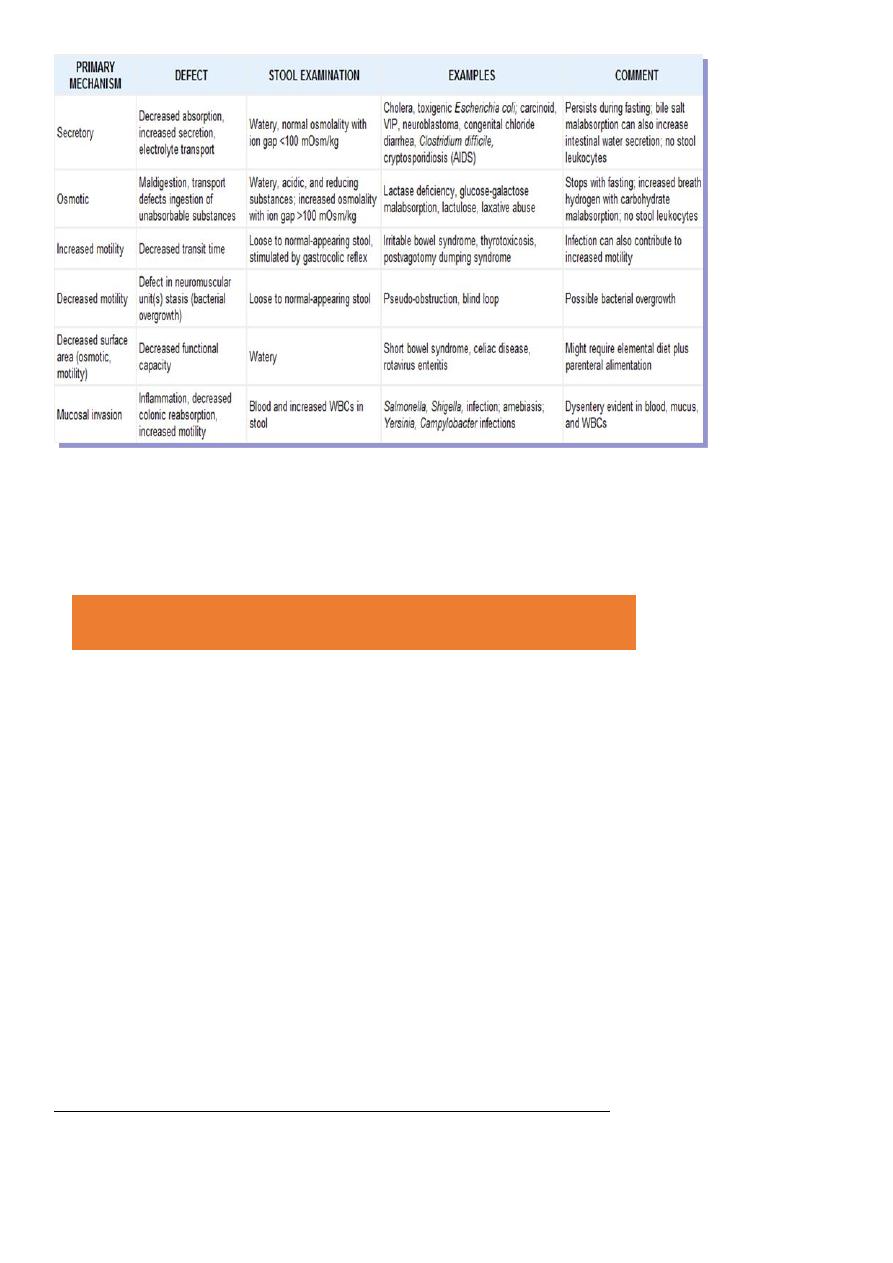
4
NOTE
The stool osmolality is indicated by the electrolytes and the ion gap is 100 mOsm/kg or less .
The ion gap is calculated by subtracting the concentration of electrolytes from total
osmolality:
PATHOLOGY
1.Noninflammatory Diarrhea
Through
i.
enterotoxin production by some bacteria
ii.
destruction of villus (surface) cells by viruses
iii.
adherence by parasites, and by bacteria.
2.Inflammatory Diarrhea
usually caused by bacteria that
directly invade the intestine
produce cytotoxins with consequent fluid, protein, and cells (erythrocytes, leukocytes)
that enter the intestinal lumen.
Some enteropathogens possess more than one virulence property
Ion gap = Stool osmolality – [ (stool Na + stool K) × 2]
5
ETIOLOGY OF DIARRHEA
Infectious Diarrhea
Gastroenteritis is due to infection acquired through the feco-oral route or by ingestion of
contaminated food or water .
Gastroenteritis is associated with poverty and poor environmental hygiene .
Viral gastroenteritis
i.
Viral gastroenteritis (“stomach flu”)
rotavirus
ii.
noroviruses (small round viruses such as Norwalk-like virus and caliciviruses)
iii.
sapovirus
iv.
enteric adenoviruses
v.
astroviruses
Rotavirus
Rotavirus invades the epithelium and damages villi of the upper small intestine and in
severe cases involves the entire small bowel and colonRotavirus is the most frequent cause
of diarrhea during the winter months. Vomiting may last 3 to 4 days, and diarrhea may last
7 to 10 days.
Dehydration is common in younger childrenUsually cause watery diarrhoea no blood
and pus in stool
Bacterial gastroenteritis
Escherichia Coli
i.
gram-negative bacilli
ii.
major groups of diarrheagenic E. coli :
iii.
enterotoxigenic E. coli (ETEC)
iv.
enteroinvasive E. coli (EIEC)
v.
enteropathogenic E. coli (EPEC)
vi.
Shiga toxin–producing E. coli (STEC)also known
vii.
as enterohemorrhagic E. coli (EHEC)
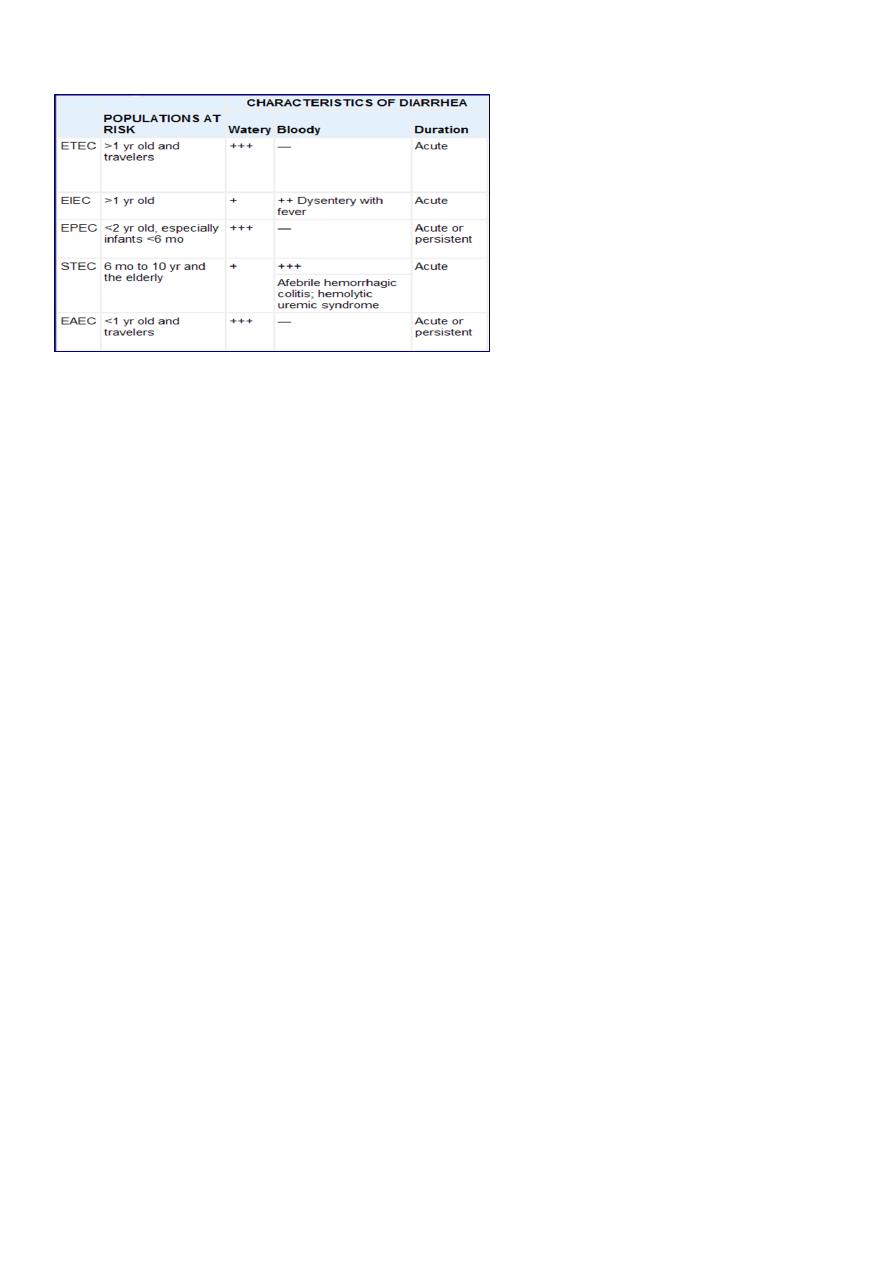
6
viii.
enteroaggregative E. coli (EAEC).
Shigella
Four species of Shigella are responsible for bacillary dysentery :
S. dysenteriae
S. flexneri
S. boydii
S. sonnei
It is most common in the 2nd and 3rd year of life, infection in the 1st 6 mo of life is rare
(may be due to Breast feeding)
The colon is the target organ for shigellae
Symptoms :
generalized toxicity
urgency, and painful defecation characteristically occur.
watery → bloody mucoid stools
Convulsions, headache, lethargy, confusion, nuchal rigidity, or hallucinations may be
present before or after the onset of diarrhea .
Salmonella
Salmonella causes 2 clinical syndromes in humans: a GE that is usually self-limited, and
typhoid fever that is a relatively severe systemic illness classically caused by S. typhi.
Nontyphoidal strains of Salmonella can also cause a severe bacteremic illness in some
circumstances.

7
CLINICAL MANIFESTATIONS.
Acute Enteritis :
mild to severe watery diarrhea
Bloody diarrhea
Campylobacter
The organism invades the mucosa of the jejunum, ileum, and colon, producing
enterocolitis.
DISEASES IN HUMANS: Gastroenteritis, bacteremia, Guillain-Barré syndrome
Acute Gastroenteritis.
Watery or bloody diarrhea
The abdominal pain is periumbilical; cramping but may mimic appendicitis or
intussusception.
Yersinia Enterocolitica
Infants & young children characteristically have a diarrheal disease, whereas older
children usually have acute mesenteric lymphadenitis mimicking appendicitis or Crohn
disease. Arthritis, rash, and spondylopathy may develop.
Parasitic gastroenteritis
Entamoeba histolytica
Clinical presentations range from asymptomatic cyst passage to amebic colitis, amebic
dysentery, ameboma, and extraintestinal disease as amebic liver disease.
Amebic colitis, gradual onset of colicky abdominal pains and frequent bowel
movements (6–8/day). Diarrhea is frequently associated with tenesmus. Stools are blood
stained and contain a fair amount of mucus with few leukocytes. Generalized constitutional
symptoms and signs are characteristically absent, with fever documented in only ⅓ of
patients.
Giardia Lamblia
It infects the duodenum and small intestine

8
Clinically: asymptomatic, acute infectious diarrhea (insidious onset of progressive anorexia,
nausea, gaseousness, abdominal distention, watery diarrhea) or chronic diarrhea with
persistent GIT signs and symptoms, including FTT and abdominal pain or cramping.
There is usually no extraintestinal spread.
Non-infectious diarrhea
i.
Allergy to milk or its components
ii.
Malabsorption
iii.
Endocrinopathies
iv.
Poisoning
v.
Neoplasia e.g.: neuroblastoma
vi.
IBD
vii.
Drugs / medications
viii.
Traveller’s Diarrhoea
Diarrhea
1.watery
2.bloody
Watery diarrhea
Viral enteritis
Enterotoxin producing bacteria:
Escherichia coli
Klebsiella organisms
Clostridium perfringens
Vibrio species
Parasitic GE:
Giardia
Cryptosporidium
Extraintestinal Infections:
Parenteral Diarrhea e.g.: otitis media & urinary tract infection
.
9
Bloody diaeehea
BACTERIAL
Shigella
Salmonella
Campylobacter
Yersinia enterocolitica
Invasive E. coli
NON-BACTERIAL
Amoebic dysentery
Pseudomembranous enterocolitis (C. difficile toxin )
Ulcerative or granulomatous colitis (acute presentation )
Necrotizing enterocolitis in neonates
RISK FACTORS FOR GASTROENTERITIS
Major risks include environmental contamination and increased exposure to
enteropathogens.
Additional risks include:
Lack of exclusive or predominant breast-feeding .
Young age
Immune deficiency
Measles
Malnutrition, malnutrition increases severalfold the risk of diarrhea and associated
mortality.The risks are particularly higher with micronutrient malnutrition; in children with
vitamin A deficiency, the risk of dying from diarrhea, measles, and malaria is increased by
20–24%. Zinc deficiency increases the risk of mortality from diarrhea, pneumonia, and
malaria by 13–21%.
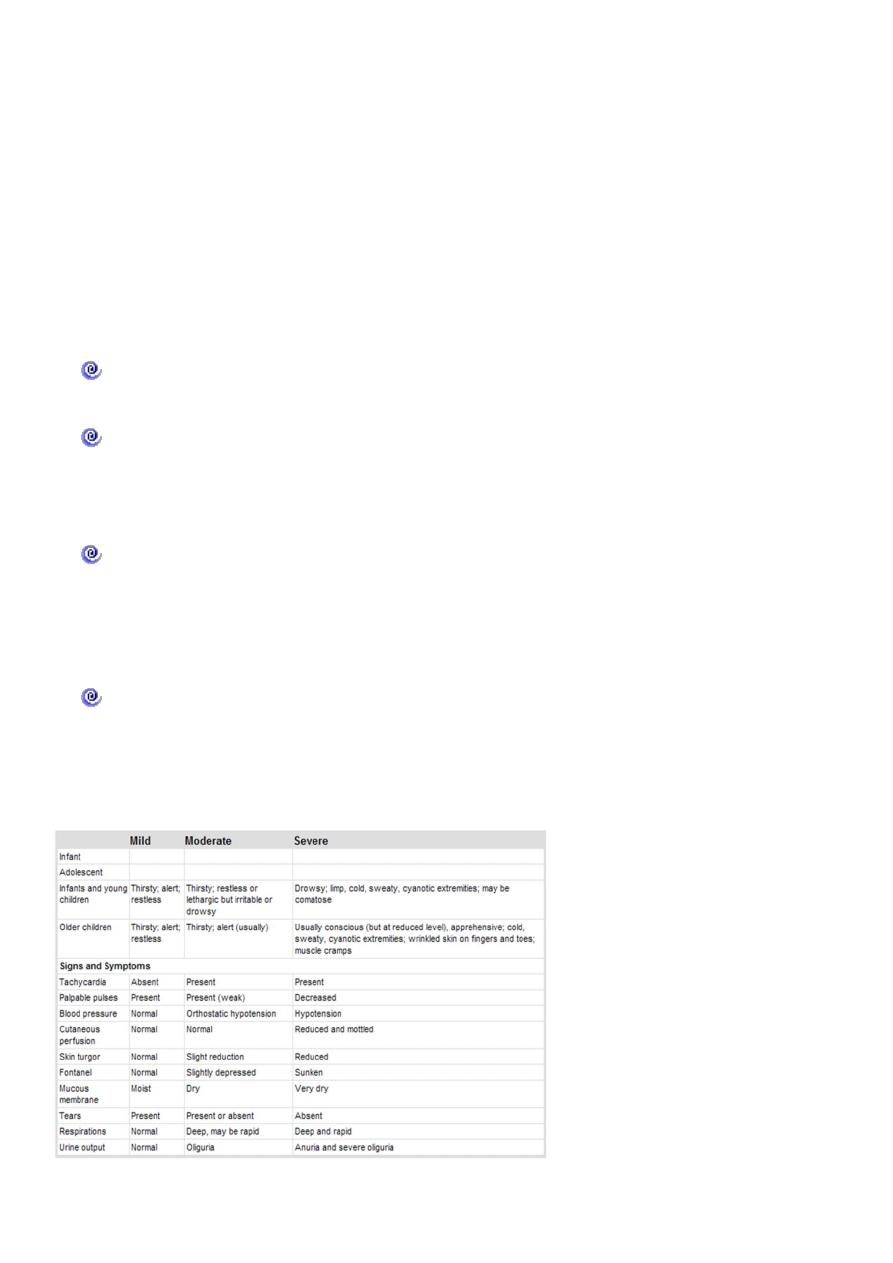
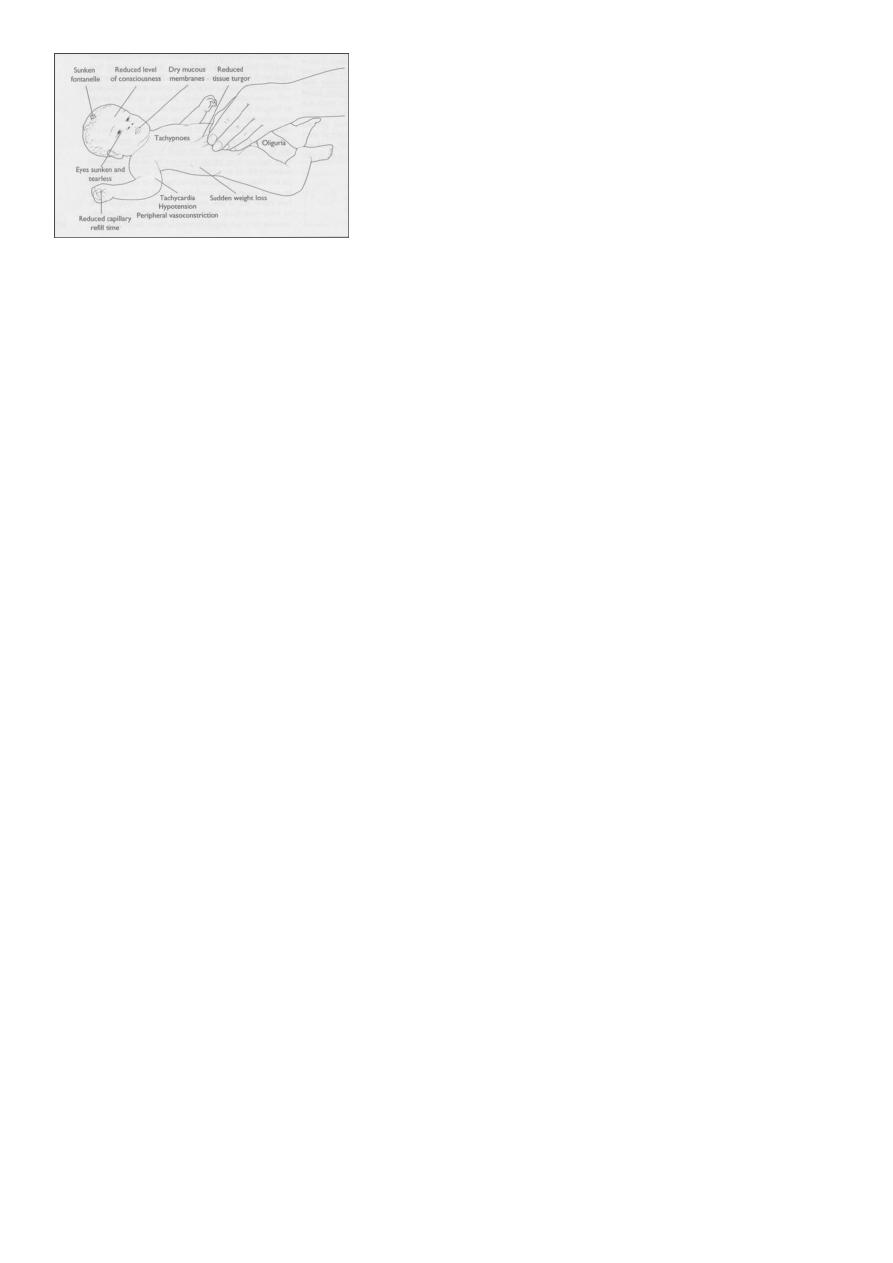
CLINICAL MANIFESTATIONS
Diarrhea, vomiting ,nausea, anoroxia, abdomenal distension, abdominal cramps.
Manifestation of complications: dehydration & electrolyte disturbance.
11
Extra intestinal: Fever, malaise, reactive arthritis, systemic spread of M.O., Guillain-
Barre Synd, HUS, hemolytic anaemia.
DIAGNOSIS OF GE
The diagnosis of gastroenteritis is based on clinical recognition, an evaluation of its
severity by rapid assessment, and confirmation by appropriate laboratory investigations, if
indicated.
CLINICAL EVALUATION OF DIARRHEA
Assess the degree of dehydration and acidosis and provide rapid resuscitation
and rehydration with oral or intravenous fluids as required
Obtain appropriate contact or exposure history. This includes information on
exposure to contacts with similar symptoms, intake of contaminated foods or water,
child-care center attendance, recent travel to a diarrhea-endemic area, and use of
antimicrobial agents.
Clinically determine the etiology of diarrhea for institution of prompt antibiotic
therapy, if indicated. Although nausea and vomiting are nonspecific symptoms, they
are indicative of infection in the upper intestine. Fever is suggestive of an
inflammatory process but also occurs as a result of dehydration or co-infection (e.g.,
urinary tract infection, otitis media).
Fever is common in patients with inflammatory diarrhea. Severe abdominal pain
and tenesmus are indicative of involvement of the large intestine and rectum.
Features such as nausea and vomiting and absent or low-grade fever with mild to
moderate periumbilical pain and watery diarrhea are indicative of small intestine
involvement and also reduce the likelihood of a serious bacterial infection.
11
LABORATORY STUDIES
Initial laboratory evaluation of moderate to severe diarrhea includes:
electrolytes
Blood sugar.
BUN, creatinine
Blood pH , S. [HCO3]
urinalysis for specific gravity as an indicator of hydration.
CBP .
GSE for:
Macroscopical
Microscopical.: mucus, blood, and leukocytes
Chemical
Stool cultures are recommended for patients with:
fever
profuse diarrhea
if HUS is suspected.
bloody diarrhea.
in immunosuppressed children with diarrhea.
ELISA for rotavirus..
The diagnosis of E. histolytica is based on identification of the organism in the stool.
Serologic tests are useful for diagnosis of extraintestinal amebiasis, including amebic
hepatic abscess.
Giardiasis can be diagnosed by identifying trophozoites or cysts in stool; less often a
duodenal aspirate or biopsy of the duodenum or upper jejunum is needed.
GUE
